Abstract
Background
Urinary incontinence is a common short-term complication of radical prostatectomy (RP). Little is known about the long-term impact of RP on continence.
Objective
To elucidate the long-term progression of continence after RP.
Design, setting, and participants
From October 2000 through September 2012, 1788 men undergoing open RP for clinically localized prostate cancer by a single surgeon at an urban tertiary care center prospectively signed consent to be followed before RP and at 3, 6, 12, 24, 96, and 120 mo after RP. A consecutive sampling method was used and all men were included in this study.
Intervention Men underwent open RP
Outcome measurements and statistical analysis
Regression models controlled for preoperative University of California, Los Angeles–Prostate Cancer Index urinary function score (UCLA-PCI-UFS), age, prostate-specific antigen level, Gleason score, stage, nerve-sparing status, race, and marital status were used to evaluate the association of time since RP with two dependent variables: UCLA-PCI-UFS and continence status.
Results and limitation
The mean UCLA-PCI-UFS declined between 2 yr and 8 yr (83.8 vs 81.8; p = 0.007) and marginally between 8 yr and 10 yr (81.8 vs 79.6; p = 0.036) after RP, whereas continence rate did not significantly change during these intervals. Men ≥60 yr old experienced a decline in mean UCLA-PCI-UFS between 2 yr and 8 yr (p = 0.002) and a marginal decline in continence rate between 2 yr and 10 yr (p = 0.047), whereas these variables did not change significantly in men <60 yr old. These outcomes are for an experienced surgeon, so caution should be exercised in generalizing these results.
Conclusions
Between 2 yr and 10 yr after RP, there were slight decreases in mean UCLA-PCIUFS and continence rates in this study. Men aged <60 yr had better long-term outcomes. These results provide realistic long-term continence expectations for men undergoing RP.
Keywords: Incontinence, Outcomes, Prostate cancer, Prostatectomy, Quality of life
1. Introduction
Radical prostatectomy (RP) is a common treatment for prostate cancer, the most common noncutaneous malignancy in men and second-leading cause of death from cancer for men in the United States [1,2]. Stress urinary incontinence is a complication of RP and has a significant negative impact on quality of life and satisfaction following RP [3–5]. Reported rates of incontinence depend on surgical technique, definition, and methodology for assessing continence [6–8]. Continence rates and scores, measured by surveys capturing multiple continence domains, worsen immediately after RP and subsequently improve up to 2 yr after RP [6,9–13]. A majority of men recover continence by 3 mo and continence rates exceed 90% by 12 mo [12,13]. There is a paucity of studies characterizing continence beyond 2 yr after RP, and these report inconsistent findings. The literature indicates that after 2 yr, continence rates decline and continence scores stabilize or steadily decline [3,11,14–16]. We have reported that as many as 23% of men experience qualitative improvements in continence from 2 yr to 4 yr after RP [9]. The objective of the present study was to elucidate long-term continence in a cohort of men undergoing RP and who were followed in a prospective outcomes study using validated, self-administered questionnaires obtained prior to, and at several times following, RP. We also sought to define the characteristics of men who may be more likely to achieve long-term improvement in continence.
2. Methods
From October 2000 through September 2012, 1836 men underwent open RP by a single surgeon (HL). Of these men, 1788 (97%) signed informed consent to participate in our institutional review board-approved, prospective, longitudinal outcomes study. The University of California, Los Angeles–Prostate Cancer Index–Urinary Function Index (UCLA-PCI-UFI) was completed at baseline and at 3, 6, 12, 24, 96, and 120 mo after surgery. The questionnaires were self-administered during scheduled office visits or returned via mail to a data manager whose sole responsibility is maintenance of the outcomes database. The operating surgeon was not involved in data collection, entry, retrieval, and statistical analysis.
The UCLA-PCI-UFI is a validated, self-administered continence score that captures five domains of continence: leaking frequency, urinary control, diaper and pad use, dripping problems, and climacturia (Appendix 1) [17]. Both the UCLA-PCI-UFI composite score (UCLA-PCI-UFS) and the continence rate, using a definition of up to one pad daily, were ascertained at all follow-up intervals.
Two multiple regression models were used to evaluate the association of time since RP with UCLA-PCI-UFS and continence status. The first was a generalized, linear model, where the dependent variable was total UCLA-PCI-UFS, specified in continuous terms. The second model was a logistic regression in which the dependent variable was continence status (1 = continent, 0 = incontinent). In both models, there was one observation per patient per follow-up period, for a total of up to six observations (3, 6, 12, 24, 96, and 120 mo). Key independent variables of interest were dummies for each follow-up period (6, 12, 24, 96, and 120 mo; reference: 3 mo). Both models controlled for preoperative UCLA-PCI-UFS, age (continuous, in years), preoperative prostate-specific antigen (PSA) level (continuous, in nanograms per milliliter), Gleason score (≤6, 3 + 4, 4 + 3, 7 [unspecified], ≥8, missing), stage (T2a, T2b, T2c, T3a, T3b, T3c, other, or missing), type of nerve-sparing surgery (bilateral, unilateral, none, missing), race (white, black, Hispanic, Asian, other, missing), and marital status (married, single, widowed, divorced or separated, other, or missing). Missing categories allowed us to include the minority (generally <1%) of respondents who only completed a portion of the survey (Table 1). Standard errors were clustered by individual. We also included a random effect for each man to represent other distinguishing characteristics not controlled for by our independent covariates. In men who responded at both baseline and 3 mo, the McNemar test and paired sample t tests were used to assess whether the proportion of continent men or mean UCLA-PCI-UFS, respectively, differed significantly between these assessments.
Table 1.
Characteristics of 1788 men undergoing radical prostatectomy for prostate cancer
| Characteristic | Men, no. (%) (N = 1788) |
|---|---|
| Age, yr, mean ± SEM | 58.9 ± 0.17 |
| Race | |
| Black | 72 (4) |
| Asian | 36 (2) |
| White | 1608 (90) |
| Hispanic | 29 (2) |
| Other | 28 (2) |
| No response | 15 (1) |
| Marital status | |
| Divorced | 73 (4) |
| Married | 1537 (86) |
| Separated | 16 (1) |
| Single | 113 (6) |
| Widowed | 27 (2) |
| No response | 22 (1) |
| PSA level, ng/ml, mean ± SEM | 6.27 ± 0.128 |
| Pathologic Gleason score | |
| 0–6 | 867 (48) |
| 7 | 791 (43) |
| 8–10 | 114 (6) |
| Missing | 16 (1) |
| Pathologic stage | |
| 0–2 | 1352 (76) |
| 3–4 | 420 (23) |
| Missing | 16 (1) |
| Nerve-sparing status | |
| Bilateral | 1405 (79) |
| Unilateral | 270 (15) |
| None or blank | 149 (8) |
| Preoperative UCLA-PCI-UFS, mean ± SEM | 97.3 ± 0.17 |
SEM = standard error of the mean; PSA = prostate-specific antigen; UCLA-PCI-UFS = University of California, Los Angeles–Prostate Cancer Index urinary function score.
Finally, when evaluating outcomes, we were concerned about potential bias, in that men with good or bad outcomes may have been more likely to respond. Therefore, we performed chi-square and paired t tests comparing mean preoperative UCLA-PCI-UFS between respondents and nonrespondents at years 2, 8, and 10 and comparing mean 2-yr UCLA-PCI-UFS between respondents and nonrespondents at years 8 and 10.
Analyses were conducted in SPSS v.19.0.0.1 (IBM Corp., Armonk, NY, USA) and STATA/SE v.12.0 (StataCorp LP, College Station, TX, USA). Differences were deemed to be significant at a two-sided p < 0.05.
3. Results
Of the 1788 men who consented to participate in the study (Table 1), a total of 98%, 99%, 95%, 90%, 84%, 53%, and 43% completed the UCLA-PCI-UFI at baseline and 3, 6, 12, 24, 96, and 120 mo, respectively. There was no significant difference in age, race, marital status, nerve-sparing status, preoperative PSA level, or preoperative UCLA-PCI-UFS between men who did and did not complete the outcome assessment at 10 yr (data not shown). In addition, no significant differences among groups were found when comparing mean preoperative UCLAPCI-UFS between respondents and nonrespondents or mean 2-yr UCLA-PCI-UFS between respondents and nonrespondents at years 8 and 10 (p = 0.17–0.87; data not shown).
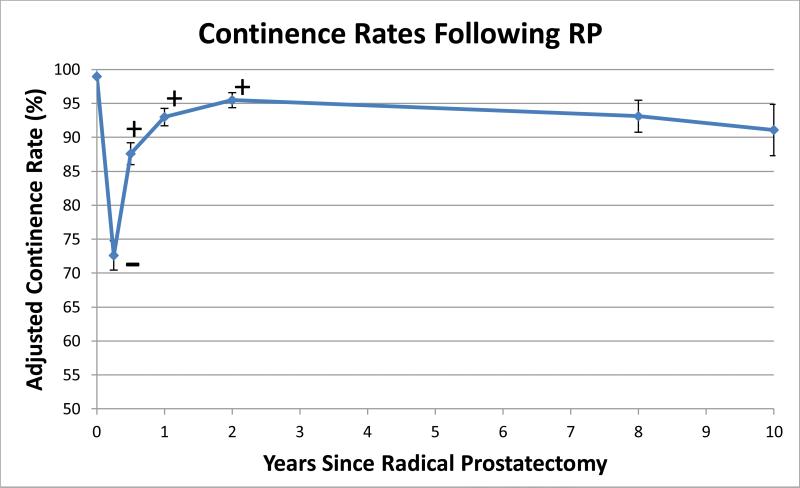
Adjusted time-dependent mean UCLA-PCI-UFS for all men worsened between baseline and 3 mo (97.4 vs 68.2; p < 0.001) (Fig. 1). Mean UCLA-PCI-UFS significantly improved between all successive time points until 2 yr and then declined significantly between 2 yr and 8 yr (83.8 vs 81.8; p = 0.007) and marginally but significantly between 8 yr and 10 yr after RP (81.8 vs 79.6; p = 0.036). UCLA-PCI-UFS was significantly lower at 10 yr compared with 2 yr (p < 0.001). The adjusted continence rate for all men declined significantly from baseline to 3 mo after RP (99.0% vs 72.6%; p < 0.001) (Fig. 2). Continence rates significantly improved between all time points up to 2 yr after RP, reaching 95.5%. Thereafter, continence rates did not significantly change between 2 yr and 8 yr (95.5% vs 93.1%; p = 0.059) and between 8 yr and 10 yr (93.1% vs 91.1%; p = 0.229). Continence rates, however, were marginally but significantly lower at 10 yr compared with 2 yr (p = 0.024).
Fig. 1.
– Adjusted mean University of California, Los Angeles–Prostate Cancer Index urinary function score following radical prostatectomy. Error bars represent 95% confidence intervals. UCLA-PCI-UFS = University of California, Los Angeles–Prostate Cancer Index urinary function score; RP = radical prostatectomy; + = significant increase in mean UCLA-PCI-UFS from previous time point; – = significant decrease in mean UCLA-PCI-UFS from previous time point.
Fig. 2.
– Adjusted continence rates following radical prostatectomy. Error bars represent 95% confidence intervals. RP = radical prostatectomy; + = significant increase in mean University of California, Los Angeles–Prostate Cancer Index urinary function score (UCLA-PCI-UFS) from previous time point; – = significant decrease in mean UCLA-PCIUFS from previous time point.
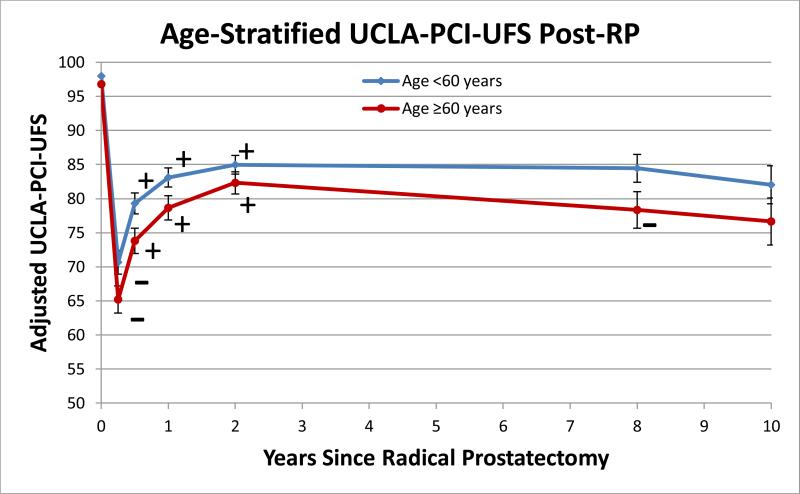
Figure 3 shows the adjusted mean UCLA-PCI-UFS stratified by preoperative age. For men aged <60 yr, mean UCLA-PCI-UFS declined significantly from baseline to 3 mo (98.0 vs 70.7; p < 0.001), followed by significant interval increases until 2 yr. Mean UCLA-PCI-UFS did not significantly change between 2 yr and 8 yr (85.0 vs 84.4; p = 0.571) and 8 yr and 10 yr (84.4 vs 82.0; p = 0.063) but was marginally significantly lower at 10 yr when compared with 2 yr (p = 0.029). For men aged ≥60 yr, mean UCLA-PCI-UFS followed the same trends as younger men up to 2 yr. However, a significant decrease in mean UCLA-PCI-UFS was observed between 2 yr and 8 yr (82.3 vs 78.3; p = 0.002). Mean UCLA-PCI-UFS did not significantly change between 8 yr and 10 yr (78.3 vs 76.7; p = 0.298) but was significantly lower at 10 yr when compared with 2 yr (p < 0.001).
Fig. 3.
– Adjusted mean University of California, Los Angeles–Prostate Cancer Index urinary function score following radical prostatectomy, stratified by age. Error bars represent 95% confidence intervals. UCLA-PCI-UFS = University of California, Los Angeles–Prostate Cancer Index urinary function score; RP = radical prostatectomy; + = significant increase in mean UCLA-PCI-UFS from previous time point; – = significant decrease in mean UCLA-PCI-UFS from previous time point.
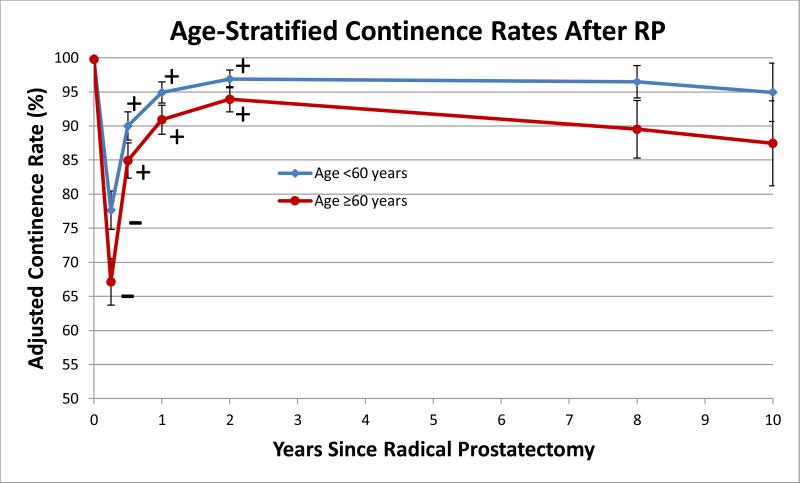
When adjusted continence rates were stratified by age, both groups (<60 and ≥60 yr old) experienced a significant decline between baseline and 3 mo, with subsequent interval improvements until 2 yr after RP (Fig. 4). Continence rates declined by a larger magnitude in men aged ≥60 yr versus <60 yr between both 2 yr and 8 yr (4.4% vs 0.4%) and 8 yr and 10 yr (2.1% vs 1.6%). Continence rates in men aged ≥60 yr marginally but significantly declined from 2 yr to 10 yr (93.9% vs 87.5%; p = 0.047), whereas this rate remained stable in men <60 yr old during this same interval (96.5% vs 94.9%; p = 0.364).
Fig 4.
– Adjusted continence rates following radical prostatectomy, stratified by preoperative age. Error bars represent 95% confidence intervals. RP = radical prostatectomy; + = significant increase in mean University of California, Los Angeles– Prostate Cancer Index urinary function (UCLA-PCI-UFS) from previous time point; – = significant decrease in mean UCLA-PCI-UFS from previous time point.
Regression coefficients and odds ratios are included in Appendix 2.
4. Discussion
Median survival after treatment for prostate cancer is approximately 14 yr [18]. Therefore, it is important to examine quality of life outcomes beyond the 2-yr time frame when initial functional recovery appears to plateau. This is especially important when examining outcomes such as lower urinary tract symptoms (LUTS), erectile and sexual function, and continence, which are also influenced by the natural aging process. Elucidating the long-term impact of RP on continence is important in establishing realistic expectations for men electing surgical treatment of clinically localized prostate cancer. Unfortunately, there is a paucity of outcome studies of continence in the after RP patient beyond 2 yr [3,5,14–16].
There are many strengths of our study, including its prospective design, inclusion of a consecutive cohort of men undergoing RP, use of validated questionnaires at baseline and multiple follow-up intervals, and data management performed without the involvement of the operating surgeon. Ninety-seven percent of men undergoing RP by the operating surgeon signed informed consent, thereby minimizing selection bias.
The only other large prospective assessment of quality of life outcomes at, or beyond, 10 yr following RP is the Prostate Cancer Outcomes Study (PCOS). One limitation of the PCOS is that baseline data were obtained at least 6 mo following RP, introducing recall bias. In addition, the 15-yr PCOS outcome assessment excluded 38% of men who did not respond to the initial surveys at 6 or 12 mo and an unspecified number of men who failed to respond to surveys at 2 and 5 yr. After exclusion of these cases, another 28% were censored due to mortality [14]. By contrast, in calculating our response rate, we considered the entire cohort of men undergoing RP who signed consent. The proportion of this original cohort responding to our long-term outcomes assessment exceeds that of the PCOS. Since the baseline characteristics of those responding and not responding at 10 yr were similar, we attribute any attrition of subjects to random events. Last, we used a regression model that adjusted for key preoperative variables and accounted for repeated observations by factoring in the interdependence between survey responses. Our unstratified analysis of mean UCLA-PCI-UFS is consistent with literature reporting that men undergoing RP experience an immediate decline in continence score, followed by improvement up to 2 yr after RP [19–23]. Continence rates similarly demonstrate declines immediately after surgery and recovery that diminishes over time until around 2 yr after RP [9– 13,24,25]. In the present long-term study, mean UCLA-PCI-UFS declined from 2 yr to 8 yr, and marginally, but significantly, from 8 yr to 10 yr after RP. Men in the PCOS showed similar declines in UCLA-PCI-UFS from 5 yr to 15 yr [14]. Other longitudinal studies using the Expanded Prostate Cancer Index Composite Incontinence subscale, a modified version of the UCLA-PCI-UFI, have reported stable continence between 1 yr and 5 yr [15] and over a median follow-up of 2.6 yr to 6.2 yr [3].
There is no consensus regarding the long-term impact of RP on continence rate. This is due to the paucity of long-term studies and the lack of a universally agreed upon definition of continence. Definitions used in the literature include daily use of no pads [6,10,12], daily use of up to one pad [6,13,26,27], total control or occasional dribbling [9,13,14,28], no problem dripping or leaking urine [26], and leaking once daily [26]. To better identify how men self-define continence status, Lepor et al correlated responses to the UCLA-PCI-UFI and patients’ self-assessments of whether they considered themselves continent or incontinent [29]. At 3 mo and 24 mo following RP, 82.5% and 100% of men using one pad per day considered themselves continent, respectively. Therefore, we considered men continent at 24 mo and beyond who required up to one pad daily.
Continence rates in the present study at 2 yr, 8 yr, and 10 yr following RP were 95.5%, 93.1%, and 91.1%, respectively. Although there appears to be a long-term trend of decreasing continence rates, interval changes in continence rates were not statistically significant. Our observed slight decline in continence rates after 2 yr is consistent with a study by Nandipati et al that showed the proportion of 156 men using one pad per day increased from 12.5% to 17.7% between 2 yr and a mean 7.8 yr of follow-up, respectively [16]. The limitations of this study, however, were the relatively small number of evaluable men, the lack of a prospective design, the potential selection bias due to the unknown number of men undergoing RP, and the lack of statistical analysis to determine the significance of reported changes.
The PCOS also demonstrated a similar decline in long-term continence rates. The definition of incontinence in the PCOS was frequent urinary leakage or no urinary control, a definition that is consistent with patients’ perceptions of being incontinent following RP [29]. In the 15-yr follow-up of the PCOS, incontinence rates increased with time from 9.6% to 13.4% to 18.3% at 2, 5, and 15 yr after RP, respectively [14]. Unfortunately, it is unknown whether this progressive trend in urinary incontinence was statistically significant. The doubling of incontinence rates between 2 yr and 15 yr, however, is of concern.
Our continence rates stratified by age suggested that men ≥60 yr old experience declines in mean UCLA-PCI-UFS between 2 yr and 8 yr, whereas men <60 yr old have stable scores during this interval. Similarly, men ≥60 yr old experience larger absolute declines in continence rates from 2 yr to 8 yr and from 8 yr to 10 yr compared with men <60 yr of age. Only men aged ≥60 yr experienced statistically significant declines in continence rate from 2 to 10 yr, although this change was marginally significant (p = 0.047). The negative effect of age on short-term incontinence rate has been recognized [19,27,28], but ours is the first study to report on this finding at long-term follow-up. Demonstrated declines in UCLA-PCI-UFS or continence rate from 2 yr to 10 yr in our cohort may be attributable to men ≥60 yr of age. Since many men are not followed by urologists long-term after RP, it is important to counsel men ≥60 yr old at the time of RP that they may experience long-term declines in continence.
The UCLA-PCI-UFS comprises five questions related to urinary continence and does not include a single question on LUTS, an important component of urinary function. It is, consequently, of no surprise that studies reporting on continence rate and urinary function based on the UCLAPCI-UFS show similar trends, since they are capturing the same end point. The UCLA-PCI-UFS better resolves statistically significant differences among groups because it is based on five questions about continence. In addition, since it is scored as a continuous variable, it may resolve dynamic changes in continence that are not easily detectable by a binary continence rate.
Our study has several limitations. It is possible that continence was affected between 2 yr and 10 yr because men were being treated for incontinence. Overall, only 20 men (1%) and 26 men (1%) in our cohort underwent treatment with a male sling or artificial urethral sphincter, respectively, so this is unlikely to have changed our results meaningfully. In addition, our study lacks a control group, so it is unclear if the development of incontinence is due to surgical intervention or the natural history of sphincteric or bladder dysfunction. Furthermore, our results are from patients undergoing open RP. Since the overwhelming majority of studies show no difference in continence outcomes between open and robot-assisted RP, we are confident that our results apply to men undergoing robot-assisted RP [30]. Finally, the outcomes presented here reflect those of a highly experienced surgeon and, therefore, may not be generalizable to all men undergoing RP.
5. Conclusions
Between 2 yr and 10 yr after RP, there are slight decreases in mean UCLA-PCI-UFS and continence rate, with only the interval changes in mean UCLA-PCI-UFS being statistically significant. Younger men have better long-term outcomes. The results of these analyses are relevant to the pre- and postoperative counseling of men diagnosed with prostate cancer and may provide realistic long-term expectations for men undergoing RP.
Take-home message.
In this long-term, prospective, longitudinal outcomes study of men undergoing open radical prostatectomy, we demonstrated that from 2 yr to 10 yr following surgery, men generally experience declines in continence. These declines are more prominent among men ≥60 yr old.
Acknowledgments
Funding/Support and role of the sponsor: This study was supported in part by grant UL1 TR000038 from the National Center for the Advancement of Translational Science, US National Institutes of Health, to Vinay Prabhu.
Appendix 1 – University of California, Los Angeles-Prostate Cancer Index (UCLA-PCI) Urinary Function Index
1. Over the last 4 weeks, how often have you leaked urine?
_Every day (0)
_About once a week (33)
_Less than once a week (66)
_Not at all (100)
2. Which of the following best describes your urinary control during the last 4 weeks?
_No control whatsoever (0)
_Frequent dribbling (33)
_Occasional dribbling (66)
_Total control (100)
3. How many pads or adult diapers per day did you usually use to control leakage duringthe last 4 weeks?
_3 or more pads per day (0)
_1–2 pads per day (50)
_No pads (100)
4. How big a problem, if any, has each of the following been for you during the last 4 weeks?
a. Dripping urine or wetting your pants?
_No problem (100)
_Very small problem (75)
_Small problem (50)
_Moderate problem (25)
_Big problem (0) b. Urine leakage interfering with your sexual activity?
_No problem (100)
_Very small problem (75)
_Small problem (50)
_Moderate problem (25)
_Big problem (0)
The UCLA-PCI urinary function score is calculated as an average score of the values listed above. If more than 50% of the items are missing from the scale, the score cannot be calculated.
Appendix
Appendix 2.
Regression results for urinary function and continence *
| Model | 1 | 2 |
|---|---|---|
| Dependent variable | Mean UCLA-PCI-UFS ** | Continence § |
| Follow-up period | ||
| 3 mo | Ref. | Ref. |
| 6 mo | 8.62 † | 2.78 † |
| 12 mo | 12.88 † | 5.30 † |
| 2 yr | 15.56 † | 8.52 † |
| 8 yr | 13.53 † | 5.40 † |
| 10 yr | 11.40 † | 4.06 † |
| Observations, no. | 6603 | 6004 |
| Patients, no. | 1626 | 1596 |
| Log likelihood | –2227.26 | |
| r2, within observations | – | 0.22 |
| r2, between observations | – | 0.08 |
| r2, overall | – | 0.10 |
UCLA-PCI-UFS = University of California, Los Angeles-Prostate Cancer Index-urinary function score; Ref = reference.
Adjusted for age at time of radical prostatectomy, preoperative urinary function, preoperative PSA, Gleason score, stage, type of nerve-sparing surgery, race/ethnicity, and marital status. Similar results were obtained when using a dummy variable for age ≥60 yr and the interaction of follow-up period with age ≥60 yr.
Regression coefficient.
Odds ratio.
p < 0.001
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author contributions: Herbert Lepor had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Lepor. Acquisition of data: Laze, Prabhu. Analysis and interpretation of data: Prabhu, Taksler, Sivarajan. Drafting of the manuscript: Prabhu, Lepor. Critical revision of the manuscript for important intellectual content: Sivarajan, Taksler, Lepor. Statistical analysis: Taksler, Prabhu. Obtaining funding: None. Administrative, technical, or material support: None.
Supervision: Lepor. Other (specify): None.
Financial disclosures: Herbert Lepor certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/ affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: Herbert Lepor is co-owner of MedReviews, has been a lecturer for Amgen and a speaker for Watson, is a consultant for and investor in Serenity, and is a consultant for TheraCoat.
References
- 1.Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics. CA Cancer J Clin. 2012;62:220–41. doi: 10.3322/caac.21149. [DOI] [PubMed] [Google Scholar]
- 2.Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol. 2010;28:1117–23. doi: 10.1200/JCO.2009.26.0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller DC, Sanda MG, Dunn RL, et al. Long-term outcomes among localized prostate cancer survivors: health-related quality-of-life changes after radical prostatectomy, external radiation, and brachytherapy. J Clin Oncol. 2005;23:2772–80. doi: 10.1200/JCO.2005.07.116. [DOI] [PubMed] [Google Scholar]
- 4.Abraham NE, Makarov DV, Laze J, Stefanovics E, Desai R, Lepor H. Patient centered outcomes in prostate cancer treatment: predictors of satisfaction up to 2 years after open radical retropubic prostatectomy. J Urol. 2010;184:1977–81. doi: 10.1016/j.juro.2010.06.099. [DOI] [PubMed] [Google Scholar]
- 5.Penson DF, McLerran D, Feng Z, et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the prostate cancer outcomes study. J Urol. 2005;173:1701–5. doi: 10.1097/01.ju.0000154637.38262.3a. [DOI] [PubMed] [Google Scholar]
- 6.Ficarra V, Novara G, Rosen RC, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol. 2012;62:405–17. doi: 10.1016/j.eururo.2012.05.045. [DOI] [PubMed] [Google Scholar]
- 7.Litwin MS, Lubeck DP, Henning JM, Carroll PR. Differences in urologist and patient assessments of health related quality of life in men with prostate cancer: results of the CaPSURE database. J Urol. 1998;159:1988–92. doi: 10.1016/S0022-5347(01)63222-1. [DOI] [PubMed] [Google Scholar]
- 8.Loughlin KR, Prasad MM. Post-prostatectomy urinary incontinence: a confluence of 3 factors. J Urol. 2010;183:871–7. doi: 10.1016/j.juro.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Glickman L, Godoy G, Lepor H. Changes in continence and erectile function between 2 and 4 years after radical prostatectomy. J Urol. 2009;181:731–5. doi: 10.1016/j.juro.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Kundu SD, Roehl KA, Eggener SE, Antenor JA, Han M, Catalona WJ. Potency, continence and complications in 3,477 consecutive radical retropubic prostatectomies. J Urol. 2004;172:2227–31. doi: 10.1097/01.ju.0000145222.94455.73. [DOI] [PubMed] [Google Scholar]
- 11.Penson DF, McLerran D, Feng Z, et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the Prostate Cancer Outcomes Study. J Urol2008. 179(Suppl):S40–4. doi: 10.1016/j.juro.2008.03.136. [DOI] [PubMed] [Google Scholar]
- 12.Walsh PC, Marschke P, Ricker D, Burnett AL. Patient-reported urinary continence and sexual function after anatomic radical prostatectomy. Urology. 2000;55:58–61. doi: 10.1016/s0090-4295(99)00397-0. [DOI] [PubMed] [Google Scholar]
- 13.Lepor H, Kaci L. The impact of open radical retropubic prostatectomy on continence and lower urinary tract symptoms: a prospective assessment using validated self-administered outcome instruments. J Urol. 2004;171:1216–9. doi: 10.1097/01.ju.0000113964.68020.a7. [DOI] [PubMed] [Google Scholar]
- 14.Resnick MJ, Koyama T, Fan KH, et al. Long-term functional outcomes after treatment for localized prostate cancer. N Engl J Med. 2013;368:436–45. doi: 10.1056/NEJMoa1209978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parker WR, Wang R, He C, Wood DP., Jr Five year expanded prostate cancer index composite-based quality of life outcomes after prostatectomy for localized prostate cancer. BJU Int. 2011;107:585–90. doi: 10.1111/j.1464-410X.2010.09579.x. [DOI] [PubMed] [Google Scholar]
- 16.Nandipati KC, Raina R, Agarwal A, Zippe CD. Nerve-sparing surgery significantly affects long-term continence after radical prostatectomy. Urology. 2007;70:1127–30. doi: 10.1016/j.urology.2007.07.042. [DOI] [PubMed] [Google Scholar]
- 17.Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Brook RH. The UCLA Prostate Cancer Index: development, reliability, and validity of a health-related quality of life measure. Med Care. 1998;36:1002–12. doi: 10.1097/00005650-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Walz J, Gallina A, Saad F, et al. A nomogram predicting 10-year life expectancy in candidates for radical prostatectomy or radiotherapy for prostate cancer. J Clin Oncol. 2007;25:3576–81. doi: 10.1200/JCO.2006.10.3820. [DOI] [PubMed] [Google Scholar]
- 19.Huang GJ, Sadetsky N, Penson DF. Health related quality of life for men treated for localized prostate cancer with long-term followup. J Urol. 2010;183:2206–12. doi: 10.1016/j.juro.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gore JL, Kwan L, Lee SP, Reiter RE, Litwin MS. Survivorship beyond convalescence: 48-month quality-of-life outcomes after treatment for localized prostate cancer. J Natl Cancer Inst. 2009;101:888–92. doi: 10.1093/jnci/djp114. [DOI] [PubMed] [Google Scholar]
- 21.Rice K, Hudak J, Peay K, et al. Comprehensive quality-of-life outcomes in the setting of a multidisciplinary, equal access prostate cancer clinic. Urology. 2010;76:1231–8. doi: 10.1016/j.urology.2010.03.087. [DOI] [PubMed] [Google Scholar]
- 22.Knight SJ, Latini DM, Hart SL, et al. Education predicts quality of life among men with prostate cancer cared for in the Department of Veterans Affairs: a longitudinal quality of life analysis from CaPSURE. Cancer. 2007;109:1769–76. doi: 10.1002/cncr.22597. [DOI] [PubMed] [Google Scholar]
- 23.Pardo Y, Guedea F, Aguilo F, et al. Quality-of-life impact of primary treatments for localized prostate cancer in patients without hormonal treatment. J Clin Oncol. 2010;28:4687–96. doi: 10.1200/JCO.2009.25.3245. [DOI] [PubMed] [Google Scholar]
- 24.Sanda MG, Dunn RL, Michalski J, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008;358:1250–61. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- 25.Abdollah F, Sun M, Suardi N, et al. Prediction of functional outcomes after nerve-sparing radical prostatectomy: results of conditional survival analyses. Eur Urol. 2012;62:42–52. doi: 10.1016/j.eururo.2012.02.057. [DOI] [PubMed] [Google Scholar]
- 26.Wei JT, Dunn RL, Marcovich R, Montie JE, Sanda MG. Prospective assessment of patient reported urinary continence after radical prostatectomy. J Urol. 2000;164:744–8. doi: 10.1097/00005392-200009010-00029. [DOI] [PubMed] [Google Scholar]
- 27.Sacco E, Prayer-Galetti T, Pinto F, et al. Urinary incontinence after radical prostatectomy: incidence by definition, risk factors and temporal trend in a large series with a long-term follow-up. BJU Int. 2006;97:1234–41. doi: 10.1111/j.1464-410X.2006.06185.x. [DOI] [PubMed] [Google Scholar]
- 28.Stanford JL, Feng Z, Hamilton AS, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA. 2000;283:354–60. doi: 10.1001/jama.283.3.354. [DOI] [PubMed] [Google Scholar]
- 29.Lepor H, Kaci L, Xue X. Continence following radical retropubic prostatectomy using self-reporting instruments. J Urol. 2004;171:1212–5. doi: 10.1097/01.ju.0000110631.81774.9c. [DOI] [PubMed] [Google Scholar]
- 30.Montorsi F, Wilson TG, Rosen RC, et al. Best practices in robot-assisted radical prostatectomy: recommendations of the Pasadena Consensus Panel. Eur Urol. 2012;62:368–81. doi: 10.1016/j.eururo.2012.05.057. [DOI] [PubMed] [Google Scholar]