Abstract
Linear Endosonography has been used to image the Portal Venous System but no established standard guidelines exist. This article presents techniques to visualize the portal venous system and its tributaries by linear endosonography. Attempt has been made to show most of the first order tributaries and some second order tributaries of splenic vein, superior mesenteric vein and portal vein.
Keywords: linear endosonography, portal venous system, portal vein, splenic vein, superior mesenteric vein
INTRODUCTION
Endoscopic ultrasonography (EUS) provides a unique opportunity to evaluate the portal venous system and its tributaries.1 This evaluation may be helpful in portal hypertension, portal venous thrombosis, staging of pancreatic malignancies and for therapeutic intervention by endosonography.2,3,4,5 The portal venous system is generally not accessible by standard angiographic methods.6 If an abnormality is found in portal venous system, endosonography-guided access can provide alternative to percutaneous methods for diagnostic and therapeutic interventions.5 There have been animal studies, few small case series and reports that describe the role of endosonography in intervention by endotherapy of portal venous system.6,7,8,9,10,11,12,13,14,15
The portal venous system has a very variable anatomy and sometimes the best of interventionists have been shown to misinterpret the variations. The key to avoid the fallacy is to understand the anatomical relations of the veins, with organs. The imaging techniques for visualization of portal venous system have evolved over the years to include several abdominal stations and use of ultrasonographic techniques such as color and power Doppler. Application of color and power Doppler while scanning has led to visualization of smaller tributaries, which were not visible before by standard ultrasonographic and endosonographic methods. This article describes standard imaging technique in the assessment of the portal venous system and its tributaries using linear endoscopic ultrasound.
NORMAL ANATOMY
The anatomy of the portal venous system described in the literature has been based on cadaveric and radiographic analysis (Fig. 1).16,17,18,19,20,21,22
Figure 1.
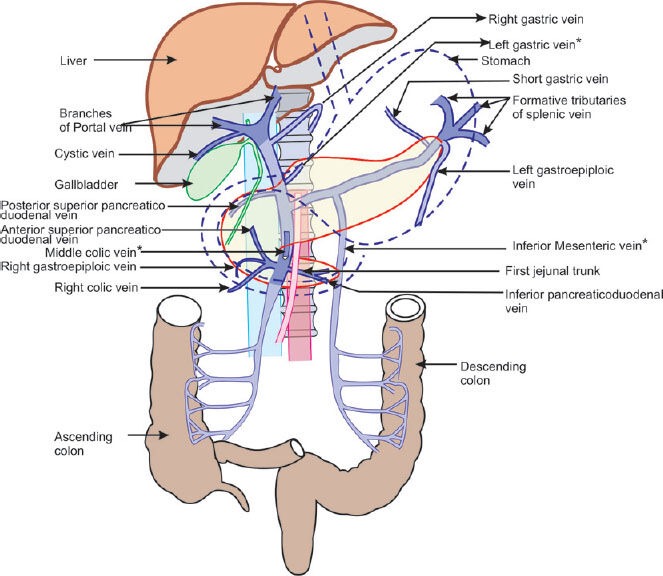
Portal venous system consists of three major veins (portal vein, splenic vein, superior mesenteric vein) and their tributaries. The diagram also shows some important relation of the veins with abdominal organs. *marks veins, which have a variable place of joining in portal venous system.
Portal Vein
The portal vein is radiologically up to 12.6 ± 1.7 mm in diameter and about 8 cm long and is formed at the portal vein confluence behind the neck of pancreas by the right angled junction of superior mesenteric vein and splenic vein at the level of L2 vertebra. It takes an oblique course towards the right shoulder at a 20 to 80 degree angle to the spine.6 It is a thin-walled, valve less vascular structure that courses along the pancreatic neck and bile duct, and enters the liver at the porta hepatis. As it enters the liver, the portal vein bifurcates into 2 trunks and eventually into several branches. The main trunk tributaries here are posterior superior pancreaticoduodenal vein, left and right gastric veins.16,18,20,21
Splenic Vein
The splenic vein is a large horizontal vein that begins in the hilum of the spleen by confluence of about half a dozen tributaries with left gastroepiploic vein. It passes to the right with a little slope downwards in contact with the posterior surface of the pancreas, first behind the tail and then behind the body of pancreas to end behind the neck of pancreas by joining the superior mesenteric vein at the level of L2 vertebra. The posterior relations are hilum of left kidney, left adrenal gland, left crus of diaphragm, superior mesenteric artery and aorta. Splenic vein has tributaries merging on the anterior surface or the superior and inferior borders. The main trunk tributaries here are left gastroepiploic vein, inferior mesenteric vein, posterior gastric veins, short gastric veins, and pancreatic veins.16,17 (Fig. 2A)
Figure 2.
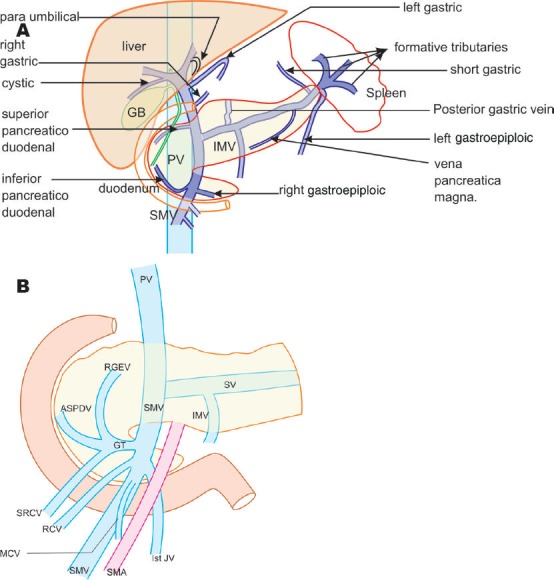
A: The course, relations and tributaries of splenic vein are shown in this diagram. Whereas anteriorly the splenic vein is related to the pancreatic neck, body and tail. Posterior relations of splenic vein are left renal hilum and vessels, left adrenal gland, left crus of diaphragm and superior mesenteric artery. B: The superior mesenteric vein has got two important tributaries which join the superior mesenteric vein 1-5 cm below the union of superior mesenteric vein with splenic vein. The gastrocolic trunk joins the lateral aspect whereas the first jejunal vein joins the medial aspect. Gastrocolic trunk has three small tributaries which are right gastroepiploic vein, anterior superior pancreaticoduodenal vein and superior right colic vein. The right colic vein and middle colic vein have got a variable joining into superior mesenteric venous system.
Superior Mesenteric Vein
The union of right colic and ileocloic veins forms superior mesenteric vein with tributaries from the ileum. Several smaller jejunal and ileal veins join the left border of superior mesenteric vein. As it ascends upwards the superior mesenteric vein crosses the uncinate process and the third part of the duodenum while lying on the right side of superior mesenteric artery. As it crosses the uncinate process two major tributaries of superior mesenteric vein, gastrocolic trunk and first jejunal trunk join it. Gastrocolic trunk joins the right side and the first jejunal vein joins the left side of the superior mesenteric vein. Occasionally the middle colic vein joins the trunk of superior mesenteric vein on the anterior aspect just before it joins the splenic vein posterior to the neck of pancreas as the third tributary (Fig. 2B).21
Inferior Mesenteric Vein
Inferior mesenteric vein originates anterior to the sacrum as the superior rectal (hemorrhoidal) vein and receives branches from the sigmoid and descending colon as it ascends to the left of midline, adjacent to the inferior mesenteric artery and left gonadal vein.22 Inferior mesenteric vein is a vein with variable drainage into portal venous system. When inferior mesenteric vein joins the splenic vein, it passes behind the lower border of the body of the pancreas, in front of the left renal vein. When it drains into the superior mesenteric vein or the portal venous confluence, it curves sharply to the right and passes below and parallel to the splenic vein behind the pancreas in front of the superior mesenteric artery (Fig. 3A-D)23,24. This information can be useful during resection of borderline pancreatic malignancies.24
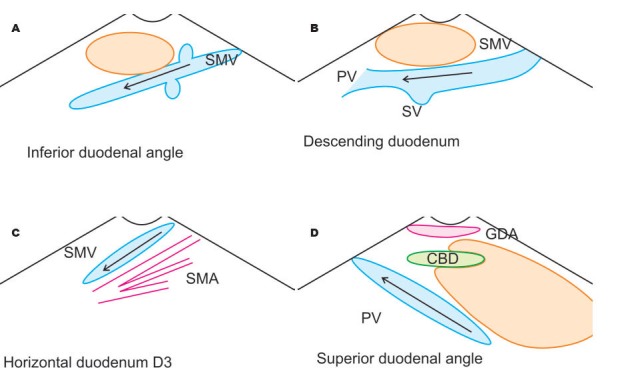
Figure 3.
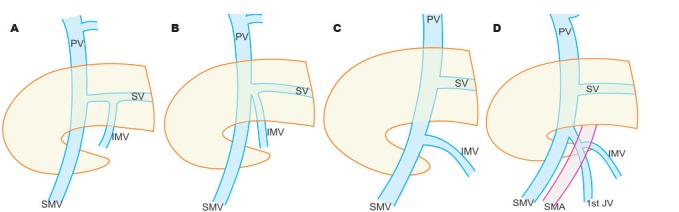
Inferior mesenteric vein has got a variable joining in portal venous system. A: Inferior mesenteric vein join the splenic vein in 38%; B: Splenoportal junction in 32.7%; C: Superior mesenteric vein in 29.3%; D: Occasionally inferior mesenteric vein can join the first jejunal vein.
Left and Right Gastric Veins
The left gastric vein (coronary vein) drains the stomach and lower 1/3 of esophagus and is a vein with variable drainage into portal venous system. When it passes anterior to the hepatic artery, it accompanies the left gastric artery in the hepatogastric ligament and passes down to join the portal vein (30%) at the upper border of pancreas near the upper part of duodenal bulb. When it passes posterior to the hepatic artery it joins near the right of the portal venous confluence (33%) or the splenic vein (37%) (Fig. 4A-D)25. The right gastric vein is a small vein that runs along the lesser curvature to drain into the portal vein behind the first part of duodenum.17,26
Figure 4.
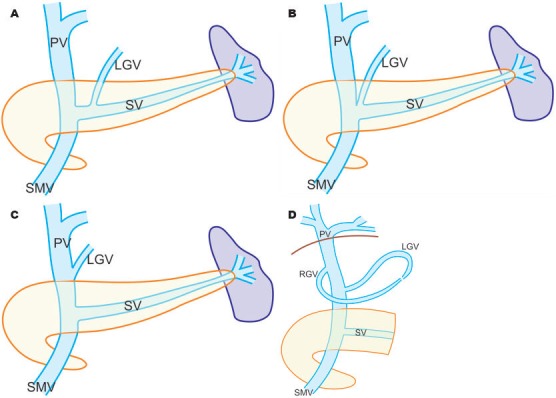
Left gastric vein has got a variable joining in portal venous system. A: Left gastric vein ends in the splenic vein in 37%; B: Splenoportal junction in 33%; C: 30% in portal vein; D: The left gastric vein can join the right gastric vein with joins the portal vein a little higher up.
Left and Right Gastroepiploic Veins
The left gastroepiploic vein drains both the posterior and anterior gastric surfaces and runs along the greater curvature superolaterally to drain into the splenic vein within the gastrosplenic ligament. During its course it runs anterior to the hilum of the left kidney.27,28 The right gastroepiploic vein, a tributary of gastrocolic trunk proceeds along the greater curvature of the stomach between the layers of the gastrocolic ligament and enters the right edge of transverse mesocolon. It joins the right and sometimes the middle colic veins running in the transverse mesocolon to form the gastrocolic trunk.27,28
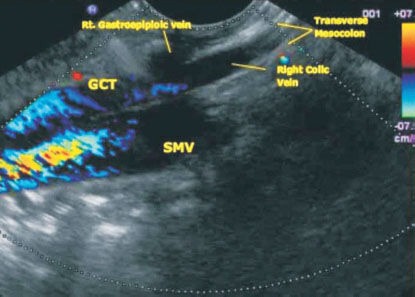
Gastrocolic and First Jejunal Trunk
Anterior superior pancreaticoduodenal v ein, right gastroepiploic vein, right superior colic vein (drain hepatic flexure) and the right colic vein (drain ascending colon) form gastrocolic trunk. The gastrocolic trunk runs transversely in front of the inferior portion of the head of the pancreas to drain into the right anterolateral aspect of superior mesenteric vein within 1-5 cm below its confluence with the splenic vein. In some instances, the middle colic vein also joins to form the gastrocolic trunk. (Fig. 5A-G)29,30
Figure 5.
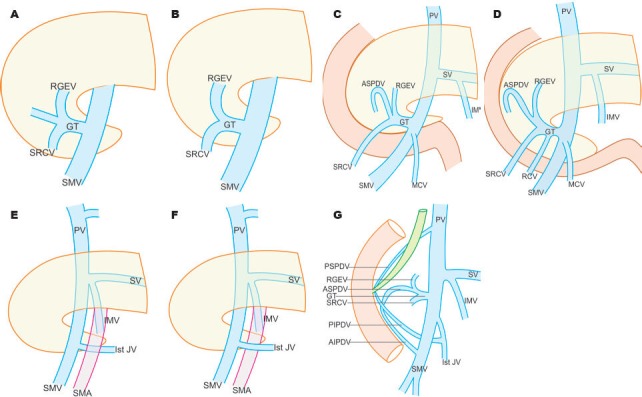
The gastrocolic trunk has a variable formation. A: Tripodal; B: Bipodal; C: Tripodal with variation; D: Quadripodal; E: The first jejunal vein generally goes behind superior mesenteric artery to join superior mesenteric vein; F: Sometimes the first jejunal vein generally goes in front of behind superior mesenteric artery to join superior mesenteric vein; G: The posterior, superior pancreatico duodenal vein opens up in the portal vein.
First jejunal vein joins the left lateral aspect of the superior mesentric vein at the level of gastrocolic trunk. First jejunal vein is identified as the only vein coursing posterior to the superior mesenteric artery before its termination into superior mesenteric vein. In a smaller percentage the first jejunal vein can traverse anterior to the superior mesenteric artery (Fig. 5E, F)31,32,33
Pancreatic Venous Drainage
The head of pancreas is drained by an anastomosis between anterior superior pancreaticoduodenal vein, anterior inferior pancreaticoduodenal vein, posterior superior pancreaticoduodenal vein and posterior inferior pancreaticoduodenal vein (Fig. 5G). Anterior inferior pancreaticoduodenal vein and postero-inferior pancreaticoduodenal vein join to form the inferior pancreaticoduodenal vein, which merges in the first jejunal vein. Anterior superior pancreaticoduodenal vein passes between the inferior surface of the pancreatic head and the third portion of the duodenum to drain into gastrocolic trunk.31,32,33 Posterior superior pancreaticoduodenal vein is formed medial to the mid point of descending duodenum, runs supero-medially on the posterior surface of head of pancreas, posterior to common bile duct and drains into portal vein behind the neck of pancreas at around the upper border of pancreas.34,35 The body of the pancreas is drained by numerous short pancreatic tributaries, which join the anterior surface of splenic vein. Sometimes the veins coalesce to form the pancreatica vena magna, which may join with the splenic vein near the confluence.35,36
Other Gastric Venous Tributaries
Posterior gastric veins are one or multiple small vessels draining the posterior surface of stomach into splenic vein. Short gastric veins drain the fundus of the stomach and drains into the splenic vein.
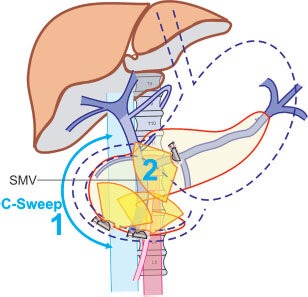
An experienced operator may be able to determine the vessel by gray scale imaging alone. The use of color Doppler however helps in separating out smaller tributaries which are related to the surface of portal venous system. Slow movement along the border of portal vein can sometimes be more helpful in tracing the origin of a vein from near the border of portal venous system. The evaluation of major vessels can be done at the designated stations (Fig. 6, Tab. 1, 2). Initially gray scale optimization of vessel of interest should be done. The setting of gray scale optimization should be set to as low as possible. This leaves enough pixels available for color flow analysis. A single focal zone is set to the range of target vessel. A color Doppler box is applied on the vessel and color gain is adjusted by first setting it high enough to produce color bleed and then gradually lowering the gain until the spurious signals disappear but the lumen still remains completely filled with color. After optimal adjustment of color gain, the size of the color box is optimally adjusted (decreased) to save the computer memory and keep the frame rate as high as possible. The venous nature of the vessel is confirmed by pulse Doppler. Continuous color application can be done while doing slow movement. If movement of the probe happens at a faster pace or interference occurs due to respiratory artifacts 3 to 4 sweeps can be taken to obtain the information. Studying their course, location and relation to major organs in the abdomen identifies most of the tributaries. Four types of movements are used to trace the vessel. Slow clockwise or anticlockwise movement is the most common movement to trace the course of a vessel seen in a transverse axis. Pushing the whole scope in or out is the most common movement to trace a vessel seen in a longitudinal axis. Up and down or right and left movements were mainly used after inflating the balloon and wedging it in the duodenal bulb. The choice of movement is however dependent on the operator and sometimes a combination of all movements is required to obtain proper imaging of tributaries.
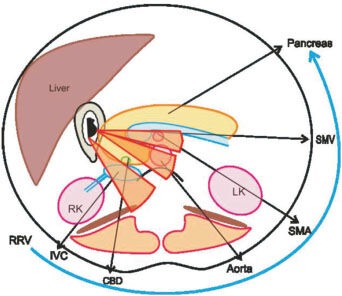
Figure 6.
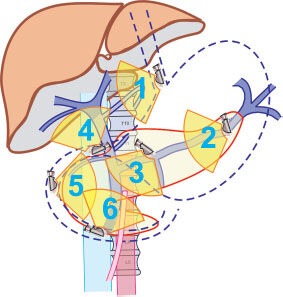
The stations of linear endosonography of the abdomen are demonstrated in the diagram with their respective scope positions. 1: Gastroesophageal junction portal vein is seen; 2: Body of stomach- Splenic vein and its tributaries are seen; 3: Antrum of the stomach- Portal vein is traced from butterfly shaped portal venous confluence to the hilum of liver; 4: Duodenal bulb- On CW and CCW the entire course of portal vein can be traced; 5: Descending duodenum- Superior mesenteric vein can’t be seen in a longitudinal axis; 6: Horizontal duodenum- Pulling back from the distal part of duodenum will reveal the tributaries of the superior mesenteric vein like gastrocolic and first jejunal trunk.
Table 1.
EUS of Portal Venous System: Linear EUS Points of Examination
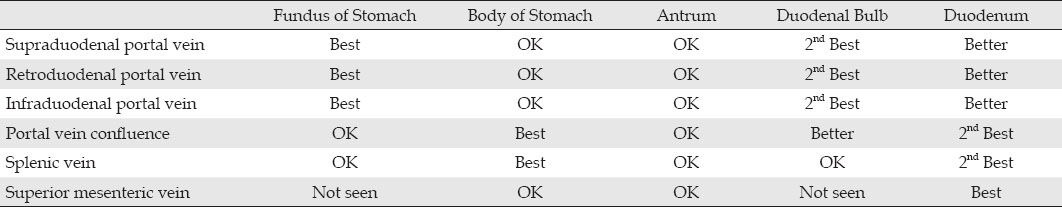
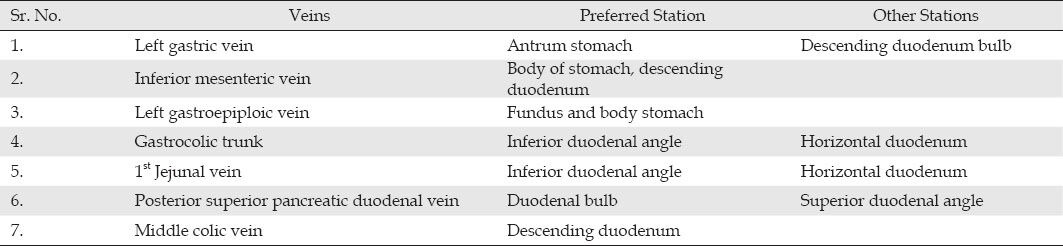
Table 2.
Linear EUS Point of Examination of Tributaries
ENDOSONOGRAPHIC TECHNIQUE
Portal Vein
Portal vein can be evaluated from fundus of stomach, antrum of stomach, duodenal bulb and descending duodenum (Fig. 6).37,38,39,40,41,42,43
Fundus of stomach
The scope is advanced just beyond the oesophagogastric junction and the left lobe of liver is located without angulations. Rotating anticlockwise from the fundus of the stomach brings the intrahepatic portion of inferior vena cava into view.38 Once the inferior vena cava (IVC) is located clockwise rotation of the scope traces the intrahepatic portion of IVC from a 9 o'clock cranial position to 2 o'clock caudal position. In the same position the anticlockwise rotation of the scope moves the portal vein from a 2 o'clock caudal position to 5 o'clock cranial position. In this position the common bile duct (CBD) is seen behind the portal vein and the caudate lobe of liver lies between the Inferior vena cava and the scope. (Fig. 7)
Figure 7.
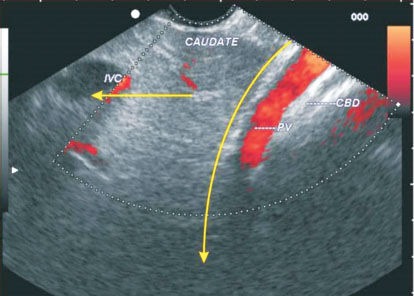
The probe is pulled up from the stomach and held at the gastro-oesophageal junction and rotated counter clockwise. The liver comes into view as a dense homogenous structure and posterior to its portal vein, hepatic artery and common bile duct can be seen. On anticlockwise rotation the inferior vena cava tends to move from 3 to 9 o'clock position whereas on anticlockwise rotation the portal vein moves from the 2-5 o'clock position. In this picture the common bile duct is seen beyond the portal vein through the liver window.
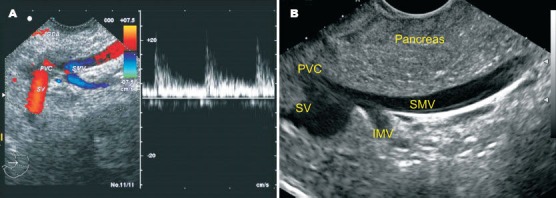
Antrum of stomach
During withdrawal of the scope, it comes back to lie in the antrum in a short position which is optimum for portal vein visualization. In this position the neck and body of pancreas lies between the scope and the portal venous confluence.37 The portal vein can be traced up from the butterfly confluence (confluence of superior mesenteric vein with splenic vein) to the hilum of liver by clockwise and/or anticlockwise rotation of the scope. (Fig. 8)
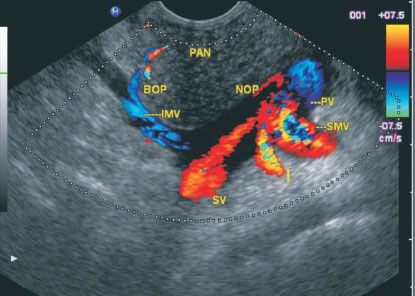
Figure 8.

The portal vein is identified in antrum of stomach and the union of splenic vein with superior mesenteric vein can be seen. In this picture the common bile duct is seen beyond the confluence through the pancreatic window.
Following up requires tilting the tip up and sometimes pulling up the scope a little back as the hilum of the liver is at a higher level as compared to the portal vein confluence. In this position the border closer to the scope is the left and the border away from the scope is the right border of portal vein. (Fig. 8, 9)
Figure 9.
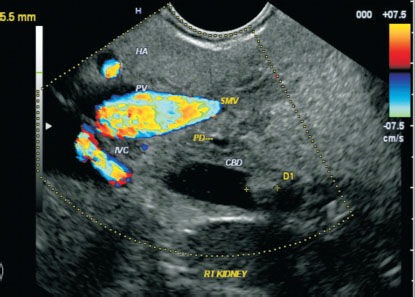
Clockwise and anticlockwise rotation of the scope in antrum can trace the course of portal vein downwards where it continues as superior mesenteric vein and the inferior vena cava can be seen going away from the screen. The common bile duct appears as a structure in between the two vascular structures and a common bile duct stone is seen in this case.
Duodenal bulb
The imaging from duodenal bulb requires nestling of scope into the duodenal bulb. When the scope is wedged into the apex of duodenal bulb (with controls loose) balloon may be inflated to occlude the lumen and gain better contact with duodenal wall. In this position the probe naturally faces the right lateral wall of duodenum. Generally moving the down knob down and maximum anti-clockwise rotation establishes good contact with the duodenal wall in this position. Pushing in and out, up and down, right and left and clockwise and anticlockwise torque will cause changes in view of scope. Manipulating the knobs identifies the gallbladder, CBD, pancreatic duct and the portal vein. The portal vein confluence and the portal vein can be seen on the right side of screen from the duodenal bulb. As the scope lies in J shape the cranial part of the portal vein (division in porta hepatis) lies to the right side of the screen and the formation of portal vein lies on the left side of the screen.39 (Fig. 10)
Figure 10.
The portal vein can be seen from the duodenal bulb with the scope in a J-shaped position. In this position the common bile duct lies closest to the duodenal wall and the hepatic artery comes to lie between the common bile duct and portal vein. The relationship of portal vein, hepatic artery and common bile duct near the liver hilum is VAD (vein, artery, and duct) from posterior to anterior.
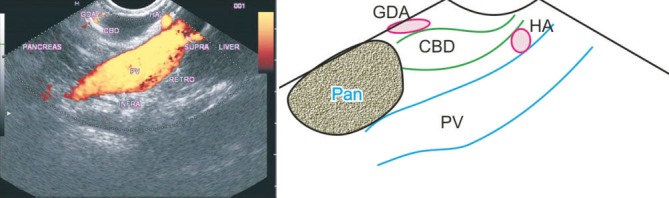
Duodenum
During withdrawal in the C loop of duodenum in the C sweep, the portal vein is traced as the continuation of the superior mesenteric vein. When the scope lies in descending duodenum some part of head of pancreas always lies between the portal vein and the scope. In this part of pancreas the two anechoic structures, CBD and pancreatic duct, are easily identified. When the scope is wedged at the superior duodenal angle, clockwise rotation traces the portal vein towards the confluence behind the neck of pancreas and anticlockwise rotation traces the portal vein towards the hilum of liver after emerging from the upper border of head of pancreas. On clockwise and anticlockwise rotation the change in relationship of portal vein to CBD and the hepatic and gastroduodenal arteries can be seen. (Fig. 10-12)
Figure 12.
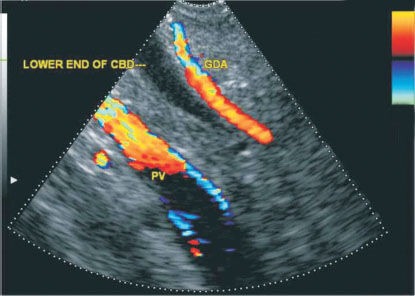
Portal vein imaging from the superior duodenal angle reveals the portal vein in a transverse axis posterior to the gastroduodenal artery and the lower end of common bile duct near the liver hilum on anticlockwise rotation after wedging the scope at the superior duodenal angle.
Figure 11.
The portal vein can be seen from the duodenal bulb with the scope in a J-shape position. In this position the course of portal vein is seen from the point of formation behind the neck of pancreas. In this picture the inferior mesenteric vein is also seen joining in the junction between splenic vein and superior mesenteric vein. The gastroduodenal artery is seen anterior to the neck of pancreas.
Relationship of CBD and portal vein
At the point of portal vein formation the portal vein lies behind the neck of pancreas in a relatively anterior position as compared to CBD, and the CBD crosses anteriorly over the portal vein to lie posterior to it to terminate at the ampulla. At this point the gastroduodenal artery lies anterior to the portal vein and these three structures (portal vein, gastroduodenal artery and CBD) have a DVA (duct, vein and artery) configuration from posterior to anterior. As the portal vein and CBD ascend, the anatomical relationship changes and the portal vein come to lie in a position posterior to CBD. Further higher up near the porta hepatis the hepatic artery as well as the CBD lies anterior to portal vein and the three structures (portal vein, hepatic artery and CBD) have a VAD (vein, artery and duct) configuration. The following figures show the three different relations of three parts of portal vein and CBD (infraduodenal, retroduodenal, and supraduodenal) from three different stations (Fig. 13A).
Figure 13.
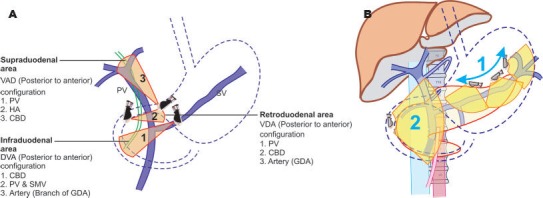
A: The stations for evaluation of the structures in porta hepatis are shown in this diagram. The infraduodenal part of the portal vein is assessed from the stomach, the retroduodenal part is best assessed from the superior duodenal angle, and the supraduodenal part is best assessed from the duodenal bulb. The infraduodenal part forms a DVA (duct, vein, and artery) configuration, retroduodenal part forms the VDA (vein, duct, and artery) configuration and the supraduodenal part forms the VAD (Vein, artery, and duct) configuration from posterior to anterior. B: The stations for linear endosonography of the splenic vein and its tributaries are shown in this diagram. The probe is taken at about 44 cm in the body of the stomach and on clockwise and anticlockwise rotation the entire course of splenic vein can be traced from the splenic hilum to portal venous confluence.
Splenic Vein
The evaluation of splenic vein can be done from body of stomach in all cases. During withdrawal from the horizontal duodenum the tracing of superior mesenteric vein was easy till the scope was withdrawn to the descending duodenum. In the descending duodenum and at the superior duodenal angle visualization of splenic vein is again possible but it is sometimes difficult as the position of the scope becomes unstable and it slips back into stomach.40 (Fig. 13B)
Body and antrum of stomach
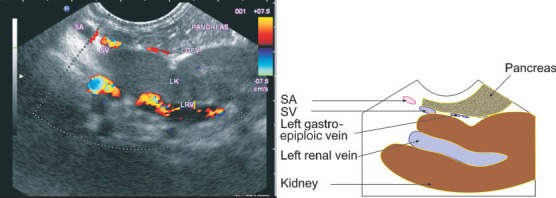
Splenic vein localization first requires tracing the aorta and the origin of the major arteries (celiac trunk and superior mesenteric artery) coming out from the aorta. Splenic vein is now located at 40 to 44 cm distance in body of stomach anterior to aorta and posterior to the body of pancreas. The entire course of splenic vein can be followed from pancreatic tail to the butterfly confluence behind the neck of pancreas by torque to right and left. On clockwise rotation the splenic vein is traced towards the splenic hilum and on anticlockwise rotation it is traced crossing in front of superior mesenteric artery and aorta to join the superior mesenteric vein. The course of splenic vein in relation to three other parallel vessels going to the left when the linear scope is rotated clockwise is also differentiated by use of color and pulse Doppler. These three vessels in relation to splenic vein are splenic artery, left renal artery and left renal vein (Fig. 14A, B). The splenic vein is generally identified below the splenic artery and above the left renal vein and left renal artery. Clockwise rotation and slight pulling up is required to trace the splenic vein towards the splenic hilum where the formative tributaries of the spleen can be seen merging with the left gastroepiploic vein to form the main trunk of splenic vein (Fig. 15, 16). After its formation the splenic vein crosses in front of the left adrenal gland and the left renal hilum (Fig. 17). The pancreatic tributaries can be seen merging into the anterior border coming from the pancreatic body (Fig. 18). Counterclockwise rotation of scope after placing scope over the aorta traces the splenic vein as it crosses over the superior mesenteric artery to join the superior mesenteric vein and makes a butterfly confluence (Fig. 7).41
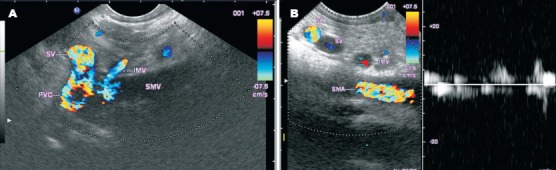
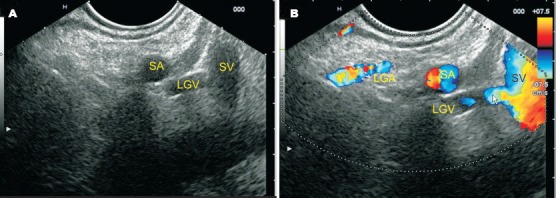
Figure 14.
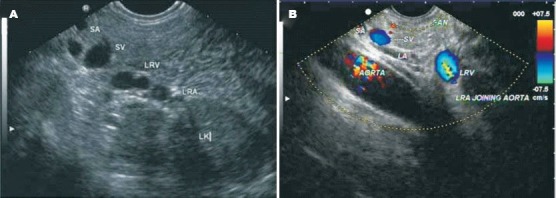
A: The relations of the splenic vein are shown. Splenic vein lies posterior to body of pancreas. Splenic artery is tortuous and seen in multiple sections superior to the splenic vein approximately at the upper border of pancreas. Left renal vessels and the hilum of left kidney are seen below the splenic vein. B: The splenic vein is seen lying behind the body of pancreas in front of aorta. The left renal artery is seen joining the aorta. The left renal vein crosses the aorta to join inferior vena cava.
Figure 15.
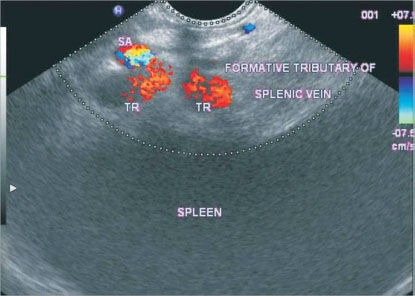
The picture shows the splenic hilum and the formative tributaries of splenic vein. Splenic artery is seen in a cross section anterior to the formative tributaries.
Figure 16.
Left gastroepiploic vein is seen in oblique section near the splenic hilum where it joins the formative tributaries of splenic vein to form the main trunk of the splenic vein. The tail of pancreas can also be seen.
Figure 17.

The relationship of splenic vessels with the left adrenal gland is seen. Left adrenal gland is posterior to the splenic artery and vein.
Figure 18.
Small tributaries coming from the pancreatic parenchyma may join the anterior surface of splenic vein as it lies behind the body of pancreas. Note that splenic artery lies at upper border of pancreas and both splenic vein and artery lie anterior to left adrenal gland.
Descending duodenum
Splenic vein is seen joining the superior mesenteric vein from the side on progressive withdrawal from the distal duodenum. It joins at a right angle behind the neck of pancreas. As the splenic vein is coming from an end on view and is joining the superior mesenteric vein from the side only a very short distance of splenic vein can be traced from the duodenum (Fig. 19).
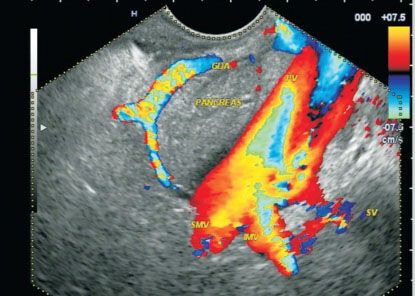
Figure 19.

Portal venous confluence is seen behind the neck of the pancreas from the descending duodenum. Inferior mesenteric vein is also seen joining the junction of splenic vein with superior mesenteric vein.
Superior Mesenteric Vein
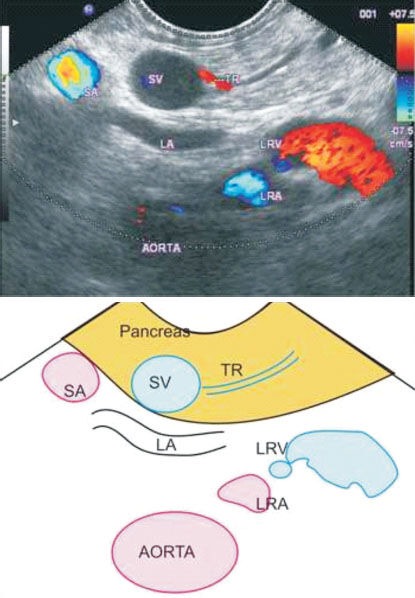
Superior mesenteric vein is evaluated from antrum of stomach, and descending duodenum (Fig. 20). The evaluation is possible both from stomach and duodenum in all cases.
Figure 20.
The stations for linear endosonography of the superior mesenteric vein are shown in this diagram. Clockwise from below: horizontal duodenum, descending duodenum and the duodenal bulb.
Antrum of stomach
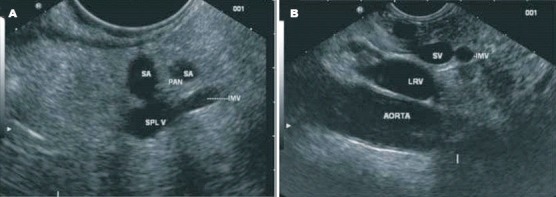
As the scope comes back from the duodenal bulb it naturally comes to lie in an optimum shortened position for scanning of the superior mesenteric vein in a longitudinal axis. In this position the body of pancreas is seen in front of the superior mesenteric vein and the head and the uncinate process are seen behind the superior mesenteric vein (Fig. 21).41,42 The superior mesenteric vein/splenic vein confluence appears as a butterfly (this confluence appears as a club on radial ultrasound) and from here the course of superior mesenteric vein can be followed for a short distance from the stomach by pushing down. The cranial wing of the butterfly is the portal vein, the caudal wing is the superior mesenteric vein, and the body where the right and left wing meet at the portal vein confluence corresponds to splenic vein. (Fig. 22)
Figure 21.
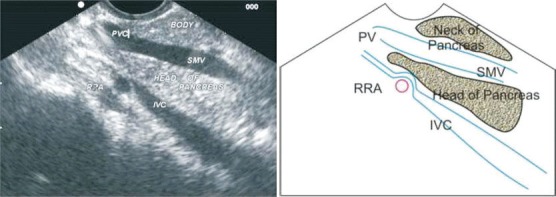
Superior mesenteric vein is viewed from descending duodenum in a longitudinal section. Superior mesenteric vein in this position separates the body of pancreas from the head. The part between the scope and the superior mesenteric vein is the neck and body of pancreas and the part between superior mesenteric vein and inferior vena cava is the head of pancreas.
Figure 22.
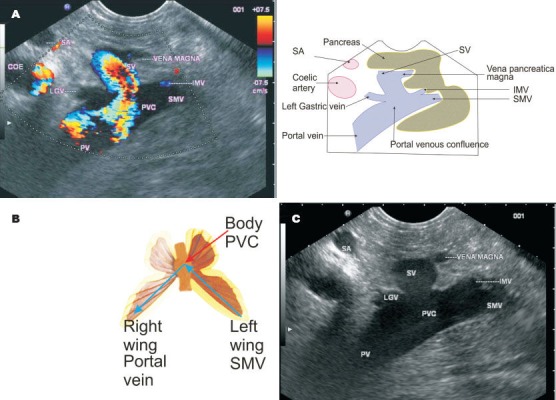
A: Imaging from the antrum shows the butterfly confluence which signifies the union of splenic vein with superior mesenteric vein. In this position the superior mesenteric vein is seen as the left wing of butterfly and portal vein is seen as the right wing of butterfly. B: The point where these two wings meet at the body signifies splenic vein. Left gastric and inferior mesenteric vein are also seen joining at the portal venous confluence. C: The left gastric and inferior mesenteric veins are highly variable in their termination into the portal venous system. In this case on grayscale imaging, the left gastric vein as well as inferior mesenteric vein is seen joining the portal venous system.
Superior mesenteric vein imaging during the C sweep of duodenum
The visualization of superior mesenteric vein in horizontal duodenum requires first positioning it into the third part of duodenum. Scope should be advanced to the deepest part of duodenum beyond the ampulla and then withdrawn into short position. Once the scope is advanced beyond the inferior duodenal angle junction, repeatedly pushing and shortening two to three times pushes the scope deeper into horizontal duodenum. From the horizontal duodenum the imaging of superior mesenteric vein can be started and continued till the scope reaches the descending duodenum where it becomes the portal vein. Pulling the scope further up near the superior duodenal angle traces the portal vein to the hilum of liver. When the scope is in horizontal duodenum the superior mesenteric vein seems to be seen at an angle from the scope and the distal end almost touches the scope. (Fig. 23)
Figure 23.
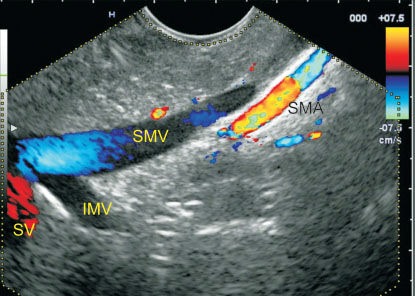
Clockwise rotation while withdrawing from the descending duodenum shows the superior mesenteric vein in a longitudinal section. In this frame the superior mesenteric artery disappears from view as lies posterior, close to its origin from the aorta. At the junction of superior mesenteric vein and splenic vein, the inferior mesenteric vein is seen joining the confluence.
On progressive withdrawal superior mesenteric vein becomes parallel to the scope and the lower part of head of pancreas comes to lie between it and the scope. The border of superior mesenteric vein close to the scope is the right border of superior mesenteric vein and the border away from the scope is the left border of superior mesenteric vein. The splenic vein, inferior mesenteric vein, first jejunal trunk, other jejunal and ileal tributaries join the left border whereas the gastrocolic trunk joins the right border (Fig. 24, 25). During this withdrawal the axis and orientation of superior mesenteric vein and portal vein with the scope changes progressively and the distal end of the probe initially lies very close to superior mesenteric vein, then parallel to superior mesenteric vein and finally further higher up away from portal vein (Fig. 26A-D, 27). The progressive withdrawal of the scope should be associated with slight clockwise and anticlockwise rotation of the scope to visualize the entire structures lying in posterior and medial relations to the second part of duodenum. The rotation is required to clarify the relationship of superior mesenteric vein and its tributaries (Fig. 26). During withdrawl of scope from horizontal duodenum the scope has a tendency to fall back and slip into stomach.
Figure 24.
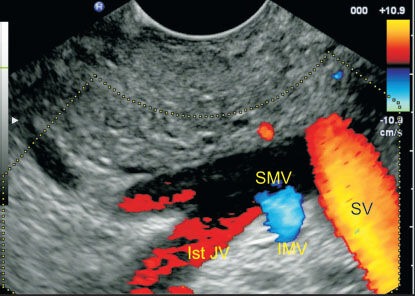
The portal venous confluence is seen in a J-shape position. The joining of first jejunal vein and inferior mesenteric vein is seen at the border away from the probe. The border of superior mesenteric vein close to the scope is the right border of superior mesenteric vein and the border away from the scope is the left border of superior mesenteric vein. The splenic vein, inferior mesenteric vein, first jejunal trunk, other jejunal and ileal tributaries join the left border whereas the gastrocolic trunk joins the right border.
Figure 25.
A: The right angled junction of splenic vein and superior mesenteric vein is seen from the descending duodenum. The inferior mesenteric vein is seen joining the junction between splenic vein and superior mesenteric vein. The pulse Doppler shows gastroduodenal artery in the top right area of the image close to the duodenal wall. B: On clockwise rotation while withdrawing from the descending duodenum, the tributaries of superior mesenteric vein are visible. The border away from the probe is the left border of the superior mesenteric vein and on that border three tributaries are seen joining from below upwards. The lowest is first jejunal trunk. Higher up the inferior mesenteric vein and then the splenic vein joins the superior mesenteric vein. The joining of splenic vein into superior mesenteric vein gives the imaging of a stub. The pancreas is seen well parallel to the superior mesenteric vein.
Figure 26.
The C sweep from horizontal duodenum to superior duodenal angle. The arrow shows direction of flow. A: In horizontal duodenum–The superior mesenteric vein is seen taking an acute angle and the distal part of superior mesenteric vein gets very close to distal end of the probe. B: At Inferior duodenal angle–As the scope is progressively withdrawn in a C sweep the superior mesenteric vein tends to become more parallel to the scope. Rotation of the scope from this position to the right and the left can demonstrate the smaller tributaries joining the superior mesenteric vein. C: In descending duodenum- As the scope reaches descending duodenum in a neutral position of the knobs the superior mesenteric vein lies parallel to the scope. Rotation of the scope at this position to the right and left can demonstrate the joining of the splenic vein. A part of pancreas is always seen between the probe and superior mesenteric vein. D: At superior duodenal angle-The gastroduodenal artery runs parallel to the wall of duodenum and portal vein seems to be going away from the distal end of the probe. Rotation of the scope to the right and left from this position may demonstrate the joining of posterior superior pancreaticoduodenal vein.
Figure 27.
When the scope is in the descending duodenum, maximum anti-clockwise rotation to the left will show the right kidney. On anticlockwise rotation, the inferior vena cava and common bile duct are first seen behind the head of pancreas; on further rotation, the uncinate process comes to lie between the probe and the aorta. On further anticlockwise rotation, the superior mesenteric artery and the vein are seen. The above figure shows a cross section of how the structures appear one after another on clockwise rotation in the following order (right renal vein-inferior vena cava–Aorta-superior mesenteric artery-superior mesenteric vein).
When the scope in descending duodenum lies close to the ampulla, the joining of splenic vein into the superior mesenteric vein at the portal venous confluence may give the appearance of a ‘stub’. (Fig. 25A, B)
Inferior Mesenteric Vein
The variable anatomy of the inferior mesenteric vein requires scanning from two stations (Fig. 3A-C). Initially the inferior mesenteric vein is traced from the stomach and found in a majority of cases merging with the lower border of splenic vein. If inferior mesenteric vein cannot be seen from stomach then it is located from duodenum.
Inferior mesenteric vein imaging from stomach
Inferior mesenteric vein draining into splenic vein is screened from stomach while scanning the borders of splenic vein from the stomach and moving the probe from the splenic hilum to the portal venous confluence. The inferior mesenteric vein is seen in a cross section coursing cranially after crossing the renal vessels to join the splenic vein at the inferior border of splenic vein (Fig. 28A, B, 29A, B).41
Figure 28.
A: Inferior mesenteric vein is shown in a cross section before it joins the splenic vein. Note the posterior relations of the splenic vein with the left kidney are clearly shown. Inferior mesenteric vein is generally seen as ascending cranially from the right to left side of the screen before merging with the splenic vein. B: The inferior mesenteric vein is crossing in front of superior mesenteric artery at around the lower border of pancreas where it lies below the splenic vein.
Figure 29.
A, B: Inferior mesenteric vein is seen joining the splenic vein on linear endosonography from the stomach in two patients. The relationship of inferior mesenteric vein with the left renal hilum and vessels is also seen in the second figure.
Inferior mesenteric vein imaging from duodenum
Inferior mesenteric vein draining into the superior mesenteric vein or the portal venous confluence is screened from the duodenum. If inferior mesenteric vein does not join splenic vein, then it curves sharply to the right and passes below and parallel to the splenic vein in front of the superior mesenteric artery to drain into the superior mesenteric vein or the portal venous confluence (Fig. 19, 30).
Figure 30.
The course of inferior mesenteric vein is seen as it proceeds to merge with the splenic vein above the renal hilum.
Left and Right Gastric Vein
The variable anatomy of the left gastric vein may require scanning from different stations.41 Initially left gastric vein is traced from fundus in a majority of cases. If it is not possible to trace it from above downwards, then an attempt is made to trace it upwards from the portal venous confluence. Left gastric vein is a vein with large diameter and is easily picked up as it is traced from above downwards from the oesophagogastric junction (Fig. 31). As the scope is introduced in stomach, the left gastric artery and the left gastric vein are the first vessels lying close to the esophagus. A pulse Doppler can differentiate the left gastric vein from the corresponding artery and then it can be followed down to the point of joining into portal venous system (Fig. 32A, B). Sometimes it is much easier to trace the left gastric vein up towards the oesophagogastric junction by tracing the point of joining at the upper border of the portal venous confluence within 2 cm of confluence (Fig. 33A).
Figure 31.

The left gastric vein is seen joining the upper border of splenic vein near the confluence. The inferior mesenteric vein is seen joining the superior mesenteric vein just before the portal venous confluence.
Figure 32.
A: The left gastric vein is seen joining the upper border of splenic vein on grayscale imaging. B: The left gastric vein is seen joining the upper border of splenic vein on color Doppler imaging. The splenic artery and the left gastric artery join near the celiac trifurcation.
Figure 33.
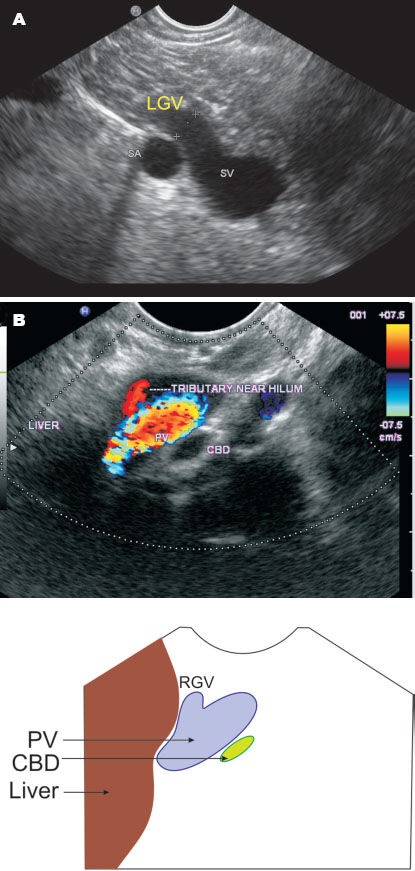
A: Imaging from the antrum reveals the left gastric vein joining the splenic vein in a patient with portal hypertension. The diameter of left gastric vein is 5.1 mb. B: The right gastric vein is seen joining near the anterior border of portal vein near the hilum.
Right gastric vein, being a small vein, is not easy to detect. It is detected below the confluence as the vein joins the anterior border of portal vein (Fig. 33B).
Left and Right Gastroepiploic Veins
Left gastroepiploic vein can be seen while scanning along the greater curvature of the stomach near the splenic hilum. It is seen joining the formative tributaries to form the splenic vein (Fig. 16). The right gastroepiploic vein is a tributary of gastrocolic trunk and is seen from the descending duodenum while scanning for the gastrocolic trunk (Fig. 34, 35).
Figure 34.
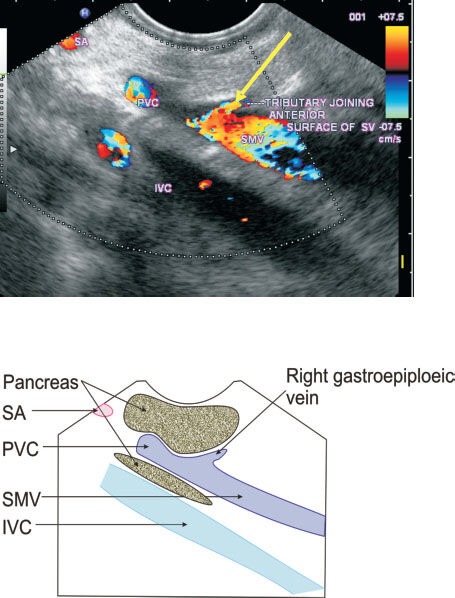
Imaging from the antrum of stomach reveals a tributary joining the anterior surface of superior mesenteric vein below the lower border of pancreas.
Figure 35.
Imaging from the descending duodenum shows the superior mesenteric vein and the gastrocolic trunk joining the superior mesenteric vein. From the gastrocolic trunk, the right colic vein is seen surrounded by a fat which goes towards transverse mesocolon. On further rotation the right gastroepiploic vein is seen piercing the transverse mesocolon to join the right colic vein and forming the gastrocolic trunk.
Gastrocolic and First Jejunal Trunk
The first jejunal trunk can be located as the scope is withdrawn from the horizontal duodenum towards the descending duodenum (Fig. 36A, B). Sometimes imaging is better while advancing the scope in J-shape towards duodenal bulb (Fig. 36C). The gastrocolic trunk can be also located as the scope is withdrawn from the horizontal duodenum towards the descending duodenum (Fig. 37). As the scope is withdrawn, a color Doppler box is applied on the entire course of superior mesenteric vein, which comes to lie exactly in a parallel position to the scope. In this position the left border of superior mesenteric vein lies away from the scope and the right border of superior mesenteric vein lies close to the scope. Both the first jejunal trunk and gastrocolic trunk can be either seen at the same level joining the opposite side of superior mesenteric vein. If they are not seen together, slight clockwise rotation will demonstrate the first jejunal trunk and anticlockwise rotation will demonstrate the gastrocolic trunk. It must be remembered that these two trunks are about 1 to 5 cm below the joining of superior mesenteric vein and splenic vein (Fig. 24, 36, 37).
Figure 36.
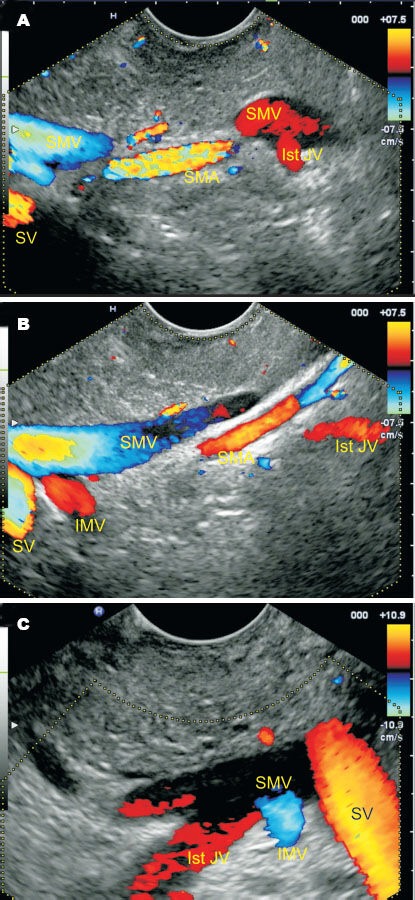
A: While withdrawing from the descending duodenum, the first jejunal trunk is seen joining the border of the superior mesenteric vein away from the transducer. Three veins are seen joining the border away from the transducer from below upwards. The three veins are the first jejunal trunk, inferior mesenteric vein and splenic vein. The first jejunal trunk goes posterior to the superior mesenteric artery and inferior mesenteric vein crosses anterior to the superior mesenteric artery. B: The first jejunal vein is seen going towards the medial aspect of superior mesenteric vein about 3 cm below the joining of inferior mesenteric vein. C: The portal venous confluence is seen in a J-shape position. The joining of the first jejunal vein and inferior mesenteric vein is very close to each other.
Figure 37.

The gastrocolic trunk is seen taking origin from the aspect of superior mesenteric vein closer to the descending duodenum.
Pancreatic Veins
Posterior superior pancreaticoduodenal vein is seen during withdrawal from the descending duodenum in a majority of cases. On slight clockwise rotation from the antrum of the stomach while visualizing the portal vein, posterior superior pancreaticoduodenal vein can be seen merging with its right postero-lateral border (Fig. 38A, B).
Figure 38.
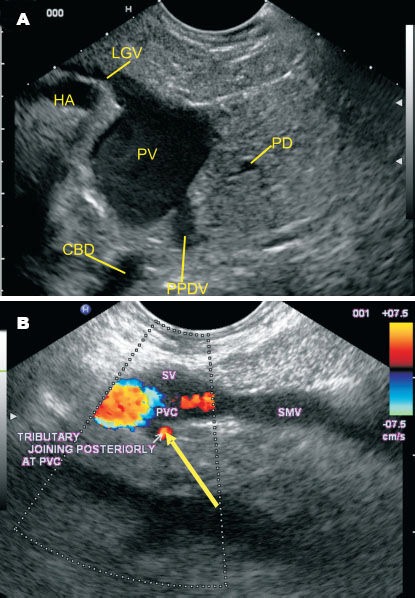
A: Imaging from the stomach shows the left gastric vein joining the portal vein above the confluence near the anterior border. Just opposite to this position in this picture the posterior superior pancreaticoduodenal vein can be seen merging with its right posterolateral border. The common bile duct is seen behind the portal vein and the pancreatic duct is seen below the portal vein. B: In this picture the posterior superior pancreaticoduodenal vein is seen crossing the common bile duct and joining the portal vein from its posterior aspect in the retroduodenal area just above the upper border of pancreas.
Alternatively the posterior superior pancreaticoduodenal vein can be seen from the antrum. The inferior pancreaticoduodenal vein can be sometimes seen as a small tributary arising from the first jejunal trunk and curving to proceed to the head of the pancreas. It is however difficult to trace it due to its small caliber (Fig. 38).
The anterior superior pancreaticoduodenal vein is not easily seen on linear endosonography.
Colic Veins
The middle colic vein is seen joining the anterior aspect of superior mesenteric vein behind the body of pancreas from the descending duodenum. It can be traced when continuous color Doppler screening is done on the border of superior mesenteric vein close to the posterior surface of pancreas just before it joins the splenic vein at the portal venous confluence (Fig. 39). The right colic vein is seen from the descending duodenum while scanning for the gastrocolic trunk. It is seen surrounded by the transverse mesocolon and merging with right gastroepiploic vein to form the gastrocolic trunk (Fig. 35).
Figure 39.
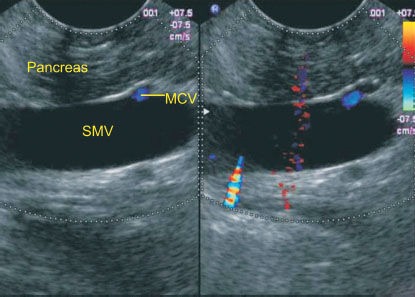
The middle colic vein is seen joining the anterior aspect of superior mesenteric vein behind the body of pancreas from the descending duodenum. It can be traced when continuous color Doppler screening is done on the border close to the scope which lies anterior to the segment of superior mesenteric vein just before it joins the splenic vein at the portal venous confluence.
DISCUSSION
EUS is an excellent imaging modality for evaluation of vascular anatomy. Various authors have shown the normal echo anatomy of the upper gastrointestinal tract over the years.37,38,39,40,41,42,43 They have described numerous abdominal stations depending on their techniques and indications. The demonstration of the various abdominal stations for the same vessel will expand an endosonographer's knowledge about the course of the vessel and show important relationship with other visceral structures. Since the linear endosonography is heavily user-dependent, confirmation of the same finding from various stations will also minimize the errors of misinterpretation of vessels. Most authors have described the normal endosonographic anatomy of three main veins of the portal venous system (splenic vein, superior mesenteric vein and portal vein) in detail and little importance have been given to smaller tributaries like inferior mesenteric vein and left gastric vein.37,40,42,43 In this article, one of our primary objectives has been to describe techniques of visualizing the tributaries of portal venous system in detail.
Numerous authors have evaluated the tributaries of the portal venous system by different radiologic modalities. Abdominal ultrasonography with color Doppler have been used to evaluate the main portal venous system vessels as well as some smaller tributaries like left gastric vein, inferior mesenteric vein and left gastroepiploic vein.21,24,25,27 Linear endosonography however provides better resolution images being closer to the vessels in the retroperitoneum and can also demonstrate smaller veins.40 It however may not be able to demonstrate the entire course of vessels and is heavily operator-dependant. We feel that abdominal ultrasound should always precede linear endosonography and the correlation of their findings will lead to an optimal vascular picture.
Evaluation of dilated common bile duct is one of the most important diagnostic indications of endosonography and thus precise elucidation of normal relationship of CBD with surrounding portal vessels is always useful. The CBD and portal vein are intimately related to each other in their course and their relationship can be evaluated from different abdominal stations (Fig. 13A). In cases of obstruction of the biliary tree, accurate identification of the portal vein and its relation to the dilated CBD is helpful in locating the level of obstruction.44 This demonstration of precise relationship may also be of clinical importance to laparoscopic surgeons.
Computed tomography scans with contrast and magnetic resonance angiography have demonstrated the tributaries of portal venous system in detail. Computed20,21,22,23,26,28,29,31,32,45,46,47 tomography scan despite being an ideal modality does not render tools for assessing hemodynamics of the portal vessels. The magnetic resonance angiography gives excellent 3-dimensional images but shows overlapping of the arterial vessels on the portal venous system and its branches. The overlapping can be avoided by subtraction of images acquired in the arterial phase from image acquired in portal phase. Real-time evaluation of linear endosonography with the help of pulse and color Doppler also allows differentiation between arterial and venous branches. It also provides numerous other tools to assess the hemodynamic parameter such as blood flow velocity, direction of flow and resistive index of the vessels.48
The variceal bleeding is an important complication of portal hypertension and endosonography has been used to study the esophageal, rectal and CBD varices. Endosonography in portal hypertension has shown that both the peri- and para-esophageal collaterals enter submucosa of esophagus after perforating the muscularis mucosa to appear as esophageal varices.12 Extrahepatic obstruction of the portal vein is a common cause of portal hypertension and may produce extensive para-choledochoduodenal and epicholedochoduodenal collateral venous circulation near the CBD and porta hepatis. Detection of these para-choledochoduodenal and epicholedochoduodenal collaterals near CBD has been done by endosonography.49,50 The perforators of duodenum in the form of duodenal varices and perforators of CBD wall from collaterals have also been demonstrated in portal hypertension by endosonography.51 Evaluation of perforators of esophageal, rectal and CBD wall varices may be better done if the operator has proper orientation of the peri-oesphageal, peri-gastric or perirectal veins from which these perforators take origin. Precise determination of anatomic courses and blood flow of left gastric vein and inferior mesenteric vein may be helpful in management of ectopic varices.
Universally, acute non-cirrhotic, non-tumor portal vein thrombosis (PVT) is the second most-frequent cause of portal hypertension. At the early stage, prompt anticoagulation allows recanalization in at least 75% of patients, which needs to be continued for 4 to 6 months. Currently, there are no studies available for intravascular thrombolysis in such cases, as portal vein remains the most inaccessible vein by standard angiographic techniques. Precise characterization of anatomy of portal vein from different stations can help in selection of the ideal position for interventional procedures.
Pancreatic cancer due to its highly invasive nature can involve the surrounding vascular structures at an early stage of cancer. Accurate staging of pancreatic cancer before surgery plays an important role in determining the extent of surgery and predicting its prognosis. Computed tomography scans has been traditionally used for this purpose but arrangement of organs around the pancreas is complex and difficult to assess.36 The peri-pancreatic veins demarcate important structures and their involvement is useful for assessing cancer invasion. Dilatations of Anterior superior pancreatico duodenal vein, Posterior superior pancreatico duodenal vein and gastrocolic trunk as collateral pathways or secondary changes in portal venous blood flow are valuable indicators of portal vein invasion at earlier stages of pancreatic cancer.29,30 Occlusion of gastrocolic trunk is indicative of involvement of transverse mesocolon and involvement of inferior veins indicates spread to extrapancreatic nerve plexus.31,32,33,34,52 Demonstration of peri-pancreatic veins by EUS may be included in the routine evaluation of pancreatic cancer to evaluate the spread to these vessels.
Depiction of vascular anatomy may have its use in portal venous puncture and measuring the portal vein pressure for suspected cases of portal hypertension. We know that hepatic venous pressure gradient (HVPG), an indirect measure of the portal vein pressure, is highly predictive of the patient's clinical course. Measuring the pressure directly should be a better predictor of mortality and morbidity of patients with portal hypertension and can be done by the aid of endosonography.6 The large needle (19-G) puncture into portal veins is more risky and the smaller needle (25-G) puncture may not give the necessary rate of injection for a proper venogram.13 In future, endotherapy may offer puncture of smaller veins with a smaller risk as compared to puncturing of larger veins. Further research is required in animal models for comparison of feasibility of puncturing of larger veins with smaller needles or smaller veins with larger needles. This type of evaluation again requires a detailed understanding of small tributaries of portal venous system. Only after detailed evaluation in animal models; portal venography, portal pressure monitoring, or portal decompression can be safely performed under endosonography guidance in human beings.13,14,15
There is paucity of data and outcome regarding the use of endosonography in endotherapy of portal venous system, but endosonography has the potential for providing an alternative to percutaneous methods for accessing intra-abdominal vasculature for diagnostic and therapeutic interventions.5 Precise therapy can be delivered by endosonography to vascular sites that are inaccessible to usual haemostatic techniques by endoscopic visualization.5
The portal venous system has a very variable anatomy and misinterpretation of vessels is possible. The best method to avoid this fallacy is to obtain a clear window in which the abdominal veins can be viewed in relation to important organs. These windows are obtained by scanning from initializing the scan from various standardized abdominal stations.
CONCLUSION
Endosonography can delineate the vascular anatomy of the portal venous system and its tributaries with accuracy and reproducibility. The establishment of such criteria will open the road for interventional diagnostic and therapeutic uses of linear endosonography in diseases affecting the portal venous system.
ACKNOWLEDGEMENTS
We would like to thank Mr. Pran Prakash, our graphic designer for his technical support in preparing the hand drawings in this article.
APPENDIX
PV: portal vein; SV (SPLV): splenic vein; SA: splenic artery; SMV: superior mesenteric vein; IMV: inferior mesenteric vein; SMA: superior mesenteric artery; LGV: left gastric vein; RGV: right gastric vein; GB: gallbladder; 1st JV: first jejunal trunk; GT(GCT): gastrocolic trunk; RGEV: right gastroepiploic vein; ASPDV: anterior superior pancreaticoduodenal vein; SRCV: superior right colic vein; RCV: right colic vein; MCV: middle colic vein; PSPDV(PPDV): posterior superior pancreaticoduodenal vein; PIPDV: posterior inferior pancreaticoduodenal vein; AIPDV: anterior inferior pancreaticoduodenal vein; IVC: inferior vena cava; CBD: common bile duct; CAUDATE: caudate lobe of liver; HA: hepatic artery; PD: pancreatic duct; RIKIDNEY: right kidney; PAN: pancreas; NOP: neck of pancreas; BOP: body of pancreas; GDA: gastroduodenal artery; LRV: left renal vein; LRA: left renal artery; RK: right kidney; LK: left kidney; LA: left adrenal gland; TR: tributary; LEGV: left gastroepiploic vein; RRA: right renal vein; COE: coelic artery; VENA MAGNA: vena pancreatica magna; PVC: portal venous confluence
REFERENCES
- 1.Sharma M, Ramesh Babu CS, Garg S, et al. Portal Venous System and Its Tributaries: A Radial Endosonographic Assessment. Endosc Ultrasound. 2012;1:96–107. doi: 10.7178/eus.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller LS. Endoscopic ultrasound in the evaluation of portal hypertension. Gastrointest Endosc Clin N Am. 1999;9:271–85. [PubMed] [Google Scholar]
- 3.Sharma M, Somasundaram A. Massive lower GI bleed from an endoscopically inevident rectal varices: diagnosis and management by EUS (with videos) Gastrointest Endosc. 2010;72:1106–8. doi: 10.1016/j.gie.2010.02.054. [DOI] [PubMed] [Google Scholar]
- 4.Sharma M, Rameshbabu CS, Dhiman RK, et al. Induced hypotension in the management of acute hemobilia during therapeutic ERCP in a patient with portal biliopathy (with videos) Gastrointest Endosc. 2010;72:1317–9. doi: 10.1016/j.gie.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 5.Tian YT, Wang CF, Wang GQ, et al. Prospective evaluation of the clinical significance of ultrasonography, helical computed tomography, magnetic resonance imaging and endoscopic ultrasonography in the assessment of vascular invasion and lymph node metastasis of pancreatic carcinoma. Zhonghua Zhongliu Zazhi. 2008;30:682–5. [PubMed] [Google Scholar]
- 6.Levy MJ, Chak A. EUS 2008 Working Group document: evaluation of EUS-guided vascular therapy. Gastrointest Endosc. 2009;69:S37–S42. doi: 10.1016/j.gie.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Brugge W. EUS is an important new tool for accessing the portal vein. Gastrointest Endos. 2008;67:343–4. doi: 10.1016/j.gie.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 8.Sharma M, Pathak A. Perforators of common bile duct wall in portal hypertensive biliopathy (with videos) Gastrointest Endosc. 2009 Nov;70(5):1041–3. doi: 10.1016/j.gie.2009.03.040. [DOI] [PubMed] [Google Scholar]
- 9.De Paulo GA, Ardengh JC, Nakao FS, et al. Treatment of esophageal varices: a randomized controlled trial comparing endoscopic sclerotherapy and EUS-guided sclerotherapy of esophageal collateral veins. Gastrointest Endosc. 2006;63:396–402. doi: 10.1016/j.gie.2005.10.039. quiz 63. [DOI] [PubMed] [Google Scholar]
- 10.Fockens P, Meenan J, Dullemen van HM, et al. Dieulafoy's disease: endosonographic detection and endosonography-guided treatment. Gastrointest Endosc. 1996;44:437–42. doi: 10.1016/s0016-5107(96)70096-2. [DOI] [PubMed] [Google Scholar]
- 11.Levy MJ, Wong Kee Song LM, Farnell MB, et al. Endoscopic ultrasound (EUS)-guided angiotherapy of refractory gastrointestinal bleeding. Am J Gastroenterol. 2008;103:352–9. doi: 10.1111/j.1572-0241.2007.01616.x. [DOI] [PubMed] [Google Scholar]
- 12.Sato T. Usefulness of endoscopic color Doppler ultrasonography (ECDUS) for evaluation of endoscopic injection sclerotherapy (EIS) and a clinical study on prognosis following EIS by ECDUS [Japanese with English abstract] Hokkaido IgakuZasshi. 1992;67:744–7. [PubMed] [Google Scholar]
- 13.Irisawa A, Obara K, Sato Y, et al. EUS analysis of collateral veins inside and outside the esophageal wall in portal hypertension. Gastrointest Endosc. 1999;50:374–80. doi: 10.1053/ge.1999.v50.97777. [DOI] [PubMed] [Google Scholar]
- 14.Lai L, Poneros J, Santilli J, et al. EUS-guided portal vein catheterization and pressure measurement in an animal model: a pilot study of feasibility. Gastrointest Endosc. 2004;59:280–3. doi: 10.1016/s0016-5107(03)02544-6. [DOI] [PubMed] [Google Scholar]
- 15.Giday SA, Clarke JO, Buscaglia JM, et al. EUS-guided portal vein catheterization: a promising novel approach for portal angiography and portal vein pressure measurements. Gastrointest Endosc. 2008;67:338–42. doi: 10.1016/j.gie.2007.08.037. [DOI] [PubMed] [Google Scholar]
- 16.Standring S. 39th Ed. Churchill Livingstone; 1999. Gray's anatomy; pp. 1219–1220. [Google Scholar]
- 17.Agur A.M.R, Lee M.J. 10th Ed. Philadelphia: Lippincott Williams and Wilkins; 1999. Grant's Atlas of Anatomy; pp. 126–127. [Google Scholar]
- 18.Douglass BE, Baggenstoss AH, Hollinshead WH. The anatomy of the portal vein and its tributaries. Surg Obstet Gynecol. 1950;91:562–76. [PubMed] [Google Scholar]
- 19.Falconer CW, Griffiths E. The anatomy of the blood-vessels in the region of the pancreas. Br J Surg. 1950;37:334–44. doi: 10.1002/bjs.18003714721. [DOI] [PubMed] [Google Scholar]
- 20.Ito K, Blasbalg R, Hussain SM, Mitchell DG. Portal vein and its tributaries: evaluation with thin-section three-dimensional contrast-enhanced dynamic fat-suppressed MR imaging. Radiology. 2000;215:381–6. doi: 10.1148/radiology.215.2.r00ap04381. [DOI] [PubMed] [Google Scholar]
- 21.Zerin JM, DiPietro MA. Mesenteric vascular anatomy at CT: normal and abnormal appearances. Radiology. 1991;179:739–42. doi: 10.1148/radiology.179.3.2027985. [DOI] [PubMed] [Google Scholar]
- 22.Zhang XM, Zhong TL, Zhai ZH, et al. Venography of the inferior mesentery vein. Eur J Radiol. 2007;64:147–51. doi: 10.1016/j.ejrad.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 23.Wachsberg RH. Inferior Mesenteric Vein: Gray-Scale and Doppler Sonographic Findings in Normal Subjects and in Patients with Portal Hypertension. AJR Am J Roentgenol. 2005;184:481–6. doi: 10.2214/ajr.184.2.01840481. [DOI] [PubMed] [Google Scholar]
- 24.Jia Y, Wang TJ, Allendorf J, Saif MW, et al. Management of Borderline Resectable Pancreatic Adenocarcinoma. JOP J Pancreas (Online) 2012;13:147–50. [PubMed] [Google Scholar]
- 25.Roi DJ. Ultrasound anatomy of the left gastric vein. Clin Radiol. 1993 Jun;47:396–8. doi: 10.1016/s0009-9260(05)81059-1. [DOI] [PubMed] [Google Scholar]
- 26.Seong LN, Chung WJ, Kim CH, et al. Right Gastric Venous Drainage: Angiographic Analysis in 100 Patients. Korean J Radiol. 2012;13:53–60. doi: 10.3348/kjr.2012.13.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Konno K, Ishida H, Komatsuda T, et al. Color Doppler sonography of the gastroepiploic vein. Abdom Imaging. 1999;24:228–31. doi: 10.1007/s002619900486. [DOI] [PubMed] [Google Scholar]
- 28.Moody AR, Poon PY. Gastroepiploic veins: CT appearance in pancreatic disease. AJR Am J Roentgenol. 1992;158:779–83. doi: 10.2214/ajr.158.4.1546593. [DOI] [PubMed] [Google Scholar]
- 29.Mori H, McGrath FP, Malone DE, et al. The gastrocolic trunk and its tributaries: CT evaluation. Radiology. 1992;182:871–7. doi: 10.1148/radiology.182.3.1535911. [DOI] [PubMed] [Google Scholar]
- 30.Ibukuro K, Ishii R, Fukuda H, et al. Collateral venous pathways in the transverse mesocolon and greater omentum in patients with pancreatic disease. AJR Am J Roentgenol. 2004;182:1187–93. doi: 10.2214/ajr.182.5.1821187. [DOI] [PubMed] [Google Scholar]
- 31.Crabo LG, Conley DM, Graney DO, et al. Venous anatomy of the pancreatic head: normal CT appearance in cadavers and patients. AJR Am J Roentgenol. 1993;160:1039–45. doi: 10.2214/ajr.160.5.8385877. [DOI] [PubMed] [Google Scholar]
- 32.Ibukuro K, Tsukiyama T, Mori K, et al. Peripancreatic veins on thin-section (3 mm) helical CT. AJR Am J Roentgenol. 1996;167:1003–8. doi: 10.2214/ajr.167.4.8819401. [DOI] [PubMed] [Google Scholar]
- 33.Vedantham S, Lu DS, Reber HA, et al. Small peripancreatic veins: improved assessment in pancreatic cancer patients using thin-section pancreatic phase helical CT. AJR Am J Roentgenol. 1998;170:377–83. doi: 10.2214/ajr.170.2.9456949. [DOI] [PubMed] [Google Scholar]
- 34.Mori H, Miyake H, Aikawa H, et al. Dilated posterior superior pancreaticoduodenal vein: recognition with CT and clinical significance in patients with pancreaticobiliary carcinomas. Radiology. 1991;181:793–800. doi: 10.1148/radiology.181.3.1947099. [DOI] [PubMed] [Google Scholar]
- 35.Birtwisle Y, Ferrari C, Bourgeon A, et al. Venous drainage of the pancreas and its relations to pancreatic phlebography. Anat Clin. 1983;5:103–13. [Google Scholar]
- 36.Hongo N, Mori H, Matsumoto S, et al. Anatomical variations of peripancreatic veins and their intrapancreatic tributaries: multidetector-row CT scanning. Abdom Imaging. 2010;35:143–53. doi: 10.1007/s00261-007-9195-3. [DOI] [PubMed] [Google Scholar]
- 37.Rosch T, Will U, Chang KJ, editors. Berlin: Springer Verlag; 2001. Longitudinal Endosonography: Atlas and Manual for Use in the Upper Gastrointestinal Tract; pp. 23–58. [Google Scholar]
- 38.Dietrich CF. Pancreaatic Adenocarcinoma: The role of Endoscopic ultrasonography in Endoscopic Ultrasound: An Introductory Manual and Atlas. ThiemeVerlag. 2006:196–200. [Google Scholar]
- 39.Hawes RH, Fockens P, editors. Endosonography. Philadelphia, USA: Saunders Elsevier; 2006. pp. 149–154. [Google Scholar]
- 40.Sharma M. Uttar Pradesh, India: Nageen Prakashan Pvt. Ltd; 2007. Endoscopic Ultrasound: How to do? pp. 31–56. [Google Scholar]
- 41.Sun SY. People's Medical Publishing House; 2008. Electronic Endoscopic Ultrasonography: Diagnostic imaging and Interventional Techniques; pp. 51–85. [Google Scholar]
- 42.Yamao K, Irisawa A, Inoue H, et al. Standard Imaging Techniques of endoscopic ultrasound-guided fine-needle aspiration using a curved linear array echoendoscope. Digest Endosc. 2007;19(S1):S180–S205. [Google Scholar]
- 43.Gress FG, Bhattacharya I. Endoscopic Ultrasonography. Blackwell Science, Inc; 2001. pp. 58–69. [Google Scholar]
- 44.Weill F, Eisenscher A, Aucant D, et al. Ultrasonic study of venous patterns in the right hypochondrium:an anatomical approach to differential diagnosis of obstructive jaundice. J Clin Ultrasound. 1975;3:23–8. doi: 10.1002/jcu.1870030106. [DOI] [PubMed] [Google Scholar]
- 45.Taylor KJW, Carpenter DA. The anatomy and pathology of the portahepatis demonstrated by grayscale ultrasonography. J Clin Ultrasound. 1975;3:117–9. doi: 10.1002/jcu.1870030208. [DOI] [PubMed] [Google Scholar]
- 46.Saddik D, Frazer C, Robins P, et al. Gadolinium-enhanced three-dimensional MR portalvenography. AJR Am J Roentgenol. 1999;172:413–7. doi: 10.2214/ajr.172.2.9930794. [DOI] [PubMed] [Google Scholar]
- 47.Okumura A, Watanabe Y, Dohke M, et al. Contrast-enhanced three-dimensional MR portography. Radio Graphics. 1999;19:973–87. doi: 10.1148/radiographics.19.4.g99jl02973. [DOI] [PubMed] [Google Scholar]
- 48.Zhang L, Duan YY, Li JM, et al. Hemodynamic features of Doppler ultrasonography in patients with portal hypertension: intraoperative direct measurement of portal pressure in the portal venous system. J Ultrasound Med. 2007;26:1689–96. doi: 10.7863/jum.2007.26.12.1689. [DOI] [PubMed] [Google Scholar]
- 49.Palazzo L, Hochain P, Helmer C, et al. Biliary Varices on endoscopic Ultrasonography. Endoscopy. 2000;32:520–4. doi: 10.1055/s-2000-9009. [DOI] [PubMed] [Google Scholar]
- 50.Ikeura T. Characteristic intraductal ultrasonographic features of portal biliopathy. Digest Endosc. 2008;20:213–6. [Google Scholar]
- 51.Sharma M, Mohan P, Rameshbabu CS, et al. Identification of Perforators in Patients with Duodenal Varices by Endoscopic Ultrasound - A Case Series. J Clin Exp Hepatol. 2012;2:229–37. doi: 10.1016/j.jceh.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hommeyer SC, Freeny PC, Crabo LG. Carcinoma of the head of the pancreas: evaluation of the pancreaticoduodenal veins with dynamic CT - potential for improved accuracy in staging. Radiology. 1995;196:233–8. doi: 10.1148/radiology.196.1.7784573. [DOI] [PubMed] [Google Scholar]


