Abstract
Utility of endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) for diagnosis of metastatic mediastinal lymph node (MLN) following an unproductive computed tomography (CT) guided-biopsy in a patient with cervical cancer. A 35-year-old woman with locally invasive cervical cancer was found to have a suspicious paraesophageal posterior MLN during the preliminary staging. Mediastinal metastasis from cervical cancer has been rarely reported. Mediastinal CT-guided-biopsy was non-diagnostic. Hence, patient underwent EUS guided-FNA of MLN confirming metastatic cervical cancer. Cervical cancer metastasis to MLN is rare. EUS can be safely and effectively used for FNA from paraesophageal lymph nodes.
Keywords: metastatic cervical cancer, endosonography, endoscopic ultrasound, fine needle aspiration, mediastinal lymph nodes, computed tomography-guided biopsy
INTRODUCTION
Cancer of the cervix and uterus has the fourth highest incidence of all types of invasive cancers among women in the United States.1 According to the recent Surveillance epidemiology and end results database, the age-adjusted incidence rate of cervical cancer cases is about 8.1/100,000 women/year.2 Lymph node involvement is the most important prognostic factor that plays a key role in determining the therapeutic approach. Mediastinal lymph node (MLN) metastasis is rare and when unrecognized can lead to inadequate treatment of such patients.3
CASE REPORT
This was a case report of a 35-year-old Asian female patient who presented with irregular menstrual bleeding was diagnosed with moderately differentiated squamous cell cervical carcinoma and referred to a tertiary cancer center for continued management. Staging positron emission tomography-computed tomography (PET/CT) scan demonstrated hypermetabolic primary cervical mass with markedly enlarged lymphadenopathy within the external iliac, common iliac and left paraaortic nodes. A soft-tissue density in the posterior mediastinum with standard uptake value of 5.2 was presumed as paraesophageal lymphadenopathy (Fig. 1). Magnetic resonance imaging (MRI) showed a parametrial extension of the cervical cancer. A CT-guided biopsy of the presumed paraesophageal lymph node was performed (Fig. 2), but on cytology neither lymphatic tissue nor cancer cells were identified. A linear echoendoscope (GF-UC140P-AL5 Olympus America, Center Valley, PA, USA) was used for the procedure. At 26 cm from the incisors, a 23 mm × 6 mm oval shaped, hypoechoic, well demarcated, paraesophageal lymph node was identified in the posterior mediastinum. The endoscopic ultrasound (EUS) appearance was suggestive of two adjoining lymph nodes rather than one single node. Trans-esophageal EUS-guided fine needle aspiration (FNA) was performed with a 25-guage needle (Cook Medical) thorough an avascular window (Fig. 3). A total of two passes were performed and an adequate tissue acquisition was confirmed. Cytology was diagnostic and revealed presence of squamous cancer cells in a background of lymphatic tissue. Subsequently, patient was started on the systemic chemotherapy followed by intensity modulated radiotherapy (IMRT) to the paraaortic region. In the absence of mediastinal metastasis, management would have started with IMRT.
Figure 1.
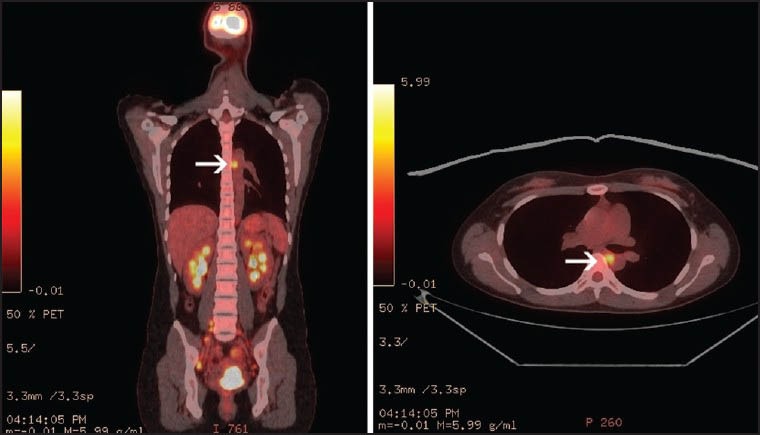
Positron emission tomography-computed tomography scan demonstrated hypermetabolic primary cervical mass. A softtissue density in the posterior mediastinum with standard uptake value of 5.2 presumed as paraesophageal posterior mediastinal lymphadenopathy (white arrow)
Figure 2.
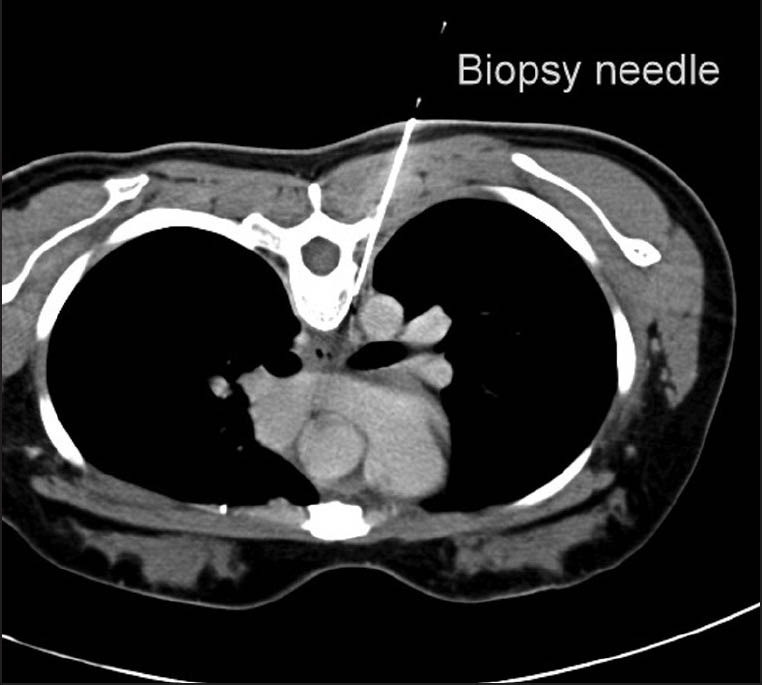
Computed tomography guided biopsy of paraesophageal posterior mediastinal lymphadenopathy
Figure 3.
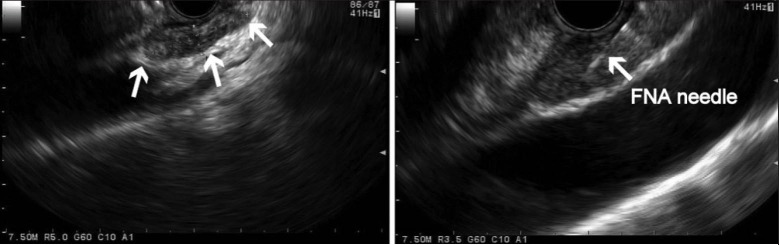
Endoscopic ultrasound: At 26 cm from the incisors, a 23 mm × 6 mm oval shaped, hypoechoic, well-demarcated, paraesophageal lymph node (white arrows) was identified in the posterior mediastinum. Fine needle aspiration was completed using a 25-gauge needle. A total of two transesophageal needle passes through an avascular area were performed
DISCUSSION
Uterine cervical cancer is the fourth most common cancer among women.1 The cancer spreads to surrounding tissue by direct infiltration and later to distant sites by lymphatic and hematogenous routes. Lymphatics from the cervix lead to the common iliac nodes from where tumor can spread to the abdominal paraaortic nodes and beyond.4 Cross-sectional imaging methods are suitable for displaying anatomical abnormalities suggestive of infiltration, but are less accurate for assessing metastases within the normal sized lymph nodes.3,5 The use of PET/CT has been demonstrated to be better than CT and MRI for detecting metastatic lymph nodes in patients with cervical cancer.6 MLN and hilar lymph node metastasis from untreated cervical cancer has rarely been described. The only case series was published two decades ago in 7 of 62 patients who presented with extensive disease during a 5-year period at a tertiary care center.7 To the best of our knowledge, this is the first report of uterine cervical cancer metastases to MLN diagnosed by EUS-FNA. This is also the first report where for similar reasons, CT-guided biopsy was non-diagnostic and subsequent EUS-FNA was not only easy to perform but also diagnostic, ensuing change in management of the patient.
Diagnostic trans-esophageal EUS-FNA is indicated for mediastinal lymphadenopathy of non-pulmonary etiology. Various cancers can metastasize to the posterior MLNs. Non-pulmonary MLN metastases diagnosed by EUS-FNA include primary cancers from breast, colon, renal, testicular, laryngeal, pancreas and esophagus.8,9 Although previous EUS studies have described the morphology of malignant lymph nodes as having a round shape, size >1 cm, hypoechoic echotexture and well-defined borders, EUS with FNA has markedly improved sensitivity and specificity for malignant lymphadenopathy.10,11 A meta-analysis of 76 studies comparing EUS and EUS-FNA for the diagnosis of mediastinal lymphadenopathy revealed a high pooled specificity (EUS: 85%; EUS-FNA: 96%).12 Furthermore, EUS-FNA of posterior mediastinal lesions is extremely safe. Rarely reported complications include, mediastinitis after aspiration of cysts13 and a single report of the esophageal wall tumor-seeding from a primary gastric cancer.14
For identification of MLN metastases, EUS-FNA and PET have similar sensitivity (~85%) and specificity (~90%).15,16 Tissue verification of PET-positive lymph nodes should ensue for confirmation. The combination of PET and EUS-FNA improves overall specificity and accuracy compared with PET alone.17 Both EUS alone and EUS-FNA are more accurate than CT alone (using nodal diameter >10 mm) in ascertaining posterior MLN metastasis.18 There are no comparative studies between EUS-FNA and CT-guided biopsy for malignant lymphadenopathy. For MLN, the multiplanar capability of EUS allows an oblique approach if required; besides the continuous visualization of the FNA-needle prevents puncture of vascular structures. Furthermore, the overall time for the procedure is approximately 15 min and esophageal needle puncture is painless and less traumatic.19 In comparison, CT is limited somewhat by scan thickness induced volume effects, soft-tissue-air interface generated streak artifacts in the main airways and high risk of pneumothorax (25%-43%).20
CONCLUSION
EUS-FNA is a valuable procedure, providing for easy, definitive tissue acquisition in suspected posterior MLN metastatic disease from a non-thoracic primary cancer. In addition, EUS-FNA tissue diagnosis can avoid supplemental invasive procedures and contribute in the formulation of appropriate oncological treatment.
REFERENCES
- 1.Atlanta: U.S. Department of Health and Human Services; 2010. United States Cancer Statistics: 1999-2007 Incidence and Mortality Web-based Report. US Cancer Statistics Working Group. Vol. 2010. [Google Scholar]
- 2.Howlader N, Noone AM, Krapcho M, et al. Bethesda, MD: National Cancer Institute; [based on November 2011 SEER data submission, posted to the SEER web site, April 2012]. SEER Cancer Statistics Review, 1975-2009 (Vintage 2009 Populations) Available from: http://seer.cancer.gov/csr/1975_2009_pops09 . [Google Scholar]
- 3.Hertel H, Köhler C, Elhawary T, et al. Laparoscopic staging compared with imaging techniques in the staging of advanced cervical cancer. Gynecol Oncol. 2002;87:46–51. doi: 10.1006/gyno.2002.6722. [DOI] [PubMed] [Google Scholar]
- 4.Park JM, Charnsangavej C, Yoshimitsu K, et al. Pathways of nodal metastasis from pelvic tumors: CT demonstration. Radiographics. 1994;14:1309–21. doi: 10.1148/radiographics.14.6.7855343. [DOI] [PubMed] [Google Scholar]
- 5.Marnitz S, Köhler C, Roth C, et al. Is there a benefit of pretreatment laparoscopic transperitoneal surgical staging in patients with advanced cervical cancer? Gynecol Oncol. 2005;99:536–44. doi: 10.1016/j.ygyno.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Dargent D, Ansquer Y, Mathevet P. Technical development and results of left extraperitoneal laparoscopic paraaortic lymphadenectomy for cervical cancer. Gynecol Oncol. 2000;77:87–92. doi: 10.1006/gyno.1999.5585. [DOI] [PubMed] [Google Scholar]
- 7.Shin MS, Shingleton HM, Partridge EE, et al. Squamous cell carcinoma of the uterine cervix. Patterns of thoracic metastases. Invest Radiol. 1995;30:724–9. doi: 10.1097/00004424-199512000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Devereaux BM, Leblanc JK, Yousif E, et al. Clinical utility of EUS-guided fine-needle aspiration of mediastinal masses in the absence of known pulmonary malignancy. Gastrointest Endosc. 2002;56:397–401. doi: 10.1016/s0016-5107(02)70045-x. [DOI] [PubMed] [Google Scholar]
- 9.Kramer H, Koëter GH, Sleijfer DT, et al. Endoscopic ultrasound-guided fine-needle aspiration in patients with mediastinal abnormalities and previous extrathoracic malignancy. Eur J Cancer. 2004;40:559–62. doi: 10.1016/j.ejca.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Catalano MF, Sivak MV, Jr, Rice T, et al. Endosonographic features predictive of lymph node metastasis. Gastrointest Endosc. 1994;40:442–6. doi: 10.1016/s0016-5107(94)70206-3. [DOI] [PubMed] [Google Scholar]
- 11.Chen VK, Eloubeidi MA. Endoscopic ultrasound-guided fine needle aspiration is superior to lymph node echofeatures: A prospective evaluation of mediastinal and peri-intestinal lymphadenopathy. Am J Gastroenterol. 2004;99:628–33. doi: 10.1111/j.1572-0241.2004.04064.x. [DOI] [PubMed] [Google Scholar]
- 12.Puli SR, Batapati Krishna Reddy J, Bechtold ML, et al. Endoscopic ultrasound: It's accuracy in evaluating mediastinal lymphadenopathy? A meta-analysis and systematic review. World J Gastroenterol. 2008;14:3028–37. doi: 10.3748/wjg.14.3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diehl DL, Cheruvattath R, Facktor MA, et al. Infection after endoscopic ultrasound-guided aspiration of mediastinal cysts. Interact Cardiovasc Thorac Surg. 2010;10:338–40. doi: 10.1510/icvts.2009.217067. [DOI] [PubMed] [Google Scholar]
- 14.Doi S, Yasuda I, Iwashita T, et al. Needle tract implantation on the esophageal wall after EUS-guided FNA of metastatic mediastinal lymphadenopathy. Gastrointest Endosc. 2008;67:988–90. doi: 10.1016/j.gie.2007.10.025. [DOI] [PubMed] [Google Scholar]
- 15.LeBlanc JK, Ciaccia D, Al-Assi MT, et al. Optimal number of EUS-guided fine needle passes needed to obtain a correct diagnosis. Gastrointest Endosc. 2004;59:475–81. doi: 10.1016/s0016-5107(03)02863-3. [DOI] [PubMed] [Google Scholar]
- 16.Tournoy KG, Praet MM, Van Maele G, et al. Esophageal endoscopic ultrasound with fine-needle aspiration with an on-site cytopathologist: High accuracy for the diagnosis of mediastinal lymphadenopathy. Chest. 2005;128:3004–9. doi: 10.1378/chest.128.4.3004. [DOI] [PubMed] [Google Scholar]
- 17.Bataille L, Lonneux M, Weynand B, et al. EUS-FNA and FDG-PET are complementary procedures in the diagnosis of enlarged mediastinal lymph nodes. Acta Gastroenterol Belg. 2008;71:219–29. [PubMed] [Google Scholar]
- 18.Fritscher-Ravens A, Bohuslavizki KH, Brandt L, et al. Mediastinal lymph node involvement in potentially resectable lung cancer: Comparison of CT, positron emission tomography, and endoscopic ultrasonography with and without fine-needle aspiration. Chest. 2003;123:442–51. doi: 10.1378/chest.123.2.442. [DOI] [PubMed] [Google Scholar]
- 19.Pedersen BH, Vilmann P, Folke K, et al. Endoscopic ultrasonography and real-time guided fine-needle aspiration biopsy of solid lesions of the mediastinum suspected of malignancy. Chest. 1996;110:539–44. doi: 10.1378/chest.110.2.539. [DOI] [PubMed] [Google Scholar]
- 20.Catalano MF, Rosenblatt ML, Chak A, et al. Endoscopic ultrasound-guided fine needle aspiration in the diagnosis of mediastinal masses of unknown origin. Am J Gastroenterol. 2002;97:2559–65. doi: 10.1111/j.1572-0241.2002.06023.x. [DOI] [PubMed] [Google Scholar]


