Abstract
Objective:
Endoscopic ultrasound-guided choledochoduodenostomy (EUS-CD) has become an alternative method after unsuccessful endoscopic retrograde cholangiopancreatography (ERCP) treatment. We present a case series study and its feasibility by using only a linear therapeutic channel echoendoscope to create both a biliary-enteral fistula and anatomic enteral recanalization.
Methods:
We presented seven cases of unresectable periampullary cancer with both biliary and duodenal obstruction. In these cases, the EUS-guided technique might be an alternative to double stenting (biliary and enteral) in the same procedure and equipment.
Results:
In all cases, the location of the biliary obstruction was in the distal common bile duct (CBD) and the grade of proximal dilation diameter varied from 15 mm to 20 mm. Two patients had type I (28.6%) and five had type II (71.4%) duodenal obstruction. Technical success of EUS-CD, by the stent placement, occurred in 100% of the cases. There were no early complications. Biliary drainage was effective clinically as well as in laboratory in 6 cases (6/7), by relieving obstructive jaundice and decreasing bilirubin levels.
Conclusion:
EUS equipment may offer an alternative to double stenting in the same procedure and with palliative propose.
Keywords: endoscopic retrograde cholangiopancreatography, endoscopic ultrasound, choledochoduodenostomy, periampullary cancer
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is the first-line therapy for palliative biliary drainage in patients with unresectable periampullary cancer.1,2,3,4,5 Its success rate varies from 90% to 95%; however, even when performed by experienced endoscopists, cannulation may be failed.6,7,8,9
Percutaneous transhepatic biliary drainage (PTBD) is an rationale option prior to the surgery, but may cause several complications, which can be bleeding, hemobilia, peritonitis and liver abscess, and poor quality of life due to the presence of an external catheter.10 Complication, morbidity and mortality rates of PTBD are 30%, 7% and 5%, respectively.4,11,12 Surgical treatment offers long period of drainage patency, but also with high rates of morbidity and mortality.12
Endoscopic ultrasound (EUS) is an established method for diagnosis of biliary and pancreatic diseases. In 1996, Wiersema et al. published the first case of EUS-guided cholangiopancreatography13. Giovannini et al.14 pioneered, in 2001, by performing a EUS-guided choledochoduodenostomy (EUS-CD). Several case studies analyzed the role of EUS-CD as an alternative method after unsuccessful ERCP in patients with unresectable periampullary cancer.2,4,15,16,17,18,19,20,21
That tumors when in advanced stages, causes biliary obstruction and also duodenal obstruction.22 Although biliary obstruction usually occurs prior to duodenal, they can occur simultaneously.22,23,24,25 In these cases, the use of self-expandable metal stents (SEMS) to stent the biliary duct and the duodenal lumen has been proved effective as palliative treatment.26
We present here a case series study and the feasibility by using only a linear therapeutic channel echoendoscope to create both a biliary-enteral fistula and anatomic enteral recanalization in seven patients with obstructive jaundice and duodenal obstruction due to unresectable periampullary cancer.
PATIENTS AND METHODS
EUS-CD, in the first portion of the duodenum, associated with duodenal SEMS placement was performed in seven patients with unresectable periampullary cancer that presented with obstructive jaundice and invasive duodenal obstruction.
ERCP treatment for biliary drainage was attempted in all cases but failed due to a complete obstruction of the distal common bile duct (CBD) or papillary invasion by the tumor.
The concept of EUS-CD was discussed with patients’ family as an alternative treatment to avoid PTBD or surgery procedures. All participants were provided with written informed consent and this study was approved by the Institutional Review Board of our institution's committee.
Laboratory tests and clinical follow-up were performed after 7 and 30 days of the procedure, and monthly until patients’ death. The mean follow-up was 140 days (30 days to 17 months). Subsequently, all patients underwent palliative chemotherapy.
The EUS-CD procedure was performed by an experienced endoscopist under conscious sedation, using a combination of intravenous midazolam, fentanyl and propofol. Prophylactic antibiotic (ciprofloxacin 400mg I.V.) was used at the beginning of the procedure, routinely used in cases of obstructed biliary system.
The CBD was visualized in the duodenal bulb window using a linear echoendoscope (GFUCT160, Olympus, Tokyo, Japan) (Fig. 1A). Color Doppler Ultrasound was used to identify vascular anatomy on the traject. The dilated bile duct was punctured with a 19-gauge FNA needle (EUSN-19-T, Cook Endoscopy, Winston-Salem, NC, USA) (Fig. 1B). The puncture position was chosen based on EUS evaluation, at the CBD above the tumor, through the distal part of the duodenal bulb.
Figure 1.
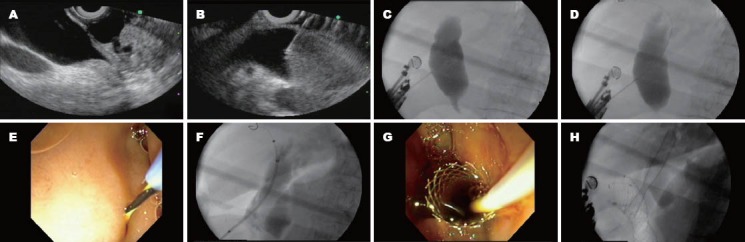
Sequence of images demonstrating the steps of the choledochoduodenostomy. The last image shows the final appearance of simultaneously biliary and duodenal metal stents.
For confirmation of biliary access, bile was aspirated and followed by iodine contrast injection under fluoroscopy view to demonstrate biliary opacification (Fig. 1C).
A 0.035-inch guidewire was introduced through the needle, under fluoroscopy view (Fig. 1D). It was attempted to pass the guidewire through the lesion, to reach the duodenum, as a Rendezvous maneuver, however in all cases without success.
After that, the needle was withdrawn and a wire-guided needle knife (KD-441Q, Olympus, Tokyo, Japan) was used to enlarge the site puncture in the duodenal wall (Fig. 1E), using the coagulation power to avoid bleeding. Then, a partially covered self-expandable metallic stent (Wallfex®, Boston Scientific) was passed over the guide (Fig. 1F, 1G), through the choledochoduodenal fistula, without any dilatation procedure.
Duodenal SEMS placement was performed during the same endoscopic procedure without the need to change EUS device for a frontal view endoscope and/or duodenoscope. Stricture evaluation was performed by injection of contrast above and immediately downstreamed it, to assess morphology, length, and degree of obstruction. Duodenal stricture was passed with a 5-6 French (Fr) ERCP catheter and a hydrophilic guidewire was inserted distally. When the guidewire was correctly positioned distally to the stricture, the stent catheter was advanced over the guidewire. At this time, the stent was released (Fig. 1H) and its correct position and performance were documented immediately after deployment by contrast injection.
RESULTS
The procedure was performed in seven patients, including five females and two males. The mean age was 66 years old, ranging between 34 and 86 years old. All cases were diagnosed by imaging studies as unresectable cancer. Six of them had pancreatic adenocarcinoma and one had papillary adenocarcinoma.
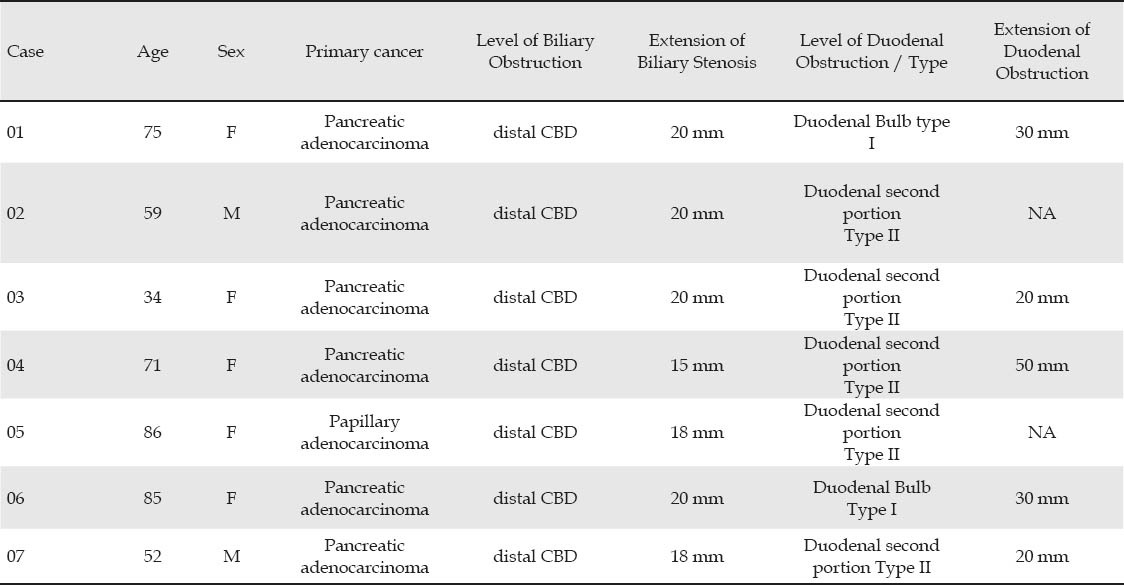
In all cases, the location of the biliary obstruction was in the distal CBD and the grade of proximal dilation diameter varied from 15 mm to 20 mm. Two patients had type I (28.6%) and five had type II (71.4%) duodenal obstruction (Tab. 1).
Table 1.
Description of cases age, gender, primary cancer and correlation between endoscopic findings of biliary and duodenal lesions
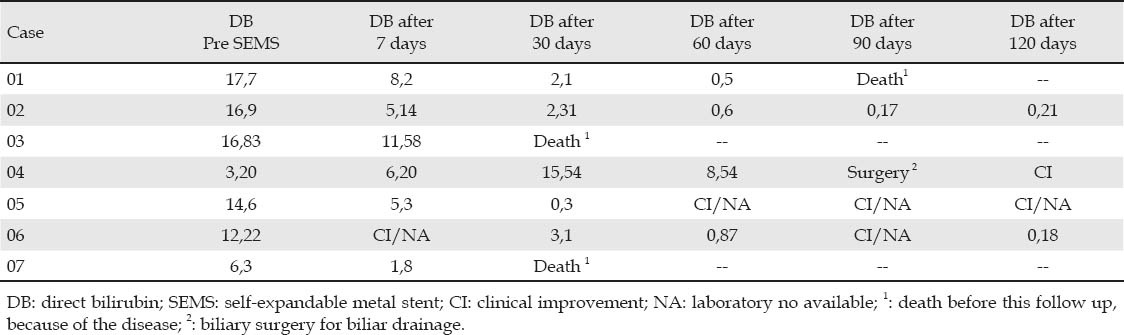
Technical success of EUS-CD, by the stent placement, occurred in 100% of the cases. There were no early complications (Tab. 2). Biliary drainage was effective clinically as well as in laboratory in 6 cases (6/7), by relieving obstructive jaundice and a decreasing bilirubin levels (Tab. 3).
Table 2.
Description of SEMS placement in biliary and duodenal obstruction correlated with additional technique features
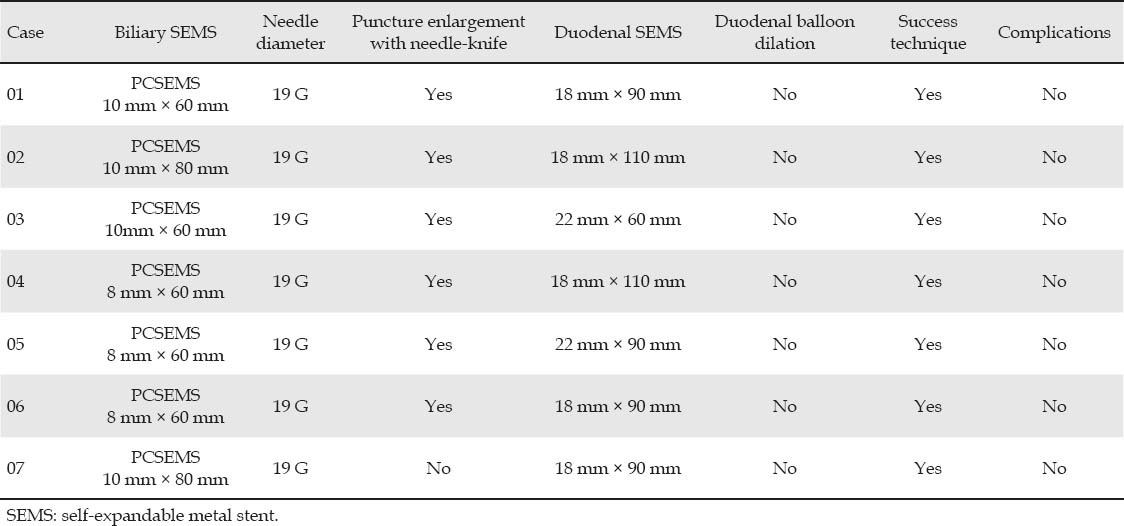
Table 3.
Direct bilirubin levels and clinical jaundice according to follow-up time period
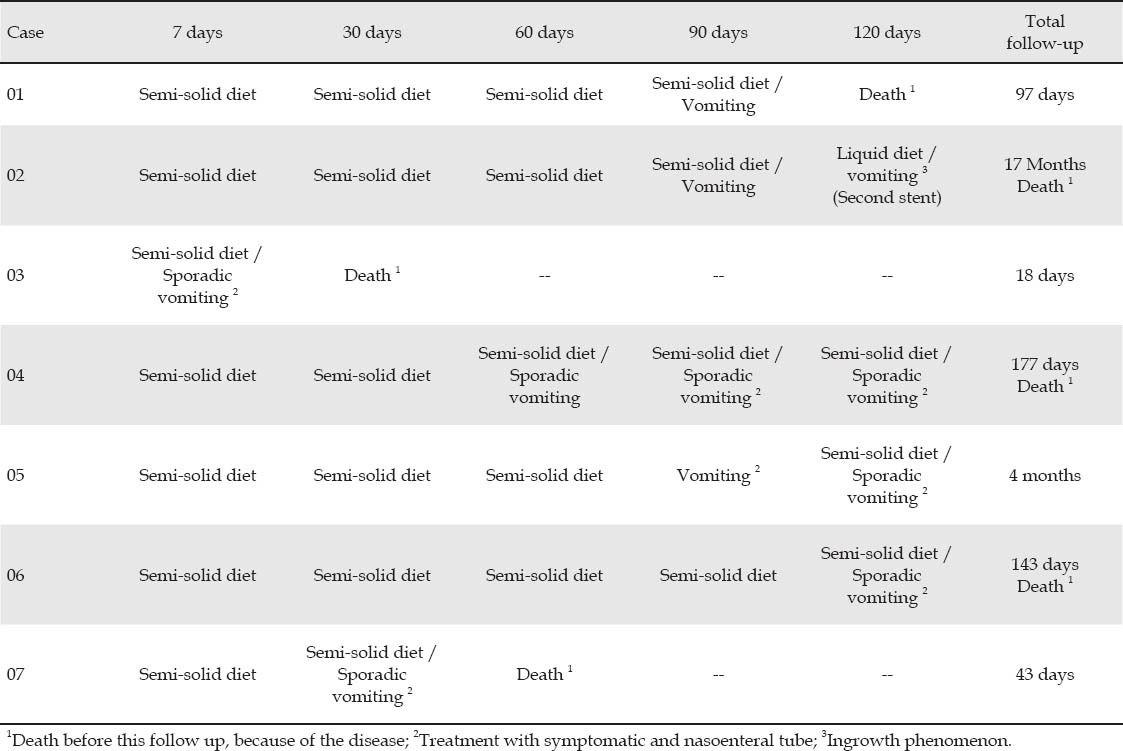
Duodenal SEMS placement was effective in 100% of the cases that remained alive after a follow up of 7 and 30 days. The major cause of failure over time was ingrowth phenomenon, requiring the placement of another duodenal SEMS over the previous one in one patient. Duodenal obstruction relief and follow-up period are represented in Table 4.
Table 4.
Symptoms, type of feeding and duodenal obstruction relief during follow up period
DISCUSSION
Patients with periampullary cancer, which includes lesions from papilla, head of the pancreas, distal CBD and duodenum or metastatic lesions are usually diagnosed in advanced stages, when curative surgical treatment is not feasible. The mean survival time of these patients ranges from 6 to 12 months. However, when concomitant duodenal obstruction occurs, their survival decreases.27
Simultaneous palliative treatment in cases of biliary and duodenal obstruction remains controversial in literature.
Surgical treatment with biliary-digestive bypass combined with gastro-jejunal anastomosis has high rates of morbidity (25%-37%) and mortality (2.5%).28,29,30 In addition, it also has an increased length of hospital stay and financial costs as compared to endoscopic treatment.28
PTBD is an alternative method for biliary drainage, even though it has a complication rate ranging from 10% to 30% and decreases the patients’ quality of life when internal drainage is not achieved and there is a necessity for an external catheter.31 In cases with concomitant duodenal obstruction, symptoms reliefs are obtained with stent placement through upper endoscopy.
Endoscopic treatments with placement of SEMS for biliary drainage during ERCP32 and duodenal SEMS, through upper endoscopy,33 have been used as less invasive methods. However, some studies describe difficulties in these techniques, such as failure in cannulation or access to the biliary tree through ERCP, and the location of duodenal obstruction for upper endoscopy.22,23,34,35
Recently, EUS-CD has become an alternative method after unsuccessful ERCP treatment.36,37,38,39,40 Park et al, in 2009,41 had 100% technical and clinical success in a study with 4 patients. In the same year, Hanada et al,20 obtained the same results without complications. Giovannini et al,42 in 2011, reported a series of 9 patients who underwent EUS-CD and achieved technical and therapeutic success rates of 88.9%, and complication was observed in only one patient.
Our results suggest therapeutic EUS as an alternative for these patients, with good clinical success, feasible technique and safety. It is a less invasive procedure to biliary drainage in patients whose ERCP treatment failed due to tumor invasion.
Mutignani et al,27 proposed a classification for the duodenal obstruction in relation to the papilla: Type I stenosis, involving duodenal bulb or first part of duodenum, without involvement of the papilla; Type II stenosis, affecting the second part of the duodenum, with involvement of the papilla; and Type III stenosis, involving the third part of the duodenum without involvement of the papilla. The procedure of dual stent placement is more difficult in type II cases due to technical difficulty in biliary access because of previous enteral stent or tumor local invasion.22,23,34,35 In our cases most patients had the type II stenosis and all patients reported improvement of obstructive symptoms and quality of life after the stent placement.
This case series presents seven cases of unresectable periampullary cancer with both biliary and duodenal obstruction. In these cases, the technique may be an alternative to double stenting in the same procedure and equipment.
However, further studies are needed to standardize this procedure technique and compare it with PTBD.
REFERENCES
- 1.Fogel EL, Sherman S, Devereaux BM, et al. Therapeutic biliary endoscopy. Endoscopy. 2001;33:31–8. doi: 10.1055/s-2001-11186. [DOI] [PubMed] [Google Scholar]
- 2.Ang TL, Teo EK, Fock KM. EUS-guided transduodenal biliary drainage in unresectable pancreatic cancer with obstructive jaundice. JOP. 2007;8:438–43. [PubMed] [Google Scholar]
- 3.Artifon EL, Chaves DM, Ishioka S, et al. Echoguided hepatico-gastrostomy: a case report. Clinics (Sao Paulo) 2007;62:799–802. doi: 10.1590/s1807-59322007000600023. [DOI] [PubMed] [Google Scholar]
- 4.Burmester E, Niehaus J, Leineweber T, et al. EUS-cholangio-drainage of the bile duct: report of 4 cases. Gastrointest Endosc. 2003;57:246–51. doi: 10.1067/mge.2003.85. [DOI] [PubMed] [Google Scholar]
- 5.Kahaleh M, Hernandez AJ, Tokar J, et al. Interventional EUS-guided cholangiography: evaluation of a technique in evolution. Gastrointest Endosc. 2006;64:52–9. doi: 10.1016/j.gie.2006.01.063. [DOI] [PubMed] [Google Scholar]
- 6.Ponchon T, Pilleul F. Diagnostic ERCP. Endoscopy. 2002;34:29–42. doi: 10.1055/s-2002-19397. [DOI] [PubMed] [Google Scholar]
- 7.Cortas GA, Mehta SN, Abraham NS, et al. Selective cannulation of the common bile duct: a prospective randomized trial comparing standard catheters with sphincterotomes. Gastrointest Endosc. 1999;50:775–9. doi: 10.1016/s0016-5107(99)70157-4. [DOI] [PubMed] [Google Scholar]
- 8.Schöfl R. Diagnostic endoscopic retrograde cholangiopancreatography. Endoscopy. 2001;33:147–57. doi: 10.1055/s-2001-11667. [DOI] [PubMed] [Google Scholar]
- 9.Martin DF. Combined percutaneous and endoscopic procedure for bile duct obstruction. Gut. 1994;35:1011–12. doi: 10.1136/gut.35.8.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yee AC, Ho CS. Complications of percutaneous biliary drainage: benign vs malignant diseases. AJR Am J Roentgenol. 1987;148:1207–9. doi: 10.2214/ajr.148.6.1207. [DOI] [PubMed] [Google Scholar]
- 11.Ferrucci JT, Mueller PR, Harbin WP. Percutaneous transhepatic biliary drainage: technique, results, and applications. Radiology. 1980;135:1–13. doi: 10.1148/radiology.135.1.7360943. [DOI] [PubMed] [Google Scholar]
- 12.Irisawa A, Hikichi T, Shibukawa G, et al. Pancreatobiliary drainage using the EUS-FNA technique: EUS-BD and EUS-PD. J Hepatobiliary Pancreat Surg. 2009;16:598–604. doi: 10.1007/s00534-009-0131-5. [DOI] [PubMed] [Google Scholar]
- 13.Wiersema MJ, Sandusky D, Carr R, et al. Endosonography-guided cholangiopancreatography. Gastrointest Endosc. 1996;43(2 Pt 1):102–6. doi: 10.1016/s0016-5107(06)80108-2. [DOI] [PubMed] [Google Scholar]
- 14.Giovannini M, Moutardier V, Pesenti C, et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy. 2001;33:898–900. doi: 10.1055/s-2001-17324. [DOI] [PubMed] [Google Scholar]
- 15.Kahaleh M, Wang P, Shami VM, et al. EUS guided transhepatic cholangiography: report of 6 cases. Gastrointest Endosc. 2005;61:307–13. doi: 10.1016/s0016-5107(04)02585-4. [DOI] [PubMed] [Google Scholar]
- 16.Puspok A, Lomoschitz F, Dejaco C, et al. Endoscopic ultrasound guided therapy of benign and malignant biliary obstruction: a case series. Am J Gastroenterol. 2005;100:1743–47. doi: 10.1111/j.1572-0241.2005.41806.x. [DOI] [PubMed] [Google Scholar]
- 17.Fujita N, Noda Y, Kobayashi G, et al. Histological changes at an endosonography-guided biliary drainage site: a case report. World J Gastroenterol. 2007;13:5512–5. doi: 10.3748/wjg.v13.i41.5512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tarantino I, Barresi L, Repici A, et al. EUS-guided biliary drainage: a case series. Endoscopy. 2008;40:336–9. doi: 10.1055/s-2007-995455. [DOI] [PubMed] [Google Scholar]
- 19.Itoi T, Sofuni A, Itokawa F, et al. Endoscopic ultrasonography-guided biliary drainage. J Hepatobil Pancreat Sci. 2010;17:611–6. doi: 10.1007/s00534-009-0196-1. [DOI] [PubMed] [Google Scholar]
- 20.Hanada K, Iiboshi T, Ishii Y. Endoscopic ultrasound-guided choledochoduodenostomy for palliative biliary drainage in cases with inoperable pancreas head carcinoma. Dig Endosc. 2009;21(Suppl 1):75–8. doi: 10.1111/j.1443-1661.2009.00855.x. [DOI] [PubMed] [Google Scholar]
- 21.Hara K, Yamao K, Mizuno N, Sawaki A, Takagi T, Bhatia V. Endoscopic ultrasound-guided choledochoduodenostomy. Dig Endosc. 2010;22:147–50. doi: 10.1111/j.1443-1661.2010.00944.x. [DOI] [PubMed] [Google Scholar]
- 22.Maetani I, Nambu T, Omuta S, et al. Treating bilio-duodenal obstruction: Combining new endoscopic technique with 6Fr stent introducer. World J Gastroenterol. 2010;16:2828–2831. doi: 10.3748/wjg.v16.i22.2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moon JH, Choi HJ. Endoscopic double-metallic stenting for malignant biliary and duodenal obstructions. J Hepatobil Pancreat Sci. 2011;18:658–663. doi: 10.1007/s00534-011-0409-2. [DOI] [PubMed] [Google Scholar]
- 24.Adler DG, Baron TH. Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol. 2002;97:72–8. doi: 10.1111/j.1572-0241.2002.05423.x. [DOI] [PubMed] [Google Scholar]
- 25.Laasch HU, Martin DF, Maetani I. Enteral stents in the gastric outlet and duodenum. Endoscopy. 2005;37:74–81. doi: 10.1055/s-2004-826103. [DOI] [PubMed] [Google Scholar]
- 26.Baron TH, Harewood GC. Enteral self-expandable stents. Gastrointest Endosc. 2003;58:421–33. doi: 10.1067/s0016-5107(03)00023-3. [DOI] [PubMed] [Google Scholar]
- 27.Mutignani M, Tringali A, Shah SG, et al. Combined endoscopic stent insertion in malignant biliary and duodenal obstruction. Endoscopy. 2007;39:440–7. doi: 10.1055/s-2007-966327. [DOI] [PubMed] [Google Scholar]
- 28.Wong YT, Brams DM, Munson L, et al. Gastric outlet obstruction secondary to pancreatic cancer: surgical vs endoscopic palliation. Surg Endosc. 2002;16:310–2. doi: 10.1007/s00464-001-9061-2. [DOI] [PubMed] [Google Scholar]
- 29.Lillemoe KD, Cameron JL, Hardacre JM, et al. Is prophylactic gastrojejunostomy indicated for unresectable periampullary cancer? A prospective redomized trial. Ann Surg. 1999;230:322–8. doi: 10.1097/00000658-199909000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van Wagensveld BA, Coene PP, van Gulik TM, et al. Outcome of palliative biliary and gastric bypass surgery for pancreatic head carcinoma in 126 patients. Br J Surg. 84:1402–6. [PubMed] [Google Scholar]
- 31.Pessa ME, Hawkins IF, Vogel SB. The treatment of acute cholangitis. Percutaneous transhepatic biliary drainage before definitive therapy. Ann Surg. 1987;205:389–92. doi: 10.1097/00000658-198704000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moss AC, Morris E, Leyden J, et al. Do the benefits of metal stents justify the costs? A systematic review and meta-analysis of trials comparing endoscopic stents for malignant biliary obstruction. Eur J Gastroenterol Hepatol. 2007;19:1119–24. doi: 10.1097/MEG.0b013e3282f16206. [DOI] [PubMed] [Google Scholar]
- 33.Jeurnink SM, Steyerberg EW, van Hooft JE, et al. Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointest Endosc. 2010;71:490–9. doi: 10.1016/j.gie.2009.09.042. [DOI] [PubMed] [Google Scholar]
- 34.Iwamuro M, Kawamoto H, Harada R, et al. Combined duodenal stent placement and endoscopic ultrasonography-guided biliary drainage for malignant duodenal obstruction with biliary stricture. Digest Endosc. 2010;22:236–40. doi: 10.1111/j.1443-1661.2010.00997.x. [DOI] [PubMed] [Google Scholar]
- 35.Baron TH. Management of simultaneous biliary and duodenal obstruction: The endoscopic perspective. Gut and Liver. 2010;4:S50–6. doi: 10.5009/gnl.2010.4.S1.S50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tarantino I, Barresi L, Fabbri C, et al. Endoscopic ultrasound guided biliary drainage. World J Gastrointest Endosc. 2012;4:306–311. doi: 10.4253/wjge.v4.i7.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Voegeli DR, Crummy AB, Wesse JL. Percutaneous transhepatic cholangiography, drainage, and biopsy in patients with malignant biliary obstruction. An alternative to surgery. Am J Surg. 1985;150:243–7. doi: 10.1016/0002-9610(85)90129-1. [DOI] [PubMed] [Google Scholar]
- 38.Oh HC, Lee SK, Lee TY, et al. Analysis of percutaneous transhepatic cholangioscopy-related complications and the risk factors for those complications. Endoscopy. 2007;39:731–6. doi: 10.1055/s-2007-966577. [DOI] [PubMed] [Google Scholar]
- 39.Maranki J, Hernandez AJ, Arslan B, et al. Interventional endoscopic ultrasound-guided cholangiography: long-term experience of an emerging alternative to percutaneous transhepatic cholangiography. Endoscopy. 2009;41:532–8. doi: 10.1055/s-0029-1214712. [DOI] [PubMed] [Google Scholar]
- 40.Yamao K, Sawaki A, Takashi K, et al. EUS-guided choledochoduodenostomy for palliative biliary drainage in cae of papillary obstruction: report of 2 cases. Gastrointest Endosc. 2006;4:663–7. doi: 10.1016/j.gie.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 41.Park do H, Koo JE, Oh J, et al. EUS-guided biliary drainage with one-step placement of a fully covered metal stent for malignant biliary obstruction: a prospective feasibility study. Am J Gastroenterol. 2009;104:2168–74. doi: 10.1038/ajg.2009.254. [DOI] [PubMed] [Google Scholar]
- 42.Luna Mar, Ávila TFI, Giovannini M, et al. Endoscopic ultrasound-guided biliodigestive drainage is a good alternative in patients with unresectable cancer. Endoscopy. 2011;43:826–30. doi: 10.1055/s-0030-1256406. [DOI] [PubMed] [Google Scholar]


