Abstract
Purpose
Bariatric surgery has become more prevalent owing to the worldwide obesity epidemic. With the growing number of bariatric procedures performed annually, the requirement for revisional and secondary operations is increasing accordingly. This study aimed to evaluate the initial experience of revisional bariatric surgery at a single specialized center.
Methods
A retrospective review of the prospectively established database identified all patients who underwent revisional bariatric surgery between January 2008 and August 2013. The causes, surgical outcomes, and efficacy of the revisional surgeries were analyzed.
Results
Twenty-two revisional surgeries were performed laparoscopically during the study period (13 laparoscopic adjustable gastric banding, 9 laparoscopic sleeve gastrectomy). The most common indication for revision was weight regain or insufficient weight loss (12/23, 52.2%), and Roux-en-Y gastric bypass (RYGB) was the most commonly performed secondary procedure (17/23, 73.9%, including four resectional RYGB procedures). Gastric pouch leak occurred in one patient following revisional RYGB, which required reoperation on the first postoperative day. The mean body mass index decreased from 35.9 to 28.8 kg/m2 at a mean follow-up period of 10 months after revision. The percent excess weight losses at 1, 3, 6, and 12 months postoperatively were 18.8%, 41.1%, 40.1%, and 47.4%, respectively.
Conclusion
Revisional bariatric surgery can be successfully performed via a laparoscopic approach with acceptable risk. Deliberate selection for the proper revisional procedure can efficiently manage undesirable results from the primary surgery.
Keywords: Morbid obesity, Bariatric surgery, Gastric bypass, Reoperation
INTRODUCTION
Obesity has become one of the most important public health problems worldwide. Bariatric surgery has become more prevalent due to the worldwide obesity epidemic, and several studies have demonstrated that it is the most effective therapy for achieving sustained weight loss and managing obesity-related comorbidities. Based upon the results of these studies, the number of bariatric procedures performed worldwide has markedly increased over the last decade. However, there is currently no ideal bariatric procedure for every patient, and all bariatric surgical procedures have an associated failure rate requiring revisional surgery. With the increasing demand for bariatric surgery, a growing number of patients require revisional surgery owing to the undesirable results of their primary bariatric procedure.
Bariatric surgery was adopted relatively recently in Asian countries and in South Korea because the prevalence of obesity (body mass index [BMI] > 30 kg/m2) in the Korean population is less than 5% according to data from the Korean National Health and Nutritional Examination Survey [1]. This rate is much lower than that in western countries; as such, the need for its management is not well recognized. Nevertheless, the obese population in Korea has been markedly increasing due to lifestyle changes such as increased energy intakes and decreased physical activity. Since the first bariatric surgery was performed in 2003, the number of bariatric surgeries performed in South Korea has exponentially escalated along with the trend in Asia and recently surpassed 1,000 cases annually. Thus, the demand for revisional surgery is expected to increase accordingly.
Here, we review our initial experience with revisional bariatric surgery at a single specialized bariatric center of a tertiary referral institution in South Korea. This study aimed to review the indications for revisional bariatric surgery and assess the short-term surgical outcomes.
METHODS
A prospectively maintained database of all patients undergoing bariatric surgery at our Metabolic and Bariatric Center was thoroughly reviewed and all patients who underwent revisional bariatric surgery between January 2008 and August 2013 were identified. Patient demographics, weight, and BMI at the time of the operation, types of initial and revisional operations, indication for revision, surgical outcomes, and follow-up data were retrospectively reviewed in all the patients.
All of the patients underwent a thorough preoperative evaluation before making a decision on revisional surgery. A detailed history was taken regarding weight progress after primary bariatric surgery, dietary habits, changes in comorbidities, and psychosocial factors. In addition, all the patients underwent an upper gastrointestinal (GI) endoscopy or contrast upper GI study to evaluate the possible anatomic changes after primary surgery.
Operative procedures
All the procedures were performed via the laparoscopic approach by a single surgeon with sufficient experience. Sleeve gastrectomy (SG) could be easily converted to Roux-en-Y gastric bypass (RYGB) by transecting the sleeved stomach to create a gastric pouch and then with similar following of the usual RYGB procedures. In cases of failed laparoscopic adjustable gastric banding (LAGB), the band was identified by intraoperative following of the band tube. Dense adhesion around the device, especially to the left lobe of the liver, was carefully dissected, and the fibrotic capsule of the band was released to isolate the band. Previously placed gastro-gastric sutures were identified and separated with caution. Once the band was freely mobilized, the device was then either unbuckled or transected and then removed. The remnant fibrotic capsule was removed as thoroughly as possible to prevent further adhesion or stricture after the secondary operation.
If the patient was scheduled for a single-stage operation, further procedures were continued following band removal. In case of conversion to RYGB, dissection on the lesser curvature of the stomach was carried out approximately 1-2 cm below the location where the band was placed to create a new gastric pouch. Care was taken to save the arterial blood supply to the new gastric pouch. The stomach was then transected below the scar tissue of the band, and the gastric pouch was created using laparoscopic linear staplers. After creating a gastric pouch, the following procedures were similar to those of well-known primary RYGB. In the conversion to SG, the stomach was restored to the normal anatomic position after the band device was removed, and then dissection along the greater curvature was carried out up to the angle of His. Longitudinal gastric resection was done using laparoscopic linear staplers under the guidance of a bougie tube as usual.
Selection of the staple loads depended on the condition of the gastric wall. Generally, a staple height of 4.8 mm was chosen because of the thickened gastric wall. Anastomotic or staple-line leakage was assessed with air or methylene blue-stained saline injection into the gastric pouch. All of the staple lines on the stomach and anastomoses involving the gastric wall were reinforced with either the interrupted method or running sutures to avoid possible postoperative leakage.
In cases of two-stage revision from LAGB, the band was removed in the first procedure, while the revisionary operation, that is, SG or RYGB, was performed 2-3 months later after recovery of the stomach wall. The procedures themselves were the same as those in the single-stage operations. These two-staged operations were nevertheless counted as a single revision in the statistics.
Postoperative management and follow-up
The patients initiated oral intake on the first postoperative day after the absence of anastomotic leakage was confirmed by contrast upper GI study and were discharged once they had achieved adequate oral intake, their pain was under control, and they were ambulating without difficulty. The postoperative nutritional regimen was similar to that of primary surgery and consisted of a liquid or soft diet for the first 3 weeks with gradual increases in food texture thereafter. Patients returned to the outpatient clinic 2 weeks after surgery and then every 3 months for the first postoperative year to monitor weight loss, appetite, dysphagia or food intolerance, eating behavior, comorbidity status, and the presence of any complications. Follow-up was then decreased to every 12 months after the first year. Telephone interviews were also used to monitor patients who could not visit the outpatient clinic. Inadequate weight loss was defined as percent of excess weight loss (%EWL) less than 50% or BMI of 35 kg/m2 and over at one year or more after the surgery.
Statistical analysis
Microsoft Excel (Microsoft Co., Redmond, WA, USA) was used for the data management. Data are presented as median (range) for continuous variables and frequency percentages for categorical variables. The ideal body weight of each patient was estimated based on the formula that corresponds to the midpoint of the medium frame of the Metropolitan tables. The degree of weight loss was assessed with %EWL and percent of excess BMI loss (%EBL), which were calculated using the following formulas [2]:
RESULTS
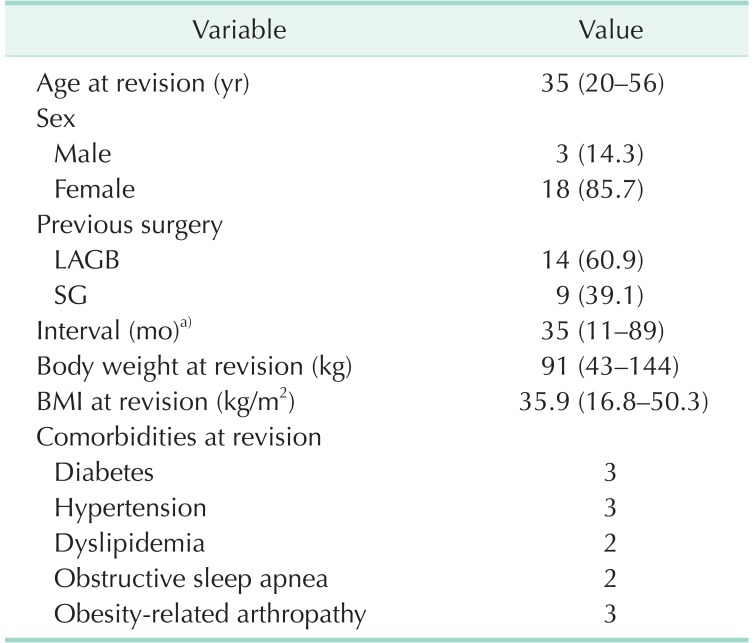
Twenty-two revisional surgeries in 21 patients were performed during the study period. The patients' clinical characteristics before revisional surgery are shown in Table 1. The patients included three men (14.3%) and 18 women (85.7%). The previous bariatric procedure was LAGB in 13 cases and laparoscopic SG in nine cases. Sixteen (72.7%) underwent LAGB or SG at an outside institution and then came under our care, while two patients had more than one previous bariatric procedure. The mean time interval from the previous bariatric surgery to revisional surgery was 35 months, while the mean BMI at revision was 35.9 kg/m2.
Table 1.
Prerevision baseline characteristics (22 surgeries in 21 patients)
Values are presented as median (range) or number (%).
LAGB, laparoscopic adjustable gastric banding; SG, sleeve gastrectomy; BMI, body mass index.
a)Defined as the period from previous bariatric surgery to revisional surgery.
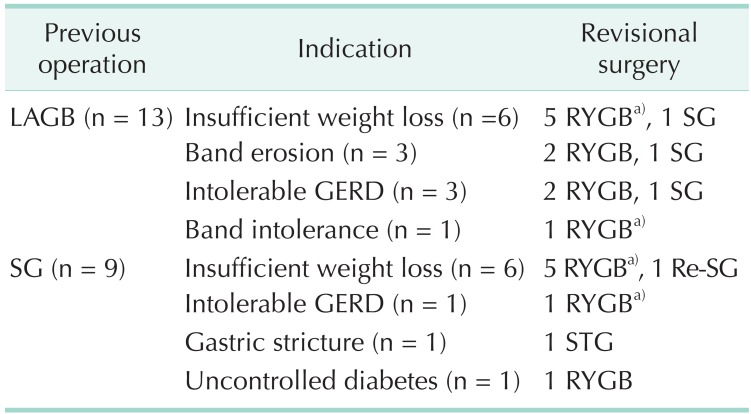
The most common primary indication for revisional surgery was inadequate weight loss after LAGB (n = 6, 46.2%) or SG (n = 6, 66.7%; Table 2). Other indications after failed LAGB include direct band-related complications such as band erosion or intolerable reflux symptoms after adjustment and psychological band intolerance. Three other patients decided to undergo revisional bariatric surgery after primary SG because of intolerable reflux symptoms, gastric stricture and uncontrolled diabetes along with insufficient weight loss.
Table 2.
Indications for revisional bariatric surgery (23 surgeries in 22 patients)
Band removal converted to other surgical options after a certain period of time, which were two surgical procedures in the same patient at different time points, is counted as one.
LAGB, laparoscopic adjustable gastric banding; RYGB, Roux-en-Y gastric bypass; SG, sleeve gastrectomy; GERD, gastroesophageal reflux disease; STG, subtotal gastrectomy.
a)Including one patient who underwent resectional RYGB in each category.
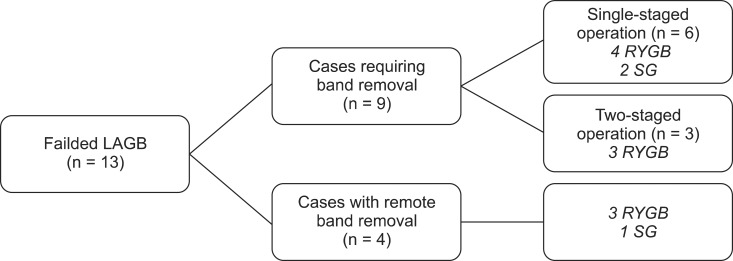
Detailed flow of the revisional procedures following failed LAGB are shown in Fig. 1. Four patients who had band erosion (n = 3) or severe reflux (n = 1) and underwent band removal at other clinics visited our institution because of eventual weight regain with the lapse of time after band removal. The other 9 patients required band removal; gastric band was removed at the same time as the conversion to other bariatric procedures in the former six patients, while the latter three patients underwent band removal followed by revisional procedures with an interval of 2-3 months between procedures.
Fig. 1.
Revisional procedures following failed laparoscopic adjustable gastric banding (LAGB), Roux-en-Y gastric bypass (RYGB), or sleeve gastrectomy (SG).
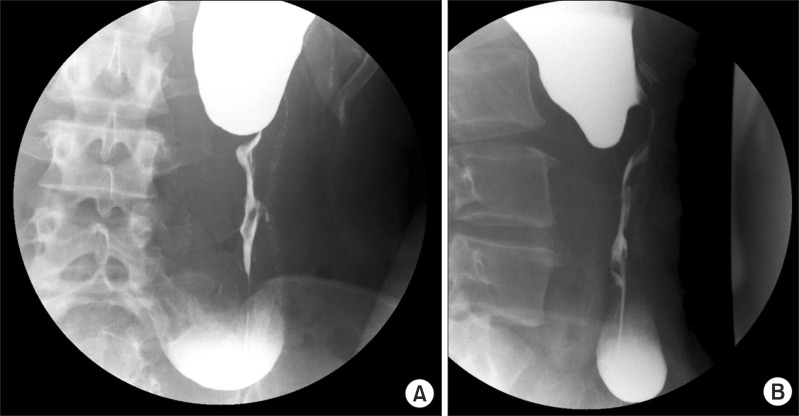
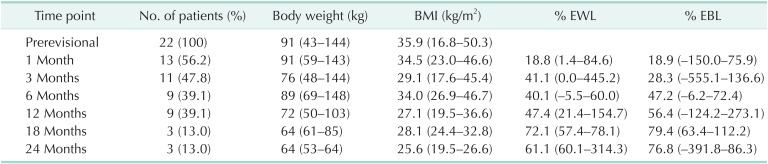
One patient was referred to our institution for persistent postprandial vomiting and abdominal discomfort after SG. The patient had a history of previous LAGB followed by band removal due to gastric stricture even before undergoing SG. A contrast upper GI study revealed a gastric stricture at a midbody of the stomach with marked dilatation of the proximal portion (Fig. 2). Her BMI at revision was 16.8 kg/m2. The patient was converted to laparoscopic subtotal gastrectomy and her BMI increased to 20.3 kg/m2 at the 5-year postoperative time point without any long-term complications.
Fig. 2.
Contrast upper gastrointestinal series of a patient who developed gastric stricture following laparoscopic sleeve gastrectomy. (A) AP view, (B) lateral view.
One female patient received two revisional surgeries. She required revisional surgery after LAGB due to inadequate weight loss and her BMI at first revision was 35.7 kg/m2. She chose to undergo SG according to her preference. After revisional SG, her BMI and %EWL reached 30.4 kg/m2 and 41.1%, respectively, during the initial 3 months postoperatively, but did not changed thereafter. She also complained about persistent reflux symptoms and requested another revision. She underwent secondary revisional surgery and converted to RYGB 1 year after the primary revision. Her BMI was 25.6 kg/m2 at 2 years after the secondary revision.
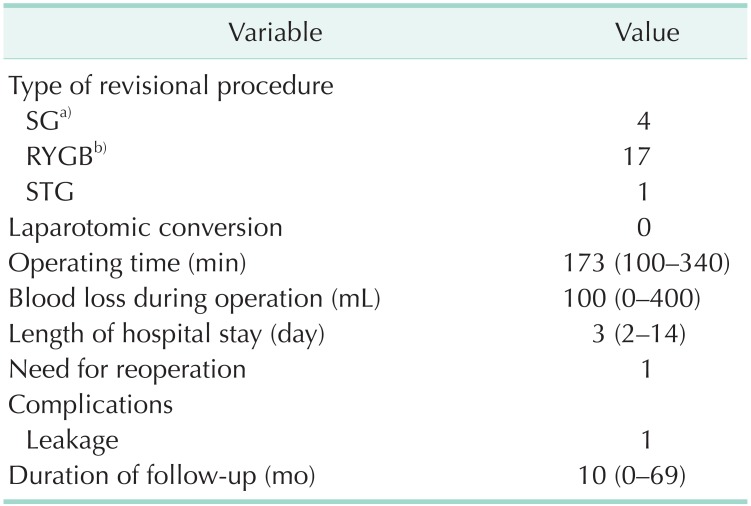
The most commonly selected procedure for revision was RYGB (17/22, 77.3%; Table 3). Resectional RYGB, in which the remnant stomach was completely removed, was performed in four patients who seriously feared possible cancer occurrence in the remnant stomach. All revisional operations were successfully performed using a laparoscopic approach without laparotomic conversion, and the patients were discharged at an average of 3 postoperative days. Anastomosis site bleeding was noticed in one patient during an RYGB procedure and was well managed with intraoperative endoscopic intervention. Gastric pouch leak developed in one patient after revisional RYGB and required reoperation of the primary repair with external drainage on the first postoperative day. This patient was discharged on the 14th postoperative day without further complications. There was no surgical mortality.
Table 3.
Short-term surgical outcomes of revisional surgery
Values are presented as number or median (range).
SG, sleeve gastrectomy; RYGB, Roux-en-Y gastric bypass; STG, subtotal gastrectomy.
a)Including one patient who underwent re-sleeve gastrectomy.
b)Including four patients who underwent resectional RYGB.
Detailed weight parameters following revisional surgery are shown in Table 4. The mean BMI decreased from 35.9 to 28.8 kg/m2 at a mean follow-up period of 10 months after revision. The percent of excess weight loss (%EWL) and excess BMI loss (%EBL) reached 47.4% and 56.4%, respectively, at 12 postoperative months in all the patients.
Table 4.
Weight parameters following the 23 revisional surgeries
Values are presented as mean (range) unless otherwise indicate.
BMI, body mass index; EWL, excess weight loss; EBL, excess body mass index loss.
DISCUSSION
As the number of bariatric procedures performed increases, the number of patients requiring revisional procedures continues to rise. Aside from revisional procedures to manage early surgical complications, many patients require a redo operation months or years after the primary surgery for various reasons including insufficient weight loss or weight regain, delayed complications associated with implants, or other intolerable side effects. Revisional bariatric surgery comprises 5%-15% of total cases of bariatric surgery [3,4,5]. The rate of revisional surgery is 20%-60% after LAGB [6,7,8,9,10,11], 9%-17% after RYGB [6,10,12,13], and 9%-11% after SG [14,15]. Although many articles have investigated the results of various bariatric procedures used as the initial surgical intervention for morbid obesity, studies addressing the proper revisional surgery of choice after failed primary surgery remain limited. It is necessary to establish a proper revisionary strategy tailored for various indications to guide bariatric surgeons in the decision-making process after failed primary surgery.
The most frequently adopted bariatric procedure in South Korea is LAGB, which comprises approximately 70% of total national bariatric procedures. The reason for this may be due to its simplicity, reversibility, and relatively low perioperative complications. However, according to many previously published studies, the efficacy of LAGB seems to be limited with a high reoperation rate, and more patients with band device will require revision or conversion to other bariatric procedures in the near future. Several studies have suggested that RYGB or SG could be appropriate revisional procedures after failed LAGB [16,17,18]. Our data also showed that RYGB or SG could successfully manage undesirable results from the primary LAGB.
In our bariatric center, revisional surgery accounted for 4.1% (25/616) of all bariatric surgeries during the study period. A total of 72.7% of those patients undergoing revisional surgery were referred to our institution from outside clinics. Different types of primary surgery lead to different reasons for conversion; however, in our series, insufficient weight loss or regain was the most frequent reason for revisional bariatric surgery, which is in concordance with the findings of other studies. Others were more procedure-specific reasons and gastric band-related complications were the second most common indications for revision among them. However, these indications are not completely independent from each other, and many patients have a combination of these complaints. For example, all the patients who underwent band removal due to implant-related complications in the present study eventually showed weight regain shortly after simple band removal and visited our institution to deal with rebound obesity. Consequently, a total of 71.4% (15/21) of all the patients who demanded revisions had weight problems, that is, inadequate weight loss or weight regain. It has already been established that simple band removal is technically the easiest procedure to manage band-related complications, but this intervention invariably leads to weight regain and the recurrence of obesity-related comorbidities [19,20].
The reoperative procedure of choice should depend on several factors, including patient history and intraoperative findings. If the initial LAGB achieved adequate weight loss but failure occurred due to band slippage or pouch dilatation, similar weight loss can be expected for reoperation with a different restrictive procedure; therefore, SG would be a reasonable alternative [20,21]. However, when the major reason for considering revisional surgery is weight regain or inadequate weight loss, the commonly advocated key principle is to convert a purely restrictive procedure to include malabsorptive components [21]. In our series, all of the primary procedures requiring revisions were purely restrictive and they were selectively converted to SG or RYGB considering the respective indications. The priority was usually given to RYGB, to which most of the patients were converted, although some underwent revisional SG mainly due to their preference. The only exception was the first patient of this series, who developed gastric stricture after revisional SG and was converted to laparoscopic subtotal gastrectomy when the surgeon was completely inexperienced. To date, there have been no patients who required revisional surgery after RYGB at our center, probably due to our rather short history of experience with bariatric surgery.
Revisional bariatric surgery is complex and technically demanding. It is generally associated with a higher risk of postoperative complications than that of primary procedures, and the perioperative morbidity rate is reportedly 19%-50% [5,22,23,24]. With the advancement of laparoscopic surgical skills, several studies have recently demonstrated that laparoscopic revision can be performed safely by well-trained and highly experienced bariatric surgeons in specialized bariatric centers [17,25]. The complication rates for laparoscopic revision are reportedly 14.3%-46.3% with laparotomic conversion rates of 3.0%-27.8% [17,25,26,27,28,29]. Our results showed a perioperative complication rate of 9.1% without any laparotomic conversion. Although the number of the enrolled patient is too small to draw any conclusions, the laparoscopic approach could be a safe measure for revision with acceptable risks. It seems that open surgery, in itself, could be rather troublesome in morbidly obese patients because it would be very difficult to approach the deeply seated intra-abdominal organs and secure an appropriate surgical view because of excessive fat tissues. Instead, the laparoscopic approach could provide a better vision with a close view, facilitating more precise dissection.
Controversy remains over the matter of performing a conversion from failed LAGB to other bariatric procedures in one or two steps. Some investigators prefer to perform the operations in two steps for several reasons, including a predictable surgical time, lower risk of postoperative complications, and reduced incidence of delayed anastomotic stricture [8,17,27]. Others have advocated single-staged operation, suggesting that it could be safely performed without increasing the risk of surgical complications [28,29]. Here, we performed the revisional procedures in a single stage in the early six consecutive cases, but the sixth patient developed a staple-line leakage after conversion to RYGB and required reoperation on the first postoperative day. Since that event, we have been performing a two-staged procedure (i.e., laparoscopic band removal first and the subsequent SG or RYGB a few months later) concerning staple line safety. As other bariatric surgeons already have pointed out, the operating time is unpredictable before the surgery and easily prolonged in the single-stage revisional operation. The inflammation caused by an installed foreign body induces adhesion around the device and creates marked gastric wall thickening, which consequently might cause a staple-line disruption. Furthermore, it is difficult to identify the original anatomy when severe adhesion caused anatomic distortion and adhesiolysis usually causes bleeding that disturbs surgical vision and accurate dissection; these could serve as factors to increase the risk of severe postoperative complications. Therefore, a two-staged operation would be recommended for surgeons who are inexperienced with revisions.
There are several limitations of the present study. First, this was a retrospective study from a single institution and the number of enrolled patients is very small. Second, the anthropometric data of the enrolled patients before the primary surgery were often missing, so the efficacy of revisional surgery compared with the primary operation could not be clearly demonstrated. Finally, the follow-up duration is somewhat short, and the collection of long-term results is still needed.
In conclusion, revisional bariatric surgery using the laparoscopic approach can be successfully performed with an increased but acceptable risk of postoperative morbidity and demonstrates satisfactory short-term weight loss. Other undesirable results from the primary surgery could also be successfully managed with deliberate determination on the choice of revisional procedures. Long-term outcomes regarding weight loss and delayed complications are required in the future.
ACKNOWLEDGEMENTS
This research was supported by the Soonchunhyang University Research Fund.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Heo YS, Park JM, Kim YJ, Kim SM, Park DJ, Lee SK, et al. Bariatric surgery versus conventional therapy in obese Korea patients: a multicenter retrospective cohort study. J Korean Surg Soc. 2012;83:335–342. doi: 10.4174/jkss.2012.83.6.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deitel M, Gawdat K, Melissas J. Reporting weight loss 2007. Obes Surg. 2007;17:565–568. doi: 10.1007/s11695-007-9116-0. [DOI] [PubMed] [Google Scholar]
- 3.Behrns KE, Smith CD, Kelly KA, Sarr MG. Reoperative bariatric surgery. Lessons learned to improve patient selection and results. Ann Surg. 1993;218:646–653. doi: 10.1097/00000658-199321850-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Radtka JF, 3rd, Puleo FJ, Wang L, Cooney RN. Revisional bariatric surgery: who, what, where, and when? Surg Obes Relat Dis. 2010;6:635–642. doi: 10.1016/j.soard.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Spyropoulos C, Kehagias I, Panagiotopoulos S, Mead N, Kalfarentzos F. Revisional bariatric surgery: 13-year experience from a tertiary institution. Arch Surg. 2010;145:173–177. doi: 10.1001/archsurg.2009.260. [DOI] [PubMed] [Google Scholar]
- 6.Sjostrom L, Narbro K, Sjostrom CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–752. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 7.Boza C, Gamboa C, Perez G, Crovari F, Escalona A, Pimentel F, et al. Laparoscopic adjustable gastric banding (LAGB): surgical results and 5-year follow-up. Surg Endosc. 2011;25:292–297. doi: 10.1007/s00464-010-1176-x. [DOI] [PubMed] [Google Scholar]
- 8.Van Nieuwenhove Y, Ceelen W, Stockman A, Vanommeslaeghe H, Snoeck E, Van Renterghem K, et al. Long-term results of a prospective study on laparoscopic adjustable gastric banding for morbid obesity. Obes Surg. 2011;21:582–587. doi: 10.1007/s11695-010-0341-6. [DOI] [PubMed] [Google Scholar]
- 9.Himpens J, Cadiere GB, Bazi M, Vouche M, Cadiere B, Dapri G. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011;146:802–807. doi: 10.1001/archsurg.2011.45. [DOI] [PubMed] [Google Scholar]
- 10.Romy S, Donadini A, Giusti V, Suter M. Roux-en-Y gastric bypass vs gastric banding for morbid obesity: a case-matched study of 442 patients. Arch Surg. 2012;147:460–466. doi: 10.1001/archsurg.2011.1708. [DOI] [PubMed] [Google Scholar]
- 11.O'Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257:87–94. doi: 10.1097/SLA.0b013e31827b6c02. [DOI] [PubMed] [Google Scholar]
- 12.Higa K, Ho T, Tercero F, Yunus T, Boone KB. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis. 2011;7:516–525. doi: 10.1016/j.soard.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 13.Himpens J, Coromina L, Verbrugghe A, Cadiere GB. Outcomes of revisional procedures for insufficient weight loss or weight regain after Roux-en-Y gastric bypass. Obes Surg. 2012;22:1746–1754. doi: 10.1007/s11695-012-0728-7. [DOI] [PubMed] [Google Scholar]
- 14.Weiner RA, Theodoridou S, Weiner S. Failure of laparoscopic sleeve gastrectomy: further procedure? Obes Facts. 2011;4(Suppl 1):42–46. doi: 10.1159/000327343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Rutte PW, Smulders JF, de Zoete JP, Nienhuijs SW. Indications and short-term outcomes of revisional surgery after failed or complicated sleeve gastrectomy. Obes Surg. 2012;22:1903–1908. doi: 10.1007/s11695-012-0774-1. [DOI] [PubMed] [Google Scholar]
- 16.Acholonu E, McBean E, Court I, Bellorin O, Szomstein S, Rosenthal RJ. Safety and short-term outcomes of laparoscopic sleeve gastrectomy as a revisional approach for failed laparoscopic adjustable gastric banding in the treatment of morbid obesity. Obes Surg. 2009;19:1612–1616. doi: 10.1007/s11695-009-9941-4. [DOI] [PubMed] [Google Scholar]
- 17.Victorzon M. Revisional bariatric surgery by conversion to gastric bypass or sleeve: good short-term outcomes at higher risks. Obes Surg. 2012;22:29–33. doi: 10.1007/s11695-011-0548-1. [DOI] [PubMed] [Google Scholar]
- 18.Jennings NA, Boyle M, Mahawar K, Balupuri S, Small PK. Revisional laparoscopic Roux-en-Y gastric bypass following failed laparoscopic adjustable gastric banding. Obes Surg. 2013;23:947–952. doi: 10.1007/s11695-013-0888-0. [DOI] [PubMed] [Google Scholar]
- 19.Weber M, Muller MK, Michel JM, Belal R, Horber F, Hauser R, et al. Laparoscopic Roux-en-Y gastric bypass, but not rebanding, should be proposed as rescue procedure for patients with failed laparoscopic gastric banding. Ann Surg. 2003;238:827–833. doi: 10.1097/01.sla.0000098623.53293.bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gagner M, Gumbs AA. Gastric banding: conversion to sleeve, bypass, or DS. Surg Endosc. 2007;21:1931–1935. doi: 10.1007/s00464-007-9539-7. [DOI] [PubMed] [Google Scholar]
- 21.Zundel N, Hernandez JD. Revisional surgery after restrictive procedures for morbid obesity. Surg Laparosc Endosc Percutan Tech. 2010;20:338–343. doi: 10.1097/SLE.0b013e3181f6287a. [DOI] [PubMed] [Google Scholar]
- 22.Schwartz RW, Strodel WE, Simpson WS, Griffen WO., Jr Gastric bypass revision: lessons learned from 920 cases. Surgery. 1988;104:806–812. [PubMed] [Google Scholar]
- 23.Owens BM, Owens ML, Hill CW. Effect of Revisional bariatric surgery on weight loss and frequency of complications. Obes Surg. 1996;6:479–484. doi: 10.1381/096089296765556377. [DOI] [PubMed] [Google Scholar]
- 24.Sugerman HJ, Kellum JM, Jr, DeMaria EJ, Reines HD. Conversion of failed or complicated vertical banded gastroplasty to gastric bypass in morbid obesity. Am J Surg. 1996;171:263–269. doi: 10.1016/S0002-9610(97)89565-7. [DOI] [PubMed] [Google Scholar]
- 25.Gagner M, Gentileschi P, de Csepel J, Kini S, Patterson E, Inabnet WB, et al. Laparoscopic reoperative bariatric surgery: experience from 27 consecutive patients. Obes Surg. 2002;12:254–260. doi: 10.1381/096089202762552737. [DOI] [PubMed] [Google Scholar]
- 26.Mognol P, Chosidow D, Marmuse JP. Laparoscopic conversion of laparoscopic gastric banding to Roux-en-Y gastric bypass: a review of 70 patients. Obes Surg. 2004;14:1349–1353. doi: 10.1381/0960892042584003. [DOI] [PubMed] [Google Scholar]
- 27.Van Dessel E, Hubens G, Ruppert M, Balliu L, Weyler J, Vaneerdeweg W. Roux-en-Y gastric bypass as a re-do procedure for failed restricive gastric surgery. Surg Endosc. 2008;22:1014–1018. doi: 10.1007/s00464-007-9576-2. [DOI] [PubMed] [Google Scholar]
- 28.Hii MW, Lake AC, Kenfield C, Hopkins GH. Laparoscopic conversion of failed gastric banding to Roux-en-Y gastric bypass: short-term follow-up and technical considerations. Obes Surg. 2012;22:1022–1028. doi: 10.1007/s11695-012-0594-3. [DOI] [PubMed] [Google Scholar]
- 29.Tran TT, Pauli E, Lyn-Sue JR, Haluck R, Rogers AM. Revisional weight loss surgery after failed laparoscopic gastric banding: an institutional experience. Surg Endosc. 2013;27:4087–4093. doi: 10.1007/s00464-013-3065-6. [DOI] [PubMed] [Google Scholar]