Abstract
Purpose
Early recurrence after hepatectomy is a well-known poor prognostic factor in patients with hepatocellular carcinoma. This study was undertaken to identify the risk factors of early recurrence in patients with hepatocellular carcinoma after hepatectomy.
Methods
One hundred and sixty-seven patients that underwent hepatectomy for hepatocellular carcinoma from January 2005 to December 2010 were enrolled. The numbers of patients with or without early recurrence group were 40 and 127, respectively. Clinico-pathologic factors were retrospectively analyzed.
Results
Potential risk factors were classified as host, tumor, or surgical factors. Of the host factors examined, lobular hepatitis activity was found to be a significant risk factor of early recurrence, and of the tumor factors, infiltrative type of gross appearance, level of preoperative AFP and worst Edmondson-Steiner grade were significant.
Conclusion
The present study shows that an infiltrative gross appearance, a high preoperative AFP level, high lobular hepatitis activity, and a poor Edmondson-Steiner grade are independent risk factors of early recurrence. Accordingly, patients with these risk factors should be followed closely after hepatectomy.
Keywords: Hepatocellular carcinoma, Recurrence, Hepatectomy
INTRODUCTION
Hepatic resection is a curative treatment is performed preferentially for hepatocellular carcinoma (HCC) patients with a well-preserved liver function. Overall survival rates have been reported to depend on several factors, such as, tumor size, treatment modality, degree of cirrhosis, and portal hypertension, and 5-year survival after hepatic resection has been reported to be 25%-74%, but as high as 93% among selected patients [1].
Intrahepatic recurrence occurs in 70%-80% of patients within 5 years of surgery, and is known to be the strongest risk factor of poor survival after surgical treatment [1,2,3,4,5]. This recurrence can be divided into early and late recurrence according to time elapsed between surgery and the recurrence, and early recurrence (ER) is a well-known independent prognostic factor in HCC patients that have undergone hepatic resection [5,6,7].
This study was performed to identify the risk factors of ER after hepatectomy in patients with HCC.
METHODS
This retrospective study was conducted on 167 patients that underwent hepatic resection for histopathologically diagnosed HCC from January 1, 2005 to December 30, 2010. Subjects were divided into two groups; those that developed intrahepatic recurrence within one year of hepatic resection were allocated to the ER group (n = 40) and the others were allocated to the nonearly recurrence (NER) group (n = 127). The NER group consisted of 44 patients who developed recurrence more than one year later and 83 patients that did not develop recurrence during follow-up; the mean follow-up period was 39.9 months.
Intrahepatic recurrence was determined using blood test results, such as, serum AFP level, PIVKA-II, and abdominal ultrasonography and CT or MRI findings, and when necessary was confirmed by angiography. Potential risk factors of recurrence were classified as host, tumor, or surgical factors.
All histopathologic findings are described according to the guidelines issued by The Korean Liver Cancer Study Group. In patients with more than two tumors, the tumor with the poorest Edmondson-Steiner (E-S) grade was taken to be representative and when tumor had the same E-S grade, the largest tumor was chosen. In addition, hepatitis severity was described using grade of hepatitis activity and stage of cirrhosis. And, grade of hepatitis activity were evaluated using lobular and porto-periportal activities, as described by the guideline issued by the Korean Society of Pathologists [8,9].
Results were expressed as a mean ± standard deviation. Differences between group discontinuous variables were analyzed using the chi-square test and Fisher exact test, as appropriate. Multivariate analysis was performed using logistic regression analysis to identify variables independently associated with recurrence from among those found to be significant by univariate analysis. Survival rates were analyzed by using Kaplan-Meier curves and the log rank test was used to compare group survival rates. The analysis was performed using IBM SPSS ver. 19.0 (IBM Co., Armonk, NY, USA) using a significance level of 5% (P < 0.05).
RESULTS
Host factors
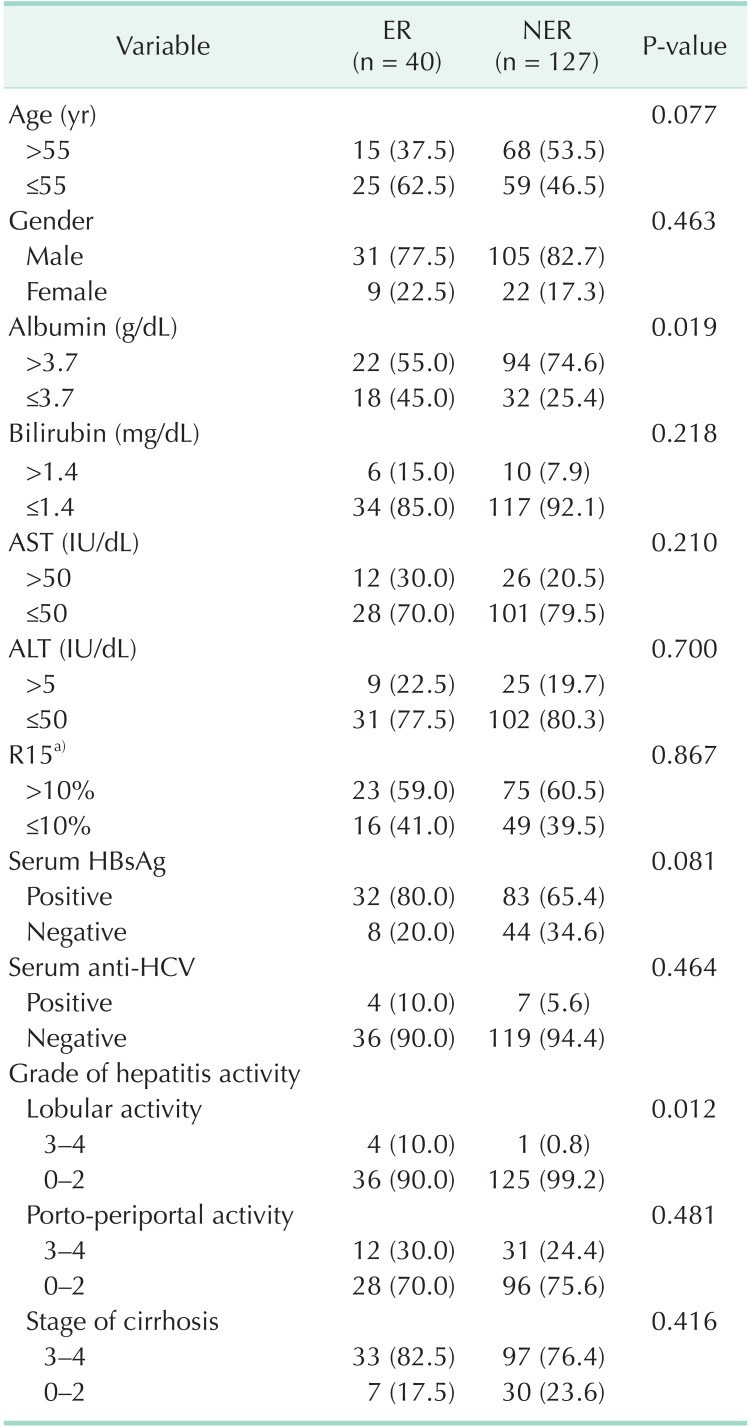
Of the host factors, a high grade of lobular activity was more prevalent in the ER group than in the NER group (10.0% vs. 0.8%, P = 0.012).
However, no significant difference was found for ages, sex, serum albumin levels, presences of hepatitis B and C, portoperiportal activity of the hepatitis and the stages of cirrhosis between ER and NER group (Table 1).
Table 1.
Comparison of clinicopathologic host factors in the early recurrence group (ER) and the nonearly recurrence group (NER)
Values are presented as number (%).
R15, indocyanine green dye retention rate at 15 minutes.
a)Data was unavailable for 4 patients (1 in ER, 3 in NER).
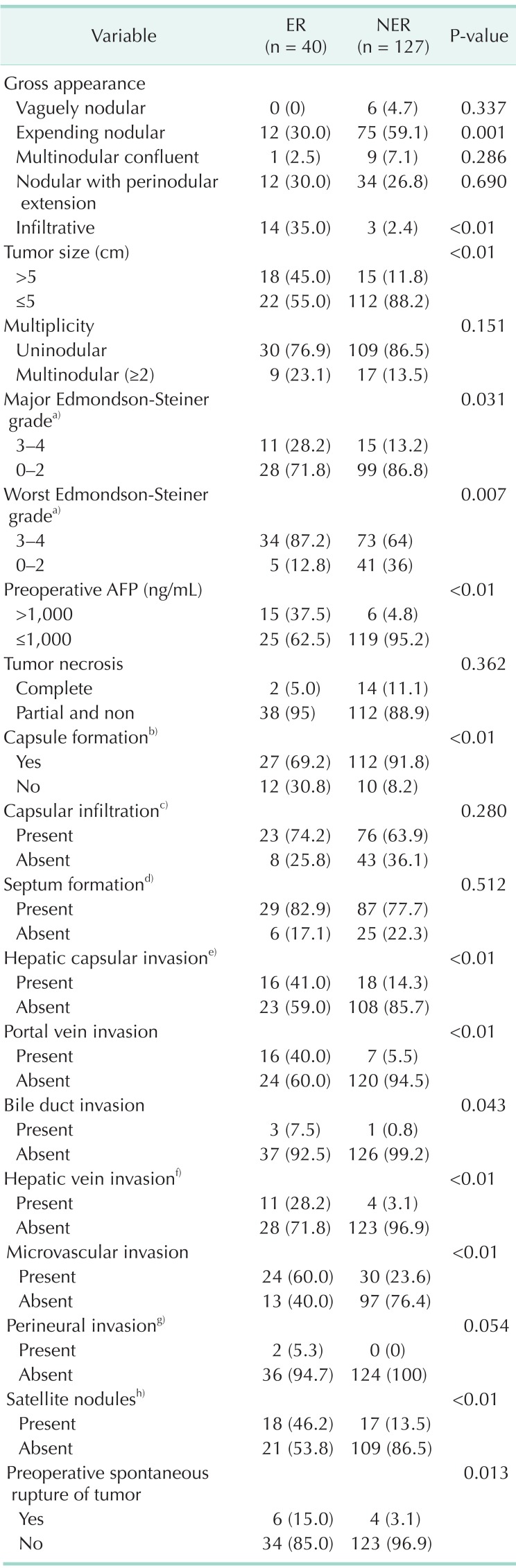
Tumor factors
Of the tumor factors, gross appearance and sizes of tumors, E-S grade, preoperative AFP level, presence of capsules, portal vein invasion, bile duct invasion, hepatic vein invasion, microvascular invasion, and preoperative spontaneous tumor rupture were significantly related with ER. However, no significant association was observed between tumor multiplicity, tumor necrosis, capsular infiltration, septal formation, or perineural invasion and ER.
Regarding gross findings, the expanding nodular tumor type was more prevalent in the NER group (P = 0.001) than in the ER group. In contrast, infiltrative type was more prevalent in the ER group (P < 0.01). No significant intergroup differences were observed for the vaguely nodular type, multinodular confluent type, or nodular type with perinodular extension.
E-S grades were classified a worst and major as described by the guidelines issued by the Korean Liver Cancer Study Group. The worst grade was more significantly prevalent than the major grade in the ER group (P = 0.031 vs. P = 0.007) (Table 2).
Table 2.
Comparison of clinicopathologic tumor factors in the early recurrence group (ER) and the nonearly recurrence group (NER)
Values are presented as number (%).
a)Data was unavailable for 14 patients due to total tumor necrosis. b-h)Data was unavailable for 6, 17, 20, 2, 1, 5, and 2 patients, respectively.
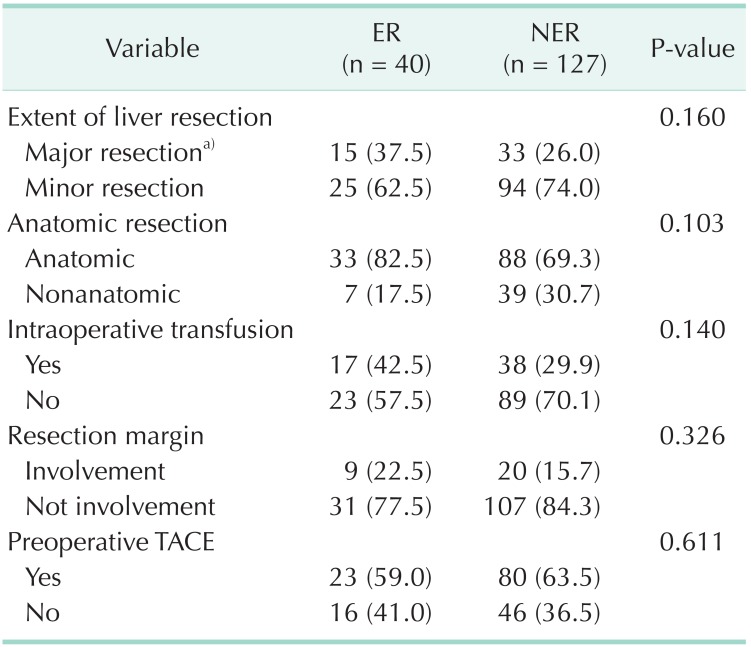
Surgical factors
Extent of liver resection (minor vs. major), anatomical resection, intraoperative blood transfusion, tumor infiltration of resection margin, and preoperative transarterial chemoembolization were not found to be significantly related to ER (Table 3).
Table 3.
Comparison of clinicopathologic surgical factors with in thearly recurrence group (ER) and the nonearly recurrence group (NER)
Values are presented as number (%).
TACE, transarterial chemoembolization.
a)More than three segments were resected.
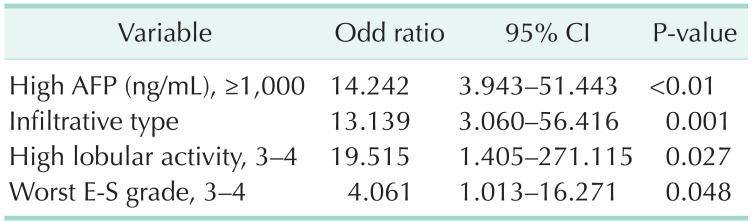
Independent risk factors
Multivariate regression analysis showed that an infiltrative type, a higher preoperative AFP, a higher lobular activity, and a poor E-S grade in the worst part of tumors were independent risk factors of ER (Table 4).
Table 4.
Multivariate analysis of clinicopathologic factors of early recurrence after hepatectomy
CI, confidence interval; E-S grade, Edmondson-Steiner grade.
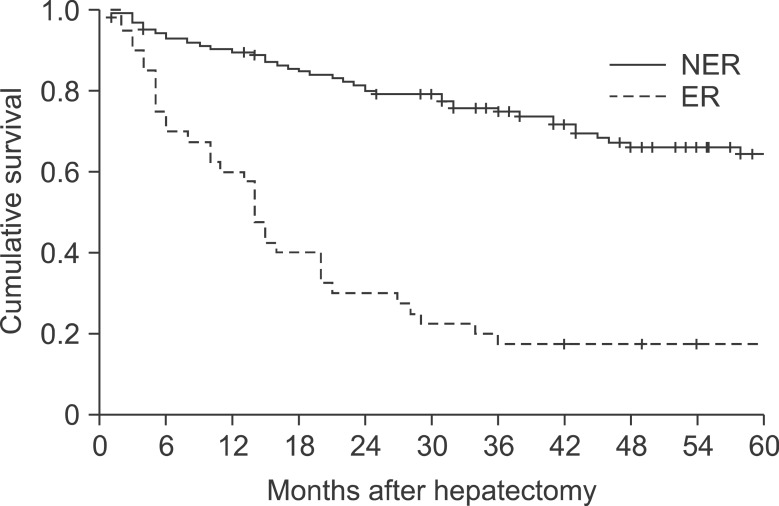
Overall survival rates
Survival rates of 1- and 3-year were 60.0% and 17.5% in ER group and 90.0% and 74.8% in NER group, which showed significant differences between groups, respectively (P < 0.01) (Fig. 1).
Fig. 1.
Cumulative survivals in the early recurrence group (ER) and the nonearly recurrence group (NER).
DISCUSSION
Intrahepatic recurrence often occurs in HCC patients after hepatic resection, and can be divided into intrahepatic metastasis caused by the primary tumor and newly developed multicentric occurrence caused by carcinogenesis in the remnant liver after surgery [3,4,10]. The risk factors of recurrence in the patients with HCC also can be classified as tumor, host, and surgical factors. Intrahepatic metastasis and multicentric occurrence are referred to as tumor and host factors, respectively. Furthermore, when intrahepatic recurrence is divided into early and late recurrence about a cutoff of one or two years, ER appears to be caused by intrahepatic metastasis related to tumor factors and late recurrence to be caused by multicentric occurrence related to host factors. ER is known to be a poor prognostic factor in HCC patients after hepatic resection [4,5,6,11]. In the present study, ER was defined as recurrence within one year of resection.
Several studies have concluded that tumor gross appearance of tumor is prognostically important [12,13,14]. In the case of nodular HCC, the tumor capsule acts as a barrier and prevents tumor cells from spreading, but in case of infiltrative HCC cells can infiltrate peritumoral tissues. Furthermore, the unclear boundary in cases of infiltrative HCC makes the disease difficult to diagnose in the early stage by imaging [15,16,17,18,19]. In the present study, an infiltrative gross appearance was found to be an important risk factor of ER by univariate and multivariate analyses. In addition, 88% of patients with infiltrative HCC developed recurrence within one year, and for the 17 patients with infiltrative HCC, median disease-free survival and median overall survival were only three (1-26 months) and six months (2-49 months), respectively, and one and two year survival rate were only 23.5% and 11.7%.
AFP has been used as the important tumor marker for the patients with HCC and is also known to be the important prognostic factor [20,21], and a high AFP level has also been reported to be a risk factor of ER, but the cutoff values used by authors differ appreciably [12,20]. When Nomura et al. [22] classified AFP as <20 ng/mL, 20-1,000 ng/mL, or >1,000 ng/mL, patients with levels of <20 ng/mL or 20-1000 ng/mL showed similar survival rates, but patient with a level of >1 000 ng/mL had significantly lower survival rates than patients in either of the two lower classes. In the present study, multivariate analysis based on an AFP cutoff of 100 ng/mL showed no significant difference, but analysis based on a cutoff of 1,000 ng/mL showed that AFP level is a significant, independent risk factor of ER.
Histological grade (E-S) and its relation with ER are different depending on each reporter [23,24,25]. In this study, poor E-S grade acted as the important risk factor of ER. More than anything else, this study divide E-S grade into worst grade and major grade and the former showed the higher relation with ER than the latter. (P = 0.007 vs. P = 0.031).
Hepatitis and cirrhosis are a host factor and known to be the risk factors of intrahepatic recurrence related to multicentric occurrence [5,24]. The present study shows that hepatitis B, hepatitis C, porto-periportal activity grade, and stage of cirrhosis are not related to ER. However, interestingly, a high lobular activity grade in hepatitis was found to be a risk factor of ER by univariate and multivariate analysis. That is to say, porto-periportal activity seems to affect developing HCC by the carcinogenesis following the occurrence of cirrhosis and its progress. On the other hand, severe lobular activity that shows extensive necrosis in lobules and con?uent necrosis from the central vein seems to be related to the development of HCC not only through the destruction of hepatic lobular structure from the portal-central septum but also accelerates the regeneration of hepatocytes and genetic alteration after vigorous and massive hepatocellular damage [26,27]. Therefore, the high lobular activity grade is supposed to be related to ER.
In conclusion, ER is an important prognostic factor in patients with HCC. The present study shows that the tumor factors, infiltrative gross appearance, a high AFP level (>1,000 ng/mL) and a poor E-S grade in the worst part of tumor, and the host factor, a high lobular activity grade, are independent risk factors of ER. Accordingly in the case of the patients with HCC with these risk factors, intensive follow-up is required for about one year after surgery.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003;362:1907–1917. doi: 10.1016/S0140-6736(03)14964-1. [DOI] [PubMed] [Google Scholar]
- 2.Bruix J, Sherman M Practice Guidelines Committee, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–1236. doi: 10.1002/hep.20933. [DOI] [PubMed] [Google Scholar]
- 3.Poon RT, Fan ST, Lo CM, Liu CL, Wong J. Intrahepatic recurrence after curative resection of hepatocellular carcinoma: long-term results of treatment and prognostic factors. Ann Surg. 1999;229:216–222. doi: 10.1097/00000658-199902000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38:200–207. doi: 10.1016/s0168-8278(02)00360-4. [DOI] [PubMed] [Google Scholar]
- 5.Poon RT, Fan ST, Ng IO, Lo CM, Liu CL, Wong J. Different risk factors and prognosis for early and late intrahepatic recurrence after resection of hepatocellular carcinoma. Cancer. 2000;89:500–507. [PubMed] [Google Scholar]
- 6.Shah SA, Greig PD, Gallinger S, Cattral MS, Dixon E, Kim RD, et al. Factors associated with early recurrence after resection for hepatocellular carcinoma and outcomes. J Am Coll Surg. 2006;202:275–283. doi: 10.1016/j.jamcollsurg.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 7.Sakon M, Umeshita K, Nagano H, Eguchi H, Kishimoto S, Miyamoto A, et al. Clinical significance of hepatic resection in hepatocellular carcinoma: analysis by disease-free survival curves. Arch Surg. 2000;135:1456–1459. doi: 10.1001/archsurg.135.12.1456. [DOI] [PubMed] [Google Scholar]
- 8.The Korean Liver Cancer Study Group. The general rules for the study of primary liver cancer. 2nd ed. Seoul: The Korean Liver Cancer Study Group; 2004. [Google Scholar]
- 9.Park YN, Kim HG, Chon CY, Park JB, Sohn JH, Yang SH, et al. Histological grading and staging of chronic hepatitis standardized guideline proposed by the Korean study group for the pathology of digestive diseases. Korean J Pathol. 1999;33:337–346. [Google Scholar]
- 10.Tung-Ping Poon R, Fan ST, Wong J. Risk factors, prevention, and management of postoperative recurrence after resection of hepatocellular carcinoma. Ann Surg. 2000;232:10–24. doi: 10.1097/00000658-200007000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu JC, Huang YH, Chau GY, Su CW, Lai CR, Lee PC, et al. Risk factors for early and late recurrence in hepatitis B-related hepatocellular carcinoma. J Hepatol. 2009;51:890–897. doi: 10.1016/j.jhep.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Choi GH, Han DH, Kim DH, Choi SB, Kang CM, Kim KS, et al. Outcome after curative resection for a huge (>or=10 cm) hepatocellular carcinoma and prognostic significance of gross tumor classification. Am J Surg. 2009;198:693–701. doi: 10.1016/j.amjsurg.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 13.Shimada M, Rikimaru T, Hamatsu T, Yamashita Y, Terashi T, Taguchi K, et al. The role of macroscopic classification in nodular-type hepatocellular carcinoma. Am J Surg. 2001;182:177–182. doi: 10.1016/s0002-9610(01)00682-1. [DOI] [PubMed] [Google Scholar]
- 14.Hui AM, Takayama T, Sano K, Kubota K, Akahane M, Ohtomo K, et al. Predictive value of gross classification of hepatocellular carcinoma on recurrence and survival after hepatectomy. J Hepatol. 2000;33:975–979. doi: 10.1016/s0168-8278(00)80131-2. [DOI] [PubMed] [Google Scholar]
- 15.Ng IO, Lai EC, Ng MM, Fan ST. Tumor encapsulation in hepatocellular carcinoma. A pathologic study of 189 cases. Cancer. 1992;70:45–49. doi: 10.1002/1097-0142(19920701)70:1<45::aid-cncr2820700108>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 16.Sasaki Y, Imaoka S, Ishiguro S, Nakano H, Kasugai H, Fujita M, et al. Clinical features of small hepatocellular carcinomas as assessed by histologic grades. Surgery. 1996;119:252–260. doi: 10.1016/s0039-6060(96)80110-3. [DOI] [PubMed] [Google Scholar]
- 17.Adachi E, Maeda T, Kajiyama K, Kinukawa N, Matsumata T, Sugimachi K, et al. Factors correlated with portal venous invasion by hepatocellular carcinoma: univariate and multivariate analyses of 232 resected cases without preoperative treatments. Cancer. 1996;77:2022–2031. doi: 10.1002/(SICI)1097-0142(19960515)77:10<2022::AID-CNCR9>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 18.Demirjian A, Peng P, Geschwind JF, Cosgrove D, Schutz J, Kamel IR, et al. Infiltrating hepatocellular carcinoma: seeing the tree through the forest. J Gastrointest Surg. 2011;15:2089–2097. doi: 10.1007/s11605-011-1614-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kneuertz PJ, Demirjian A, Firoozmand A, Corona-Villalobos C, Bhagat N, Herman J, et al. Diffuse infiltrative hepatocellular carcinoma: assessment of presentation, treatment, and outcomes. Ann Surg Oncol. 2012;19:2897–2907. doi: 10.1245/s10434-012-2336-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li D1, Mallory T, Satomura S. AFP-L3: a new generation of tumor marker for hepatocellular carcinoma. Clin Chim Acta. 2001;313:15–19. doi: 10.1016/s0009-8981(01)00644-1. [DOI] [PubMed] [Google Scholar]
- 21.Peng SY, Chen WJ, Lai PL, Jeng YM, Sheu JC, Hsu HC. High alpha-fetoprotein level correlates with high stage, early recurrence and poor prognosis of hepatocellular carcinoma: significance of hepatitis virus infection, age, p53 and beta-catenin mutations. Int J Cancer. 2004;112:44–50. doi: 10.1002/ijc.20279. [DOI] [PubMed] [Google Scholar]
- 22.Nomura F, Ohnishi K, Tanabe Y. Clinical features and prognosis of hepatocellular carcinoma with reference to serum alpha-fetoprotein levels: analysis of 606 patients. Cancer. 1989;64:1700–1707. doi: 10.1002/1097-0142(19891015)64:8<1700::aid-cncr2820640824>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 23.Kumada T, Nakano S, Takeda I, Sugiyama K, Osada T, Kiriyama S, et al. Patterns of recurrence after initial treatment in patients with small hepatocellular carcinoma. Hepatology. 1997;25:87–92. doi: 10.1053/jhep.1997.v25.pm0008985270. [DOI] [PubMed] [Google Scholar]
- 24.Li SL, Su M, Peng T, Xiao KY, Shang LM, Xu BH, et al. Clinicopathologic characteristics and prognoses for multicentric occurrence and intrahepatic metastasis in synchronous multinodular hepatocellular carcinoma patients. Asian Pac J Cancer Prev. 2013;14:217–223. doi: 10.7314/apjcp.2013.14.1.217. [DOI] [PubMed] [Google Scholar]
- 25.Zhou YM, Yang JM, Li B, Yin ZF, Xu F, Wang B, et al. Risk factors for early recurrence of small hepatocellular carcinoma after curative resection. Hepatobiliary Pancreat Dis Int. 2010;9:33–37. [PubMed] [Google Scholar]
- 26.Lee SH, Chung YH, Kim JA, Jin YJ, Park WH, Choi JG, et al. Histological characteristics predisposing to development of hepatocellular carcinoma in patients with chronic hepatitis B. J Clin Pathol. 2011;64:599–604. doi: 10.1136/jclinpath-2011-200036. [DOI] [PubMed] [Google Scholar]
- 27.Park BK, Park YN, Ahn SH, Lee KS, Chon CY, Moon YM, et al. Long-term outcome of chronic hepatitis B based on histological grade and stage. J Gastroenterol Hepatol. 2007;22:383–388. doi: 10.1111/j.1440-1746.2007.04857.x. [DOI] [PubMed] [Google Scholar]