Abstract
Heterotopic pancreas is usually asymptomatic and does not change throughout the patient's life, but sometimes it can present symp-toms and complications, which are rarely discrete in the literature. We present here a case of heterotopic pancreas in the gastric wall complicated with pseudocyst, and suggest that heterotopic pancreatic pseudocyst should be included in the differential diagnosis of gastric wall cysts.
Keywords: heterotopic pancreas, pseudocyst, gastric wall cyst, pancreatic cyst, endoscopic ultrasound, fine needle aspiration
INTRODUCTION
The term heterotopic pancreas is used to describe ectopic pancreatic tissue lying outside its normal location with no anatomic or vascular connection to the pancreas.1 These lesions are also termed ectopic pancreas, pancreatic rest, or aberrant pancreas. They are typically discovered incidentally during endoscopy, surgery, or autopsy.2 Its prevalence varies from 0.55% to 13.7%.3,4,5
The main location of heterotopic pancreas is in the stomach wall (frequently along the greater curvature of the antrum). Other locations are described in the literature: Duodenum, small intestine, or anywhere in the gastrointestinal tract.6
Endoscopic ultrasound (EUS) features of heterotopic pancreas are heterogeneous lesions, mainly hypoechoic or intermediate echogenic masses accompanied by scattered small hyperechoic areas, with indistinct margins within the gut wall. They commonly arise from the third and fourth layers.7
Usually, these lesions are asymptomatic and they do not change throughout the patient's life, but sometimes they can present symptoms. Complications are rarely described in the literature. This case report presents a case of heterotopic pancreas in the gastric wall, complicated by pseudocyst.
CASE REPORT
A 42-year-old male with chronic pancreatitis due to alcohol abuse presented with recurrent pain in the upper abdomen for the last 8 years, and progressive deterioration with the loss of 4 kg over the past 6 months. Other diseases are type 2 diabetes mellitus and exocrine pancreatic insufficiency. He takes pancreatic enzymes, insulin and omeprazole. On physical examination, the patient is emaciated and has pain in the epigastric region, with no palpable masses.
In endoscopic examination performed to investigate abdominal pain, subepithelial lesion was found in the lesser curvature of the gastric body with normal mucosa. Patient was referred to perform EUS.
EUS showed a cystic lesion of the gastric wall measuring 35 mm × 13 mm (Fig. 1), originating from the third layer, with anechoic contents and debris. Besides this, during the pancreatic EUS, heterogeneous pancreatic parenchyma and two cysts in the cephalic portion of the pancreas were accidentally found (Figs. 2 and 3). We perform fine-needle aspiration on the gastric wall cyst and also on the pancreatic head cyst. After emptying the gastric cyst, we observed a hypoechoic, heterogeneous residual lesion, with hyperechoic dots, suggestive of heterotopic pancreas in the third layer of the gastric wall. The material was sent for biochemical analysis, cytology, “cell block”, and bacteriological evaluation.
Figure 1.
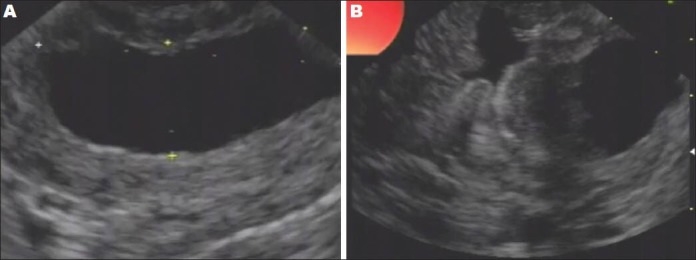
A and B: Endoscopic ultrasound shows a cystic lesion of the gastric wall
Figure 2.

Endoscopic ultrasound shows the function of the cystic lesion
Figure 3.

Endoscopic ultrasound shows the cystic lesion after the function
The biochemical analysis of the content of the gastric wall cystic lesion showed amylase 62.075 U/L and carcinoembryonic antigen (CEA) 253.2 ng/mL and the content of the pancreatic cyst presented amylase 53.464 U/L and CEA 77.7 ng/mL. Both analyses showed negative neoplastic cells and negative cultures.
After 3 weeks, patient continued to have abdominal pain and EUS re-evaluation of the gastric wall cyst shows the same characteristics as the first EUS, therefore, the final diagnosis was heterotopic pancreas with pseudocyst. The patient was treated with analgesics and continued to take pancreatic enzymes responding well to treatment, thus; no surgery was performed.
DISCUSSION
Patients with heterotopic pancreas are usually asymptomatic, but literature described rare complications such as pancreatitis, ulceration, bleeding, gastric outlet obstruction, obstructive jaundice, malignancy and pseudocyst formation.6,8,9,10
Pseudocyst formation in heterotopic pancreas could result from retention of exocrine secretions in the absence of a communication between the glandular epithelium and the gastric lumen.11 Furthermore, the accumulation of pancreatic secretions can lead to recurrent episodes of acute obstructive pancreatitis and the formation of retention pseudocysts.12
In our case, the patient also showed changes in the pancreatic parenchyma caused by the toxic effect of alcohol. We believe that toxicity in pancreatic parenchyma caused by the effect of alcohol may have occurred in ectopic pancreatic tissue and led to the formation of the pseudocyst. In other studies, pathological examination of cystic lesions shows dilated ducts forming the pseudocysts and intense inflammation intermingled with heterotopic pancreas.13,14,15
Cizginer et al.16 presents an optimal cutoff value of CEA 109.9 ng/mL, with 86% accuracy in predicting the mucinous cyst (P < 0.0001). However, other studies have cut of values for CEA 400 ng/mL and 800 ng/mL with specificity of 100% and 98% respectively in predicting mucinous cyst.17,18 In this case, CEA 253.2 ng/mL was below 400 ng/mL.
The cell block evaluation of the cystic lesion in the gastric wall was negative for neoplasia. The specificity varies from 55%19 to 97%20 for differentiating benign from malignant or potentially malignant pancreatic cystic lesions, and sensitivity of cytology is controversial in the literature.
Almost all complications of heterotopic pancreas described in literature were treated with surgery.8,9,10 Our patient has some comorbidities that increase the surgical risk, and we opted for conservative treatment.
In conclusion, the heterotopic pancreas tissue can be affected by the same changes of the pancreatic parenchyma and may have complications such as pseudocyst formation. Heterotopic pancreatic pseudocyst should be included in the differential diagnosis of gastric wall cysts.
REFERENCES
- 1.Kim EY. Sumucosal lesions. In: Hawes RH, Fockens P, Varandarajulu S, editors. Endosonography. 2nd ed. Philadelphia: Saunders; 2011. pp. 84–96. [Google Scholar]
- 2.Armstrong CP, King PM, Dixon JM, et al. The clinical significance of heterotopic pancreas in the gastrointestinal tract. Br J Surg. 1981;68:384–7. doi: 10.1002/bjs.1800680606. [DOI] [PubMed] [Google Scholar]
- 3.Thoeni RF, Gedgaudas RK. Ectopic pancreas: Usual and unusual features. Gastrointest Radiol. 1980;5:37–42. doi: 10.1007/BF01888597. [DOI] [PubMed] [Google Scholar]
- 4.Pang LC. Pancreatic heterotopia: A reappraisal and clinicopathologic analysis of 32 cases. South Med J. 1988;81:1264–75. [PubMed] [Google Scholar]
- 5.Marshall SF, Curtiss FM. Aberrant pancreas in stomach wall. Surg Clin North Am. 1952;32:867–75. doi: 10.1016/s0039-6109(16)33650-7. [DOI] [PubMed] [Google Scholar]
- 6.Jovanovic I, Knezevic S, Micev M, et al. EUS mini probes in diagnosis of cystic dystrophy of duodenal wall in heterotopic pancreas: A case report. World J Gastroenterol. 2004;10:2609–12. doi: 10.3748/wjg.v10.i17.2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matsushita M, Hajiro K, Okazaki K, et al. Gastric aberrant pancreas: EUS analysis in comparison with the histology. Gastrointest Endosc. 1999;49:493–7. doi: 10.1016/s0016-5107(99)70049-0. [DOI] [PubMed] [Google Scholar]
- 8.Surov A, Hainz M, Hinz L, et al. Case report: Ectopic pancreas with pseudocyst and pseudoaneurysm formation. Clin Radiol. 2009;64:734–7. doi: 10.1016/j.crad.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 9.Schmitz H, Spelsberg F, Janson M. Heterotopic pancreatic cyst of the stomach wall. Leber Magen Darm. 1991;21:33–5. [PubMed] [Google Scholar]
- 10.Eisenberger CF, Kropp A, Langwieler TE, et al. Heterotopic pancreatitis: Gastric outlet obstruction due to an intramural pseudocyst and hamartoma. Z Gastroenterol. 2002;40:259–62. doi: 10.1055/s-2002-25146. [DOI] [PubMed] [Google Scholar]
- 11.Mulholland KC, Wallace WD, Epanomeritakis E, et al. Pseudocyst formation in gastric ectopic pancreas. JOP. 2004;5:498–501. [PubMed] [Google Scholar]
- 12.Galloro G, Napolitano V, Magno L, et al. Diagnosis and therapeutic management of cystic dystrophy of the duodenal wall in heterotopic pancreas. A case report and revision of the literature. JOP. 2008;9:725–32. [PubMed] [Google Scholar]
- 13.Yen HH, Soon MS, Soon A. Heterotopic pancreas presenting as gastric submucosal cyst on endoscopic sonography. J Clin Ultrasound. 2006;34:203–6. doi: 10.1002/jcu.20184. [DOI] [PubMed] [Google Scholar]
- 14.Claudon M, Verain AL, Bigard MA, et al. Cyst formation in gastric heterotopic pancreas: Report of two cases. Radiology. 1988;169:659–60. doi: 10.1148/radiology.169.3.3055030. [DOI] [PubMed] [Google Scholar]
- 15.Fléjou JF, Potet F, Molas G, et al. Cystic dystrophy of the gastric and duodenal wall developing in heterotopic pancreas: An unrecognised entity. Gut. 1993;34:343–7. doi: 10.1136/gut.34.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cizginer S, Turner BG, Bilge AR, et al. Cyst fluid carcinoembryonic antigen is an accurate diagnostic marker of pancreatic mucinous cysts. Pancreas. 2011;40:1024–8. doi: 10.1097/MPA.0b013e31821bd62f. [DOI] [PubMed] [Google Scholar]
- 17.Hammel P, Voitot H, Vilgrain V, et al. Diagnostic value of CA 72-4 and carcinoembryonic antigen determination in the fluid of pancreatic cystic lesions. Eur J Gastroenterol Hepatol. 1998;10:345–8. doi: 10.1097/00042737-199804000-00012. [DOI] [PubMed] [Google Scholar]
- 18.van der Waaij LA, van Dullemen HM, Porte RJ. Cyst fluid analysis in the differential diagnosis of pancreatic cystic lesions: A pooled analysis. Gastrointest Endosc. 2005;62:383–9. doi: 10.1016/s0016-5107(05)01581-6. [DOI] [PubMed] [Google Scholar]
- 19.Brandwein SL, Farrell JJ, Centeno BA, et al. Detection and tumor staging of malignancy in cystic, intraductal, and solid tumors of the pancreas by EUS. Gastrointest Endosc. 2001;53:722–7. doi: 10.1067/mge.2001.114783. [DOI] [PubMed] [Google Scholar]
- 20.Frossard JL, Amouyal P, Amouyal G, et al. Performance of endosonography-guided fine needle aspiration and biopsy in the diagnosis of pancreatic cystic lesions. Am J Gastroenterol. 2003;98:1516–24. doi: 10.1111/j.1572-0241.2003.07530.x. [DOI] [PubMed] [Google Scholar]


