A 32-year-old male patient, a known case of non-cirrhotic portal fibrosis (NCPF), on follow-up endoscopic examination was found to be having a small submucosal bulge in the duodenal bulb. He had variceal bleed 3 years ago and thereafter the varices were eradicated by endoscopic variceal ligation. Since then, he has been on beta blockers and regular follow up. His serum bilirubin was 0.7 mg/dL (N: 0.3-1.3 mg/dL) but his serum alkaline phosphatase was elevated, being 182 IU/L (N: 42-128 IU/L) with normal aminotransferases. Abdominal ultrasound revealed prominent central intrahepatic biliary radicles with prominent intra-abdominal venous collaterals. Endoscopic ultrasound (EUS) revealed thickened common bile duct wall with a maximum diameter of 7 mm. There were multiple peri-choledochal venous collaterals (Fig. 1). The duodenal wall was found to be thickened and there was a small anechoic lesion in the wall of the duodenum (Fig. 1; small arrow). On color Doppler imaging, this anechoic lesion demonstrated vascularity and on pulsed mode it had a venous flow pattern, suggestive of duodenal varix (Fig. 1, DV). On careful inspection, the communication of this varix to the peri-choledochal venous plexuses could be demonstrated (Fig. 2, arrow). Since the patient is asymptomatic, he has been advised regular follow up with periodic liver function tests and endoscopy.
Figure 1.
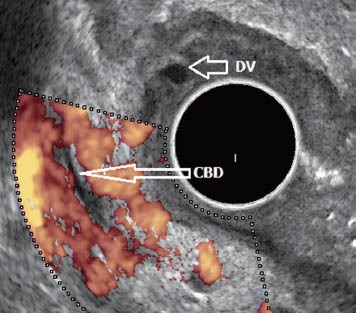
Multiple peri choledochal venous collaterals. CBD: common bile duct; DV: duodenal varix.
Figure 2.
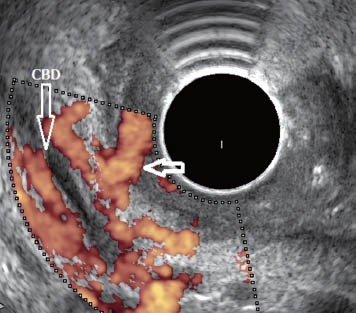
Duodenal varix communicating with peri choledochal venous plexuses (arrow).
Duodenal varices (DV) are a very rare complication of portal hypertension and the duodenal bulb is the most common site, followed by the second part of the duodenum.1,2 The afferent vessel to DV arises either from the superior or inferior pancreaticoduodenal vein or from the superior mesenteric vein, and the blood from DV flows either hepatofugally into the inferior vena cava via retroperitoneal shunts or hepatopetally through portoportal collaterals that develop either from the preformed peri-choledochal plexuses or from the patent tributaries of the portal vein (in patients with extra hepatic portal vein obstruction)1,3,4. Increased blood flow in these collateral vessels can lead on to formation of DV or portal hypertensive biliopathy.
REFERENCES
- 1.Hashizume M, Tanoue K, Ohta M, et al. Vascular anatomy of duodenal varices: angiographic and histopathological assessments. Am J Gastroenterol. 1993;88:1942–5. [PubMed] [Google Scholar]
- 2.Rana SS, Bhasin DK, Singh K. Duodenal varix diagnosed by endoscopic ultrasound. Clin Gastroenterol Hepatol. 2010;8:A24. doi: 10.1016/j.cgh.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 3.Yoshida S, Watabe H, Akahane M, et al. Usefulness of multi-detector helical CT with multiplanar reconstruction for depicting the duodenal varices with multiple collateral shunt vessels. Hepatol Int. 2010;4:775–8. doi: 10.1007/s12072-010-9191-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cottam D, Clark R, Hayn E, et al. Duodenal varices: a novel treatment and literature review. Am Surg. 2002;68:407–9. [PubMed] [Google Scholar]


