Abstract
The practical use of EUS in small children below the age of 4 years is not described. The aim of the study was to evaluate the feasibility, safety, and clinical utility of smaller caliber echo-bronchoscope in the management of gastrointestinal, pancreatobiliary, and mediastinal disease in children below 4 years. Consecutive children of age younger than 4 years where EUS was clinically considered useful were evaluated by echo-bronchoscopes. The findings showed that EUS by echo-bronchoscopes is feasible and safe in young children.
Keywords: endoscopic ultrasound, endobronchial ultrasound, pancreatobiliary
INTRODUCTION
The indications for simple procedures like upper endoscopy and advanced procedures such as endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound (EUS) in the pediatric age group are similar to those for adult endoscopy.1,2 Adult gastroenterologists perform most of the EUS procedures in the pediatric patients. Lack of a dedicated pediatric EUS scope forces the adult gastroenterologists to use adult EUS scopes in pediatric population. The adult linear EUS scope is however useful only in a subgroup of pediatric age group population, and the usage is limited due to a larger diameter (12-12.8 mm) and difficulty in maneuvering the echoendoscope around the duodenal sweep. Several case reports and series have reported successful use of EUS in pediatric patients for upper gastrointestinal tract tumors, pancreatic disorders, characterization of esophageal strictures, and eosinophilic esophagitis.3,4,5,6,7,8,9 Two case reports have used a smaller-diameter (7.4 mm) echo-bronchoscope in young children to perform EUS.10,11 The utility and feasibility of EUS in pediatric population, especially in infants and young children (< 4 years) are largely unclear. The aim of this case series was to evaluate indications, feasibility, safety, and impact of using the echo-bronchoscope for EUS (EB-EUS)in the pediatric patient population below the age of 4 years.
MATERIALS AND METHODS
All EUS procedures were performed by an experienced endosonographer who has independently performed more than 4000 EUS procedures in adults. Between September 2010 to August 2012, 1800 EUS studies were done, of which 46 were done in pediatric age group (<18 years). In 10 children (6 boys, 4 girls) less than 4 years of age (range 2 months to 4 years), EB-EUS was done by a linear echo-bronchoscope (EUB-1970 UK). The indications for EB-EUS included characterization of esophageal strictures in 3 cases, evaluation of pancreatobiliary tract in 4 cases, evaluation of abdominal cyst in 1 case, liver abscess in 1 case and fine needle aspiration (FNA) cytology of abdominal lymphadenopathy in 1 case. After obtaining, appropriate informed consents procedures were performed on an outpatient basis with moderate conscious sedation in the left lateral decubitus position. The echo-bronchoscope was advanced up to stomach for evaluation of mediastinal diseases and to the duodenum for evaluation of pancreatobiliary disease. As there was no insufflation channel in the echo-bronchoscope, the gastrointestinal lumen was distended after manual insufflation of 50-100 mL of air into stomach by biopsy channel. In 3 patients of recurrent corrosive esophageal strictures who had undergone standard esophageal dilatation more than 5 times in last 1 year, EB-EUS was done after balloon dilation of the esophageal stricture to 9 mm. A 22-G endobronchial ultrasound (EBUS) needle occluded with a stylet (ECHO-HD 22-EBUS-P, Wilson Cook Inc.) was used for FNA in 1 case.
RESULTS
All the procedures were completed successfully without any complication. Introduction of the echoendoscope into stomach was successfully achieved in all cases. The echo-bronchoscope was not advanced to the duodenum in 4 cases: 3 cases of esophageal strictures, and a 2-month old child with choledochal cyst. The average time for procedure was 13.6 min. The results are given in Table 1.
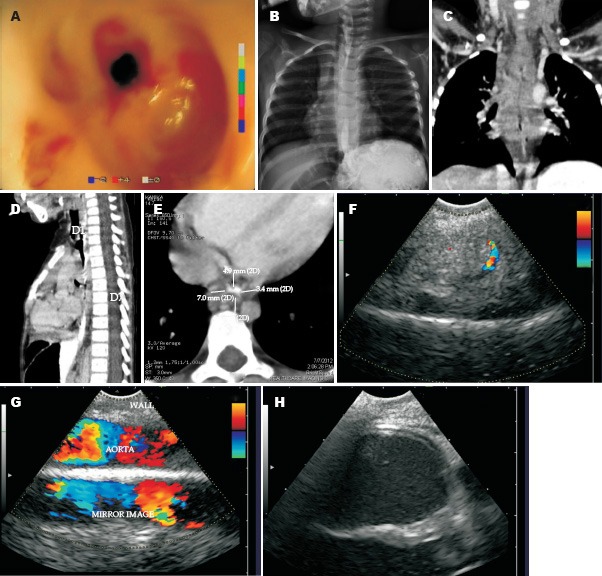
Table 1.
Demographic profile, indication, findings and outcome in 10 cases of EUS by Echo-bronchoscope
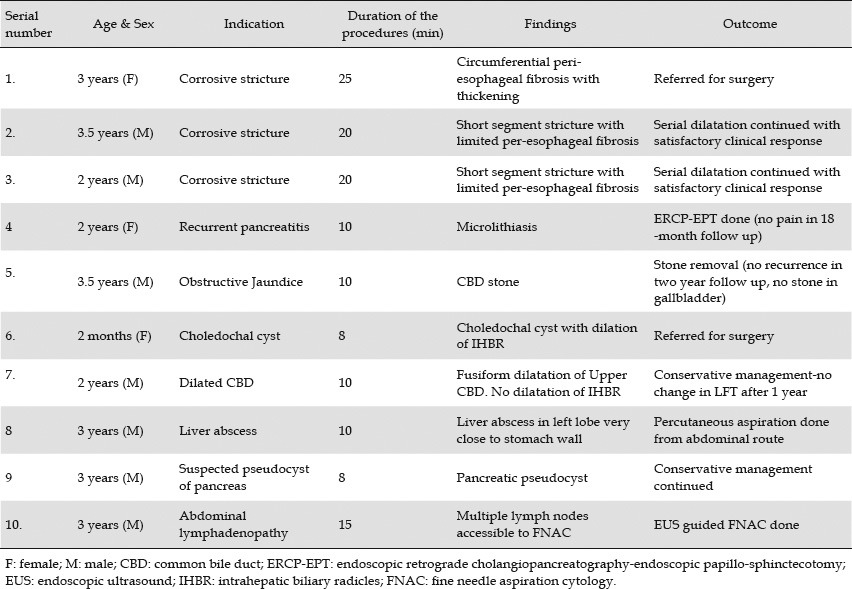
In 3 cases of corrosive stricture of esophagus, EB-EUS showed peri-esophageal thickening. In a 3-year-old child with dysphagia after corrosive ingestion, who had undergone more than 30 sessions of stricture dilatation in last 1 and a half year), peri-esophageal thickening was seen in the entire circumference (Fig. 1 & Video 1). This child was referred for surgery. In 2 cases where endoscopy after dilation had shown a short segment of stricture involving esophagus, EB-EUS showed peri-esophageal thickening only in the lateral wall of esophagus (Fig. 2A, 2B & 2C).
Figure 1.
Endoscopy showed narrowing of lumen (A). A barium swallow showed narrowing of a long segment of mid esophagus (B). Computed tomography scan showed circumferential thickening around the mid part of esophagus (C, D, and E). EB-EUS showed 17 mm thickening of the lateral wall of esophagus, 6 mm thickening of posterior wall esophagus (between probe and aorta) and 6.5 mm thickening of anterior wall of esophagus between probe and left atrium (F, G and H).
Figure 2.

A 2-year-old child had short segment corrosive esophageal stricture requiring repeated dilation. EB-EUS showed a thickening of esophageal wall limited to lateral wall of esophagus. No thickening was seen at the level of left atrium in the anterior wall or in the posterior wall of esophagus.
EB-EUS was done in 4 patients for pancreatobiliary disorders. EB-EUS showed microlithiasis of common bile duct in 1 case (Fig. 3A & Video 2) and common bile duct stone in another (Fig. 3B and Video 3). Computed tomography and magnetic resonance imaging/magnetic resonance cholangiopancreatography (MRI/MRCP) of the bile duct were non-diagnostic in both the cases. The third and fourth patient with pancreatobiliary disorder had choledochal cysts. EB-EUS demonstrated dilated common bile duct of 2 cm in diameter in a 2-month-old child along with dilated intrahepatic biliary radicles (IHBR) and this case was referred for surgery (Video 4). The second patient with choledochal cyst had a fusiform dilation of common bile duct involving the upper part of the bile duct (Fig. 3C and Video 5). This patient had normal liver function tests, which relatively avoided surgery.
Figure 3.
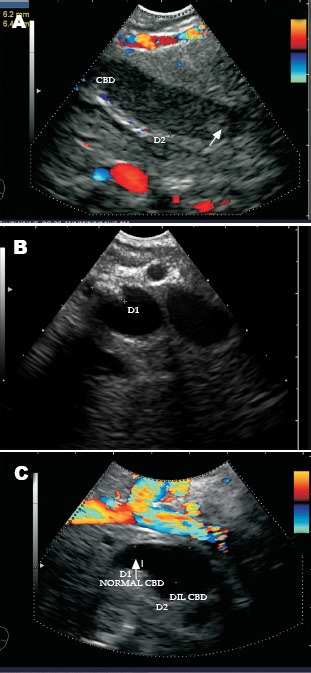
A: A 2-year-old child presented with recurrent abdominal pain and during the episodes of pain amylase levels were high. Ultrasound revealed a bile duct diameter of 6 mm (normal 3 mm for a 2-year-old child). EUS revealed microlithiasis (yellow arrow). Endoscopic sphincterotomy was done. B: A 3.5-year-old child presented with recurrent abdominal pain. Ultrasound revealed a bile duct diameter of 8 mm. Computed tomography scan and magnetic resonance cholangiopancreatography were normal. Endoscopic ultrasound revealed a common bile duct (CBD) stone. Endoscopic sphincterotomy and stone removal was done. C: The 3.5 year old child was referred for evaluation of dilated CBD. EB-EUS showed dilated CBD in the upper part up to the neck of pancreas. The CBD in the intrapancreatic part abruptly narrowed down to a diameter of 5.4 mm. The pancreatic duct was normal.
Abdominal ultrasound revealed an abscess in the left lobe of liver in 1 child 2 cm away from the surface of liver. The radiologist wanted to look for a shorter window for aspiration. EB-EUS showed that the abscess was only 3 mm away from the wall of the stomach (Fig. 4A). In absence of availability of a thick needle for EB-EUS-guided aspiration, a percutaneous aspiration was done. It resulted in shrinkage of the size of the abscess, and on a repeat EB-EUS the abscess wall had moved 1 cm away from the wall of the stomach (Fig. 4B).
Figure 4.
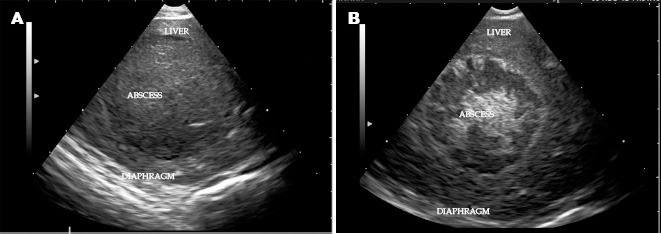
A: A 3-year-old child presented with complain of pain in abdomen. Ultrasound revealed an abscess in left lobe of liver 2 cm away from the surface. EB-EUS showed that the abscess was only 3 mm away from the stomach wall. B: After aspiration the wall of the abscess had moved 1 cm away from the wall of the stomach.
EB-EUS showed a cyst with mature cyst wall related to head of the pancreas in a child who had a history of blunt injury of abdomen 3 months back (Fig. 5A & 5B). Possible consideration was given to surgical intervention, but conservative management resulted in resolution of the cyst in 4 months. In the final case, multiple enlarged lymph nodes inaccessible for percutaneous aspiration or biopsy were seen near the abdominal aorta. EB-EUS demonstrated the presence of lymph nodes posterior to pancreas and anterior to aorta (Fig. 1F & Fig. 6A). EB-EUS-FNA cytology was done by EBUS needle (Fig. 6B). EB-EUS-FNA cytology revealed features of Hodgkin's lymphoma. Immunocytochemical markers were positive for CD15 and CD30, and the child was referred to pediatric oncology unit (Fig. 6A, 6B & 6C and Video 6).
Figure 5.
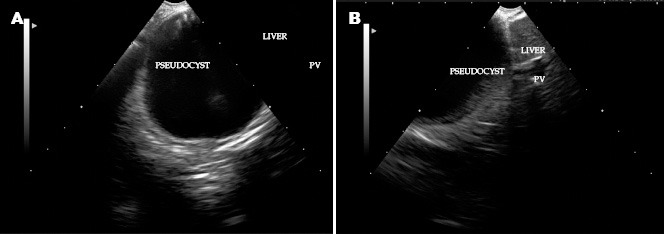
A three year old child had history of blunt injury of abdomen. The computed tomography (CT) scan and magnetic resonance imaging (MRI) has shown a cyst located between the liver and pancreas. The exact origin and nature of the cyst was suggested to be from pancreatic origin by CT scan and MRI. EB-EUS supplemented by providing the information that the cyst was related to pancreas.
Figure 6.
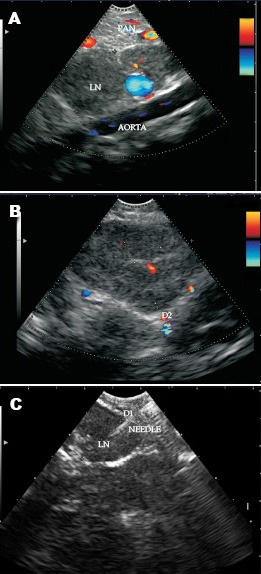
A, B: A three year old child presented with pyrexia of unknown origin. Investigations revealed lymphadenopathy only in the para aortic region. The lymph nodes were seen lying anterior to aorta and posterior to pancreas on EB-EUS. C: An EB-EUS guided fine needle aspiration cytology was done from the para-aortic lymph node.
DISCUSSION
Our case series shows that EB-EUS is safe, successful and feasible in the pediatric patient population below the age of 4 years. The use of standard adult EUS scopes can be limited in pediatric population. The limitation can arise from multiple factors. Besides the large external diameter, another factor to consider is the difficulty of passage of an adult echoendosocpe across the oro-pharynx and maneuvering around the duodenal sweep. Due to the size of the transducer and limited flexibility of the tip of the echoendoscope, this can be restricted. In our series, because of the small caliber of the echoendoscope and higher flexibility of the tip, these limitations were easily overcome.
EB-EUS evaluation provided a definite diagnosis in 2 cases with microlithiasis and common bile duct stones. The diameter of common bile duct in these 2 children was more than normal (~3.3 mm). EB-EUS allowed a definite diagnostic evaluation by FNA cytology in 1 case of abdominal lymphadenopathy and suggested long-term management in 3 cases of esophageal stricture12. In 1 case of liver abscess, EB-EUS guided aspiration was considered because of close proximity of abscess (<5mm) to the wall of stomach, but a satisfactory window ultimately allowed easy aspiration from the percutaneous route. In 1 case of pancreatic cyst, the findings on EB-EUS collaborated with computed tomography and MRI findings.
Although the usefulness of EUS in children has been only recently appreciated, published studies remain limited to a few patients and single center experiences.3,4,5,6,7,8 The current series illustrates the experience of EB-EUS at a large volume, single center with 10 children from 2 months age to 4 years for management of pediatric pathologies involving the gastrointestinal tract, pancreatobiliary system, and mediastinum. The average duration of procedure was less than 15 min and the information obtained helped in ultimate management.
In the present series of pediatric EB-EUS, we found this modality to have multiple advantages. All of the procedures were performed on an outpatient basis and EB-EUS may prove to be preferable to MRI, especially if it is easier to obtain, more affordable, and/or better tolerated. This may open the door to the possibility of replacing MRI studies with EB-EUS studies, or at least, using the two modalities to maximize the information obtained in a particular patient and to avoid more invasive interventions. In conclusion, EB-EUS appears to be a feasible and safe technique in children and provides clinically useful information with a significant impact on the management of gastrointestinal, pancreatobiliary and mediastinal diseases. It is a promising technology, but is used infrequently in children. Larger studies are needed to further evaluate a more widespread role for EB-EUS in the assessment of young children.
REFERENCES
- 1.Squires RH. Indications for pediatric gastrointestinal endoscopy: a medical position statement of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr. 1996;23:107–10. doi: 10.1097/00005176-199608000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Lee KK. Endoscopy. In: Osborn LM, DeWitt TG, First LR, et al., editors. Pediatrics. Philadelphia: Elsevier Mosby; 2005. pp. 1750–6. [Google Scholar]
- 3.Lee KK. Modifications in endoscopic practice for pediatric patients. Gastrointest Endosc. 2008;67:1–9. doi: 10.1016/j.gie.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Roseau G. Endoscopic ultrasonography in the evaluation of pediatric digestive diseases: preliminary results. Endoscopy. 1998;30:477–81. doi: 10.1055/s-2007-1001311. [DOI] [PubMed] [Google Scholar]
- 5.Varadarajulu S. Impact of EUS in the evaluation of pancreaticobiliary disorders in children. Gastrointest Endosc. 2005;62:239–44. doi: 10.1016/s0016-5107(05)00312-3. [DOI] [PubMed] [Google Scholar]
- 6.Cohen S. Endoscopic ultrasonography in pediatric patients with gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2008;46:551–4. doi: 10.1097/MPG.0b013e31815ce571. [DOI] [PubMed] [Google Scholar]
- 7.Fox VL. High-resolution EUS in children with eosinophilic “allergic” esophagitis. Gastrointest Endosc. 2003;57:30–6. doi: 10.1067/mge.2003.33. [DOI] [PubMed] [Google Scholar]
- 8.Nadler EP. The use of endoscopic ultrasound in the diagnosis of solid pseudopapillary tumors of the pancreas in children. J Pediatr Surg. 2002;37:1370–3. doi: 10.1053/jpsu.2002.35028. [DOI] [PubMed] [Google Scholar]
- 9.Usui N. Usefulness of endoscopic ultrasonography in the diagnosis of congenital esophageal stenosis. J Pediatr Surg. 2002;37:1744–6. doi: 10.1053/jpsu.2002.36711. [DOI] [PubMed] [Google Scholar]
- 10.Faigel DO. The role of endoscopic ultrasound in the evaluation and management of foregut duplications. Gastrointest Endosc. 1997;45:99–103. doi: 10.1016/s0016-5107(97)70315-8. [DOI] [PubMed] [Google Scholar]
- 11.Sharma M. Dead worm in common bile duct. Trop Gastroenterol. 2011;32:343–5. [PubMed] [Google Scholar]
- 12.Sharma M. Picture of the month. Recurrent biliary colic in a young girl. Arch Pediatr Adolesc Med. 2011;165:957. doi: 10.1001/archpediatrics.2011.156-a. [DOI] [PubMed] [Google Scholar]
- 13.Rana SS. Education and imaging. Gastrointestinal: endoscopic ultrasonography (EUS) in corrosive esophageal stricture. J Gastroenterol Hepatol. 2010;25:840. doi: 10.1111/j.1440-1746.2010.06314.x. [DOI] [PubMed] [Google Scholar]
- 14.Hernanz-Schulman M. Common bile duct in children: sonographic dimensions. Radiology. 1995;195:193–5. doi: 10.1148/radiology.195.1.7892467. [DOI] [PubMed] [Google Scholar]


