Abstract
Background
The UK has implemented a national strategy for organ donation that includes a centrally coordinated network of specialist nurses in organ donation embedded in all intensive care units and a national organ retrieval service for deceased organ donors. We aimed to determine whether despite the national approach to donation there is significant regional variation in deceased donor kidney donation rates.
Methods
The UK prospective audit of deaths in critical care was analysed for a cohort of patients who died in critical care between April 2010 and December 2011. Multivariate logistic regression was used to identify the factors associated with kidney donation. The logistic regression model was then used to produce risk-adjusted funnel plots describing the regional variation in donation rates.
Results
Of the 27 482 patients who died in a critical care setting, 1528 (5.5%) became kidney donors. Factors found to influence donation rates significantly were: type of critical care [e.g. neurointensive vs general intensive care: OR 1.53, 95% confidence interval (CI) 1.34–1.75, P<0.0001], patient ethnicity (e.g. ‘Asian’ vs ‘white’: OR 0.17, 95% CI 0.11–0.26, P<0.0001), age (e.g. age >69 vs age 18–39 yr: OR 0.2, 0.15–0.25, P<0.0001), and cause of death [e.g. ‘other’ (excluding ‘stroke’ and ‘trauma’) vs ‘trauma’: OR 0.04, 95% CI 0.03–0.05, P<0.0001]. Despite correction for these variables, kidney donation rates for the 20 UK kidney donor regions showed marked variation. The overall standardized donation rate ranged from 3.2 to 7.5%. Four regions had donation rates of >2 standard deviations (sd) from the mean (two below and two above). Regional variation was most marked for donation after circulatory death (DCD) kidney donors with 9 of the 20 regions demonstrating donation rates of >2 sd from the mean (5 below and 4 above).
Conclusions
The marked regional variation in kidney donation rates observed in this cohort after adjustment for factors strongly associated with donation rates suggests that there is considerable scope for further increasing kidney donation rates in the UK, particularly DCD.
Keywords: donors, organ transplantation; kidney, transplantation; model, statistical; surgery, transplantation; transplantation, kidney
Editor's key points.
There is a significant shortfall in the availability of donor kidneys for transplantation.
Factors influencing donor rates were studied in a large cohort of patients who died in UK intensive care units.
Significant factors included: type of unit, region, age, and ethnicity.
Kidney transplantation prolongs life, improves quality-of-life and is more cost-effective than dialysis.1,2 However, there is a severe global shortage of kidneys for transplantation and a continuing need for countries to improve deceased donor kidney donation rates.3
The most common mode of deceased donation is donation after brain death (DBD).4 Transplantable kidneys can also be recovered from patients whose death is determined according to cardiorespiratory criteria after planned withdrawal of life-sustaining treatments within a critical care setting. This is known as controlled donation after circulatory death (DCD). Although kidneys from controlled DCD donors incur a variable period of warm ischaemic injury at the time of donation, concerns that they are inferior to DBD donor kidneys have been allayed by recent registry data from both the UK and the USA.5–7
In 2008, the UK Organ Donation Taskforce made a number of key recommendations aimed at increasing the number of organ donors, and these have subsequently been implemented by NHS Blood and Transplant (the special authority with responsibility for organ donation and transplantation)8 and others. The changes made include the creation of a centrally coordinated UK-wide network of specialist nurses in organ donation embedded in all intensive care units (ICUs) and a national organ retrieval service for all potential organ donors. The work of the Taskforce resulted in the provision of a professional, ethical, and legal framework for controlled DCD, thereby establishing this mode of deceased donation into clinical practice in the UK.9,10
The introduction of these changes in UK organ donation practice has been associated with a 17% increase in deceased kidney donor numbers from 2007 to 2011. However, this increase is due exclusively to a doubling of DCD kidney donors. Overall deceased donor organ donation rates in the UK remain disappointing on a per capita basis and were exceeded in 2011 by the USA, and several European countries, most notably Spain, Belgium, Portugal, France, and Italy.4,11 When DBD and DCD donor rates are considered separately, the UK compares unfavourably for DBD donor rates. In contrast, DCD donation rates in the UK have doubled since 2007 and UK DCD donation rates in 2011 were exceeded only by those in The Netherlands.4,11
Kidney donation in the UK expressed on a per capita basis suggests significant regional variation and implies potential for increasing kidney donor numbers.12 However, a major shortcoming of using the per capita metric in such comparisons in organ donor numbers is that it does not take into account geographical differences in key factors, such as death rates and number of critical care beds, along with other patient characteristic variations. Accordingly, a risk-adjusted model was developed to allow more accurate and meaningful comparisons of deceased donor rates between UK regions, specifically donations that result in kidney transplantation. In this study, patient characteristics and other relevant characteristics of patients dying in critical care settings were used to develop a model that identified key variables associated with kidney donation. This has allowed calculation of regional risk-adjusted kidney donation rates that provide a robust description of the current variations in DCD kidney donation in the UK.
Methods
Clinical setting
There are 275 acute hospitals in the UK grouped into 20 kidney donation zones. Each kidney donation zone is linked to a kidney transplant unit (with the exception of London) and donation zones are named after the city in which their transplant centre is based. In London, there are several transplant units that fall within the two donation zones designated North and South Thames.
In the UK, there is a national sharing scheme for kidneys from DBD donors13 but if for whatever reason DBD kidneys are not allocated nationally, they are offered to the central transplant unit within the same zone as the retrieval hospital. Kidneys from DCD donors are always offered initially for use in the transplant centre within the regional zone, although, if refused, the kidney is offered to other transplant centres across the UK. In the UK organ donation policy, organ allocation and mandatory data collection is overseen by National Health Service Blood and Transplant (NHSBT). NHSBT have, since April 2010, commissioned a national organ retrieval service that incorporates seven abdominal organ retrieval teams that provide a comprehensive service for recovery of both DBD and DCD donor kidneys.8
Data and statistics
This study is based on the data collected as part of the UK Potential Donor Audit, which was initiated in 2005. The audit collects prospective, basic, non-patient identifiable patient characteristic information for all patients younger than 76 yr who die in a non-cardiothoracic ICU or emergency department, together with date, time, cause of death, and whether organ donation was possible and whether organ donation occurred.14 For the purposes of this study, a deceased kidney donor was defined as a donor from whom at least one kidney was transplanted. The present analysis is based on the data collected during a 20-month period between April 1, 2010 (when the audit was expanded to capture data from emergency departments) and December 31, 2011.
Multivariate logistic regression analysis was performed to determine factors associated with overall deceased donor kidney donation, and with DCD and DBD donation when considered separately. Factors considered for inclusion were those variables that the authors considered may be associated with organ donation and selected from the Potential Donor Audit. The factors considered within the multifactorial model in a forward step-wise fashion were: age, cause of death, ethnicity, and type of critical care in which the death took place. All were found to explain independently significant variation in donation rates. The logistic regression model was used to produce ‘standardized-donation rates’ for each of the 20 kidney donation zones in the UK, adjusting for the impact that these factors would have on the donation rates in their catchment populations. Funnel plots15 were used to display the standardized data using funnel limits based upon confidence intervals (CIs) of 95 and 99.8% [2 and 3 standard deviations (sds), respectively]. The software used for the data analysis was SAS 9.1 (SAS Institute, Cary, NC, USA).
Results
Factors associated with organ donation
Table 1 shows patient characteristic data for all deaths in UK critical care areas (including emergency departments) captured by the UK Potential Donor Audit during the 20-month study period. There were 27 482 deaths, of which 78% occurred in general ICUs, 11% in neurosurgical ICUs, and 11% in emergency departments. The majority (94.4%) of those dying in critical care settings did not become kidney donors for various reasons including unsuitable mode of death, organ failure, major systemic infection, active cancer, and lack of consent for organ donation. Of the 1528 (5.6%) patients who died and became kidney donors, the majority were DBD donors (n=984) but over a third (n=544) were DCD donors. Two hundred and seventy-four of the hospitals studied had at least one death in critical care and 237 of the donation hospitals had at least one deceased kidney donor during the study period (median 4.0, range 1–39). Of note, 101/275 (37%) of the hospitals provided 5 or more deceased donors. All of the hospitals with at least 5 donors during the study period had at least 1 DBD donor with 7/101 (7%) of these providing no DCD donors.
Table 1.
Factors associated with organ donation: multivariate logistic regression analysis for death in critical care leading to kidney donation for all deceased donors, DCD donors, and DBD donors
| Number of deaths n=27 482 | All donors |
DCD donors |
DBD donors |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of all donors n=1528 | OR (95% CI) | P-values | Number of DCD donors n=544 | OR (95% CI) | P-values | Number of DBD donors n=984 | OR (95% CI) | P-values | ||
| Type of critical care | ||||||||||
| General | 21 526 (78%) | 973 (64%) | 1 | 343 (63%) | 1 | 630 (64%) | 1 | |||
| Neurosurgical | 2906 (11%) | 488 (32%) | 1.53 (1.34–1.75) | <0.0001 | 177 (33%) | 1.56 (1.28–1.90) | <0.0001 | 311 (32%) | 1.36 (1.17–1.60) | <0.0001 |
| Emergency Department | 3050 (11%) | 67 (4%) | 0.44 (0.34–0.57) | <0.0001 | 24 (4%) | 0.44 (0.29–0.68) | 0.0002 | 43 (4%) | 0.48 (0.34–0.66) | <0.0001 |
| Patient cause of death | ||||||||||
| Trauma | 480 (2%) | 112 (7%) | 1 | 49 (9%) | 1 | 63 (6%) | 1 | |||
| Stroke | 5551 (20%) | 1241 (81%) | 1.05 (0.83–1.34) | 0.65 | 408 (75%) | 0.69 (0.50–0.97) | 0.03 | 883 (84%) | 1.38 (1.03–1.85) | 0.03 |
| Other | 21 019 (76%) | 173 (11%) | 0.04 (0.03–0.05) | <0.0001 | 85 (16%) | 0.04 (0.03–0.07) | <0.0001 | 88 (9%) | 0.04 (0.03–0.06) | <0.001 |
| Missing | 432 (2%) | 2 (0%) | 0.02 (0.01–0.09) | <0.0001 | 2 (0%) | 0.06 (0.01–0.23) | <0.0001 | 0 (0%) | n/a | <0.0001 |
| Patient ethnicity | ||||||||||
| White | 21 401 (78%) | 1450 (95%) | 1 | 522 (96%) | 1 | 928 (94%) | 1 | |||
| Asian | 1470 (5%) | 21 (1%) | 0.17 (0.11–0.26) | <0.0001 | 7 (1%) | 0.20 (0.10–0.43) | <0.0001 | 14 (1%) | 0.19 (0.11–0.33) | <0.0001 |
| Other | 876 (1%) | 36 (2%) | 0.35 (0.24–0.50) | <0.0001 | 6 (1%) | 0.20 (0.09–0.45) | 0.0001 | 30 (3%) | 0.48 (0.33–0.71) | 0.0003 |
| Missing | 3735 (3%) | 21 (1%) | 0.13 (0.08–0.20) | <0.0001 | 9 (2%) | 0.17 (0.09–0.33) | <0.0001 | 12 (1%) | 0.12 (0.07–0.22) | <0.0001 |
| Patient age at death | ||||||||||
| Under 18 yr | 1189 (4%) | 63 (4%) | 0.70 (0.51–0.95) | 0.02 | 20 (4%) | 0.75 (0.46–1.24) | 0.26 | 43 (4%) | 0.73 (0.51–1.05) | 0.09 |
| 18–39 yr | 2911 (11%) | 354 (23%) | 1 | 112 (21%) | 1 | 242 (25%) | 1 | |||
| 40–49 yr | 3502 (13%) | 321 (21%) | 0.80 (0.66–0.96) | 0.02 | 94 (17%) | 0.80 (0.60–1.08) | 0.15 | 227 (23%) | 0.84 (0.68–1.03) | 0.10 |
| 50–59 yr | 5487 (20%) | 381 (25%) | 0.66 (0.55–0.78) | <0.0001 | 126 (23%) | 0.78 (0.60–1.03) | 0.08 | 255 (26%) | 0.66 (0.54–0.81) | <0.0001 |
| 60–69 yr | 8439 (31%) | 319 (21%) | 0.41 (0.34–0.49) | <0.0001 | 141 (26%) | 0.70 (0.54–0.92) | 0.01 | 178 (18%) | 0.35 (0.28–0.43) | <0.0001 |
| More than 69 yr | 5954 (22%) | 90 (6%) | 0.20 (0.15–0.25) | <0.0001 | 51 (9%) | 0.45 (0.32–0.64) | <0.0001 | 39 (4%) | 0.14 (0.10–0.19) | <0.0001 |
Logistic regression analysis identified several factors that were associated with death proceeding to kidney donation, and these were broadly similar for both DCD and DBD donors (Table 1). The type of critical care unit in which the death occurred was an important determinant of whether kidney donation took place, with death in a neurosurgical unit more likely to result in kidney donation than death in a general ICU (OR 1.53, 95% CI 1.34–1.75, P<0.0001) and death in the emergency department less likely to result in kidney donation (OR 0.44, 95% CI 0.34–0.57, P<0.0001). Only a minority of deaths in critical care were caused by trauma (2%) or stroke (20%), although these causes accounted for 88% of the kidney donor deaths. Patients who were not of white ethnicity (6%) were less likely to donate than those of white ethnicity (‘Asian’ vs ‘white’ OR 0.17, 95% CI 0.11–0.26, P<0.0001 and ‘other’ vs white’ OR 0.35, 95% CI 0.24–0.50, P<0.0001). Increasing patient age (from age 18 to 69 yr) was associated with a greater chance of death in critical care, but an incrementally decreasing chance of becoming a kidney donor (e.g. patient age >69 vs age 18–39, OR 0.2, 0.15–0.25, P<0.0001).
Regional variation in kidney donation rates
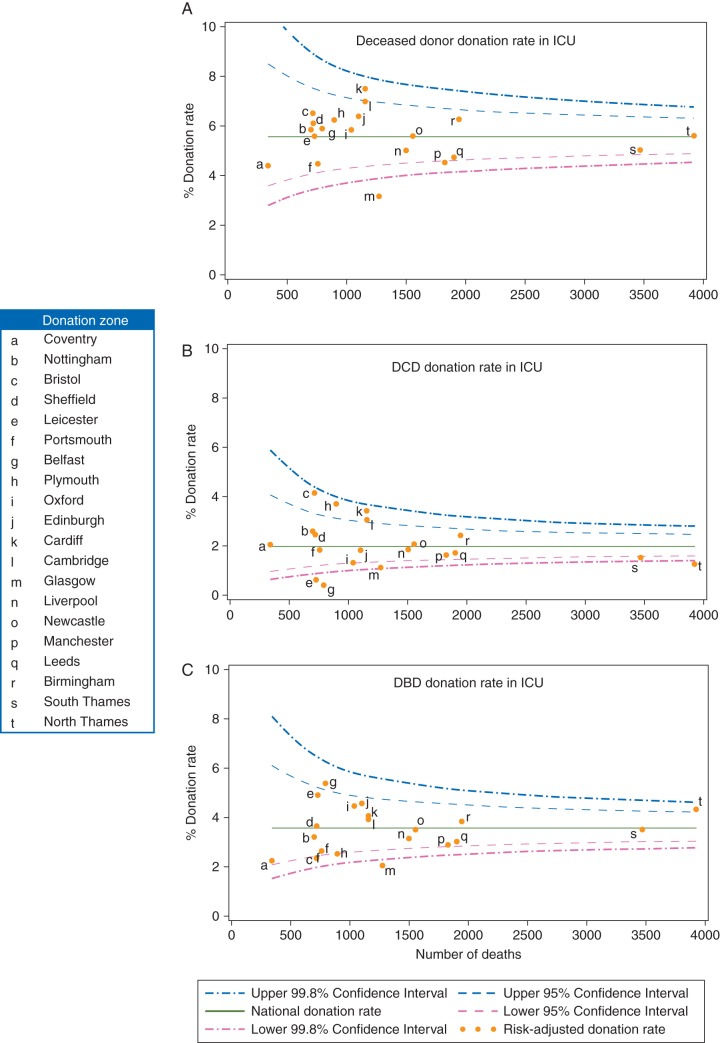
The kidney donation rates (after standardization using the logistic regression models developed in Table 1) for each of the 20 regional kidney donation zones in the UK are plotted in Figure 1a–c. For completeness, the non-standardized kidney donation rates are shown in the Appendix but all the subsequent comments relate exclusively to the standardized-donation rates.
Fig 1.
(a–c) Funnel plots demonstrating regional variation in donation rates.
The 20 kidney donation zones differed considerably in size, with the number of deaths of critical care patients ranging 450–4000. There was marked variation between donation zones in standardized kidney donation rates. The overall deceased donor standardized donation rate (i.e. for both DBD and DCD donors) ranged from 3.2 to 7.5%. Two zones (Cardiff and Cambridge) had significantly higher overall deceased donor standardized donation rates than the mean national donation rate (Fig. 1a). Two zones (Glasgow and Manchester) had significantly lower overall deceased donor standardized donation rates, and Glasgow differed from the mean by more than 3 sds. When DCD donors were considered separately, the degree of zonal variation was more marked, with 4 zones demonstrating DCD donation rates significantly above (>2 sd) and 5 significantly below the mean donation rate (Fig. 1b). DBD donation rates showed less variation than those for DCD donors (Fig. 1c): two zones had high and three zones low donation rates compared with the UK mean. It was notable that two of the four zones (i.e. Cardiff and Cambridge) with significantly high standardized DCD donation rates also had standardized DBD donation rates that were close to the UK mean (Fig. 1b and c). The other two zones (Plymouth and Bristol) with high standardized DCD donation rates had standardized DBD donation rates that were significantly below the national average (Fig. 1b and c). The converse applied to two zones with high standardized DBD donation rates and low standardized DCD donation rates (North London and Belfast).
Discussion
The present in-depth analysis of deceased kidney donors in the UK is based on data collected as part of the prospective UK Potential Donor Audit.16 This allowed factors associated with kidney donation to be identified in a cohort of patients that included all of those ever likely to donate (i.e. those dying in a critical care setting, rather than using the general population as a comparator group). The factors that are associated with organ donation are generally well known but, to the best of our knowledge, this is the first analysis to quantify the relative strength of these associations.17–19 Overall, the factors associated with organ donation were similar for DBD and DCD donors and included ethnicity, cause of death, type of critical care, and age.
While it is widely appreciated that non-white ethnicity is associated with a low donation rate,19 the finding that white patients who died in critical care settings are more than five times more likely to become organ donors than Asian patients was particularly striking, and highlights the magnitude of the challenge to encourage organ donation from ethnic minority groups in the UK. A number of initiatives have been introduced in the UK to address the low organ donation rate in ethnic minorities, including targeted advertising campaigns,8,20 but more is clearly required.
Cause of death was a major predictor of kidney donation in the present study, with those dying from stroke (including subarachnoid haemorrhage) and trauma being 20 times more likely to become kidney donors than those dying of other causes. The magnitude of this effect is to be expected, given that most deceased organ donors have catastrophic intracranial injury, although it is interesting to note that some DCD donors in particular did not have a neurological injury as their primary cause of death. However, given the strong association between neurological injury and kidney donation, it is surprising that those dying in a neurosurgical intensive care setting were only one and a half times more likely to become kidney donors than those dying in a general intensive care setting. This may reflect the relative under-provision of specialist neurointensive care beds in the UK, which means that some patients who may potentially have benefitted from admission to neurointensive care are instead cared for in a general setting.21,22 The majority of deaths in intensive care occurred in patients aged more than 60 yr (53%), but older patients were less likely to become organ donors. A major reason for this is that older patients are more likely to have serious comorbidities, including malignancy, that preclude them from being accepted as organ donors. While kidneys from older donors fare less well after transplantation,6,7,23 there is recognition that kidneys from older deceased donors may still provide useful organs for transplantation, particularly for older recipients, and there may be further scope for considering older patients as potential kidney donors.
While DCD kidney donor rates have risen markedly in the UK,24 a crude analysis of regional kidney donation rates indicated great variation in activity across the UK, particularly for DCD kidney donation.12 Care is needed in the interpretation of this type of raw donation rate data, however, because it does not take into account underlying differences between regions in the death rate of patients in critical care, the level of critical care provision and patient characteristic differences, and discard rates of retrieved kidneys. In the present analysis of regional kidney donor activity, only kidney donors in whom at least one kidney was subsequently transplanted were included and adjustment was made for the above variables to give a more accurate ‘standardized’ assessment of kidney donation rate. This revealed that significant differences in regional donation rates exist, even after adjusting for regional heterogeneity.
One of the aims of the Organ Donor Taskforce was to ensure greater consistency in decision-making across the UK, with regard to both the referral of potential donors and their assessment and acceptance. This study reveals that considerable variation in practice persists. Regional variation was most striking for DCD kidney donor rates, with 9 of the 20 kidney donation regions having DCD kidney donor rates that were more than 2 sds from the mean. The reasons for such a large regional variation in deceased kidney donor numbers were not identified in this study and are likely to be complex. Variations in donor identification rates, consent for organ donation, and variations in kidney acceptance criteria by the receiving transplant centres are likely to be the most important factors.
Our findings on regional variation of adjusted kidney donor rates suggest that there is considerable scope for further increasing donor numbers in many regions, particularly in the case of DCD donors. An important difference between DBD and DCD kidney donation is that while all DBD kidneys are allocated according to a national sharing algorithm, a national sharing scheme for kidneys from DCD donors remains under development.13 Instead kidneys from such donors are often only offered to the local transplant centre, and it is likely that the level of enthusiasm of the local centre for use of DCD donor kidneys is a major determinant of regional DCD kidney donation rate. Differences in local acceptance criteria for DCD kidneys contribute to inequality in access to transplantation, and patients on the waiting list for renal transplantation at centres that are within donation zones with low DCD donation rates will wait longer overall for a kidney transplant than those listed at centres with a high level of enthusiasm for using kidneys from DCD donors including older DCD donors.25
DCD donors provide fewer organs per donor than DBD donors, and liver and pancreas transplants from DCD donors have poorer outcomes after transplantation than those from DBD donors.26–28 Furthermore, there is concern that a proportion of DCD donors might have become DBD donors had they been managed differently. However, the management of patients dying in critical care must be made by critical care clinicians acting in the best interest of the patient independently of transplant clinicians and there is no clear evidence that the increase in DCD donors in the UK has occurred at the expense of DBD donors.28,29 In the present study, two centres with high DCD kidney donor rates had low DBD kidney donor rates. However, the two centres with the highest overall deceased kidney donation rate achieved this by having significantly higher DCD donor rates and DBD donor rates that were above the mean, showing that a high DCD donor rate need not be achieved at the expense of reduced DBD donor activity.
While the present study was confined to deceased donors in the UK, the risk adjustment methodology used is readily applicable to other countries that have prospective audits of deceased organ donation potential, and it would be interesting to know whether such marked regional variations in adjusted deceased donor kidney donation rates also exist in such countries. In particular, it would be instructive to know whether countries with very high donation rates show less adjusted regional variation rates in kidney donation. The methodology might also be of value in making international comparisons for adjusted deceased organ donation rates. Inevitable limitations of the present study are that it is based on a fixed period of observation in a time of changing practice and it will be interesting to observe whether regional variations in kidney donation persist in future years. Another limitation of this and other registry analyses is the failure to take into account the residual confounding factors in the modelling to produce risk-adjusted data; for example, no information was available on the socio-economic class of potential donors. A further limitation of this study is that it controls for differences in ICU capacity by using the total number of deaths in ICU as the denominator in the analysis. Variation in ICU admission policy, capacity, and workload may mean that the chances of death progressing to organ donation differ between units.30
In conclusion, there is marked regional variation in deceased kidney donation rates in the UK, even after correction for factors known to influence strongly the likelihood of patients dying in critical care proceeding to kidney donation. The overall vision of the UK Organ Donation Taskforce was that donation should become a routine component of end-of-life care and considered wherever possible, regardless of the mode of death or where in a hospital the patient happened to be when its inevitability was recognized. This study suggests that there is considerable scope for further increasing donor numbers in the UK by ensuring that all centres adopt best practice for identification and management of potential kidney donors, to give more patients the option of donation when they die.
Authors' contributions
All the authors contributed to the study design and data interpretation. D.M.S., R.J.J., A.J.H., and D.C. undertook the analysis and validation of the data. D.M.S. and J.A.B. drafted the initial report, and all the authors contributed to the final draft. Data were provided for the NHS Blood and Transplant registry by staff from UK hospitals and compiled from the registry by D.M.S.
Declaration of interest
None declared.
Funding
This work was supported by a grant from UK National Health Service Blood and Transplant (grant number UKT07-2); Cambridge National Institute for Health Research Biomedical Research Centre. Funding for open access was provided by the Cambridge National Institute for Health Research Biomedical Research Centre, Cambridge, UK.
Supplementary Material
Acknowledgements
We are grateful to all the critical care physicians, emergency physicians, and nurses who contributed the data for this study.
Appendix
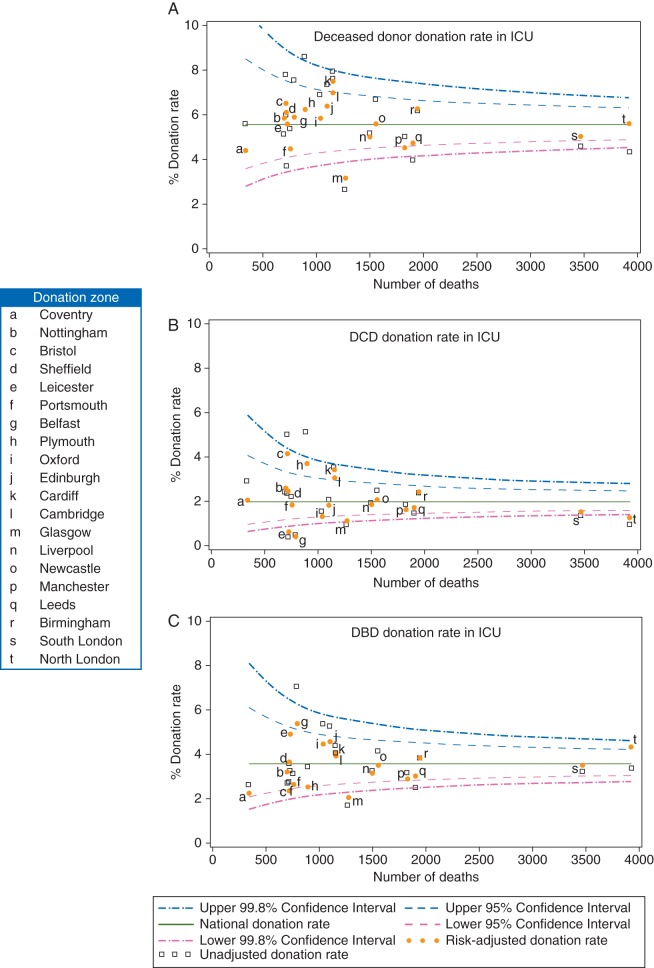
Figure A1.
(a–c) Funnel plots demonstrating regional variation in donation rates for both risk-adjusted and non-adjusted data.
References
- 1.Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11:2093–109. doi: 10.1111/j.1600-6143.2011.03686.x. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–30. doi: 10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- 3.Garcia GG, Harden P, Chapman J World Kidney Day Steering Committee 2012. The global role of kidney transplantation. Lancet. 2012;379:e36–8. doi: 10.1016/S0140-6736(12)60202-5. [DOI] [PubMed] [Google Scholar]
- 4.Council of Europe. International figures on donation and transplantation 2011. Newsl Transplant [Internet] 17:34–40. Available from http://www.ont.es/publicaciones/Paginas/Publicaciones.aspx. (accessed 26 November 2013) [Google Scholar]
- 5.Locke J, Segev D, Warren D, Dominici F, Simpkins C, Montgomery R. Outcomes of kidneys from donors after cardiac death: implications for allocation and preservation. Am J Transplant. 2007;7:1797–807. doi: 10.1111/j.1600-6143.2007.01852.x. [DOI] [PubMed] [Google Scholar]
- 6.Summers DM, Johnson RJ, Allen J, et al. Analysis of factors that affect outcome after transplantation of kidneys donated after cardiac death in the UK: a cohort study. Lancet. 2010;376:1303–11. doi: 10.1016/S0140-6736(10)60827-6. [DOI] [PubMed] [Google Scholar]
- 7.Summers DM, Johnson RJ, Hudson A, Collett D, Watson CJ, Bradley JA. Effect of donor age and cold storage time on outcome in recipients of kidneys donated after circulatory death in the UK: a cohort study. Lancet. 2013;381:727–34. doi: 10.1016/S0140-6736(12)61685-7. [DOI] [PubMed] [Google Scholar]
- 8.Organ Donation Taskforce. Department of Health; 2008. Organs for transplants: a report from the Organ Donation Taskforce [Internet] [cited 2012 25/03/2012] Available from http://www.nhsbt.nhs.uk/to2020/resources/OrgansfortransplantsTheOrganDonorTaskForce1streport.pdf. (accessed 26 November 2013) [Google Scholar]
- 9.UK Donation Ethics Committee. An Ethical Framework for Controlled Donation after Circulatory Death [Internet] Academy of Royal Medical Colleges; 2011. [cited 2012 Jun 25] Available from http://www.aomrc.org.uk/publications/reports-a-guidance.html. (accessed 26 November 2013) [Google Scholar]
- 10.British Transplantation Society and The Intensive Care Society. Donation after circulatory death: report of a consensus meeting [Internet] 2010. bts.org.uk . [cited 2012 Jun 25] Available from http://www.bts.org.uk/Documents/Guidelines/Active/DCDforBTSandICSFINAL.pdf. (accessed 26 November 2013)
- 11.Council of Europe. International figures on donation and transplantation—2007. Newsl Transplant [Internet] 13:23–9. Available from http://www.ont.es/publicaciones/Documents/Newsletter2008.pdf. (accessed 26 November 2013) [Google Scholar]
- 12.Reid AWN, Harper S, Jackson CH, et al. Expansion of the kidney donor pool by using cardiac death donors with prolonged time to cardiorespiratory arrest. Am J Transplant [Internet] 2011;11:995–1005. doi: 10.1111/j.1600-6143.2011.03474.x. [DOI] [PubMed] [Google Scholar]
- 13.Johnson R, Fuggle S, Mumford L, Bradley J, Forsythe J, Rudge C. A New UK 2006 National Kidney Allocation Scheme for deceased heart-beating donor kidneys. Transplantation. 2010;89:387–94. doi: 10.1097/TP.0b013e3181c9029d. [DOI] [PubMed] [Google Scholar]
- 14.Barber K, Falvey S, Hamilton C, Collett D, Rudge C. Potential for organ donation in the United Kingdom: audit of intensive care records. Br Med J. 2006;332:1124–7. doi: 10.1136/bmj.38804.658183.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spiegelhalter DJ. Funnel plots for comparing institutional performance. Stat Med. 2005;24:1185–202. doi: 10.1002/sim.1970. [DOI] [PubMed] [Google Scholar]
- 16.Barber KM, Hussey JC, Bond ZC, Falvey SJ, Collett D, Rudge CJ. The UK National Potential Donor Audit. Transplant Proc. 2005;37:568–70. doi: 10.1016/j.transproceed.2004.12.088. [DOI] [PubMed] [Google Scholar]
- 17.Simpkin AL, Robertson LC, Barber VS, Young JD. Modifiable factors influencing relatives’ decision to offer organ donation: systematic review. Br Med J. 2009;338:b991. doi: 10.1136/bmj.b991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis C, Randhawa G. The influence of religion on organ donation and transplantation among the Black Caribbean and Black African population—a pilot study in the United Kingdom. Ethn Dis. 2006;16:281–5. [PubMed] [Google Scholar]
- 19.Randhawa G. Death and organ donation: meeting the needs of multiethnic and multifaith populations. Br J Anaesth. 2012;108(Suppl 1):i88–91. doi: 10.1093/bja/aer385. [DOI] [PubMed] [Google Scholar]
- 20.NHSBT. Black and Asian Organ Donation Campaign [Internet] organdonation.nhs.uk. [cited 2013 Feb 4] Available from http://www.organdonation.nhs.uk/campaigns/other_campaigns/black_and_asian/index.asp. (accessed 26 November 2013) [Google Scholar]
- 21.Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38:1647–53. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- 22.Crimmins DW, Palmer JD. Snapshot view of emergency neurosurgical head injury care in Great Britain and Ireland. J Neurol Neurosurg Psychiatr. 2000;68:8–13. doi: 10.1136/jnnp.68.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rao P, Schaubel D, Guidinger M, et al. A comprehensive risk quantification score for deceased donor kidneys: the kidney donor risk index. Transplantation. 2009;88:231–6. doi: 10.1097/TP.0b013e3181ac620b. [DOI] [PubMed] [Google Scholar]
- 24.NHSBT. Transplant activity in the UK—activity report 2010–11 [Internet] 2011. [cited 2012 Jun 18] Available from http://www.organdonation.nhs.uk/statistics/transplant_activity_report/archive_activity_reports/ (accessed 26 November 2013)
- 25.NHSBT. Median Waiting Time to Kidney Transplant [Internet] organdonation.nhs.uk . [cited 2012 Jun 18] Available from http://www.organdonation.nhs.uk/ukt/statistics/centre-specific_reports/pdf/waiting_time_to_transplant.pdf. (accessed 26 November 2013) [Google Scholar]
- 26.Mallik M, Callaghan CJ, Hope M, et al. Comparison of liver transplantation outcomes from adult split liver and circulatory death donors. Br J Surg. 2012;99:839–47. doi: 10.1002/bjs.8755. [DOI] [PubMed] [Google Scholar]
- 27.Qureshi MS, Callaghan CJ, Bradley JA, Watson CJ, Pettigrew GJ. Outcomes of simultaneous pancreas-kidney transplantation from brain-dead and controlled circulatory death donors. Br J Surg. 2012;99:831–8. doi: 10.1002/bjs.8733. [DOI] [PubMed] [Google Scholar]
- 28.Summers DM, Counter C, Johnson RJ, Murphy PG, Neuberger JM, Bradley JA. Is the increase in DCD organ donors in the United Kingdom contributing to a decline in DBD donors? Transplantation. 2010;90:1506–10. doi: 10.1097/TP.0b013e3182007b33. [DOI] [PubMed] [Google Scholar]
- 29.Saidi RF, Bradley J, Greer D, et al. Changing pattern of organ donation at a single center: are potential brain dead donors being lost to donation after cardiac death? Am J Transplant. 2010;10:2536–40. doi: 10.1111/j.1600-6143.2010.03215.x. [DOI] [PubMed] [Google Scholar]
- 30.Bion JF, Nightingale P, Taylor BL. Will the UK ever reach international levels of organ donation? Br J Anaesth. 2012;108(Suppl. 1):i10–3. doi: 10.1093/bja/aer406. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.