Abstract
This study aims to examine which resources older adults utilize for their health information needs, how trustworthy and reliable they find these resources, and the difficulties they face in obtaining health-related information. A 41-item survey designed to understand the information-seeking characteristics of older adults was developed and distributed to retirement communities. Some items were taken from the Health Information National Trends Survey. Of 1520 surveys, 403 were returned completed (26.6%). Respondents’ mean age was 77.65 years. Average scores indicated respondents trusted particular sources of health information in the following order (highest to lowest): health care providers, pharmacists, friends and relatives, retirement community staff, newspapers, the Internet, television, and the radio. In conclusion, older adults have a greater amount of trust in a person with whom they are able to actively discuss their health as opposed to a nonliving source, which they have to access or manipulate, such as the Internet. Efforts must be made to help older adults better navigate and utilize the Internet and recognize dependable online sources so that they may increase their trust in its use, thereby increasing satisfaction with their own ability to seek and use sources of health information.
Keywords: Health Information National Trends Survey, Health information-seeking behavior, Krantz Health Opinion Survey, Survey
As of 2009, the Administration on Aging estimated the current population of older adults in the US (those aged ≥65 years) to be 39.6 million representing 12.9% of the US population, a number projected to grow to 19% by 2030.1 Within this group, health and well-being are important considerations in order to maintain independence. Older adults have differing healthcare challenges that are often more prevalent and chronic compared with younger adults.2 Providing older adults with multiple health information resources both during and outside clinical encounters becomes essential to informed health decision making as demonstrated by studies that have shown that patients who pose questions, provide feedback, and actively engage during clinical visits have measurably improved health outcomes.3
Understanding health information-seeking behavior, which focuses on understanding how individuals obtain information about health, illness, and various risks to health,4 is a growing area of research. One example of ongoing research in this domain is the Health Information National Trends Survey (HINTS), a routinely collected national survey created to understand how adults use different communication channels to obtain health information and to create more effective health communication strategies across populations.5 Health information seeking of the general public related to cancer is specifically targeted by HINTS. However, health information-seeking behavior pertaining to general health specifically within the older adult population is an understudied area. This is a critical topic to better understand as older adults have been cited as the heaviest users of healthcare resources, and their information needs can differ from the general population.6 These differences may include limited proficiency with computer usage and the Internet, as well as reluctance to depart from traditional paternalistic models of healthcare.7,8 Although these differences do exist, older adults have been found to be just as likely to use health information as other age groups.9
A limited number of studies to date have examined health information needs and behaviors of older adults. For cancer survivors, it has been documented that older survivors were less likely to seek out information compared with their younger counterparts and more likely to seek information from friends, family, or books than from the Internet.10 Other work has examined the extent to which older adults utilize the Internet to search for information on heart attacks and found that only 57% of older adults had access to the Internet, and of these about half sought health information on the Internet.11 Haverhals et al12 interviewed older adults to better understand their health information-seeking behaviors and found the majority of participants sought medication information from pharmacists and clinicians. Although physicians and nurses were highly valued as trusted sources for health related questions, many subjects felt their doctors were too busy to address information needs. Pharmacists were generally the most trusted information source. Other sources included the patient’s family, friends, reference books, and even medication inserts. Participants reported using the Internet when they needed quick answers but were skeptical about the reliability of Web sites. The study did not specifically examine the role of nurses in medication education or management. These findings are similar to the study by Taha et al13 that included focus groups with older adults who were divided into Internet-user and nonuser groups. Whereas the most common source of information for all groups included physicians, the second most common source differed between the groups with non-Internet users reporting friends and family, and Internet users reporting the Internet.
The current literature examining health information needs and behaviors of older adults provides insight into the sources of information but limited evidence on access to these sources. In order to fully address information-seeking behaviors and improve health communication for older adults, we need to examine the sources and tools used to access information as well as the barriers to accessing and processing the retrieved information.
The purpose of this study was to understand older adults’ health information-seeking behaviors. Specifically, we aimed to answer the following research questions: (1) Which resources do older adults utilize for their health information needs? (2) How trustworthy and reliable do they find these resources? (3) What are the difficulties they face in obtaining health-related information? The ultimate goal of this work was to provide evidence that will inform the design of communication strategies and interventions that reduce the burden of decision making of older adults and more effectively meet their healthcare needs.
METHODS
Design
We conducted a cross-sectional anonymous survey using a convenience sample of community-dwelling older adults in the state of Washington.
Sample and Settings
We distributed the survey to 11 retirement communities throughout the Puget Sound area. The communities selected for inclusion represented a wide range of socioeconomic backgrounds. Eligible subjects were residents 55 years or older of the participating communities with the ability to read and write English. The study received human subject approval from the University of Washington’s institutional review board.
Instrument
We developed a survey based on a review of the literature and available instruments. Our study was informed in part by the HINTS theoretical framework, which recognizes two general stages in consumer-oriented health communication: (1) an awareness stage in which persuasive media push messages into awareness and contemplation, and (2) an information-seeking stage in which consumers pull information from sources.5 We expanded upon the HINTS instrument with our work to gain further insight into the second stage “pull” processing specifically for older adults; this was reflected by the additional components in our survey instrument. Specifically, we added items on sociodemographic characteristics that may affect health communication, barriers to information seeking, and control in information retrieval. These items were added to better understand what prevented older adults from retrieving their information and assess their degree of control over their information. The final survey consisted of 41 items presented in three sections.
The first section of the survey contained demographic questions. Two of the items assessed frequency of usage of (1) a television and (2) a computer with Internet access on a Likert-type scale. The second section contained trust and information retrieval questions. We used previously validated questions found from the HINTS survey related to trust in sources of information and access to information. These questions ask how much people would trust various sources on a Likert-type scale of 1 (“not at all”) to 4 (“a lot”). Finally, to validate subjects’ responses and solicit additional options for information sources, we included two open-ended questions asking the subject to provide more detail about information sources. A third open-ended item includes a scenario about new medication and then asks how subjects would seek additional information to resolve the situation. The final section of the survey addressed control in information retrieval using items from the information subscale of the Krantz Health Opinion Survey (HOS),14 a validated instrument developed to measure a person’s attitude toward treatment. High scores represent favorable attitudes toward self-directed or informed treatment.
Procedures
Surveys were distributed and collected in winter 2012. A box was placed in a central location within each of the facilities for participants to return completed surveys. In general, 2 weeks were allowed in between drop-off and collection of the survey.
Survey responses were manually entered into a study database. Double data entry was conducted for 25% of survey responses to ensure accuracy.
Analysis
Demographics and Likert-type scaled items were analyzed using descriptive statistics as well as Kruskal-Wallis analysis of variance, Mann-Whitney U tests, Tukey tests, and t tests as appropriate. Mann-Whitney U tests were applied to make comparisons between this sample and publicly available 2007 HINTS sample data. Survey data were also compared for differences by several demographic criteria. Bonferroni correction was used to adjust for multiple comparisons.
To determine similarities in trust levels among different sources, cluster analyses were conducted. For each pair of information sources, a count was generated representing the number of occurrences where the sources were equally rated for trust. The total count was normalized by calculating a cosine similarity measure between any two information sources. This cosine similarity was used to generate a distance matrix across each information source. We applied an agglomerative hierarchical clustering using the cosine metric to identify and visualize information sources similarly rated in trust. All analyses and visualization were generated in Excel or R.
An initial analysis of open-ended responses was conducted. The most common answers were initially coded to form a list that was then discussed with the research team to determine agreement with labeling. Then each team member was asked to review and code approximately 100 open-ended answers using the themes from the previously discussed list. Interrater reliability was performed on a random sample of 10% of items to ensure proper coding.
RESULTS
Survey Distribution
Of 1520 distributed surveys, 403 were returned completed (26.6% response rate). The 403 survey respondents ranged in age from 57 to 100 years (mean, 77.65 [SD, 9.77] years). Further demographic data describing the sample are available in the Table 1.
Table 1.
Demographic Data From 403 Respondents
| Demographic Data | |
|---|---|
| Age, mean (SD), y | 77.65 (9.77) |
| Gender, % (n) | |
| Male | 28.5 (115) |
| Female | 70.2 (283) |
| Race, % (n) | |
| White | 90.7 (341) |
| Asian/American | 4.8 (18) |
| Black/African American | 2.9 (11) |
| Multiracial | 1.7 (7) |
| American Indian or Alaskan Native | 1.3 (5) |
| Native Hawaiian or other Pacific Islander | 0.3 (1) |
| Economic status median (1st quartile, 3rd quartile) | |
| Will you have enough income for the future? | 2 (2, 3) |
| Would you say you have enough income for the little extras? | 2 (1, 3) |
| Would you say your household is able to make ends meet? | 3 (2, 3) |
| Education level, % (n) | |
| Less than high school | 4.21 (16) |
| High school/GED | 19.74 (75) |
| Some college | 29.47 (112) |
| Associates degree | 10.00 (38) |
| Bachelor’s degree | 20.26 (77) |
| Graduate degree | 16.32 (62) |
Percentages do not add up to 100 because of blank or double answers in various categories. Range: 1–4, 1 indicating having difficulty in managing finances and 4 indicating ease in managing finances.
Use of Television and the Internet
When asked how often the subjects watch television, the majority (57.8%) responded “frequently,” whereas less than 5% responded “never.” In contrast, when asked how often the subjects use a computer with an Internet connection, almost equal proportion of respondents responded “frequently” or “never” (36.7% vs 37.5%).
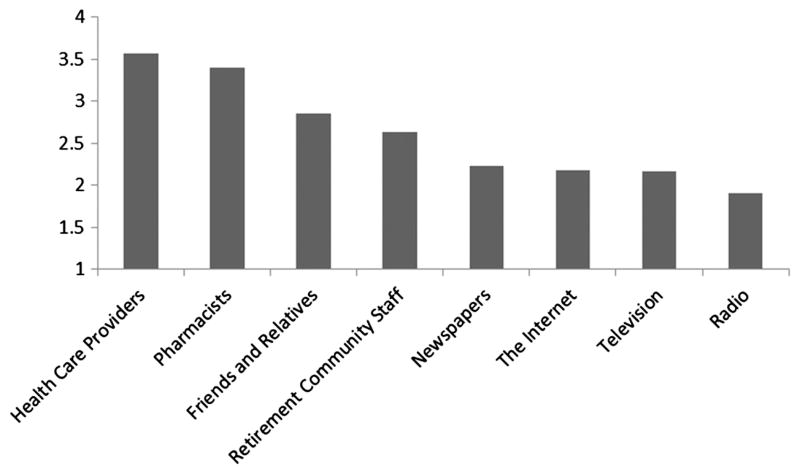
Trust/Information Retrieval/Krantz Survey
Average trust scores indicated that our participants had the highest levels of trust in health care providers, and the lowest levels of trust in the radio. Scores for the various sources can be seen in Figure 1. Hierarchical clustering of information sources based on similarity of responses to the information trust question initially shows a division in trust among media sources such as the Internet, newspaper, television, and radio compared with human-based sources. Within human-based sources, there is a further grouping into health care providers (eg, nurses, physicians) and pharmacists as one set and friends and relatives and retirement community staff as another set.
FIGURE 1.
Average trust level rating for each source. Higher scores indicate greater level of trust (possible range, 1–4).
Three open-ended questions were utilized to check the reliability of the short answers and to discover any unlisted sources (Figure 2). Answers to all three questions indicate health care providers and the Internet as highly used sources of information. Pharmacists were seen as the most used source of information for the third question. Other commonly cited sources included books, family, friends, and clinics.
FIGURE 2.
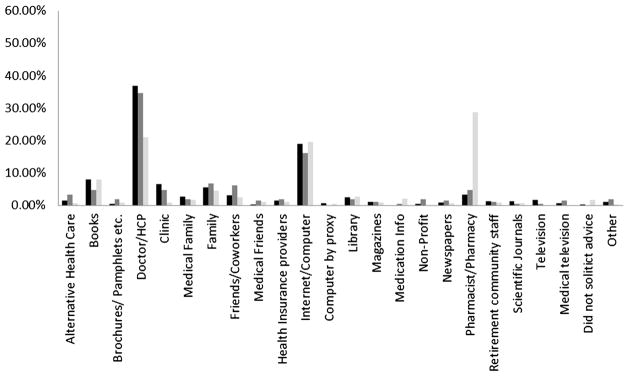
Where health information is sought by older adults: answers to three open-ended questions. Black = when you looked for information, where did you seek it first? Dark gray = if yes, where else did you seek information? Light gray = where would you look for more information?
In terms of information retrieval, the survey asks four questions focusing on the last time the subject searched for health information, including the amount of effort it took to get the necessary information, how frustrated they felt while searching for information, the concern they felt for the quality of information, and how easy the information was to understand. The average answer to each of the four questions was similar, ranging from 2.1 to 2.4 with an SD of approximately 1.0 for all questions. The average Krantz HOS information score for survey respondents (n = 334) was 4.46 (SD, 2.12), indicating a fairly average desire to ask questions or be informed about medical decisions in our sample.
Gender Stratification
There were no significant differences between men and women in terms of trust and information retrieval. However, women had a significantly higher HOS score than did men (P = .001).
Education Level Stratification
The overall population was stratified into three groups: those who had reported having a high school degree/GED or less (n = 90), those who attended some college (n = 150), and those who had a bachelor’s degree or higher (n = 139). Information was reported to be more difficult to understand as education level decreased (P = .04); however, this difference did not hold under post hoc testing with Bonferroni correction.
Use of a computer with an Internet connection significantly increased as education level increased (P <.001). On post hoc analysis, the group with high school education or less was significantly less likely to use a computer than the group with some college (P = .02). Similarly, those in the group with high school education or less were less likely to use a computer than those in the group with a bachelor’s degree or higher (P <.001).
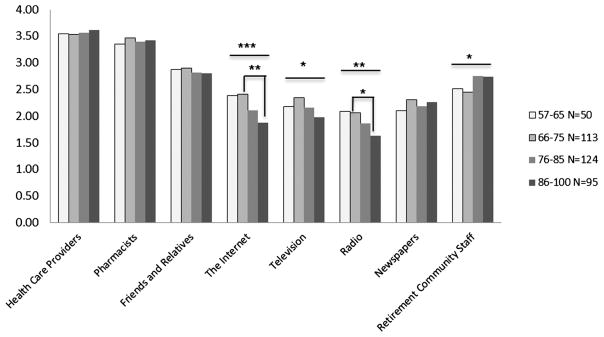
Stratification by Age
When looking at age, the overall population was stratified into four separate groups: 55 to 65 years (n = 50), 66 to 75 years (n = 113), 76 to 85 years (n = 124), and 86 to 100 years (n = 95). Differences in trust among age groups can be seen in Figure 3. No significant differences were found among the four groups in terms of information retrieval. It was also seen that frustration during a search for information tended to decrease with age.
FIGURE 3.
Comparison of trust between the four age groups. *P ≤.05, **P ≤.01,***P ≤.001.
There was a decrease in computer use noted with increasing age (P <.001). Post hoc testing showed significant differences in computer use when comparing the 57- to 65-year and 86- to 100-year group (P = .002), the 66- to 75-year and 86- to 100-year group (P <.001), and the 76- to 85-year with the 86- to 100-year group (P = .04). Krantz HOS score decreased significantly as age increased (P <.001), indicating reduced attitude toward self-directed care. Post hoc testing revealed significant group differences in HOS score between those aged 55 to 65 years and 76 to 85 years (P = .02) and those aged 86 to 100 years (P <.001). Similar differences in HOS score were also seen between those aged 65 to 75 years and the older two age categories (76–85 years, P <.001; 86–100 years, P <.001).
Stratification by Economic Status
In order to analyze trust by wealth, the answers to the three economic questions were averaged. The scores were on a scale of 1 to 4, with 1 indicating having difficulty in managing finances and 4 indicating ease in managing finances. The population was split into three groups based on their average scores: those whose average scores were less than 2, lower socioeconomic (LS); those that averaged between 2 and 3, middle socioeconomic; and those whose average answers were greater than 3, upper socioeconomic.
As economic status increased, trust in health care providers (P = .03) and retirement community staff (P = .001) increased. Post hoc testing indicated that those in the upper socioeconomic group reported significantly higher levels of trust in health information provided by retirement community staff (P = .01) than did the LS group. Furthermore, as economic status increased, the effort required (P = .03) and frustration experienced (P = .009) when looking to retrieve health information decreased. Interestingly, as wealth increased, there was a significant decrease in desire for health information and to be informed about medical decision making, indicated by a decline in HOS information subscale score (P <.001). Both the LS and the middle socioeconomic groups scored significantly higher on the HOS than on the upper socioeconomic group (P <.001, P = .02, respectively).
Stratification by Internet Use
The sample was grouped into three categories by responses to how often they used a computer with Internet access: those who reported “never” (n = 151) and those who reported “frequently” (n = 148) represented two distinct groups. In order to account for their smaller sample sizes, those who reported “rarely” (n = 34) and those who reported “sometimes” (n = 60) were grouped together. Not surprisingly, as frequency of Internet use increases, trust in the Internet increased (P <.001). In terms of information retrieval, there was a significant increase in ability to understand the information as computer usage increased (P = .002).
DISCUSSION
Our sample’s responses to questions related to trust of information sources and retrieval of information are similar to those of the nationally validated HINTS findings for people 55 years or older (n = 3887). Some significant differences, however, were found between our sample and the national population when looking at trust in radio, the Internet, or friends and relatives. However, trust in health care providers and television or concerns over the quality of the information and ability to understand information the two samples were similar. These results provide support toward the consistency and generalizability of our findings to a national sample as well as provide a glimpse into how older adults have changed over the last 5 years.
Trust in information sources appears to be grouped into two categories: living and nonliving sources. Survey respondents indicated trusting living sources (eg, health care providers, relatives, and retirement community staff) to a greater extent than any of the nonliving sources (eg, radio, the Internet). Some of these results, especially the overwhelming trust in health care providers, are supported by other studies.10,12,13,15,16 Our data indicate that older adults appear to have a greater amount of trust in a person with whom they are able to actively discuss their health as opposed to a nonliving source, which they have to access or manipulate. This finding aligns with previous results about older adult treatment behaviors, which indicate that as people age they are less inclined toward self-directed forms of health management.17–21 Older adults may therefore have a greater need to trust living sources for health information as they are less interested in independently gathering health information to manage their own health. With the aging of the “baby boomer” generation, who have been shown to have more interest in wellness activities and are generally more technologically savvy, it will be important to monitor these trends in the future.22
Interestingly, responses to open-ended questions produced slightly different results in terms of source utilization. The most cited responses for where people go to for their health information still involve health care providers; however, the next most common response was the Internet. According to people’s trust level, we might have expected another living source such as pharmacists. However, this is not too surprising as answers based on trust do not necessarily indicate levels of efficiency, accessibility, or use. Similar to previous work by Haverhals et al, 12 where patients trusted physicians but felt uncomfortable bothering them, the respondents in our study may not fully trust the Internet but find it to be the easiest source to consult when in need of information. Past studies have shown that other sources are even used to prepare for a discussion with a healthcare provider or to help understand what was discussed.13,23 Our study indicates that those who reported using the Internet more often reported being better able to understand the information they were given. Given this finding, efforts need to be made by nurses and other healthcare providers to help older adults better understand the Internet and recognize dependable online sources so that their trust in its use increases. Many different methods of increasing the ability of older adults to gain access to the Internet have been tried with success.3,7,24–26 By helping older adults trust and utilize the Internet effectively, researchers and system designers may be able reduce the information burden on other sources and increase the satisfaction of older adults with their ability to seek and use sources of health information.
The demographic analyses also revealed interesting trends in trust, as trust in retirement community staff and health care providers increases significantly as wealth increases. Similarly, information retrieval appears to be most affected by income, as those in the upper socioeconomic class were significantly less frustrated in their search for information than those who reported being in an LS class. This divide could be caused by several factors including a lack of information sources for those with less means or even a lack of understanding on how to use such sources.27,28 This is a cause for concern as health information should be available to all people regardless of economic status through such venues as public libraries and health systems. Bridging this gap should not only involve increasing the amount of information available to everyone, but also improving older adults’ user experience in utilizing technology to gather this information.3,7,24,27
Although we made every attempt to draw from a racially and ethnically diverse population, our sample consisted mostly of white older adults. This can be viewed as a limitation, and future work should explore these issues in more diverse samples of older adults. The relatively low (26%) response rate seen in this study may indicate a nonresponse bias; however, the response rate is similar to that of other published paper-and-pencil–based surveys with older adults, especially those in which no compensation or follow-up reminders for survey completion were provided.29–32
CONCLUSION
The nature of the survey limits generalizability of findings. However, our work provides a glimpse into the ways older adults get their information and which sources they find the most trustworthy. In terms of trust, health care providers, such as nurses, stand out as the most trusted source of health information for adults older than 55 years, even more than pharmacists. This highlights the need to design tools that support increased communication between older adults and these sources. This work can inform the development of personal health information management tools as well as inspire more research into how older adults seek and process health information. In addition, this work provides evidence to inform communication strategies and interventions when working with older adults. Efforts need to be made by nurses and other healthcare professionals to help older adults better understand the Internet and recognize dependable online sources so that they may increase their trust in its use. By assisting older adults to trust and utilize the Internet effectively, we may allow them to be more satisfied with their own ability to seek and use sources of health information.
Acknowledgments
This work was supported by the National Library of Medicine Biomedical and Health Informatics Training Grant Program (grant 2T15LM007442-11).
The authors acknowledge and thank ERA living, the Senior Housing Assistance Group, and Council House for allowing and assisting them in distributing their surveys to their communities. They also thank all of the members of the HEALTH-E group for their assistance in coding and reviewing this article: Amanda Lazar, Blaine Reeder, Jane Chung, Jonathan Joe, Ellen Meyer, Jina Huh, and Alex Constant.
Footnotes
The authors confirm that all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
The authors have disclosed that they have no significant relationship with, or financial interest in, any commercial companies pertaining to this article.
References
- 1.Administration on Aging. [Accessed June 8, 2012];A Profile of Older Americans. 2011 http://www.aoa.gov/aoaroot/aging_statistics/Profile/2011/docs/2011profile.pdf.
- 2.Kovner CT, Mezey M, Harrington C. Who cares for older adults? Workforce implications of an aging society. Health Aff (Millwood) 2002;21(5):78–89. doi: 10.1377/hlthaff.21.5.78. [DOI] [PubMed] [Google Scholar]
- 3.Campbell RJ, Nolfi DA. Teaching elderly adults to use the Internet to access health care information: before-after study. J Med Internet Res. 2005;7(2):e19. doi: 10.2196/jmir.7.2.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cutilli CC. Seeking health information: what sources do your patients use? Orthop Nurs. 2010;29(3):214–219. doi: 10.1097/NOR.0b013e3181db5471. [DOI] [PubMed] [Google Scholar]
- 5.Nelson DE, Kreps GL, Hesse BW, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9(5):443–460. doi: 10.1080/10810730490504233. discussion 444–481. [DOI] [PubMed] [Google Scholar]
- 6.Rice DP, Fineman N. Economic implications of increased longevity in the United States. Annu Rev Public Health. 2004;25:457–473. doi: 10.1146/annurev.publhealth.25.101802.123054. [DOI] [PubMed] [Google Scholar]
- 7.Detlefsen EG. Where am I to go? Use of the Internet for consumer health information by two vulnerable communities. Libr Trends. 2004;53(2):283–300. [Google Scholar]
- 8.Smith-Barbaro PA, Licciardone JC, Clarke HF, Coleridge ST. Factors associated with intended use of a Web site among family practice patients. J Med Internet Res. 2001;3(2):E17. doi: 10.2196/jmir.3.2.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wagner LS, Wagner TH. The effect of age on the use of health and self-care information: confronting the stereotype. Gerontologist. 2003;43(3):318–324. doi: 10.1093/geront/43.3.318. [DOI] [PubMed] [Google Scholar]
- 10.Bennett JA, Cameron LD, Whitehead LC, Porter D. Differences between older and younger cancer survivors in seeking cancer information and using complementary/alternative medicine. J Gen Intern Med. 2009;24(10):1089–1094. doi: 10.1007/s11606-009-0979-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meischke H, Eisenberg M, Rowe S, Cagle A. Do older adults use the Internet for information on heart attacks? Results from a survey of seniors in King County, Washington. Heart Lung. 2005;34(1):3–12. doi: 10.1016/j.hrtlng.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Haverhals LM, Lee CA, Siek KA, et al. Older adults with multi-morbidity: medication management processes and design implications for personal health applications. J Med Internet Res. 2011;13(2):e44. doi: 10.2196/jmir.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taha J, Sharit J, Czaja S. Use of and satisfaction with sources of health information among older Internet users and nonusers. Gerontologist. 2009;49(5):663–673. doi: 10.1093/geront/gnp058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krantz DS, Baum A, Wideman M. Assessment of Preferences for self-treatment and information in health care. J Pers Soc Psychol. 1980;39(5):977–990. doi: 10.1037//0022-3514.39.5.977. [DOI] [PubMed] [Google Scholar]
- 15.Donohue JM, Huskamp HA, Wilson IB, Weissman J. Whom do older adults trust most to provide information about prescription drugs? Am J Geriatr Pharmacother. 2009;7(2):105–116. doi: 10.1016/j.amjopharm.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hillen MA, de Haes HC, Smets EM. Cancer patients’ trust in their physician—a review. Psychooncology. 2011;20(3):227–241. doi: 10.1002/pon.1745. [DOI] [PubMed] [Google Scholar]
- 17.Woodward NJ, Wallston BS. Age and health care beliefs: self-efficacy as a mediator of low desire for control. Psychol Aging. 1987;2(1):3–8. doi: 10.1037//0882-7974.2.1.3. [DOI] [PubMed] [Google Scholar]
- 18.Turk-Charles S, Meyerowitz BE, Gatz M. Age differences in information-seeking among cancer patients. Int J Aging Hum Dev. 1997;45(2):85–98. doi: 10.2190/7CBT-12K3-GA8H-F68R. [DOI] [PubMed] [Google Scholar]
- 19.Arora NK, McHorney CA. Patient preferences for medical decision making: who really wants to participate? Med Care. 2000;38(3):335–341. doi: 10.1097/00005650-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20(6):531–535. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Say R, Murtagh M, Thomson R. Patients’ preference for involvement in medical decision making: a narrative review. Patient Educ Couns. 2006;60(2):102–114. doi: 10.1016/j.pec.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Rainie L. [Accessed July 8, 2012];Baby Boomers and Technology. 2012 http://www.pewinternet.org/Presentations/2012/Mar/Baby-Boomer-Summit.aspx.
- 23.Tian Y, Robinson JD. Incidental health information use and media complementarity: a comparison of senior and non-senior cancer patients. Patient Educ Couns. 2008;71(3):340–344. doi: 10.1016/j.pec.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 24.Campbell R. Older women and the Internet. J Women Aging. 2004;16(1–2):161–174. doi: 10.1300/J074v16n01_11. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz DG, Mosher E, Wilson S, Lipkus C, Collins R. Seniors connect: a partnership for training between health care and public libraries. Med Ref Serv Q. 2002;21(3):1–19. doi: 10.1300/J115v21n03_01. [DOI] [PubMed] [Google Scholar]
- 26.Xie B, Bugg JM. Public library computer training for older adults to access high-quality Internet health information. Libr Inf Sci Res. 2009;31(3):155. doi: 10.1016/j.lisr.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lorence DP, Park H, Fox S. Racial disparities in health information access: resilience of the digital divide. J Med Syst. 2006;30(4):241–249. doi: 10.1007/s10916-005-9003-y. [DOI] [PubMed] [Google Scholar]
- 28.Eng TR, Maxfield A, Patrick K, Deering MJ, Ratzan SC, Gustafson DH. Access to health information and support: a public highway or a private road? JAMA. 1998;280(15):1371–1375. doi: 10.1001/jama.280.15.1371. [DOI] [PubMed] [Google Scholar]
- 29.Kaldenberg DO, Koenig HF, Becker BW. Mail survey response rate patterns in a population of the elderly: does response deteriorate with age? Public Opin Q. 1994;58(1):68–76. [Google Scholar]
- 30.Parker L. Collecting data the e-mail way. Train Dev J. 1992;46(7):52. [Google Scholar]
- 31.Cabrera A, Castaneda M, Nora A, Hengstler D. The convergence between two theories of college persistence. J Higher Educ. 1992;63(2):143. [Google Scholar]
- 32.Health Information National Trends Survey 4 (HINTS 4): Cycle 1 Methodology Report. Rockville, MD: Publisher Westat; 2012. [Google Scholar]