A epigastric mass was found on examination in a 67-year-old woman with abdominal pain and 10 kg weigth loss for the past 6 months. Abdominal computed tomography (CT) showed a mass in the pancreatic head and uncinated process, with a cystic central area, irregular bounds and a central small calcification. The contrast demonstrated invasion of the spleno-portal junction and superior mesenteric vein and a half circumference contact with superior mesenteric artery. The mass was 6.8 cm × 5.8 cm × 5 cm. There was, also, a possible mesenteric fat invasion, with some normal size lymph nodes and a dilatation of the proximal portion of the main pancreatic duct (Fig.1).
Figure 1.
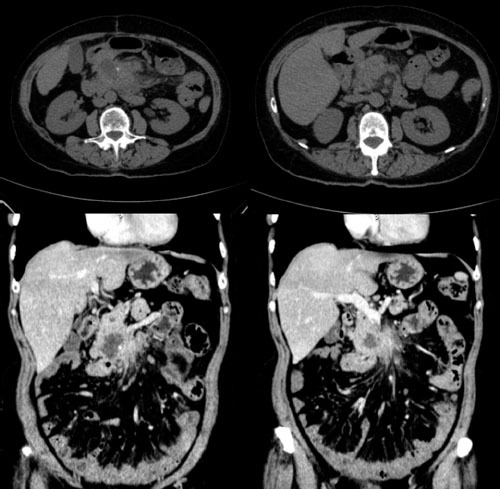
Computed tomography images of the pancreatic lesion.
She underwent an right hemicolectomy 6 years ago and made an uneventful recovery. Colonoscopy showed ileocolic anastomosis without lesions. Endoscopic ultrasound (EUS) showed a hypoechoic heterogeneous lesion in the head and uncinated process of the pancreas with hyperechoic central area and well-defined limits, measuring 4 cm × 4 cm, infiltrating gastric antral mucosa and vascular structures (portal vein and superior mesenteric artery). Main pancreatic duct was dillated (4.8 mm). There was peri-pancreatic, homogeneous, well-limited lymph nodes, measuring more than 1 cm (Fig. 2A, 2B, and 2C). EUS-guided fine needle aspiration (EUS-FNA) was performed with a 22-G EchoTip® needle (Cook Medical Inc, Limerick, Ireland) and a sufficient cytology material was obtained after 3 needle passes. The slides were stained and analyzed by an on-site cytopathologist, showing a suspicious material for malignancy (Fig. 3A). The cell block histology (Fig. 3B) and immunohistochemistry (Fig. 4A, 4B, and 4C) confirmed the diagnosis of pancreatic metastasis from colon carcinoma.
Figure 2.

Endoscopic ultrasound view of a hypoechoic and heterogeneous lesion in the head and uncinated process of the pancreas (A), main pancreatic duct with 4.8mm (B) and peri-pancreatic lymph nodes (C).
Figure 3.
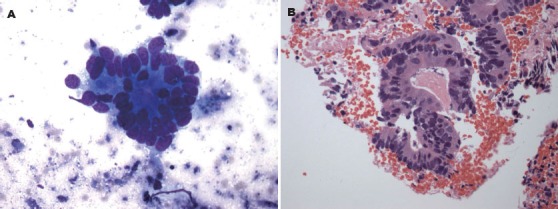
Rapid on-site cytopathological evaluation demonstrating a suspicious material for malignancy (A) and histological section (Hematoxylin and Eosin stain) showing pancreatic metastasis from colon carcinoma (B).
Figure 4.
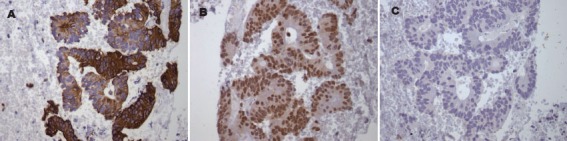
Histological sections (Immunohistochemistry) showing positive staining for CK20 (A), CDX2 (B) and negative staining for CK7 (C).
Pancreatic masses remains a diagnostic challenge, even with all procedure enhancements. All the efforts are done to make a preoperative diagnosis, reducing the morbi-mortality of unnecessary surgical procedures. Many different histological kind of lesions, with different treatments, make tissue acquisition almost mandatory to define the sequence of procedures. In some cases, resection procedures are feasible and in others, only chemotherapy should be considered.
Pancreatic metastasis from colon carcinoma is rare and accounts for less than 2% of all pancreatic metastases.[1,2] More frequent metastases to the pancreas are from kidney cell carcinoma, lung cancer, breast cancer and melanoma. The median interval for colorectal metastasis to the pancreas was found to be 24 months.[3] EUS-FNA has been reported as a safe and minimally invasive method for diagnosing non-primary neoplasms. An accurate diagnosis is facilitated by careful evaluation of the clinical history, cytology and histopathological study including immunohistochemistry.[1,4] The role of treatment for metastatic colorectal tumors to the pancreas is not well-defined due to a paucity of such cases reported in the literature, with possible surgical resection or chemotherapy. Thus, in this case, we showed a rare case of pancreatic metastasis, diagnosed by EUS-FNA, from colon carcinoma 6 years after a hemicolectomy.
REFERENCES
- 1.Machado NO, Chopra P. Pancreatic metastasis from renal carcinoma managed by Whipple resection. A case report and literature review of metastatic pattern, surgical management and outcome. JOP. 2009;10:413–8. [PubMed] [Google Scholar]
- 2.Pereira-Lima JC, Coral GP, Bayer LR, et al. Metastasis from colon carcinoma in the dorsal pancreas of a patient with pancreas divisum: report of a case. Hepatogastroenterology. 2000;47:554–5. [PubMed] [Google Scholar]
- 3.Sperti C, Pasquali C, Berselli M, et al. Metastasis to the pancreas from colorectal cancer: is there a place for pancreatic resection? Dis Colon Rectum. 2009;52:1154–9. doi: 10.1007/DCR.0b013e31819f7397. [DOI] [PubMed] [Google Scholar]
- 4.Baierlein SA, Wistop A, Looser C, et al. Primary pancreatic neoplasia or metastasis from colon carcinoma? Acta Gastroenterol Belg. 2008;71:401–8. [PubMed] [Google Scholar]


