Abstract
Background and Objectives
Current studies give us inconsistent results regarding the association of neoplasms and zinc(II) serum and tissues concentrations. The results of to-date studies using meta-analysis are summarized in this paper.
Methods
Web of Science (Science citation index expanded), PubMed (Medline), Embase and CENTRAL were searched. Articles were reviewed by two evaluators; quality was assessed by Newcastle-Ottawa scale; meta-analysis was performed including meta-regression and publication bias analysis.
Results
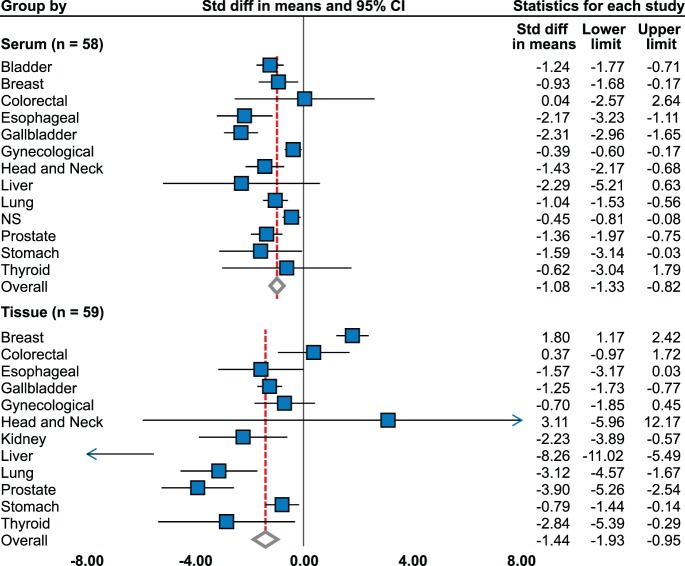
Analysis was performed on 114 case control, cohort and cross-sectional studies of 22737 participants. Decreased serum zinc level was found in patients with lung (effect size = −1.04), head and neck (effect size = −1.43), breast (effect size = −0.93), liver (effect size = −2.29), stomach (effect size = −1.59), and prostate (effect size = −1.36) cancers; elevation was not proven in any tumor. More specific zinc patterns are evident at tissue level, showing increase in breast cancer tissue (effect size = 1.80) and decrease in prostatic (effect size = −3.90), liver (effect size = −8.26), lung (effect size = −3.12), and thyroid cancer (effect size = −2.84). The rest of the included tumors brought ambiguous results, both in serum and tissue zinc levels across the studies. The association between zinc level and stage or grade of tumor has not been revealed by meta-regression.
Conclusion
This study provides evidence on cancer-specific tissue zinc level alteration. Although serum zinc decrease was associated with most tumors mentioned herein, further – prospective - studies are needed.
Introduction
Zinc(II) plays a role in several intracellular signalling pathways. It is also a cofactor of numerous enzymes [1]. Its dysregulation is present in various cancers. Imbalance of zinc transporters causing intracellular and serum zinc(II) levels alteration was described in prostate and breast cancers. [2]–[5]. Questions were raised whether these associations have clinical applications. Studies focusing on zinc content in biological materials in cancer patients provide inconsistent results. Zinc levels in tumor tissues of prostate [6], liver [7], and lung [8] and its serum levels in breast, lung, stomach, and prostate cancer patients were reviewed previously [9].
We investigated the associations of serum and cellular zinc(II) levels with carcinomas via meta-analysis.
Methods
Literature Search
Search was performed in Web of science (Science citation index expanded 1945 to April 2013), PubMed (Medline 1968 to April 2013), Embase (1977 to April 2013), and Cochrane Library (CENTRAL 1953 to April 2013); keywords are shown in Figure 1. Moreover, cited references of found articles were analyzed.
Figure 1. Flow diagram for identification of relevant studies.
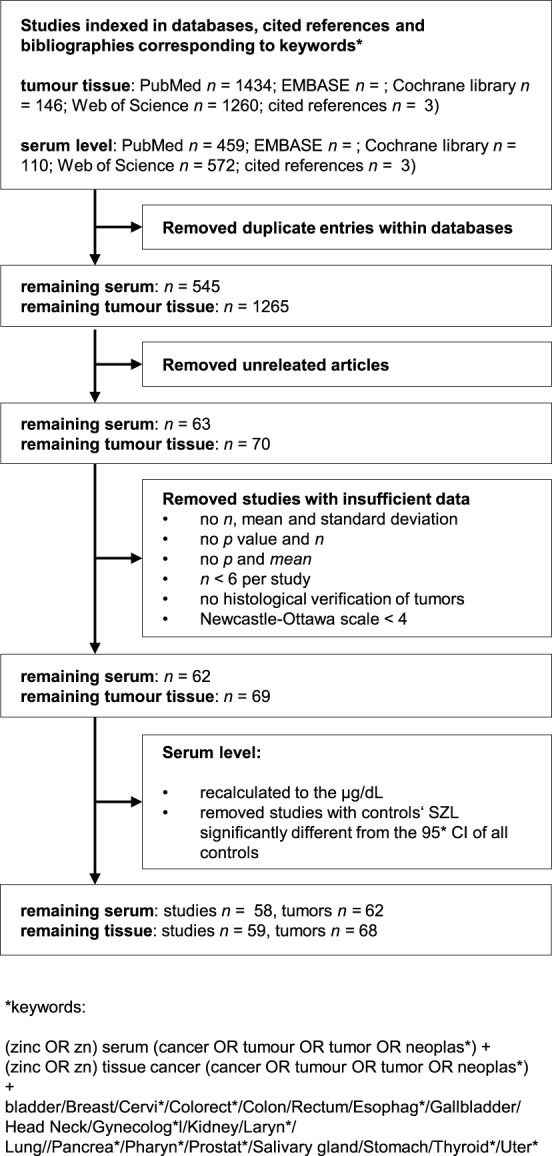
Selection Criteria
Diagram (Fig. 1) shows acquisition process. Among published articles, the search was done for clinical trials, case-control and cohort studies investigating the associations between carcinoma and tissues and serum zinc levels. Because no difference in zinc(II) level between serum and plasma was found [10], both materials were referred as “serum”. Studies with full texts available were included only. Only the studies where the data were displayed in the following ways were accepted: (1) sample size, means and standard deviations, or (2) sample size, means, P values and statistical test type (one- or two-tailed). If similar data were found in more studies by the same group, study with most data was included.
The eligibility of the studies for meta-analysis was evaluated by J.G. and V.A., discrepancies were discussed with R.K and M.M.
Assessment of Methodological Quality
The quality of studies was assessed by the Newcastle-Ottawa Scale (NOS) [11]. NOS ranges from 0 to 9 stars. The studies with <4 stars were excluded, with >6 stars were considered as high quality; the mean was 5.6 stars.
Main and Subgroup Analyses
First, differences of the serum and tissue zinc levels between overall tumors and controls were analysed (Table 1). Then, analyses by tumor type, histology, and methodological quality were performed (Table 2). To meet conditions of between-study independence, zinc level was averaged in studies with multiple tumors, forming age groups or detecting gender separately in case of the summary. For comparison of individual tumors, the tumor was taken as a unit of analysis unless violated between-study independence.
Table 1. Overall results of meta-analysis by tumor type and statistical model used.
| Tumor | No. of studies | Point estimate | 95% CI of point estimate | Heterogeneity, I2 | Model used |
| Bladder - serum | 2 | −1.24 | −1.77 to −0.71 | 61.74 | random |
| Breast serum | 12 | −0.93 | −1.68 to −0.17 | 96.16 | random |
| Breast tissue | 15 | 1.80 | 1.17 to 2.42 | 94.89 | random |
| Colorectal serum | 5 | 0.04 | −2.57 to 2.64 | 98.98 | random |
| Colorectal tissue | 7 | 0.37 | −0.97 to 1.72 | 96.23 | random |
| Esophageal serum | 4 | −2.17 | −3.23 to −1.11 | 86.46 | random |
| Esophageal tissue | 3 | −1.57 | −3.17 to 0.03 | 94.72 | random |
| Gallbladder - serum | 1 | −2.31 | −2.96 to −1.65 | - | |
| Gallbladder - tissue | 2 | −1.25 | −1.73 to −0.77 | 0.00 | fixed |
| Gynecological serum | 3 | −0.39 | −0.6 to −0.17 | 49.48 | fixed |
| Gynecological tissue | 4 | −0.70 | −1.85 to 0.45 | 91.40 | random |
| Head and neck tissue | 2 | 3.11 | −5.96 to 12.17 | 98.75 | random |
| Head Neck serum | 5 | −1.43 | −2.17 to −0.68 | 77.46 | random |
| Kidney - tissue | 4 | −2.23 | −3.89 to −0.57 | 89.51 | random |
| Liver - serum | 3 | −2.29 | −5.21 to 0.63 | 97.64 | random |
| Liver - tissue | 7 | −8.26 | −11.02 to −5.49 | 98.49 | random |
| Lung - serum | 13 | −1.04 | −1.53 to −0.56 | 92.94 | random |
| Lung - tissue | 6 | −3.12 | −4.57 to −1.67 | 96.76 | random |
| Prostate serum | 7 | −1.36 | −1.97 to −0.75 | 97.93 | random |
| Prostate tissue | 12 | −3.90 | −5.26 to −2.54 | 94.67 | random |
| Stomach serum | 4 | −1.59 | −3.14 to −0.03 | 98.24 | random |
| Stomach tissue | 3 | −0.79 | −1.44 to −0.14 | 60.85 | random |
| Thyroid serum | 3 | −0.62 | −3.04 to 1.79 | 97.69 | random |
| Thyroid tissue | 3 | −2.84 | −5.39 to −0.29 | 97.56 | random |
| Overall - serum | 58 | −1.08 | −1.33 to −0.82 | 96.71 | random |
| Overall - tissue | 59 | −1.44 | −1.93 to −0.95 | 97.08 | random |
CI, confidence interval.
Table 2. Subgroup analysis by study quality and histological type.
| Subgroup | Tumor | Factor | No. of studies | Point estimate (95% CI) | Heterogeneity, I2 | Model used |
| Study quality | ||||||
| Breast serum | high | 3 | 0.22 (−0.08 to 0.51) | 0.00 | fixed | |
| Breast serum | low | 9 | −1.32 (−2.23 to −0.42) | 97.06 | random | |
| Breast tissue | high | 9 | 2.33 (1.46 to 3.21) | 95.88 | random | |
| Breast tissue | low | 6 | 1.11 (0.08 to 2.14) | 91.22 | random | |
| Colorectal tissue | high | 2 | −0.50 (−2.84 to 1.85) | 81.73 | random | |
| Colorectal tissue | low | 5 | 0.80 (−0.84 to 2.43) | 96.55 | random | |
| Esophageal serum | high | 2 | −1.56 (−3.23 to 0.10) | 72.04 | random | |
| Esophageal serum | low | 2 | −2.99 (−4.79 to −1.19) | 93.50 | random | |
| Esophageal tissue | high | 2 | −1.60 (−3.86 to 0.65) | 97.29 | random | |
| Esophageal tissue | low | 1 | −1.52 (−2.56 to −0.47) | - | ||
| Gynecological tissue | high | 3 | −0.14 (−1.02 to 0.75) | 82.33 | random | |
| Gynecological tissue | low | 1 | −2.49 (−3.31 to −1.66) | - | ||
| Head Neck serum | high | 2 | −0.88 (−1.26 to −0.49) | 3.16 | fixed | |
| Head Neck serum | low | 3 | −1.59 (−2.08 to −1.10) | 86.60 | random | |
| Kidney - tissue | high | 2 | −1.03 (−1.80 to −0.26) | 22.30 | fixed | |
| Kidney - tissue | low | 2 | −3.12 (−6.49 to 0.25) | 96.07 | random | |
| Liver - tissue | high | 2 | −8.03 (−15.12 to −0.94) | 98.00 | random | |
| Liver - tissue | low | 5 | −12.29 (−17.08 to −7.51) | 98.84 | random | |
| Lung - serum | high | 7 | −1.01 (−1.69 to −0.33) | 95.95 | random | |
| Lung - serum | low | 6 | −1.09 (−1.84 to −0.34) | 70.97 | random | |
| Prostate serum | high | 5 | −2.07 (−3.82 to −0.32) | 98.59 | random | |
| Prostate serum | low | 2 | −0.34 (−3.07 to 2.39) | 78.33 | random | |
| Prostate tissue | high | 3 | −6.25 (−9.71 to −2.78) | 98.02 | random | |
| Prostate tissue | low | 9 | −3.59 (−5.34 to −1.85) | 92.34 | random | |
| Stomach serum | high | 1 | −0.13 (−0.32 to 0.06) | - | ||
| Stomach serum | low | 3 | −2.09 (−4.14 to −0.04) | 97.68 | random | |
| Stomach tissue | high | 2 | −1.14 (−1.55 to −0.73) | 0.00 | fixed | |
| Stomach tissue | low | 1 | −0.26 (−0.96 to 0.45) | - | ||
| Overall - serum | high | 26 | −1.30 (−1.72 to −0.88) | 96.62 | random | |
| Overall - serum | low | 32 | −0.92 (−1.3 to −0.54) | 96.77 | random | |
| Overall - tissue | high | 23 | −0.42 (−1.23 to 0.38) | 97.38 | random | |
| Overall - tissue | low | 36 | −2.12 (−2.77 to −1.47) | 96.95 | random | |
| Histological type | ||||||
| Gynecological serum | Ovary | 1 | −0.07 (−0.47 to 0.32) | - | ||
| Gynecological serum | Uterine cervix | 1 | −0.49 (−0.77 to −0.21) | - | ||
| Head Neck serum | Larynx | 4 | −1.52 (−2.35 to −0.69) | 81.96 | random | |
| Head Neck serum | Oral Cavity | 2 | −0.95 (−1.38 to −0.53) | 0.00 | fixed | |
| Lung - serum | adenocarcinoma | 2 | 0.02 (−1.49 to 1.54) | 95.48 | random | |
| Lung - serum | large cell | 2 | −0.78 (−1.32 to −0.23) | 0.00 | fixed | |
| Lung - serum | NSCLC | 4 | −0.94 (−1.36 to −0.53) | 58.87 | random | |
| Lung - serum | small cell | 2 | −1.42 (−3.05 to 0.21) | 88.46 | random | |
| Lung - serum | squamous cell | 2 | −1.23 (−2.75 to 0.29) | 97.01 | random | |
| Lung - tissue | adenocarcinoma | 2 | −0.89 (−2.96 to 1.19) | 92.20 | random | |
| Lung - tissue | large cell | 1 | −1.22 (−2.22 to −0.23) | - | ||
| Lung - tissue | NSCLC | 2 | −0.62 (−1.88 to 0.65) | 88.90 | random | |
| Lung - tissue | small cell | 2 | −0.52 (−0.80 to −0.23) | 0.00 | fixed | |
| Lung - tissue | squamous cell | 2 | −0.48 (−2.54 to 1.58) | 92.14 | random | |
| Thyroid serum | folicular | 2 | −1.86 (−4.83 to 1.11) | 96.81 | random | |
| Thyroid serum | papillary | 2 | −1.48 (−4.43 to 1.48) | 96.38 | random | |
| Thyroid tissue | folicular | 1 | 0.00 (−0.59 to 0.59) | - | ||
| Thyroid tissue | papillary | 1 | −0.50 (−1.09 to 0.09) | - | ||
Note low is for Newcastle-Ottava scale <6, high for NOS >6. Random and fixed effect meta-analysis. NSCLC, non-small cell lung cancer, CI, confidence interval.
Statistical Analyses
To express the differences in serum and tissue concentrations, standardized difference in means (Cohen’s d) was used. To assess heterogeneity across studies, Higgins I2 (describes percentage of variability) was calculated [12]. Random effects model meta-analysis was employed when I2>50%; otherwise, fixed model was used. Publication bias was evaluated using funnel plots and two-sided Egger tests in groups with >3 studies. Funnel plots of studies with Egger’s test p<0.05 are asymmetric (Table S1). There was performed meta-regression using unrestricted maximum likehood method of studies reporting stage or grade if number of studies with corresponding moderators was >10 [13], [14]. Comprehensive Meta-analysis Version 2 software (Biostat, Englewood, NJ) was used for analysis.
Results
Identification of Relevant Studies and their Characteristics
Total of 3201 articles were found. After excluding articles not meeting the criteria (Fig. 1) and duplicates, 114 articles studying 130 tumors were included (several studies studied more tumors, Table S2).
Overall 114 studies including 22737 participants (8584 cases, 14153 controls) were analyzed. From studies reporting age, sex and ethnicity, the mean age was 54.5±12.3 (male) and 49.6±12.2 (female); male were included 49.5% and 51.0% in “tumor” and control groups. Publication date ranged within 1952–2012. Caucasians, Asians, Hispanics, and Afro-Americans were reported in 52%, 45%, 1%, and 2%, respectively. Characteristics of studies are summarized in Table S2. Two clinical, 4 cohort, 6 cross-sectional, and 102 case control studies were included.
Overall Zinc Level in Sera and Tumors
Serum level
As shown on Fig. 2 and Table 1, serum zinc level is significantly decreased in patients with tumors (effect size = −1.08; 95% confidence interval, CI, −1.33 to −0.82) using random effects model of 58 studies (6223 cases, 10364 controls). This is consistent with subgroup of 26 high-quality studies (effect size = −1.30; 95% CI, −1.72 to −0.88). High level of heterogeneity is observed (Higgins I2 = 96.71%). Meta-regression did not reveal that stage, grade, and age or publication year affect effect size (Table S1). Six studies analyzed serum zinc level in group of patients with malignant tumor without other specification (516 cases, 3871 controls), and significant decrease was found (Fig. 2) [15]–[20].
Figure 2. Level of zinc in sera and tissues by tumor type.
Summary of individual meta-analyses. For model used and heterogeneity, see Table 1.
Tissue level
There was a significant decrease in tissue zinc level using random effects model meta-analysis of 59 studies (2361 cases, 3789 controls) with effect size −1.44 (CI−1.93 to −0.95). However, publication bias was observed at p = 0.01 and no significance found in 24 high-quality studies. Meta-regression did not reveal any moderators to affect global effect size.
Bladder
Significant decrease of serum zinc level was observed (−1.24; 95% CI, −1.77 to −0.77) using random effects model of two studies [21], [22] (86 cases, 92 controls); both were “high-quality”.
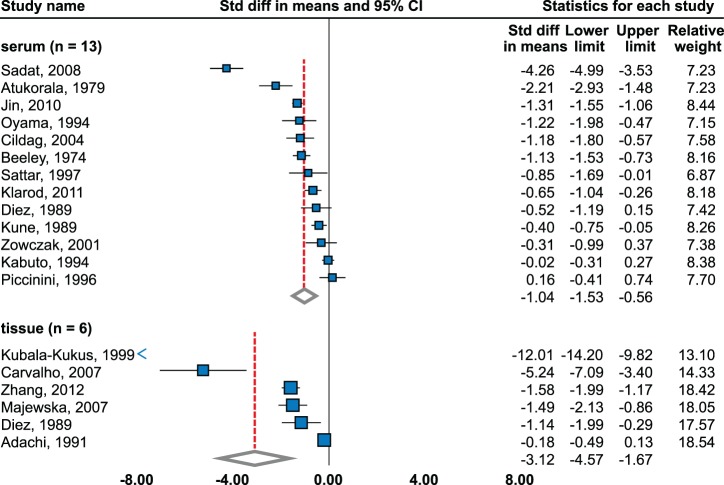
Breast
Serum
There was significant decrease (−0.93; 95% CI, −1.68 to −0.17) using random effects model meta-analysis of 12 studies (604 cases, 663 controls) [20], [23]–[33] (Fig. 3, Table 1). However, no significant change was observed in six studies [20], [23], [25], [27], [30], [31] and significantly increased level in one [24]. No publication bias was observed (Begg’s funnel plot was symmetrical, Egger’s 2-tailed test p = 0.086). Subgroup meta-analysis by methodological quality of study revealed significant decrease in nine low-quality studies (− 1.32, CI–2.23 to–0.42) using random effects model, but no significant change in three high-quality studies using fixed effects model [25], [27], [31]. With regard to stage, Yucel et al. found no difference between stages [33]; in contrary, studies by Gupta et al. and Kuo et al. showed a decrease in advanced cancer in comparison to early stages [26] and significantly decreasing trend in relation to stage [29].
Figure 3. Zinc level in sera and tissues of breast cancer patients.
Random effects model meta-analysis. Studies sorted by standardized mean difference.
Tissue level
Significant elevation was determined using random effects model of 15 studies (635 cases, 714 controls), effect size = 1.80 (95% CI, 1.17 to 2.42) [29], [34]–[47]. However, two studies show insignificant changes [42], [46]. The highest levels were observed in study by Ng et al., which include ductal cancers only [35]. Publication bias was observed on p = 0.018. Significant elevation was found in both low- and high- quality studies, while the levels were higher in 9 high-quality studies (2.33; CI, 1.46 to 3.21). Farquharson et al. reported significantly decreased tissue zinc concentration in estrogen receptor negative tumors [42]. Kuo et al. found no trend [29] in relation to grade, while Farquharson et al. showed significant decrease in grade II-III vs. grade I [42].
Gynecological Tumors (Uterine Corpus, Cervix and Ovarian)
Serum
Among ovarian and cervical cancers, there was a significant decrease found (−0.39; CI−0.60 to −0.17) using fixed effects model of three studies (164 cases, 171 controls) [20], [48], [49]. No publication bias was observed. When subgroup meta-analysis by histological type was done, significant decrease was found in cervical [48], insignificant changes in ovarian cancer [49]. There were no significant trends in relation to stage and grade [49].
Tissue level
No significant difference between uterine corpus and cervix cancers was determined using random-effects model of 4 studies (80 cases, 123 controls) [37], [48], [50], [51]. No publication bias was determined. Significant decrease was reported in two studies [48], [51]. Results of high-quality studies did not show a significant trend.
Digestive System Tumors (Esophageal, Stomach, Colorectal, Liver, Gallbladder and Pancreatic Carcinoma)
Esophageal, serum
All four studies included in this analysis (93 cases, 80 controls) [52]–[55] show significant reduction (−2.17; 95% CI, −3.23 to 1.11) and it was one of the highest decreases. Publication bias was identified (p = 0.04) and insignificant decrease was observed in two high-quality studies.
Esophageal, tissue
No significant change was identified using meta-analysis of three studies (104 cases, 116 controls) [52], [56], [57] due to high variability among studies, even among two high-quality ones [56], [57]. No publication bias was observed.
Stomach, serum
Significant decrease was observed (effect size = −1.59; 95% CI, −3.14 to −0.03) without publication bias. However, high variability was present in the four studies (290 cases, 474 controls) [28], [30], [58], [59] and significant decrease was reported in two studies only [28], [59]. No significant change was observed in one high-quality study [58].
Stomach, tissue
Significant decrease was determined (− 0.79; 95% CI, −1.44 to −0.14) in three studies (71 cases, 67 controls) [37], [59], [60] and one study showed significant decrease [59]. No publication bias was identified.
Colorectal cancer, serum
No significant difference was determined. No study fulfilled criteria of “high-quality”. Five studies were included (313 cases, 216 controls) [28], [30], [61]–[63] and no publication bias was detected. However, two studies showed significant decrease [28], [62], one study showed significant elevation [61], and thus, high serum zinc level variances were associated with colorectal cancer. Of studies reporting stage, one showed significantly decreasing trend on Dukes stage [62], whereas other showed no significant changes related to TNM stage [61].
Colorectal cancer, tissue
No significant difference was observed using meta-analysis of seven studies (233 cases, 159 controls) [34], [37], [46], [62], [64]–[66] and no publication bias was observed. None of the high quality studies revealed significant differences. One of the largest variation among tissue levels was observed (effect size = 0.37; 95% CI, −0.97 to 1.72). Two studies showed significant decrease [62], [64] while another two significant elevation [46], [66]. One study including grade did not show significant trend [64].
Gallbladder, serum
one high-quality study (30 cases, 30 controls), that showed significant decrease, was identified [67].
Gallbladder, tissue
Significant decrease was determined in two studies [68], [69] (39 cases, 40 controls) using fixed effects model (−1.25; 95% CI, −1.73 to −0.77). No study analyzed further classifications.
Liver, serum
No significant change was observed in three studies [70]–[72] (149 cases, 121 controls) and no publication bias was observed. Two high-quality studies [71], [72] are in accordance, showing fixed serum zinc level. One study showed no significant trend in relation to stage [70].
Liver, tissue
Significant decrease was observed in all 7 studies analysed [70], [73]–[78] (269 cases, 329 controls), effect size = −8.26 (95% CI, −11.02 to −5.49). Two high-quality studies [73], [76] provided consistent results (−8.03; 95% CI, −15.12 to −0.93). Publication bias was observed (p = 0.04).
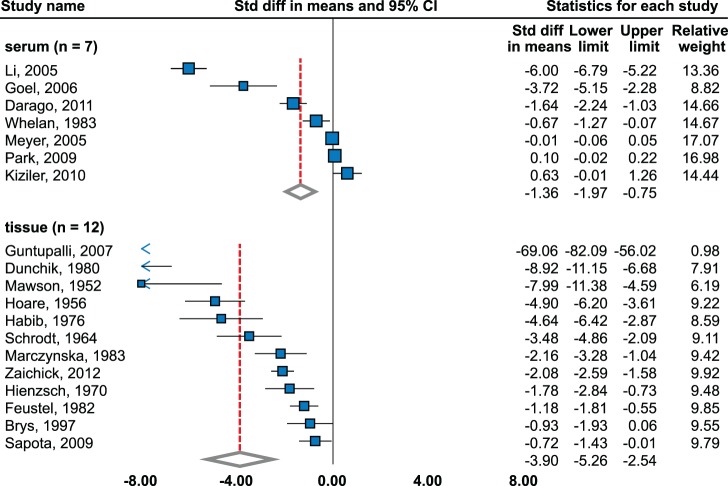
Prostate
Serum
Significant decrease was observed (effect size = −1.36; 95% CI, −1.97 to −0.75) using random effects model-meta-analysis of 7 studies [79]–[85] (2985 cases, 3539 controls, Fig. 4).
Figure 4. Zinc level in sera and tissues of prostate cancer patients.
Random effects model meta-analysis. Studies sorted by standardized mean difference.
Insignificant changes were observed in large sample studies – cohort from French SuViMax study (4961 cases and controls) [82] and Multiethnic Cohort study (1175 cases and controls) [85]. Subgroup meta-analysis found significant decrease in high quality studies (−2.07; 95 CI, −3.82 to −0.32). No publication bias was observed.
Tissue
Random effects model meta-analysis of 12 studies (240 cases, 226 controls) [86]–[97] detected a significant decrease (effect size = −3.90; 95% CI, −5.26 to −2.54). Only one study showed insignificant decrease [86]. Most significant decrease was observed in study by Guntupalli et al. [89]. High level of publication bias was observed among studies (p = 0.0007). Results are in agreement with more distinct effect size in high-quality studies (−6.03; 95% CI, −9.39 to −2.67). Trend was not observed in one study relating to stage and grade [6].
Head and Neck
Serum
Five studies including cancers of oral cavity [98], [99] and larynx [98], [100]–[102] (159 cases, 228 controls) showed significant decrease (random effects model −1.43; 95% CI, −2.17 to −0.68). No publication bias was observed – all studies, including 2 high-quality ones, showed significant decrease [98], [99]. No significant trend was observed between stage and serum zinc level [100].
Tissue
Two studies (45 cases, 27 controls) [103], [104] were included in the analysis. Findings of these studies were contradictory: one showed significant elevation [103] while the other - significant decrease [104]. Random effects model did not show any trend. No significant trend between grade and zinc level was observed in one study [104].
Thyroid
Serum
No significant difference was observed using random effects model of three studies (131 cases, 93 controls) [105]–[107]. One study showed significant elevation [107], the other showed significant decrease [105] and third, ranked as high quality [106], found no significant differences. No publication bias was observed. Subgroup analysis by histological type does not highlight significant difference between papillary and follicular cancer. Medullar carcinoma was not included in meta-analysis.
Tissue
Statistically significant decrease was observed using random effects model (effect size = −2.84; 95% CI, −5.39 to −0.29) of three studies (109 cases, 123 controls) [105], [108], [109]. However, one study reported insignificant results [105], another included papillary, follicular, medullar cancers and reticulosarcoma [108] and the third did not specify histological types. No publication bias was present. One study determined no significant difference between papillary and follicular cancers [105].
Kidney
Tissue
Significant decrease was observed using random effects model (−2.23; 95% CI, −3.89 to −0.57) of 4 studies (66 cases, 45 controls). Results agree with 2 high quality studies [37], [110]. All studies showed significant decrease [37], [110]–[112] and no publication bias was detected.
Lung
Serum
Significant decrease (−1.04; 95% CI, −1.53 to −0.56) was identified using random effect model of 13 studies [20], [31], [58], [113]–[122] (703 cases, 786 controls, Fig. 5); four of them showed insignificant changes [20], [31], [58], [115]. No publication bias was observed (p = 0.38). Analysis of only high-quality studies provided similar results. Subgroup analysis according to histology detected significant decrease in non-small cell lung cancer using random effects model in four studies. Two studies dealt with histological classification [115], [116]: no significant difference was observed in adenocarcinoma and squamous cell carcinoma using random effects and significant decrease in large cell carcinoma using fixed effects (−0.78; 95% CI, −1.32 to −0.23). serum zinc level and stage was analyzed in two studies [114], [116]. Klarod et al. determined significantly lower serum zinc level in advanced compared to low stages [114]. Similarly, descending trend was observed between stages T1, T2, and T3 [116]. Negative correlation between serum zinc level and grade was determined [116].
Figure 5. Zinc level in sera and tissues of lung cancer patients.
Random effects model meta-analysis. Studies sorted by standardized mean difference.
Tissue
Significant decrease was determined using random effects model (−3.12; 95% CI, −4.57 to −1.67) of six studies, all ranked as low-quality [34], [46], [115], [123]–[125] (470 cases, 1820 controls). However, publication bias was observed (p = 0.03). Insignificant change was observed in one study [123]. Significant decrease was determined in small cell lung cancer (−0.52; 95% CI, −0.80 to −0.23) using fixed model and no significant decrease was identified in non-small cell lung cancer using random effects model. No significant trend was observed in squamous and adenocarcinomas. Large cell cancer showed significant decrease in one study [115].
Discussion
Decreased serum zinc level was found in patients with lung, head and neck, breast, liver, stomach, and prostate cancers. The elevation was not proven in any tumor. More specific zinc patterns are evident in tumors. Unequivocal increase was observed in breast cancer tissue only and decrease in prostatic, liver, lung, and thyroid cancer. The rest of the studied tumors brought ambiguous results, both in serum and tissue zinc levels across the studies. It cannot be confirmed that the serum zinc level does not change except of the abovementioned tumors. Serum and tissue zinc level reduction was evident to certain extent in majority of tumors. Although insignificant differences were found, the analysis indicates that none of the tumors clearly disproves that the zinc levels remained unchanged. Variation of serum zinc level were found in esophageal cancer patients, in cell zinc content in liver cancer and both in serum and tissue zinc level in stomach, colorectal, and thyroid cancers.
Number of studies point to decreasing trend in tumors of higher grades or stages. Nevertheless, meta-regression could not be performed on the majority of tumors due to limited number of studies reporting stage/grade or to inconsistency in the scale used. Regression analysis of all tumors, however, did not show dependence on these parameters. Thus, this meta-analysis fails to explain the sources of high heterogeneity between the studies.
Although serum zinc level decrease in lung, head and neck, and breast carcinomas was shown by meta-analysis, it is unclear, whether hypozincaemia is a consequence of tumor, chronic stress or of a combination of both these effects. Stress, infection or chronic diseases lead to redistribution of zinc(II) between body compartments, and thus reduce zincaemia [126]. In addition, chronic inflammation is a common hallmark of cancer, and thus might be important mechanism of serum zinc level decrease.
The association of tissue zinc level and prostate [6], liver [7], and lung [8] cancers serum zinc level and risk of breast, lung, stomach, and prostate cancers [9] were in scope of several reviews. Decrease in prostate cancer tissue zinc level is well-evidenced [127]. Also review by Zaichick et al. show decrease of zinc in prostate cancer tissue as compared with benign hyperplasia [6]. A review by Catalani, focusing on zinc content in lung tumors, is the only to date meta-analysis. However, its results did not allow summarizing the significance of tissue metals. No relationship among tissue zinc level and histotype or stage was found. Zinc decrease in liver cancer tissues were reviewed by Gurusamy et al. They declared that meta-analytic approach is impossible because of heterogeneity of analyzed studies. All mentioned reviews concluded that there is poor data agreement between studies determining tissue zinc level. This fact – combined with the low metal concentrations – calls for the standardization of methods. Catalani et al. propose standardization of sample collection, storage, and analysis. Previous reviews were performed only on specific tumors, with limited number of studies and/or statistic approaches were missing. Our meta-analytical analysis was done on all identified carcinomas, serum and tissue levels were analyzed together, publication bias was assessed and meta-regression was performed when case sufficient data were present. To reduce selection and publication biases, prospective cohort study with defined conditions separating the influence of inflammation is needed. Interest should be focused on the relation of zinc level in each histological type, stage, and grade.
There are limitations in this study caused by features of individual studies: sample sizes, subjects’ characteristics, sampling, storage and detection methods, and different tumors classification. Serum zinc level has a limited predictive value, because it is particularly intracellular ion and it fluctuates in circadian rhythm.
This meta-analysis shows a decrease of zincaemia in lung, head and neck, and breast carcinoma, increase of tissue zinc in breast cancer and its decrease in prostate, liver, and lung cancers. However, this analysis does not provide conclusive data with regard to stage and grade, and thus does not clarify heterogeneity in values between the studies.
Supporting Information
Prisma 2009 checklist.
(DOC)
Meta-regression analysis of overall results using mixed effects model (unrestricted maximum likehood). SMD, standardized mean difference.
(XLSX)
Source data set extracted from studies used for analysis. Including methodological quality of studies based on Newcastle-Ottawa scale, study design, and information regarding matching cases and controls. NS, not specified, NOS, Newcastle-Ottawa scale, stdev, standard deviation.
(XLSX)
Funding Statement
Financial support from Central European Institute of Technology CZ.1.05/1.1.00/02.0068 and Internal Grant Agency of Ministry of Health of the Czech Republic (IGA MH NT14337-3/2013) is highly acknowledged. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Maret W, Li Y (2009) Coordination Dynamics of Zinc in Proteins. Chem Rev 109: 4682–4707. [DOI] [PubMed] [Google Scholar]
- 2. Gumulec J, Masarik M, Krizkova S, Adam V, Hubalek J, et al. (2011) Insight to Physiology and Pathology of Zinc(II) Ions and Their Actions in Breast and Prostate Carcinoma. Curr Med Chem 18: 5041–5051. [DOI] [PubMed] [Google Scholar]
- 3. Eckschlager T, Adam V, Hrabeta J, Figova K, Kizek R (2009) Metallothioneins and Cancer. Curr Protein Pept Sci 10: 360–375. [DOI] [PubMed] [Google Scholar]
- 4. Hogstrand C, Kille P, Nicholson RI, Taylor KM (2009) Zinc transporters and cancer: a potential role for ZIP7 as a hub for tyrosine kinase activation. Trends Mol Med 15: 101–111. [DOI] [PubMed] [Google Scholar]
- 5. Plum LM, Rink L, Haase H (2010) The Essential Toxin: Impact of Zinc on Human Health. Int J Environ Res Public Health 7: 1342–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zaichick VY, Sviridova TV, Zaichick SV (1997) Zinc in human prostate gland: Normal, hyperplastic and cancerous. J Radioanal Nucl Chem 217: 157–161. [DOI] [PubMed] [Google Scholar]
- 7. Gurusamy K (2007) Trace element concentration in primary liver cancers - A systematic review. Biol Trace Elem Res 118: 191–206. [DOI] [PubMed] [Google Scholar]
- 8. Catalani S, De Palma G, Mangili A, Apostoli P (2008) Metallic elements in lung tissues: results of a meta-analysis. Acta Biomed 79: 52–63. [PubMed] [Google Scholar]
- 9. Silvera SAN, Rohan TE (2007) Trace elements and cancer risk: a review of the epidemiologic evidence. Cancer Causes Control 18: 7–27. [DOI] [PubMed] [Google Scholar]
- 10. Hess SY, Peerson JA, King JC, Brown KH (2007) Use of serum zinc concentration as an indicator of population zinc status. Food Nutr Bull 28: S403–S429. [DOI] [PubMed] [Google Scholar]
- 11.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, et al.. (2014) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses.
- 12. Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21: 1539–1558. [DOI] [PubMed] [Google Scholar]
- 13.Littell JH, Corcoran J, Pillai V (2008) Assessing Bias and Variations in Effects. In: Tripodi T, editor. Systematic Reviews and Meta-Analysis: Oxford University Press, USA. pp. 351.
- 14.Higgins JPT, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. In: Higgins JPT, Green S, editors: The Cochrane Collaboration.
- 15. Boz A, Evliyaoglu O, Yildirim M, Erkan N, Karaca B (2005) The value of serum zinc, copper, ceruloplasmin levels in patients with gastrointestinal tract cancers. Turk J Gastroenterol 16: 81–84. [PubMed] [Google Scholar]
- 16. Federico A, Iodice P, Federico P, Del Rio A, Mellone MC, et al. (2001) Effects of selenium and zinc supplementation on nutritional status in patients with cancer of digestive tract. Eur J Clin Nutr 55: 293–297. [DOI] [PubMed] [Google Scholar]
- 17. Chen H, Tan C, Wu T (2011) Ensemble Modeling Coupled with Six Element Concentrations in Human Blood for Cancer Diagnosis. Biol Trace Elem Res 143: 143–152. [DOI] [PubMed] [Google Scholar]
- 18. Kok FJ, Van Duijn CM, Hofman A, Van der Voet GB, De Wolff FA, et al. (1988) Serum copper and zinc and the risk of death from cancer and cardiovascular disease. Am J Epidemiol 128: 352–359. [DOI] [PubMed] [Google Scholar]
- 19. Leone N, Courbon D, Ducimetiere P, Zureik M (2006) Zinc, copper, and magnesium and risks for all-cause, cancer, and cardiovascular mortality. Epidemiology 17: 308–314. [DOI] [PubMed] [Google Scholar]
- 20. Zowczak M, Iskra M, Torlinski L, Cofta S (2001) Analysis of serum copper and zinc concentrations in cancer patients. Biol Trace Elem Res 82: 1–8. [DOI] [PubMed] [Google Scholar]
- 21. Gecit I, Kavak S, Demir H, Gunes M, Pirincci N, et al. (2011) Serum Trace Element Levels in Patients with Bladder Cancer. Asian Pac J Cancer Prev 12: 3409–3413. [PubMed] [Google Scholar]
- 22. Mazdak H, Yazdekhasti F, Movahedian A, Mirkheshti N, Shafieian M (2010) The comparative study of serum iron, copper, and zinc levels between bladder cancer patients and a control group. Int Urol Nephrol 42: 89–93. [DOI] [PubMed] [Google Scholar]
- 23. Arinola OG, Charles-Davies MA (2008) Micronutrient levels in the plasma of Nigerian females with breast cancer. Afr J Biotechnol 7: 1620–1623. [Google Scholar]
- 24. Cavallo F, Gerber M, Marubini E, Richardson S, Barbieri A, et al. (1991) Zinc and copper in breast cancer. A joint study in northern Italy and southern France. Cancer 67: 738–745. [DOI] [PubMed] [Google Scholar]
- 25. Garofalo JA, Ashikari H, Lesser ML, Menendezbotet C, Cunninghamrundles S, et al. (1980) Serum Zinc, Copper, and the Cu-Zn Ratio in Patients with Benign and Malignant Breast-Lesions. Cancer 46: 2682–2685. [DOI] [PubMed] [Google Scholar]
- 26. Gupta SK, Shukla VK, Vaidya MP, Roy SK, Gupta S (1991) Serum trace elements and Cu/Zn ratio in breast cancer patients. J Surg Oncol 46: 178–181. [DOI] [PubMed] [Google Scholar]
- 27. Huang Y-L, Sheu J-Y, Lin T-H (1999) Association between oxidative stress and changes of trace elements in patients with breast cancer. Clin Biochem 32: 131–136. [DOI] [PubMed] [Google Scholar]
- 28. Isbir T, Tamer L, Erkisi M, Kekec Y, Doran F, et al. (1995) Copper, Zinc and Magnesium in Serum and Tissues from Patients with Carcinoma of Breast, Stomach and Colon. Trace Elem Electrolytes 12: 113–115. [Google Scholar]
- 29. Kuo HW, Chen SF, Wu CC, Chen DR, Lee JH (2002) Serum and tissue trace elements in patients with breast cancer in Taiwan. Biol Trace Elem Res 89: 1–11. [DOI] [PubMed] [Google Scholar]
- 30. Magalova T, Bella V, Brtkova A, Beno I, Kudlackova M, et al. (1999) Copper, zinc and superoxide dismutase in precancerous, benign diseases and gastric, colorectal and breast cancer. Neoplasma 46: 100–104. [PubMed] [Google Scholar]
- 31. Piccinini L, Borella P, Bargellini A, Medici CI, Zoboli A (1996) A case-control study on selenium, zinc, and copper in plasma and hair of subjects affected by breast and lung cancer. Biol Trace Elem Res 51: 23–30. [DOI] [PubMed] [Google Scholar]
- 32. Tinoco-Veras CM, Sousa MSB, da Silva BB, Cozzolino SMF, Pires LV, et al. (2011) Analysis of plasma and erythrocyte zinc levels in premenopausal women with breast cancer. Nutr Hosp 26: 293–297. [DOI] [PubMed] [Google Scholar]
- 33. Yucel I, Arpaci F, Ozet A, Doner B, Karayilanoglu T, et al. (1994) Serum copper and zinc levels and copper/zinc ratio in patients with breast cancer. Biol Trace Elem Res 40: 31–38. [DOI] [PubMed] [Google Scholar]
- 34. Carvalho ML, Magalhaes T, Becker M, von Bohlen A (2007) Trace elements in human cancerous and healthy tissues: A comparative study by EDXRF, TXRF, synchrotron radiation and PIXE. Spectroc Acta Pt B-Atom Spectr 62: 1004–1011. [Google Scholar]
- 35. Ng KH, Bradley DA, Looi LM (1997) Elevated trace element concentrations in malignant breast tissues. Br J Radiol 70: 375–382. [DOI] [PubMed] [Google Scholar]
- 36. Raju GJN, Sarita P, Kumar MR, Murty G, Reddy BS, et al. (2006) Trace elemental correlation study in malignant and normal breast tissue by PIXE technique. Nucl Instrum Methods Phys Res Sect B-Beam Interact Mater Atoms 247: 361–367. [Google Scholar]
- 37. Margalioth EJ, Schenker JG, Chevion M (1983) Copper and Zinc Levels in Normal and Malignant-Tissues. Cancer 52: 868–872. [DOI] [PubMed] [Google Scholar]
- 38. Singh V, Garg AN (1998) Trace element correlations in the blood of Indian women with breast cancer. Biol Trace Elem Res 64: 237–245. [DOI] [PubMed] [Google Scholar]
- 39. Ebrahim AM, Eltayeb MAH, Shaat MK, Mohmed MA, Eltayeb EA, et al. (2007) Study of selected trace elements in cancerous and non-cancerous human breast tissues from Sudanese subjects using instrumental neutron activation analysis. Sci Total Environ 383: 52–58. [DOI] [PubMed] [Google Scholar]
- 40. Silva MP, Tomal A, Perez CA, Ribeiro-Silva A, Poletti ME (2009) Determination of Ca, Fe, Cu and Zn and their correlations in breast cancer and normal adjacent tissues. X-Ray Spectrom 38: 103–111. [Google Scholar]
- 41. Geraki K, Farquharson MJ, Bradley DA (2002) Concentrations of Fe, Cu and Zn in breast tissue: a synchrotron XRF study. Phys Med Biol 47: 2327–2339. [DOI] [PubMed] [Google Scholar]
- 42. Farquharson MJ, Al-Ebraheem A, Geraki K, Leek R, Harris AL (2009) Zinc presence in invasive ductal carcinoma of the breast and its correlation with oestrogen receptor status. Phys Med Biol 54: 4213–4223. [DOI] [PubMed] [Google Scholar]
- 43. Stawarz R, Formicki G, Zakrzewski M, Rys J, Rozmus M (2009) Distribution of Heavy Metals and Trace Elements in Human Breast Cancer Tissues and in Adjacent Normal Tissues of Women in Poland. Fresen Environ Bull 18: 182–188. [Google Scholar]
- 44. Kubala-Kukus A, Banas D, Braziewicz J, Gozdz S, Majewska U, et al. (2007) Analysis of elemental concentration censored distributions in breast malignant and breast benign neoplasm tissues. Spectroc Acta Pt B-Atom Spectr 62: 695–701. [Google Scholar]
- 45. Ionescu JG, Novotny J, Stejskal V, Latsch A, Blaurock-Busch E, et al. (2006) Increased levels of transition metals in breast cancer tissue. Neuroendocrinol Lett 27: 36–39. [PubMed] [Google Scholar]
- 46. Majewska U, Banas D, Braziewicz J, Gozdz S, Kubala-Kukus A, et al. (2007) Trace element concentration distributions in breast, lung and colon tissues. Phys Med Biol 52: 3895–3911. [DOI] [PubMed] [Google Scholar]
- 47. Cui Y, Vogt S, Olson N, Glass AG, Rohan TE (2007) Levels of zinc, selenium, calcium, and iron in benign breast tissue and risk of subsequent breast cancer. Cancer Epidemiol Biomarkers Prev 16: 1682–1685. [DOI] [PubMed] [Google Scholar]
- 48. Han CZ, Jing JX, Zhao ZW, Guo JG, Zheng SM, et al. (2003) Serum and tissue levels of six trace elements and copper/zinc ratio in patients with cervical cancer and uterine myoma. Biol Trace Elem Res 94: 113–122. [DOI] [PubMed] [Google Scholar]
- 49. Shobeiri MJ, Tabrizi AD, Atashkhoei S, Sayyah-Melli M, Ouladsahebmadarek E, et al. (2011) Serum levels of Copper, Zinc and Copper/Zinc Ratio in Patients with Ovarian Cancer. Pak J Med Sci 27: 561–565. [Google Scholar]
- 50. Nasiadek M, Krawczyk T, Sapota A (2005) Tissue levels of cadmium and trace elements in patients with myoma and uterine cancer. Hum Exp Toxicol 24: 623–630. [DOI] [PubMed] [Google Scholar]
- 51. Zhong HH, Tan MJ, Fu YL, Huang JQ, Tang ZF (1999) Determination of trace elements in tissue of human uterine cancer by instrumental neutron activation analysis. Biol Trace Elem Res 71–2: 569–574. [DOI] [PubMed] [Google Scholar]
- 52. Lin HJ, Chan WC, Fong YY, Newberne PM (1977) Zinc Levels in Serum, Hair and Tumors from Patients with Esophageal Cancer. Nutr Rep Int 15: 635–643. [Google Scholar]
- 53. Goyal M, Kalwar A, Vyas R, Bhati A (2006) A study of serum zinc, selenium and copper levels in carcinoma of esophagus patients. Ind J Clin Biochem 21: 208–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mellow MH, Layne EA, Lipman TO, Kaushik M, Hostetler C, et al. (1983) Plasma zinc and vitamin a in human squamous carcinoma of the esophagus. Cancer 51: 1615–1620. [DOI] [PubMed] [Google Scholar]
- 55. Salehifar E, Khorasani G, Shokrzade M, Asadi M, Shabankhani B, et al. (2008) Comparison of plasma levels of zinc and lead in esophageal cancer patients with normal subjects. Trace Elem Electrolytes 25: 165–168. [Google Scholar]
- 56. Abnet CC, Lai B, Qiao YL, Vogt S, Luo XM, et al. (2005) Zinc concentration in esophageal biopsy specimens measured by x-ray fluorescence and esophageal cancer risk. J Natl Cancer Inst 97: 301–306. [DOI] [PubMed] [Google Scholar]
- 57. Sun ZG, Song GM, Zhang M, Wang Z (2011) Clinical study on zinc, copper and manganese levels in patients with esophageal squamous cell cancer. Trace Elem Electrolytes 28: 116–120. [Google Scholar]
- 58. Kabuto M, Imai H, Yonezawa C, Neriishi K, Akiba S, et al. (1994) Prediagnostic serum selenium and zinc levels and subsequent risk of lung and stomach cancer in Japan. Cancer Epidemiol Biomarkers Prev 3: 465–469. [PubMed] [Google Scholar]
- 59. Narang APS, Wani NA (1991) Levels of Copper and Zinc in Serum and Tissues of Patients with Gastric-Carcinoma. Trace Elem Med 8: 15–18. [Google Scholar]
- 60. Yaman M, Kaya G, Yekeler H (2007) Distribution of trace metal concentrations in paired cancerous and non-cancerous human stomach tissues. World J Gastroenterol 13: 612–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Milde D, Machacek J, Stuzka V (2007) Evaluation of colon cancer elements contents in serum using statistical methods. Chem Pap 61: 348–352. [Google Scholar]
- 62. Gupta SK, Shukla VK, Vaidya MP, Roy SK, Gupta S (1993) Serum and tissue trace elements in colorectal cancer. J Surg Oncol 52: 172–175. [DOI] [PubMed] [Google Scholar]
- 63. Zowczak-Drabarczyk M, Torlinska T, Iskra M, Mielcarz G, Matylla G, et al. (2004) Serum zinc concentration in patients with colorectal cancer. Trace Elem Electrolytes 21: 236–239. [Google Scholar]
- 64. Kim ES, Lim CS, Chun HJ, Keum B, Seo YS, et al. (2012) Detection of Cu(I) and Zn(II) ions in colon tissues by multi-photon microscopy: novel marker of antioxidant status of colon neoplasm. J Clin Pathol 65: 882–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hornik P, Milde D, Trenz Z, Vyslouzil K, Stuzka V (2006) Colon tissue concentrations of copper, iron, selenium, and zinc in colorectal carcinoma patients. Chem Pap-Chem Zvesti 60: 297–301. [Google Scholar]
- 66. Kucharzewski M, Braziewicz J, Majewska U, Gozdz S (2003) Selenium, copper, and zinc concentrations in intestinal cancer tissue and in colon and rectum polyps. Biol Trace Elem Res 92: 1–10. [DOI] [PubMed] [Google Scholar]
- 67. Shukla VK, Adukia TK, Singh SP, Mishra CP, Mishra RN (2003) Micronutrients, antioxidants, and carcinoma of the gallbladder. J Surg Oncol 84: 31–35. [DOI] [PubMed] [Google Scholar]
- 68. Gupta SK, Singh SP, Shukla VK (2005) Copper, zinc, and Cu/Zn ratio in carcinoma of the gallbladder. J Surg Oncol 91: 204–208. [DOI] [PubMed] [Google Scholar]
- 69. Rautray TR, Vijayan V, Sudarshan M, Panigrahi S (2009) Analysis of blood and tissue in gallbladder cancer. Nucl Instrum Methods Phys Res Sect B-Beam Interact Mater Atoms 267: 2878–2883. [Google Scholar]
- 70. Nagasue N, Kohno H, Chang YC, Nakamura T (1989) Iron, Copper and Zinc Levels in Serum and Cirrhotic Liver of Patients with and without Hepatocellular-Carcinoma. Oncology 46: 293–296. [DOI] [PubMed] [Google Scholar]
- 71. Poo JL, Rosas-Romero R, Montemayor AC, Isoard F, Uribe M (2003) Diagnostic value of the copper/zinc ratio in hepatocellular carcinoma: a case control study. J Gastroenterol 38: 45–51. [DOI] [PubMed] [Google Scholar]
- 72. Kolachi NF, Kazi TG, Afridi HI, Kazi NG, Khan S (2012) Investigation of essential trace and toxic elements in biological samples (blood, serum and scalp hair) of liver cirrhotic/cancer female patients before and after mineral supplementation. Clin Nutr 31: 967–973. [DOI] [PubMed] [Google Scholar]
- 73. Ebara M, Fukuda H, Hatano R, Yoshikawa M, Sugiura N, et al. (2003) Metal contents in the liver of patients with chronic liver disease caused by hepatitis C virus - Reference to hepatocellular carcinoma. Oncology 65: 323–330. [DOI] [PubMed] [Google Scholar]
- 74. Kew MC, Mallett RC (1974) Hepatic zinc concentrations in primary cancer of the liver. Br J Cancer 29: 80–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Liaw KY, Lee PH, Wu FC, Tsai JS, LinShiau SY (1997) Zinc, copper, and superoxide dismutase in hepatocellular carcinoma. Am J Gastroenterol 92: 2260–2263. [PubMed] [Google Scholar]
- 76. Maeda T, Shimada M, Harimoto N, Tsujta E, Maehara S, et al. (2005) Role of tissue trace elements in liver cancers and non-cancerous liver parenchyma. Hepato-Gastroenterol 52: 187–190. [PubMed] [Google Scholar]
- 77. Okuno T, Shimamura Y, Mizuno M, Miyata S, Miyake T, et al. (1988) Trace-Elements in Hepatoma Tissue. Trace Elem Med 5: 130–136. [Google Scholar]
- 78. Tashiro H, Kawamoto T, Okubo T, Koide O (2003) Variation in the distribution of trace elements in hepatoma. Biol Trace Elem Res 95: 49–63. [DOI] [PubMed] [Google Scholar]
- 79. Darago A, Sapota A, Matych J, Nasiadek M, Skezypinska-Gawrysiak M, et al. (2011) The correlation between zinc and insulin-like growth factor 1 (IGF-1), its binding protein (IGFBP-3) and prostate-specific antigen (PSA) in prostate cancer. Clin Chem Lab Med 49: 1699–1705. [DOI] [PubMed] [Google Scholar]
- 80. Goel T, Sankhwar SN (2006) Comparative study of zinc levels in benign and malignant lesions of the prostate. Scand J Urol Nephrol 40: 108–112. [DOI] [PubMed] [Google Scholar]
- 81. Kiziler AR, Aydemir B, Guzel S, Alici B, Ataus S, et al. (2010) May the level and ratio changes of trace elements be utilized in identification of disease progression and grade in prostatic cancer? Trace Elem Electrolytes 27: 65–72. [Google Scholar]
- 82. Meyer F, Galan P, Douville P, Bairati I, Kegle P, et al. (2005) Antioxidant vitamin and mineral supplementation and prostate cancer prevention in the SU.VI.MAX trial. Int J Cancer 116: 182–186. [DOI] [PubMed] [Google Scholar]
- 83. Whelan P, Walker BE, Kelleher J (1983) Zinc, Vitamin A and Prostatic Cancer. Br J Urol 55: 525–528. [DOI] [PubMed] [Google Scholar]
- 84. Li XM, Zhang L, Li J, Li Y, Wang HL, et al. (2005) Measurement of serum zinc improves prostate cancer detection efficiency in patients with PSA levels between 4 ng/mL and 10 ng/mL. Asian J Androl 7: 323–328. [DOI] [PubMed] [Google Scholar]
- 85. Park SY, Kolonel L (2009) Serum Zinc and Prostate Cancer Risk in the Multiethnic Cohort study. Epidemiology 20: S131–S131. [Google Scholar]
- 86. Brys M, Nawrocka AD, Miekos E, Zydek C, Foksinski M, et al. (1997) Zinc and cadmium analysis in human prostate neoplasms. Biol Trace Elem Res 59: 145–152. [DOI] [PubMed] [Google Scholar]
- 87. Dunchik VN, Zherbin EA, Zaichick VY, Leonov AI, Sviridova TV (1980) Method for differential diagnostics of malignant and benign prostate tumors. Discoveries, Inventions, Commercial Models, Trade Marks 35: 1–13. [Google Scholar]
- 88. Feustel A, Wennrich R, Steiniger D, Klauss P (1982) Zinc and cadmium concentration in prostatic carcinoma of different histological grading in comparison to normal prostate tissue and adenofibromyomatosis (BPH). Urol Res 10: 301–303. [DOI] [PubMed] [Google Scholar]
- 89. Guntupalli JNR, Padala S, Gummuluri A, Muktineni RK, Byreddy SR, et al. (2007) Trace elemental analysis of normal, benign hypertrophic and cancerous tissues of the prostate gland using the particle-induced X-ray emission technique. Eur J Cancer Prev 16: 108–115. [DOI] [PubMed] [Google Scholar]
- 90. Habib FK, Hammond GL, Lee IR, Dawson JB, Mason MK, et al. (1976) Metal-androgen interrelationships in carcinoma and hyperplasia of the human prostate. J Endocrinol 71: 133–141. [DOI] [PubMed] [Google Scholar]
- 91. Marczynska A, Kulpa J, Lenko J (1983) The concentration of zinc in relation to fundamental elements in the diseased human prostate. Int Urol Nephrol 15: 257–265. [DOI] [PubMed] [Google Scholar]
- 92. Mawson CA, Fischer MI (1952) The occurrence of zinc in the human prostate gland. Can J Med Sci 30: 336–339. [DOI] [PubMed] [Google Scholar]
- 93. Sapota A, Darago A, Taczalski J, Kilanowicz A (2009) Disturbed homeostasis of zinc and other essential elements in the prostate gland dependent on the character of pathological lesions. Biometals 22: 1041–1049. [DOI] [PubMed] [Google Scholar]
- 94. Schrodt GR, Hall T, Whitmore WF (1964) The concentration of zinc in diseased human prostate glands. Cancer 17: 1555–1566. [DOI] [PubMed] [Google Scholar]
- 95. Zaichick S, Zaichick V (2012) Trace elements of normal, benign hypertrophic and cancerous tissues of the human prostate gland investigated by neutron activation analysis. Appl Radiat Isot 70: 81–87. [DOI] [PubMed] [Google Scholar]
- 96. Hienzsch E, Schneider H, Anke M (1970) Vergleichende Untersuchungen zurn Mengenund Spurenelernentgehalt der norrnalen Prostata, des Prostataadenoms und des Prostatakarzinorns. Zsehr Urol 63: 543–546. [PubMed] [Google Scholar]
- 97. Hoare R, Delory GE, Penner DW (1956) Zinc and acid phosphatase in the human prostate. Cancer 9: 721–726. [DOI] [PubMed] [Google Scholar]
- 98. Garofalo JA, Erlandson E, Strong EW, Lesser M, Gerold F, et al. (1980) Serum zinc, serum copper, and the Cu/Zn ratio in patients with epidermoid cancers of the head and neck. J Surg Oncol 15: 381–386. [DOI] [PubMed] [Google Scholar]
- 99. Jayadeep A, Pillai KR, Kannan S, Nalinakumari KR, Mathew B, et al. (1997) Serum levels of copper, zinc, iron and ceruloplasmin in oral leukoplakia and squamous cell carcinoma. J Exp Clin Cancer Res 16: 295–300. [PubMed] [Google Scholar]
- 100. Taysi S, Akcay F, Uslu C, Dogru Y, Gulcin I (2003) Trace elements and some extracellular antioxidant protein levels in serum of patients with laryngeal cancer. Biol Trace Elem Res 91: 11–18. [DOI] [PubMed] [Google Scholar]
- 101. Akcil E, Caylakli F, Akiner M, Kocak M (2004) Trace element concentrations and superoxide dismutase and catalase activities in benign and malignant larynx tumors. Biol Trace Elem Res 101: 193–201. [DOI] [PubMed] [Google Scholar]
- 102. Drozdz M, Gierek T, Jendryczko A, Piekarska J, Pilch J, et al. (1989) Zinc, Vitamin-a and Vitamin-E, and Retinol-Binding Protein in Sera of Patients with Cancer of the Larynx. Neoplasma 36: 357–362. [PubMed] [Google Scholar]
- 103. Durak I, Kavutcu M, Canbolat O, Isik AU, Akyol O (1994) Concentrations of Some Major and Minor Elements in Larynx Tissues with and without Cancer. Biometals 7: 45–48. [DOI] [PubMed] [Google Scholar]
- 104. Yigitbasi OG, Haghighi N, Dogan P, Saraymen R, Balkani S, et al. (1998) Differences of tissue Cu and Zn levels in larynx squamous cell carcinomas. Trace Elem Electrolytes 15: 90–93. [Google Scholar]
- 105. Al-Sayer H, Mathew TC, Asfar S, Khourshed M, Al-Bader A, et al. (2004) Serum changes in trace elements during thyroid cancers. Mol Cell Biochem 260: 1–5. [DOI] [PubMed] [Google Scholar]
- 106. Przybylik-Mazurek E, Zagrodzki P, Kuzniarz-Rymarz S, Hubalewska-Dydejczyk A (2011) Thyroid Disorders-Assessments of Trace Elements, Clinical, and Laboratory Parameters. Biol Trace Elem Res 141: 65–75. [DOI] [PubMed] [Google Scholar]
- 107. Leung PL, Li XL (1996) Multielement analysis in serum of thyroid cancer patients before and after a surgical operation. Biol Trace Elem Res 51: 259–266. [DOI] [PubMed] [Google Scholar]
- 108. Zaichick VY, Tsyb AF, Vtyurin BM (1995) Trace elements and thyroid cancer. Analyst 120: 817–821. [DOI] [PubMed] [Google Scholar]
- 109. Kucharzewski M, Braziewicz J, Majewska U, Gozdz S (2003) Copper, zinc, and selenium in whole blood and thyroid tissue of people. with various thyroid diseases. Biol Trace Elem Res 93: 9–18. [DOI] [PubMed] [Google Scholar]
- 110. Homma S, Sasaki A, Nakai I, Sagai M, Koiso K, et al. (1993) Distribution of Copper, Selenium, and Zinc in Human Kidney Tumors by Nondestructive Synchrotron-Radiation X-Ray-Fluorescence Imaging. J Trace Elem Exp Med 6: 163–170. [Google Scholar]
- 111. Dobrowolski Z, Drewniak T, Kwiatek W, Jakubik P (2002) Trace elements distribution in renal cell carcinoma depending on stage of disease. Eur Urol 42: 475–480. [DOI] [PubMed] [Google Scholar]
- 112. Kwiatek WM, Drewniak T, Lekka M, Wajdowicz A (1996) Investigation of trace elements in cancer kidney tissues by SRIXE and PIXE. Nucl Instrum Methods Phys Res Sect B-Beam Interact Mater Atoms 109: 284–288. [Google Scholar]
- 113. Atukorala S, Basu TK, Dickerson JW, Donaldson D, Sakula A (1979) Vitamin A, zinc and lung cancer. Br J Cancer 40: 927–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Klarod K, Hongsprabhas P, Khampitak T, Wirasorn K, Kiertiburanakul S, et al. (2011) Serum antioxidant levels and nutritional status in early and advanced stage lung cancer patients. Nutrition 27: 1156–1160. [DOI] [PubMed] [Google Scholar]
- 115. Diez M, Arroyo M, Cerdan FJ, Munoz M, Martin MA, et al. (1989) Serum and tissue trace metal levels in lung cancer. Oncology 46: 230–234. [DOI] [PubMed] [Google Scholar]
- 116. Oyama T, Matsuno K, Kawamoto T, Mitsudomi T, Shirakusa T, et al. (1994) Efficiency of serum copper/zinc ratio for differential diagnosis of patients with and without lung cancer. Biol Trace Elem Res 42: 115–127. [DOI] [PubMed] [Google Scholar]
- 117. Beeley JM, Darke CS, Owen GCR (1974) Serum zinc, bronchiectasis, and bronchial carcinoma. Thorax 29: 21–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Cildag O, Altinisik M, Kozaci D, Karadag F, Kiter G, et al. (2004) Alterations in trace elements and oxidative stress in lung cancer. Trace Elem Electrolytes 21: 23–27. [Google Scholar]
- 119. Kune GA, Kune S, Watson LF, Pierce R, Field B, et al. (1989) Serum levels of beta-carotene, vitamin A, and zinc in male lung cancer cases and controls. Nutr Cancer 12: 169–176. [DOI] [PubMed] [Google Scholar]
- 120. Sadat AFMN, Hossain MI, Hossain MK, Reza MS, Nahar Z, et al. (2008) Serum trace elements and immunoglobulin profile in lung cancer patients. J Appl Res 8: 24–33. [Google Scholar]
- 121. Jin Y, Zhang C, Xu H, Xue S, Wang Y, et al. (2010) Combined effects of serum trace metals and polymorphisms of CYP1A1 or GSTM1 on non-small cell lung cancer: A hospital based case-control study in China. Cancer Epidemiol 35: 182–187. [DOI] [PubMed] [Google Scholar]
- 122. Sattar N, Scott HR, McMillan DC, Talwar D, O’Reilly DS, et al. (1997) Acute-phase reactants and plasma trace element concentrations in non-small cell lung cancer patients and controls. Nutr Cancer 28: 308–312. [DOI] [PubMed] [Google Scholar]
- 123. Adachi S, Takemoto K, Ohshima S, Shimizu Y, Takahama M (1991) Metal concentrations in lung tissue of subjects suffering from lung cancer. Int Arch Occup Environ Health 63: 193–197. [DOI] [PubMed] [Google Scholar]
- 124. Kubala-Kukus A, Braziewicz J, Banas D, Majewska U, Gozdz S, et al. (1999) Trace element load in cancer and normal lung tissue. Nucl Instrum Methods Phys Res Sect B-Beam Interact Mater Atoms 150: 193–199. [Google Scholar]
- 125. Zhang LL, Lv JG, Sun SK (2012) Elements in Lung Tissues of Patients from a High Lung Cancer Incidence Area of China. Biol Trace Elem Res 148: 7–10. [DOI] [PubMed] [Google Scholar]
- 126. Cousins RJ, Liuzzi JP, Lichten LA (2006) Mammalian zinc transport, trafficking, and signals. J Biol Chem 281: 24085–24089. [DOI] [PubMed] [Google Scholar]
- 127. Costello LC, Franklin RB (2011) Zinc is decreased in prostate cancer: an established relationship of prostate cancer! J Biol Inorg Chem. 16: 3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Prisma 2009 checklist.
(DOC)
Meta-regression analysis of overall results using mixed effects model (unrestricted maximum likehood). SMD, standardized mean difference.
(XLSX)
Source data set extracted from studies used for analysis. Including methodological quality of studies based on Newcastle-Ottawa scale, study design, and information regarding matching cases and controls. NS, not specified, NOS, Newcastle-Ottawa scale, stdev, standard deviation.
(XLSX)