Abstract
Objective
For over a decade, the field of medicine has recognized the importance of studying and designing strategies to prevent safety issues in hospitals and clinics. However, there has been less focus on understanding safety in prehospital emergency medical services, particularly in regard to children. Roughly 27.7 million (or 27%) of the annual ED visits are by children under the age of 19, and about 2 million of these children reach the hospital via EMS. This paper adds to our qualitative understanding of the nature and contributors to safety events in the prehospital emergency care of children.
Methods
We conducted four 8–12 person focus groups among paid and volunteer Emergency Medical Services providers to understand: 1) patient safety issues that occur in the prehospital care of children, and 2) factors that contribute to these safety issues (e.g. patient, family, systems, environmental, or individual provider factors). Focus groups were conducted in rural and urban settings. Interview transcripts were coded for overarching themes.
Results
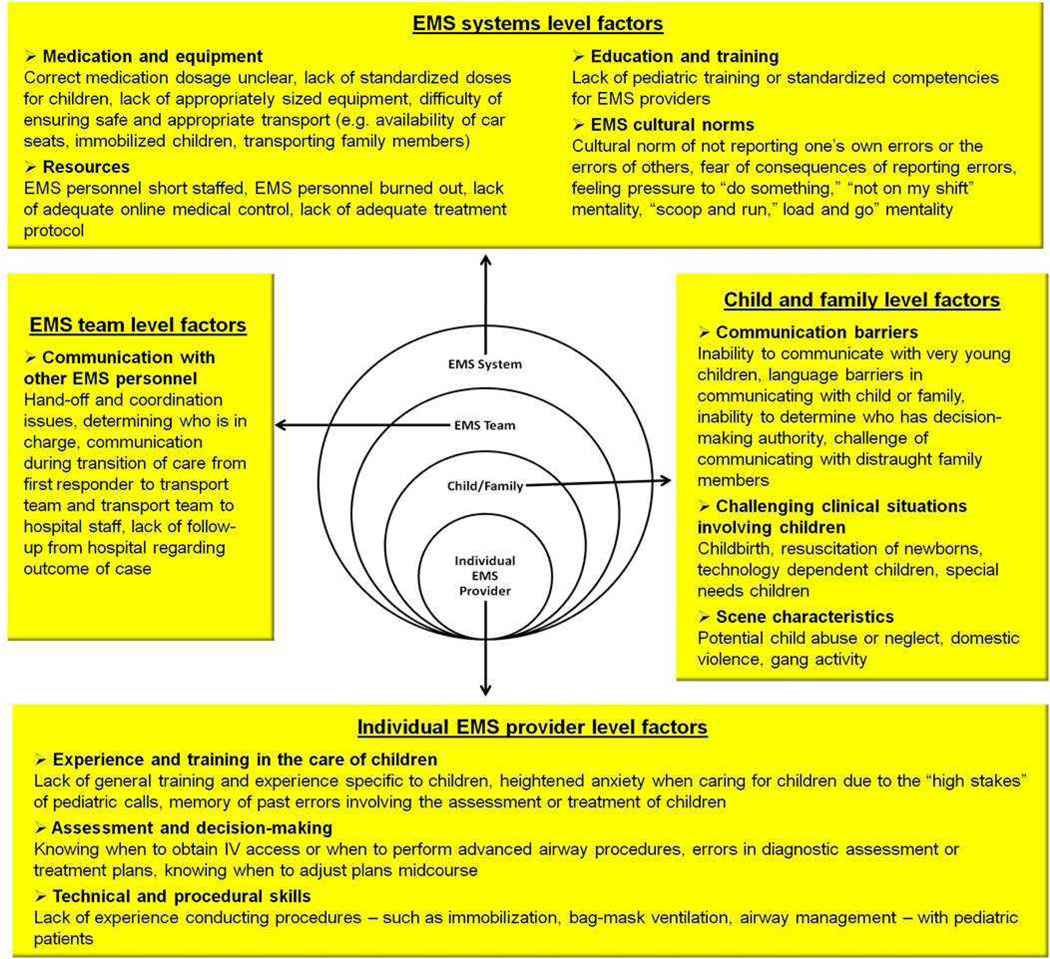
Key factors and themes identified in the analysis were grouped into categories using an ecological approach that distinguishes between systems, team, child and family, and individual provider level contributors. At the systems level, focus group participants cited challenges such as lack of appropriately sized equipment or standardized pediatric medication dosages, insufficient human resources, limited pediatric training and experience, and aspects of emergency medical services culture. EMS team level factors centered on communication with other EMS providers (both prehospital and hospital). Family and child factors included communication barriers and challenging clinical situations or scene characteristics. Finally, focus group participants highlighted a range of provider level factors including heightened levels of anxiety, insufficient experience and training with children and errors in assessment and decision-making
Conclusions
The findings of our study suggest that just as in hospital medicine, factors at the systems, team, child/family and individual provider level system contribute to errors in prehospital emergency care. These factors may be modifiable through interventions and systems improvements. Future studies are needed to ascertain the generalizability of these findings and further refine the underlying mechanisms.
Keywords: safety, emergency medicine, child health services, health services research, delivery of care
Introduction
Over a decade ago, the Institute of Medicine (IOM) report “To Err is Human” launched the patient safety movement in hospital medicine. The IOM report highlighted the importance of systems level interventions1 and ignited a field of research, development, and implementation to reduce error and improve quality and patient safety. As a result of this movement, the incidence of safety events - defined as: 1) adverse events, injuries caused by medical management rather than by the underlying condition of the patient; 2) near misses, incidents that did not result in harm to the patient, but that had the potential to do so; or 3) errors, failures of a planned action to be completed as intended or the use of a wrong plan to achieve this aim2, 3 - and their contributing factors, are now well described in the hospital setting.4–7 In contrast, there is a paucity of scientific literature exploring patient safety in emergency medical services (EMS) prior to transfer to hospital care,8–10 particular in regard to the care of pediatric patients.11
Each year, there are an average of 322.8 million visits to the emergency department (ED) in the United States. Roughly 27.7 million (or 27%) of the annual ED visits are by children under the age of 19, and about 2 million of these children reach the hospital via EMS.11 Prehospital EMS rely upon dedicated professionals who must make decisions and use complex technologies in challenging field environments, and under conditions of uncertainty considerable time pressure. In these situations, errors can occur and their consequences can be life threatening.12–17 Indeed, when surveyed about the frequency of errors over the past year, 35% of Emergency Medical Technicians (EMTs) reported making one or two errors and 9% reported making more than two errors.18, 19
Studies from the hospital setting suggest that epidemiology of adverse events in children is different than in adults20 and that when errors do occur children may be at heightened risk for adverse outcomes.21–25 Several unique aspects of pediatric care may increase the risk of safety events in the prehospital EMS setting, including: the relative infrequency of pediatric calls;26–32 the corresponding lack of experience and greater emotional anxiety of EMS providers in responding to pediatric calls;30, 32–36 communication barriers due to patient age, parental distress, and non-English language;32, 33 and the wide range of weight and size-based medication and equipment guidelines.33, 37 Moreover, compared to children who arrive at the emergency department by other means, children transported by EMS are more likely to require immediate care and more likely to be admitted to the hospital.11
A recent review of the EMS literature emphasized the need for research to improve our understanding of the magnitude and threats to patient safety.8 The majority of existing studies quantitatively examine clinical adverse events, and there is relatively little qualitative research on the contributors to safety in prehospital emergency care, or the perspectives, attitudes and behavior of EMS providers, especially in regard to the care of children.8, 11 A notable exception is a qualitative study of ambulance personnel in Western New York, which to our knowledge is the only study to explicitly explore the perceptions of and contributors to prehospital safety in the pediatric population.30, 40
The current study contributes to this gap in knowledge by building upon and further refining our understanding of the landscape of factors leading to safety events in the prehospital emergency care of children. In particular, we describe the results of focus groups conducted among EMS providers in Oregon to understand their experience providing emergency care for children and their perceptions of the range of factors that contribute to or increase the risk of pediatric safety events in the prehospital emergency setting. This exploratory study is the first phase of an NIH-funded pediatric patient safety study (NIH R01HD062478).
Methods
Study Design
This is a qualitative focus group study of EMS provider perceptions and experience of safety in the prehospital emergency care of children. Focus groups are guided discussions among a small group of participants, a format that is effective in generating group conversation around a particular topic and spurring unique insights regarding shared experiences and social norms.41–43 This method is particularly useful when the goal is to uncover underlying factors that influence behavior.43 In general, thematic saturation is reached after 4 to 6 focus groups.44 Discussion guides usually consist of 5–10 open-ended questions designed to spark conversation. Although this guide is followed for each focus group discussion, the order or wording of specific questions may vary and there is room for the conversation to move into new areas as they arise. The role of the moderator is to guide the dialogue in a way that encourages members to share their experiences and opinions openly and to ensure that all participants feel comfortable sharing their views and that no one person dominates discussion.43
Population and Setting
This study was approved by the Oregon Health & Science University institutional review board (IRB# 6942). From 2010 to 2011, EMS providers of all levels - including Basic, Intermediate, and Paramedic Emergency Medical Technicians (EMT) - were invited to participate in focus groups to discuss their experience providing EMS care to children. Participants were recruited purposively to ensure a range of perspectives, including providers from both urban/suburban and rural areas and a mix of fire, private, and volunteer providers.
Thematic saturation was reached after conducting a total of four focus groups, with between 8–12 participants each, conducted between November 2010 and March 2011. Of the 40 total participants, the mean age was 43.5 and almost 90% were male. Recruitment for two of the focus groups took place at a 2010 Mandatory EMS In-service Training, in a densely populated (>700,000) urban/suburban county of Oregon. Participants were invited during the meeting and voluntary focus groups took place immediately afterwards in a private room. We conducted separate focus groups for the fire department and private ambulance based EMS providers. In order to capture the perspectives and experience of EMS providers in more rural locations, members of the research team utilized their professional networks to facilitate two additional focus groups among volunteer and paid EMS providers from fire stations in two rural Oregon communities with service areas of less than 30,000 people. These focus groups also were voluntary and conducted in private rooms away from the primary workplace.
Data Collection
Doctoral experts in qualitative research conducted focus groups using a focus group discussion guide developed by the research team. A second team member with extensive experience in EMS attended to help facilitate discussion, and a third team member took notes. All focus groups were audio recorded and lasted 60–90 minutes. Individuals were offered a $25 gift card for their participation.
Each participant received an information sheet describing the project and the risks and benefits of participation. The facilitator obtained verbal consent to audio record the discussion, explained that to ensure confidentiality names or other personally identifying information would not be included in any published reports or papers, and advised participants that they were free not to answer questions or to withdraw from the focus group discussion at any time without penalty.
To ensure a common understanding, the facilitator presented the accepted definition of safety events cited above at the beginning of each focus group discussion (e.g. adverse events, near misses, and errors).2, 3 The focus group discussions were guided by a series of questions designed to elicit EMS providers experience with providing emergency care to children and their percecptions of the factors that contribute to safety issues. As is common in focus groups, the specific order and wording of the questions differed slightly between groups, but discussion centered around the following five questions:
-
1.
What are the most challenging calls involving children?
-
2.
Can you think about a specific example of a safety event or a near miss involving a pediatric patient?
-
4.
Are there particular situations that you think increase the risk of safety events in pediatric patients?
-
5.
What are the most important factors contributing to safety events?
-
6.
Do you feel comfortable reporting errors or near misses that you have made? How about those you have observed?
Analytic Methods
Audio recordings of the focus groups were transcribed and data were entered into NVivo9 software (QSR International, Cambridge, MA). To protect the anonymity of participants, all identifying information such as names or references to specific locations or events was removed from the transcripts. Because the field of safety science in prehospital care is still developing, our analysis was guided by principles of grounded theory, wherein an understanding of the concept of interest arises from the empirical data rather than from a priori hypotheses.45 Two investigators independently conducted a line-by-line analysis of the transcripts to identify and code themes and sub-themes. After a preliminary review of the data, the investigators developed an initial list of codes, which were modified and expanded as the analysis progressed. To ensure reliability of the coding structure, all themes and subthemes were reviewed with the larger inter-disciplinary research team – which included hospital and pre-hospital EMS providers, EMS directors, and EMS program managers. Discrepancies between coders were resolved by consensus and through discussion with the larger research team.
Results
Key factors and themes identified in the analysis were grouped into overarching categories using an ecological approach (see Figure 1), which posits that individual, familial, community, organizational, and societal level influences all contribute to the social patterning of health behavior.46, 47 For the purposes of analysis and discussion, results were categorized as EMS systems level, EMS team level, child and family level, or individual EMS provider level factors. Representative quotations from the each categories and sub-categories described below are included in Table 1.
Figure 1.
An ecological framework for understanding factors contributing to safety events in the prehospital emergency care of children
Table 1.
Emergency medical services provider perspectives on the contributors to safety events in prehospital emergency care of children
| EMS System Level Factors | |
|---|---|
| Medication and equipment | “I see medication errors as the number one…and we got a big issue…of not knowing…or not guessing right exactly how much medicine you should be giving a patient…” “Medication calculation can be a point of…potential error…I think we’ve worked to mitigate that with cheat sheets and, you know, the new pediatric book, but still, I mean, there’s the element of not doing something correctly or if you don’t have something readily available on a cheat sheet like how-, how practiced you are, how well trained you are so to speak.” “…just because it’s a pediatric electrode, or pulse oximetry, doesn’t mean it works from a newborn to 12 years old.” |
| Resources | “you need to have enough qualified people there, rapidly” “…the biggest things I see documented around here from my perspective isn’t so much a near miss than it is…it’s manpower. My medics are gone. It’s me and maybe a student, and in this case, I’m fortunate to have a student.” “when you look at the map…most of the docs in Oregon, they’re in the Portland area, which is…nice but not helpful for the guys that are out here…and you have…very long transport times. And the people there can be just as injured…” “I think that’s part of the problem that we have is that…’Well…which hospital do I send him to?’ You know the amount of expertise that the other smaller hospitals…I’m gonna overwhelm their system right away, you know, with one child that his this…bad injury. And is there a person available at this institution that’s gonna be able to manage this injury?” |
| Education and training | “the bulk of the training that I’ve been through… is either the…non-emergency kid or it is the dead kid that we’re resuscitating. The stuff that’s in between those two isn’t really dealt with all that much…” “…personally, that’s what I would sort of focus on is…how do we get more training for these guys…whether it’s simulations, whether it’s videos, you know sick/not sick…Whatever you can to sort of expose these people, for the more you expose them the better they will be able to handle it.” “…my think with the EMS has always been…what we do is a hundred percent dependent on our physician advisor…and there’s no national standard.” |
| EMS cultural norms | “I think that historically…we’ve all tried to protect each other.” “You’ve lost the ability to sit down with someone and go, ‘You know what? You’re a really good person, but this just isn’t the career for you’ or ‘You’re just not cut out for it’…I mean, I’ve worked with people that…did great on the tests but they shake and shiver and their palms sweat and you know, their mouth gets dry and they can’t think…” “…you have to hurry to get this person to where they need to be and beat the clock, but I think more training of how to slow people down and do things more efficiently…would save a lot of the near misses…” |
| EMS Team Level Factors | |
| Communication with other EMS providers | “…a true safety issue is the ability or inability to communicate. That great familiarity amongst crews that are gonna be working together…increases the safety factor.” “I’m not suggesting anybody is slacking. I think just that we all have these very highly computerized systems…that don’t communicate. There is no piece of paper…that says 'I gave him valium'…so that when I get to the patient I get the entire [report of] what’s been done to this patient and this is what I’m interested in.” “‥there may be absolutely no communication between a paramedic and physician for an individual patient.” “…a lot of paramedics will call in for advice on the medical control. And that happens, usually when they recognize they’re in trouble. But they don’t call if they don’t recognize they’re in trouble.” |
| Child and Family Level Factors | |
| Communication barriers | “…sometimes…you’ve got to get mom out of the situation, but yet you need them there to help you communicate with the child…so you have to understand how…to de-escalate her. Bring her back into the scene as somebody who can help you….” “…there’s nothing’ more frustrating, going on an ill kid…and there’s no one there that speaks English.” “I think one of our biggest safety problems with kids is that we cannot always accurately assess them…They can’t tell us what’s wrong because they can’t speak…or sometimes they just don’t know how to tell us. They don’t have the language or the words. And then you rely on the parents to tell you what they saw, and they’re frequently completely inaccurate, or they…didn’t see it and they’re making it up based on their assumptions.” “Well, those safety issues, for me, children in the custody of people that aren’t relatives…You know, so we spend a whole bunch of time trying to get in touch with the parent.” |
| Challenging clinical situations or scene characteristics | “Home birth…with a doula or midwife on the scene. They don’t call until things have gotten so far downhill…” “…we’re seeing a lot more of these kids that, quite honestly, probably should still be in the hospital and not be sent home…they’re super sick. They have basically the equivalent o an ICU in their room at home and then if something happens, we get called and we see equipment we’ve never seen before, or maybe seen once or twice.” “One of the most challenging calls is…a child at a babysitters. Because…there’s the fear of…legal ramifications, and so they kind of fudge what they were doing…and they’re more concerned about being blamed for what happened, as opposed to helping you figure out what is going on with this child…” “…and sometimes you have to make decisions based on what your being told…and we were told that the bruises on the chest were from dad giving CPR because he didn’t know how. Well, you know, the bruises were obviously old.” |
| Individual EMS Provider Level Factors | |
| Experience and training in the care of children | “…every time a call comes in for a [pediatric] call, no matter what it is, it kind of raises the hair on my neck, just because I don’t have the experience, nor the confidence in treating kids.” “Me, with a child, I would be extremely nervous because I’ve never really dealt with children other than just playin’ at the playground, you know…” “Kids are so scary. I mean, if you screw it up… you can’t imagine the repercussions.” “…unless you’re a career guy, you know, or on an ambulance, you don’t run a ton of pediatric calls. And when you do…it’s really intimidating.” “Every year [we seem to] get this whole new rash of brand new paramedics who went straight from basic education to paramedic education, so when they come out their experience level is minimal…They’re young and they don’t have the experience of even being a parent, so they don’t have those experiences of what normal children are like. And then because they are so new, they don’t have the experience to really base on how sick this child is, or…exactly what path they need to go down…” |
| Assessment and decision-making | “…everything in harder in kids. Your brain can’t dislodge from this. I have to get an IV. And so you can’t move on to the next thing because you’re still focused on this. And so that’s part of the problem I find with kids.” “There are so many gray area decisions to make with pediatric patients… which just makes it so stressful for the responders…and they’ve gotta go back to their experience, and if they don’t have it, wow.” “…because things are so difficult in kids sometimes, we have to train our guys to sort of think outside of the box and not just focus on what we can’t do.” “My guess would be that most errors come from acts of commission rather than omission. So paramedics wanting to do something whether they’re indicated or not…” “I had a 12-year-old code here several months ago. The decision, or the question was, is this an adult or pediatric patient and how are we going to treat it?…and it is hard to say OK, and they’re 13 years old, they’re an adult…there’s not even any guidelines in there. You know, these decision guidelines.” |
| Technical and procedural skills | “More predominantly it is a fear to-, to provide an advanced procedure…” “I think the biggest problem [with airway management intubation issues]…is it’s very difficult for paramedics to get any training from the pediatric population. Pediatric anesthesiologists don’t like inexperienced people touching their children…so, you know, there is a good possibility that there are paramedics out there who have never intubated a kind…but they’re given the tools…” “The problem with kids is everything is harder…[even] simple as IV access. Getting blood from a-, I mean these are simple things that we’d normally do with all of our patients [that] gives us a lot of information and yet we can’t get this stuff.” |
EMS system-level factors
Medication and equipment
Participants described a variety of issues related to pediatric medications and equipment that can contribute to safety events. In particular, weight-based pediatric dosing can be particularly challenging in the prehospital environment. Providers are encouraged to consult a manual or other resource to determine the correct medication dosage, but the utility of these guides are questionable. Moreover, it is often difficult to estimate patient weight, particularly when under pressure in an emergency situation. The lack of standardized medication packaging or changes to packaging, concentrations, etc. further increases the risk of medication and dosing errors. Participants suggested that standardization through regulation at the national level may be beneficial.
A general frustration with the “inadequacy of size-based equipment” was noted repeatedly as well as concern about the difficulty of ensuring safe and appropriate transport for children. Participants explained that the need to adapt adult-sized equipment for use in children can lead to errors and that the dramatic variability in both age and size of pediatric patients contributes to this problem.
Resources
Some participants described limited human resources as a key contributor to safety events, especially for rural agencies that rely on volunteers who may not always have pediatric training. The geographic distance to tertiary pediatric centers, and the need to transport unstable patients by air or ground, were cited as additional challenges.
Education and training
Overall, participants felt that availability of universal education and ongoing training for pediatric emergencies was inadequate. EMT’s receive insufficient pediatric training and experience initially, and if required locally to have pediatric training or certification they commented that this ongoing training was not pertinent to the prehospital role and/or issues they face providing pediatric care. Respondents described locally provided hands-on and simulation-based training as the most effective.
EMS cultural norms
Many of the focus group participants mentioned the cultural norm of not reporting their own errors or the errors of team members and the fear of consequences if an error is reported. Error reporting is almost never documented in a patient care record and most often “handled” internally by the ambulance crew or a supervisor. If documentation is required it is rarely disclosed directly to patients, families, or receiving providers. Another cultural norm mentioned repeatedly as a potential contributor to safety was the pressure to “scoop-and-run” or “do something” quickly as opposed to “stay and play” or stabilize before transport.
EMS team-level factors
Communication with other EMS providers
Participants highlighted communication among team members as an area where errors can occur. Many cited command and control issues, such as clearly identifying the paramedic-in-charge or disagreements between same-level providers. In some cases, a breakdown in communication results in a “failure to actually do something.” Moreover, difficulties in operational communications, including accessing online medical control, radio communications to other responders, and communication between police, fire, and EMS can also be challenging.
Communication issues can also arise during transitions of care; for example, from first responder to transport team or transport team to hospital staff. Participants talked about not always knowing what had happened before they arrived on the scene and not having a good way to report their actions to others. EMS providers noted that there is rarely any follow-up from the hospital regarding the outcome of a particular case. The absence of follow-up inhibits practice based learning and improvement.
Child- and family-level factors
Communication barriers
In all focus groups, participants emphasized the potential challenges of communicating with the child and family members. EMS providers sometimes find it difficult to determine who has decision-making authority in situations of joint custody or in settings where parents are not physically present, or when a child is at school or childcare centers. It is also a challenge to assess very young children who may not be able to talk or have the capacity to describe their symptoms and providers frequently need to rely on family members or guardians to communicate with the child. In addition to assessing and taking care of the needs of the child, a number of participants emphasized the additional task of managing the parent, whom one participant described as “patient number two.” It often takes an additional dedicated EMS provider just to communicate with and reassure and distraught family members.
Challenging clinical situations or scene characteristics
When asked if there are clinical situations which heighten the risk of safety events, participants pointed to childbirth, resuscitation of newborns, and special needs children including children who are dependent on medical equipment. Participants also highlighted several scene characteristics that increase the chance of safety events, including scenes involving potential child abuse or neglect, domestic violence, and gang activity.
Individual EMS provider-level factors
Experience and training in the care of children
At the individual level, almost all focus group participants emphasized the heightened level of anxiety when caring for children and that pediatric calls are “very high risk, very low frequency.” Some stated that they had little experience working with children, and described a different sense of urgency and accountability when responding to pediatric calls. “Everything is harder. Period. History’s harder, physical exam is harder. Treatments are harder. IV access is harder. Everything is harder.” Moreover, EMS providers highlighted the sheer complexity of responding to pediatric calls. When responders don’t have experience to fall back on, the complexity and high levels of anxiety associated with pediatric calls can increase the risk of a safety event.
Assessment and decision-making
Participants articulated the fact that the anxiety and lack of experience in treating children can also affect decision-making. Moreover, even when EMS providers do have experience to draw upon, the stress of responding to pediatric calls can affect the decision-making process. Examples of decision points that are especially critical include: knowing when to obtain IV access and when to perform advanced airway procedures, establishing a diagnosis and treatment plan, and knowing when to adjust plans midcourse.
Technical and procedural skills
Focus group participants also pointed to technical and procedural skills, especially the lack of experience conducting procedures with pediatric patients, as risk factors for safety events. Procedures such as immobilization, bag-mask ventilation, and airway management were noted as particular challenges. Lack of technical skill coupled with the stress of pediatric calls may contribute to procedural errors as well as a complete failure to perform required procedures.
Discussion
Improving patient care requires an understanding of the factors that predispose to error. We drew upon the ecological approach46, 47 to portray the nested and inter-related factors involved in children’s prehospital care at the level of the EMS system, EMS team, child and family, and individual EMS provider. This multilayered complexity is similarly reflected in Reason’s Swiss cheese model of patient safety, which embeds individual behavior in the context of the overall system.48 Focus group participants identified several prominent system level contributors to safety including insufficient pediatric training and experience, lack of standardization or difficulty calculating medication dosages, and equipment that was inappropriately sized for children. Team level factors centered on challenges in communication, especially during transitions of care. Child and family level factors included language and communication barriers, difficult family dynamics, and determining who has decision making authority. Finally, at the individual level, EMS providers reported heightened levels of anxiety when responding to calls involving children and a lack of experience and training specific to children, which compounds the risk of error in high stakes emergency situations.
Our findings support and build on many of the contributors to safety events identified in prior research, including the relative infrequency of pediatric calls,26–32 lower levels of comfort and training specific to children, 30, 32–36 communication barriers,32, 33 an EMS culture that doesn’t encourage the reporting of errors; 30, 40, 18, 19 and the range of weight and size-based medication and equipment guidelines specific to children.33, 37 Of particular relevance, several of the themes we identified resonate with the findings of a qualitative study of ambulance personnel perceptions of near misses and adverse events among volunteer and career EMS personnel in Western New York.30 In both studies, EMS providers expressed significant discomfort with pediatric patients and a desire for additional training and clinical experience in pediatrics. Indeed, the need for additional pediatric training is a strong theme across a range of studies in the existing literature,35, 49, 50 including a recent Institute of Medicine report on children’s emergency care.51 Our study further validates previous findings and provides additional details regarding the importance of improving pediatric training for prehospital emergency providers.
Focus group participants also highlighted the challenge of meeting the needs of the range of sizes and ages of pediatric patients, which is compounded by a lack of appropriate equipment or standardized medication dosages, a challenge highlighted in other studies in the pediatric EMS literature.30, 37, 52 For example, in simulated pediatric emergencies, appropriate organization and use of pediatric equipment and calculating and administering accurate drug doses was pinpointed as a root cause of errors.37 Moreover, a study of medication dosing errors among children under 12 across eight Michigan EMS agencies, identified inaccurate weight-based medication dosages in about 1/3 of cases.52 Indeed, improving the standardization of medication dosages and/or developing methods to facilitate calculations in emergency settings for a range of heights and weights has been called out as an important area of future research.40 Reports from pediatric care in the hospital setting identify medication errors as a prominent cause of adverse events among children, 20, 53, 54 further supporting the need for additional research and the development of interventions to improve this area of children’s prehospital care.
Finally, our findings echo previous evidence of an EMS culture that is not conducive to reporting errors. 18, 19, 30, 40This is a major barrier to understanding and improving safety in prehospital emergency care. Focus group participants repeatedly emphasized that reporting one’s own errors or the errors of others is not a routine practice, and in some cases is even actively discouraged. They also noted the lack of follow up or debriefing between hospital and prehospital providers, which limits learning from past mistakes and opportunities to develop strategies to prevent errors and improve safety.
This exploratory study was the first phase of a larger project to identify the contributors to safety in the prehospital emergency care of children. Although by design focus group methodology is limited by a small sample size and geographic area, the themes and richness of stories provide valuable information to understand the nature of pediatric medical errors. A key limitation of our findings is the inability to delineate results according to level of EMS training (i.e. EMT-Basic, Intermediate, or Paramedic). However, the overall themes provide a broad foundation to inform future research. With this broad foundation, we next plan to expand the external validity of our investigation through a national Delphi survey of EMS providers - that includes detailed information on a range of provider characteristics including level of training, years of experience, and geographic location - and further refine the underlying contributors to safety event through chart review and in situ simulations of children’s emergencies.
Conclusion
For over a decade, the field of medicine has recognized the importance of studying and designing strategies to prevent safety issues in hospitals and clinics. The findings of our study suggest that just as in hospital medicine, factors at the systems, team, child/family and individual provider level system contribute to errors in prehospital emergency care. Within these categories, focus group participants highlighted a range of potential contributors including: insufficient pediatric training, the wide variation in equipment and medication dosages, communication among team members, communication the child and family, and an overall lack of experience with children coupled with heightened anxiety when responding to calls involving children. Many of these factors may be modifiable through interventions and systems improvements. Future studies are needed to ascertain the generalizability of these findings and further refine the underlying mechanisms.
Acknowledgements
Funding Source:
All phases of this study were supported by an NIH grant, R01HD062478.
Footnotes
Financial Disclosure:
The authors have no financial relationships relevant to this article to disclose.
Declaration of Interest:
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Author Contributions:
Erika Cottrell: Dr. Cottrell facilitated focus groups, analyzed and interpreted the data, drafted the initial manuscript, and approved the final manuscript as submitted.
Kerth O’Brien: Dr. O’Brien contributed to the design of the focus group discussion guide, facilitated focus groups, interpreted the data, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Merlin Curry: Mr. Curry assisted with recruitment for and facilitation of focus groups, interpreted the data, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Garth Meckler: Dr. Meckler participated in the conceptualization and design of the study, assisted with recruitment for and facilitation of focus groups, interpreted the data, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Philip Engle: Mr. Engle assisted with facilitation of focus groups, interpreted the data, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Jon Jui: Dr. Jui participated in the conceptualization and design of the study, assisted with recruitment for the focus groups, analyzed the data, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Caitlin Summers: Ms. Summers analyzed and interpreted the data, reviewed and revised the manuscript, and approved the final manuscript as submitted.
William Lambert: Dr. Lambert participated in the conceptualization and design of the study, facilitated focus groups, interpreted the data, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Jeanne-Marie Guise: Dr. Guise conceptualized and designed the study, facilitated focus groups, analyzed and interpreted the data, reviewed and revised the manuscript, and approved the final manuscript as submitted.
References
- 1.Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 2.Reason J. Human error. Cambridge England: Cambridge University Press; 1990. [Google Scholar]
- 3.Brennan TA, Leape LL. Adverse events, negligence in hospitalized patients: results from the Harvard Medical Practice Study. Perspect Healthc Risk Manage. 1991 Spring;11(2):2–8. doi: 10.1002/jhrm.5600110202. [DOI] [PubMed] [Google Scholar]
- 4.Leape LL, Berwick DM. Five years after To Err is Human: what have we learned? JAMA. 2005;293:2384–2390. doi: 10.1001/jama.293.19.2384. [DOI] [PubMed] [Google Scholar]
- 5.Morey JC, Simon R, Jay GD, et al. Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health Serv Res. 2002;37:1553–1581. doi: 10.1111/1475-6773.01104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schenkel SM, Khare RK, Rosenthal MM, Sutcliffe KM, Lewton EL. Resident perceptions of medical errors in the emergency department. Acad Emerg Med. 2003;10:1318–1324. doi: 10.1111/j.1553-2712.2003.tb00004.x. [DOI] [PubMed] [Google Scholar]
- 7.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care unit. N Engl J Med. 2004;351:1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 8.Bigham BL, Buick JE, Brooks SC, Morrison M, Shojania KG, Morrison LJ. Patient safety in emergency medical services: a systematic review of the literature. Prehosp Emerg Care. 2012 Jan;16(1):20–35. doi: 10.3109/10903127.2011.621045. [DOI] [PubMed] [Google Scholar]
- 9.Burt CW, McCaig LF, Valverde RH. Analysis of ambulance transports and diversions among US emergency departments. Ann Emerg Med. 2006 Apr;47(4):317–326. doi: 10.1016/j.annemergmed.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 10.Institute of Medicine. Emergency Medical Services: At the Crossroads. Washington, DC: 2006. Jun, [Google Scholar]
- 11.Shah MN, Cushman JT, Davis CO, Bazarian JJ, Auinger P, Friedman B. The epidemiology of emergency medical services use by children: an analysis of the National Hospital Ambulatory Medical Care Survey. Prehosp Emerg Care. 2008;12(3):269–276. doi: 10.1080/10903120802100167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang HE, Lave JR, Sirio CA, Yealy DM. Paramedical intubation errors: isolated events or symptoms of larger problems? Health Aff (Millwood) 2006;25:501–509. doi: 10.1377/hlthaff.25.2.501. [DOI] [PubMed] [Google Scholar]
- 13.Fairbanks RJ, Caplan SH, Bishop PA, Marks AM, Shah MN. Usability study of two common defibrillators reveal hazards. Ann Emerg Med. 2007;50:424–432. doi: 10.1016/j.annemergmed.2007.03.029. [DOI] [PubMed] [Google Scholar]
- 14.Vilke GM, Tornabene SV, Stepanski B, et al. Paramedic self-reported medication errors. Prehosp Emerg Care. 2006;10:457–462. doi: 10.1080/10903120600885100. [DOI] [PubMed] [Google Scholar]
- 15.Kothari R, Barsan W, Brott T, Broderick J, Ashbrock S. Frequency and accuracy of preshospital diagnosis of acute stroke. Stroke. 1995;26:937–941. doi: 10.1161/01.str.26.6.937. [DOI] [PubMed] [Google Scholar]
- 16.Hubble MW, Paschal KR, Sanders TA. Medication calculation skills of practicing paramedics. Prehosp Emerg Care. 2000;4:253–260. doi: 10.1080/10903120090941290. [DOI] [PubMed] [Google Scholar]
- 17.Rittenberger JC, Beck PW, Paris PM. Errors of omission in the treatment of prehospital chest pain patients. Prehosp Emerg Care. 2005;9:2–7. doi: 10.1080/10903120590891688. [DOI] [PubMed] [Google Scholar]
- 18.Hobgood C, Xie J, Weiner B, Hooker J. Error identification, disclosure, and reporting: practice patterns of three emergency medicine provider types. Acad Emerg Med. 2004;11:196–199. [PubMed] [Google Scholar]
- 19.Hobgood C, Bowen JB, Brice JH, Overby B, Tamayo-Sarver JH. Do EMS personnel identify, report, and disclose medical errors? Prehosp Emerg Care. 2006;10:21–27. doi: 10.1080/10903120500366011. [DOI] [PubMed] [Google Scholar]
- 20.Woods D, Thomas E, Holl J, Altman S, Brennan T. Adverse events and preventable adverse events in children. Pediatrics. 2005;115:155–160. doi: 10.1542/peds.2004-0410. [DOI] [PubMed] [Google Scholar]
- 21.Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285:2114–2120. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- 22.Fox G. Minimizing prescribing errors in infants and children. Am FamPhysician. 1996;54:1319–1325. [PubMed] [Google Scholar]
- 23.Koren G, Haslam RH. Pediatric medication errors: predicting and preventing tenfold disasters. J Clin Pharmacol. 1994;34:1043–1045. doi: 10.1002/j.1552-4604.1994.tb01978.x. [DOI] [PubMed] [Google Scholar]
- 24.Miller MR, Elixhauser A, Zhan C. Patient safety events during pediatric hospitalization. Pediatrics. 2003;11:1358–1366. doi: 10.1542/peds.111.6.1358. [DOI] [PubMed] [Google Scholar]
- 25.Slonim AD, LaFleur BJ, Ahmed W, Joseph JG. Hospital-reported medical errors in children. Pediatrics. 2003;111:617–621. doi: 10.1542/peds.111.3.617. [DOI] [PubMed] [Google Scholar]
- 26.Seidel JS, Hornbein M, Yoshiyama K, Kuznets D, Finklestein JZ, St Geme JW., Jr Emergency medical services and the pediatric patient: are the needs being met? Pediatrics. 1984 Jun;73(6):769–772. [PubMed] [Google Scholar]
- 27.Seidel JS, Henderson DP, Ward P, Wayland BW, Ness B. Pediatric prehospital care in urban and rural areas. Pediatrics. 1991 Oct;88(4):681–690. [PubMed] [Google Scholar]
- 28.Knapp JF. A call to action: the Institute of Medicine report on emergency medical services for children. Pediatrics. 1995 Jul;96(1 Pt 2):173–174. [PubMed] [Google Scholar]
- 29.Kumar VR, Bachman DT, Kiskaddon RT. Children and adults in cardiopulmonary arrest: are advanced life support guidelines followed in the prehospital setting? Ann Emerg Med. 1997 Jun;29(6):743–747. doi: 10.1016/s0196-0644(97)70195-1. [DOI] [PubMed] [Google Scholar]
- 30.Cushman JT, Fairbanks RJ, O’Gara KG, et al. Ambulance personnel perceptions of near misses and adverse events in pediatric patients. Prehosp Emerg Care. 2010 Oct-Dec;14(4):477–484. doi: 10.3109/10903127.2010.497901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lammers RL, Byrwa MJ, Fales WD, Hale RA. Simulation-based assessment of paramedic pediatric resuscitation skills. Prehosp Emerg Care. 2009 Jul-Sep;13(3):345–356. doi: 10.1080/10903120802706161. [DOI] [PubMed] [Google Scholar]
- 32.Fleischman RJ, Yarris LM, Curry MT, Yuen SC, Breon AR, Meckler GD. Pediatric educational needs assessment for urban and rural emergency medical technicians. Pediatr Emerg Care. 2011 Dec;27(12):1130–1135. doi: 10.1097/PEC.0b013e31823a3e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Breon AR, Yarris LM, Law J, Meckler GD. Determining the paediatric educational needs of prehospital providers: part 1. Journal of Paramedic Practice. 2011;3(8):7. [Google Scholar]
- 34.Roach CL, Medina FA. Paramedic comfort level with children in medical and trauma emergencies: does the PALS course make a difference? Am J Emerg Med. 1994 Mar;12(2):260–262. doi: 10.1016/0735-6757(94)90263-1. [DOI] [PubMed] [Google Scholar]
- 35.Glaeser PW, Linzer J, Tunik MG, Henderson DP, Ball J. Survey of nationally registered emergency medical services providers: pediatric education. Ann Emerg Med. 2000 Jul;36(1):33–38. doi: 10.1067/mem.2000.107662. [DOI] [PubMed] [Google Scholar]
- 36.Spaite DW, Conroy C, Karriker KJ, Seng M, Battaglia N. Improving emergency medical services for children with special health care needs: does training make a difference? Am J Emerg Med. 2001 Oct;19(6):474–478. doi: 10.1053/ajem.2001.27146. [DOI] [PubMed] [Google Scholar]
- 37.Lammers R, Byrwa M, Fales W. Root causes of errors in a simulated prehospital pediatric emergency. Acad Emerg Med. 2012 Jan;19(1):37–47. doi: 10.1111/j.1553-2712.2011.01252.x. [DOI] [PubMed] [Google Scholar]
- 38.Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcomes: a controlled clinical trial. JAMA. 2000;283:783–790. doi: 10.1001/jama.283.6.783. [DOI] [PubMed] [Google Scholar]
- 39.Jemmet ME, Kendal KM, Fourre MW, Burton JH. Unrecognized misplacement of endotracheal tubles in a mixed urban to rural emergency medical services setting. Acad Emerg Med. 2003;10:961–965. doi: 10.1111/j.1553-2712.2003.tb00652.x. [DOI] [PubMed] [Google Scholar]
- 40.Fairbanks RJ, Crittendon CN, O’Gara KG, et al. EMS provider perceptions of the nature of adverse events and near misses in out-of-hospital care: an ethnographic view. Acad Emerg Med. 2003;10:961–965. doi: 10.1111/j.1553-2712.2008.00147.x. [DOI] [PubMed] [Google Scholar]
- 41.Strauss A, Corbin J. Basics of Qualitative Research: Techniques and procedures for developing grounded theory. Newbury Park, Calif: Sage; 1998. [Google Scholar]
- 42.Kruger R, Casey M. Focus groups. 3rd edition. Thousand Oaks, Calif: Sage; 2000. [Google Scholar]
- 43.Curry LA, Nembhard IM, Bradley EH. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009;119:1442–1452. doi: 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- 44.Morgan DL. Foucs groups. Annu Rev Sociol. 1996;22:129–152. [Google Scholar]
- 45.Corbin J, Strauss A. Grounded Theory Research: Procedures, Canons, and Evaluative Criteria. Qualitative Sociology. 1990;13(1):19. [Google Scholar]
- 46.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006 Apr;62(7):1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 47.Bronfenbrenner U. Ecological Models of Human Development. In: Gauvain M, Cole M, editors. Readings on the Development of Children. Fourth Edition. New York, NY: Worth Publishers; 1997. [Google Scholar]
- 48.Reason J. Human error: models and management. BMJ. 2000;320:768–770. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Su E, Schmidt TA, Mann NC, Zechnich AD. A randomized controlled trial to assess decay in acquired knowledge among paramedics completing a pediatric resuscitation course. Acad Emerg Med. 2000;7:779–786. doi: 10.1111/j.1553-2712.2000.tb02270.x. [DOI] [PubMed] [Google Scholar]
- 50.Youngquist ST, Hendreson DP, Gausche-Hill M, Goodrich SM, Poore PD, Lewis RJ. Paramedic selfefficacy and skill retenion in pediatric airway managemetn. Acad Emerg Med. 2008;15:1295–1303. doi: 10.1111/j.1553-2712.2008.00262.x. [DOI] [PubMed] [Google Scholar]
- 51.IOM. Future of Emergency Care Series Emergency Care for Children Growing Pains. Washginton, DC: Institute of Medicine the National Academics; 2006. [Google Scholar]
- 52.Hoyle JD, Davis AT, Putman KK, Trytko JA, Fales WD. Medication dosing errors in pediatric patients treated by emergency medical services. Prehosp Emergency Care. 2012;16:59–66. doi: 10.3109/10903127.2011.614043. [DOI] [PubMed] [Google Scholar]
- 53.Hicks RW, Becker SC, Cousins DD. Harmful medication errors in children: a 5-year analysis of data from the USP’s MED-MARX program. J Pediatr Nurs. 2006;22:39–51. doi: 10.1016/j.pedn.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 54.Fortescue EB, Kaushal R, Landrigan CP, et al. Prioritizing strategies for preventing medication errors and adverse drug events in pediatric inpatients. Pediatrics. 2003 Apr;111(4 Pt 1):722–729. doi: 10.1542/peds.111.4.722. [DOI] [PubMed] [Google Scholar]