Confocal laser endomicroscopy (CLE) is a newly developed endoscopic technique that enables imaging of the mucosal layer during endoscopy at a subcellular level of resolution. The method can therefore be used for the assessment of changes in vascular architecture, connective tissue, and cellular components in the mucosa; enabling endoscopists to collect real-time in vivo histological images or “virtual biopsies” of the gastrointestinal (GI) mucosa during endoscopy.
Confocal microscopy (CM) consists of focusing a laser beam (such as an argon-ion laser that generates an excitation wavelength of 488 nm; blue laser light) onto the plane of interest, filtering the returned light by means of a small pinhole which rejects out-of-focus light. The illumination and detection systems are in the same focal plane and are termed “confocal”.
After passing through the pinhole, the fluorescent light is detected by a photo-detection device (a photomultiplier tube or avalanche photodiode), converting the light signal into an electrical one that is recorded by a computer. All detected signals from the illuminated spot are captured and measured; As the laser scans over the plane of interest, a whole image is obtained pixel-by-pixel and line-by-line; whereas the brightness of a resulting image pixel corresponds to the relative intensity of detected fluorescent light. The gray-scale image created is an optical section representing one focal plane within the examined specimen.
Because confocal images depend on fluorescence, a fluorescent dye (contrast agent) is required to make objects visible. The contrast agents can be applied systemically (fluorescein, tetracycline) or topically (acriflavine, cresyl violet) by using a spraying catheter. Of these, intravenous fluorescein sodium (10%) and topically applied acriflavine (0.2%) are the most commonly used in humans.
CLE can be performed currently with 2 devices: integrated into an endoscope (Pentax, Tokyo, Japan, herein termed eCLE) and as a stand-alone probe (herein termed pCLE) capable of passage through the accessory channel of most endoscopes (Cellvizio, Mauna Kea Technologies, Paris, France).
Fluorescein-based CLE is becoming an increasingly important tool in both research and clinical settings for gastrointestinal diseases. Recently, new high resolution probe-based CLE (pCLE) has been developed by Mauna Kea Technologies (MKT). These probes have further expanded the potential of CLE use in gastroenterology since they can be passed through the accessory channel of any endoscope and used as needed in any endoscopy case; including passage into the bile and pancreatic ducts. Clinical studies with pCLE technology have shown promise in Barrett's esophagus, biliary cancer and colonic polyps.
The introduction of endoscopic ultrasound (EUS) represented a major advance in the diagnosis and staging of gastrointestinal malignancies; In addition to providing imaging of tumors and enhancing TMN staging, EUS also provides guidance for fine needle aspiration (FNA) and biopsies of undiagnosed masses and lymph nodes (LN) suspicious for malignant invasion, providing further diagnostic and staging information. However, FNA is technically demanding and multiple punctures of LN or masses are sometimes required to obtain sufficient tissue for histological assessment. For further consideration is the fact that pancreatic masses have a wide differential diagnosis that includes benign and malignant etiologies; FNA of the pancreas is associated with accuracies around 85% to 90% but negative predictive values of 35% to 40%. Hence, the ability of EUS-CM is to more accurately evaluate masses and lymph nodes prior to their puncture, in an effort to have an optical biopsy, and in the future a “minute” diagnosis of malignancy. To perform EUS-CM, we use the new AQ-Flex™ 19 which provides real-time microscopic imaging of pancreatic cysts during EUS-FNA procedures. It helps you see the cyst wall down to a cellular level and recognize typical features of each type of the cyst, and it is compatible with 19-G endoscopic needles. AQ-Flex™ 19 can also be used during endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA).
The first study on pig model confirmed the feasibility of the technique. Ten pigs were examined under general anesthesia, either EUS-guided organ puncture or natural-orifice transluminal endoscopic surgery (NOTES) procedure was used. The confocal miniprobe was inserted through the 22-G needle, and puncture of various intra-abdominal structures and organs was performed (lymph nodes, diaphragm, ovaries, liver, spleen, and pancreas) after the intravenous injection of fluorescein (5-10 mL 1% or 2 mL 10% solution). Real-time sequences were recorded. Biopsy specimens were taken for standard histopathology. It was technically feasible to introduce the needle-based confocal miniprobe into various organs at the time of EUS or NOTES procedures. The device enabled real-time in vivo collection of images at histological resolutions and of acceptable image quality from several intra-abdominal organs interrogated. The authors concluded that first time in main body in the pancreas was technically feasible via a 19-G needle under endosonographic guidance.
Konda et al.1 have published recently their data on 18 patients presenting for EUS-FNA. Patients were injected with 2.5 mL of 10% fluorescein. The lesion was interrogated with the nCLE probe positioned at the tip of a 19-G FNA needle. Cases included 16 cysts and 2 masses. There were no device malfunctions. Technical challenges were encountered in 6 of 18 attempts to image, including a postloading technique, the longer ferule tip, and a transduodenal approach. Performing imaging with nCLE during a pancreatic EUS-FNA procedure was technically feasible in 17 of 18 cases. Good to very good image quality was achieved in 10 cases. More recently, we have reported in this journal our first experience in 11 patients.2 Eleven patients underwent EUS for the staging of a pancreatic mass (3 cystic and 4 solid) or for the diagnosis of celiac and/or mediastinal LN (n = 4). Benign intraductal papillary mucinous neoplasm (IPMN) was characterized by the aspect of finger like projections which correspond to the villous changes of intestinal IPMN type (Fig. 1). In pancreatic adenocarcinomas, EUS-CM showed vascular leakage of fluorescein from irregular vessels into the tumor; large dark clumps which correspond to humps of malignant cells. Inflammatory LN were characterized by the presence of diffuse small cells into a homogeneous stroma with a normal vascularization. On the opposite, EUS-CM showed malignant LN glandular structures with dark cells; large dark clumps and an important neo-vascularization with huge leakage of fluorescein.
Figure 1.
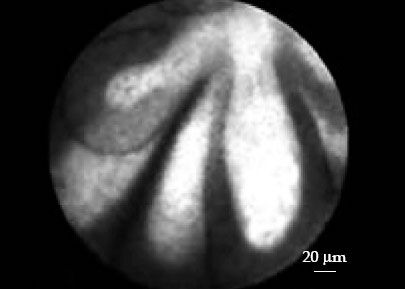
Endomicroscopic image of an intraductal papillary mucinous neoplasm (IPMN) in the pancreas, with Cellvizio® needle-based confocal laser endomicroscopy (nCLE).
During the last DDW, Dr. Nakai Y, et al. presented the results of the “Diagnosis of Pancreatic Cysts: Endoscopic Ultrasound, Through-the-Needle CLE and Cystoscopy Trial (DETECT)”,3 at the American Society of Gastrointestinal Endoscopy (ASGE) Topic Forum. The investigators identified key features seen in Cellvizio® images that were taken from inside pancreatic cysts in 21 patients. Then they correlated the presence of structures to clinical results and concluded that Cellvizio® nCLE during EUS-FNA procedures of the pancreas improved the sensitivity for the diagnosis of malignant cysts. Separately, Konda VJ, et al. presented similar results from a 65-patient, multi-center study known as INSPECT4 during the Ame rican Gastroenterological Association (AGA) poster session. The investigators were able to identify 100% of the pancreatic cystic neoplasms in these patients.
EUS-CM is feasible during EUS examination; these preliminary results are very encouraging. An international multicenter study focused on cystic and solid pancreatic lesions and LN (CONTACT study) is ongoing.
REFERENCES
- 1.Konda VJ, Aslanian HR, Wallace MB, et al. Gastrointest Endosc. 2011;74:1049–60. doi: 10.1016/j.gie.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 2.Giovannini M, Caillol F, Poizat F, et al. Feasibility of Intratumoral Confocal Microscopy under Endoscopic Ultrasound Guidance. Endosc Ultrasound. 2012;1:80–3. doi: 10.7178/eus.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakai Y, Iwashita T, Park DH, et al. Diagnosis of Pancreatic Cysts: Endoscopic Ultrasound, Through-the-Needle Confocal Laser-Induced Endomicroscopy and Cystoscopy Trial (Detect Study) Gastrointest Endosc. 2012;75(Suppl):AB145–AB146. doi: 10.1016/j.gie.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 4.Konda VJ, Meining A, Jami LH, et al. An International, Multi-Center Trial on Needle-Based Confocal Laser Endomicroscopy (nCLE): Results From the In Vivo CLE Study in the Pancreas With Endosonography of Cystic Tumors (INSPECT) Gastroenterology. 2012;142(Suppl):S–620. [Google Scholar]


