Abstract
Objectives
To assess the feasibility and safety of transulnar approach whenever transradial access fails.
Background
Radial access for coronary procedures has gained sound recognition. However, the method is not always successful.
Methods
Between January 2010 and June 2013, diagnostic with or without percutaneous coronary intervention (PCI) was attempted in 2804 patients via the radial approach. Transradial approach was unsuccessful in 173 patients (6.2%) requiring crossover to either femoral (128 patients, 4.6%) or ulnar approach (45 patients, 1.6%). Patients who had undergone ulnar approach constituted our study population. Selective forearm angiography was performed after ulnar sheath placement. We documented procedural characteristics and major adverse cardio-cerebrovascular events.
Results
Radial artery spasm was the most common cause of crossover to the ulnar approach (64.4%) followed by failure to puncture the radial artery (33.4%). Out of 45 patients (82.2%), 37 underwent successful ulnar approach. The eight failed cases (17.8%) were mainly due to absent or weak ulnar pulse (75%). PCI was performed in 17 cases (37.8%), of which 8 patients underwent emergency interventions. Complications included transient numbness, non-significant hematoma, ulnar artery perforation, and minor stroke in 15.5%, 13.3%, 2.2% and 2.2%, respectively. No major cardiac-cerebrovascular events or hand ischemia were noted.
Conclusion
Ulnar approach for coronary diagnostic or intervention procedures is a feasible alternative whenever radial route fails. It circumvents crossover to the femoral approach. Our study confirms satisfactory success rate of ulnar access in the presence of adequate ulnar pulse intensity and within acceptable rates of complications.
Keywords: Coronary procedures, Ulnar, Radial, Femoral approach, Alternative, Feasible, MACCE
List of abbreviations
- ACS/NSTEMI
Acute Coronary Syndrome/Non ST segment Elevation Myocardial Infarction
- ACC/ AHA
American College of Cardiology/American Heart Association
- DAP
Dose Area Product
- ECG
Electrocardiography
- MACCE
Major Adverse Cardio-Cerebrovascular Events
- PCI
Percutaneous Coronary Intervention
- STEMI
ST segment Elevation Myocardial Infarction
- TIG catheter
Tiger catheter
Introduction
Transradial artery approach for coronary intervention has gained solid recognition as an alternative to the standard transfemoral artery approach. It is associated with significantly lower rates of local vascular complications, shorter hospital stay and greater comfort to the patients due to early mobilization [1–3]. However, access to the radial artery is not always successful, with reported crossover rates to other routes between 3% and 8% [4]. Failure to get radial access is mainly attributed to difficulty in puncturing the artery – chiefly due to arterial spasm and infrequently to presence of a radial loop – hypoplasia, or occlusion of the radial artery [5,6]. Transfemoral artery approach may result in major life or limb-threatening complications, and remains the leading cause of morbidity after cardiac catheterization [7]. Since the first description by Terashima et al. [8], the ulnar artery has become the alternative approach when the radial artery cannot be accessed or used [9,10]. The aim of this study is to assess whether the transulnar approach is a feasible and safe alternative whenever transradial approach fails.
Patients and methods
A prospective non-randomized study was carried out between January 2010 and June 2013. During that time, we performed 2804 diagnostic coronary angiographies with and without percutaneous coronary intervention (PCI) either via a right or left transradial approach. Transradial approach was unsuccessful in 173 patients (6.2%) necessitating crossover to either transfemoral approach (128 patients, 4.6%) or transulnar approach (45 patients, 1.6%). Our study population constituted transulnar approach patients. Selective forearm angiography was performed after ulnar sheath insertion in most of the patients. We documented procedural characteristics and major adverse cardio-cerebrovascular events. Informed consent was obtained from all patients, and we received the approval of our local ethical committee. Patients were prepared according to the American College of Cardiology/American Heart Association (ACC/AHA) task force on Cardiac Catheterization Laboratory Standards [11]. Routine laboratory investigations including urea and electrolytes, full blood counts, liver and renal function tests and coagulation profile were performed. The technique of radial and ulnar artery cannulation has been documented [12].
Diagnostic angiography of transradial and transulnar approaches were performed with a dedicated 6 French Cook radial sheath (micro-puncture radial artery access, William Cook Europe, Bjaeverskov, Denmark); a 5 French diagnostic TIG catheter (Terumo Corporation, Tokyo, Japan) for both left and right coronaries; and a 5 French pigtail catheter in case left ventriculography, aortography and/or non-selective renal angiography were required. We used various 6 French guiding catheters as Extra Backup, Judkins or Amplatz in case of intervention. A mixture of 100 μg glyceryl trinitrate and 2.5 ml verapamil was injected after sheath insertion followed by 5000 international units of unfractionated heparin through the sheath. One-milligram midazolam and 25 μg of fentanyl were given intravenously as per operator discretion depending on patient’s clinical situation. The ulnar artery sheath was immediately removed at completion of the diagnostic and/or interventional procedure. Hemostasis was obtained by local compression using a tight pressure bandage for four hours. Patients were allowed to ambulate immediately unless their clinical status dictated otherwise. Only patients who experienced local vascular complications were subjected to Doppler ultrasound assessment for extravasation or deep hematoma. All patients were discharged four hours post diagnostic procedures, provided there were no symptoms or signs of hand and/or coronary ischemia, and that patients were clinically and hemodynamically stable. Most patients who underwent PCI were kept overnight for observation.
Inclusion criteria
We included all patients aged >18 years who were admitted for coronary angiography with or without intervention whose transradial approach was unsuccessful, and whose operator had chosen to cross over to transulnar approach.
Exclusion criteria
We excluded all patients who refused to participate in this study, as well as patients with planned elective femoral approach, and patients presenting with cardiogenic shock and/or hemodynamic instability. Additionally, patients with significant brachial, axillary or subclavian tortuosity were excluded as gaining ulnar access would not have resolved these problems.
Study outcomes
Primary outcomes
-
1.
Procedural success was where vascular access and completion of the procedure (either diagnostic and or intervention) were performed from ulnar approach without crossing over to other routes.
-
2.
Procedural complications were defined as local vascular complications and major adverse cardiac-cerebrovascular events (MACCE) immediately following the procedure and before discharge. Local vascular complications included major bleeding, minor bleeding or hematoma. Minor bleeding was defined as any ecchymosis or fresh bleeding from access site without the need for blood transfusion or prolonged hospitalization. Major bleeding was defined as any bleeding from access site requiring blood transfusion and/or prolonged hospitalization [13].
MACCE included acute non-fatal myocardial infarction, major cerebrovascular stroke, acute heart failure or death. Cerebrovascular stroke was classified into minor and major. Minor cerebrovascular accident is any new post procedure motor disability that improves within one week. Major cerebrovascular accident is any new post procedure motor disability that continues beyond one week. Procedural myocardial infarction was defined as documented chest pain, ECG changes and troponin elevation following the procedure [13].
Secondary procedural outcomes
-
1.
Procedural time (in minutes) is defined as total duration of the procedure starting from obtaining vascular access to performing the procedure and ending with sheath removal.
-
2.
Fluoroscopy time (in minutes).
-
3.
Radiation dose expressed as dose area product (DAP) in mGy/cm2.
Statistical analysis
Statistical analysis was carried out using SPSS version 18 for Windows. Continuous data are expressed as mean value ± SD and categorical data as percentages. Categorical data were compared using chi-square (X2) analysis.
Results
Out of 2804 diagnostic coronary angiography procedures with or without coronary intervention via radial approach between January 2010 to June 2013, 45 patients (1.6%) were crossed over to transulnar approach after radial access failure. These patients constituted our study population.
Baseline demographic characteristics are shown in Table 1. The majority of patients were males, with mean age of 56 years; hypertension, diabetes mellitus and dyslipidemia were reported in 57.7%, 51.1% and 48.8% of the patients respectively. All procedures performed via right ulnar artery, with the exception of 2 (4.4%) procedures which performed vial left ulnar artery in prior coronary artery bypass patients.
Table 1.
Demographic characteristics of study cohort.
| Variable | Total 45 patients (%) |
|---|---|
| Male gender (%) | 29 (64.4) |
| Mean age (years) | 56.6 ± 8.8 |
| Hypertension (%) | 26 (57.7) |
| Diabetes (%) | 23 (51.1) |
| Dyslipidemia (%) | 22 (48.8) |
| Old MI (%) | 14 (31.1) |
| Prior PCI (%) | 4 (8.9) |
| Prior CABG (%) | 2 (4.45) |
| Current smoker (%) | 9 (20) |
| BMI (kg/m2) | 29.9 |
MI: myocardial infarction, PCI: percutaneous coronary intervention, CABG: coronary artery bypasses graft, CVA: cerebrovascular accidents.
The procedure outcome is illustrated in Table 2. Radial artery spasm (Fig. 1) prohibiting sheath or catheter advancement constituted the most frequent reason for radial access failure (64.4%) followed by failure to puncture the radial artery due to other different reasons (33.4%) (Fig. 2), and one significant radial artery loop (2.2%) (Fig. 3).
Table 2.
Procedure outcome.
| Variable | Number of patients (%) Total 45 |
|---|---|
| Reason of crossover to ulnar | |
| Radial artery spasm | 29 (64.4) |
| Failure to puncture | 15 (33.4) |
| Radial loop | 1 (2.2) |
| Ulnar pulse intensity compared to radial | |
| Equal | 31 (68.8) |
| Weak | 7 (15.6) |
| Absent | 7 (15.6) |
| Successful ulnar approach | 37 (82.2) |
| Diagnostic angiography | 28 (62.2) |
| Diagnostic angiography + PCI | 17 (37.8) |
| Reasons for failed ulnar approach | |
| Absent ulnar pulse | 6 (13.3) |
| Weak ulnar pulse | 2 (4.4) |
| Ulnar artery spasm | 8 (17.8) |
| Reported complications | |
| Transient numbness | 7 (15.5) |
| Minor hematoma | 6 (13.3) |
| Ulnar artery perforation | 1 (2.2) |
| Minor CVA | 1 (2.2) |
| Diagnostic procedure time (minutes) | 26.4 ± 18.04 |
| Diagnostic fluoroscopy time (minutes) | 6.5 ± 4.2 |
| Diagnostic radiation dose (mGy/cm2) | 95,737 ± 47,387 |
| PCI procedure time (minutes) | 44.6 ± 25.2 |
| PCI fluoroscopy time (minutes) | 14.2 ± 10.7 |
| PCI radiation dose (mGy/cm2) | 183,402 ± 109 |
Figure 1.
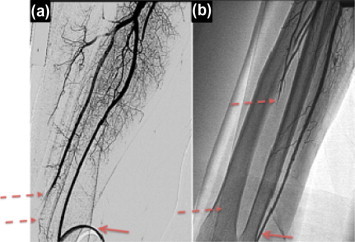
Radial artery spasm. Intense focal (a) and diffuse (b) radial artery spasm at the puncture site (2 dashed arrows). Note that radial artery spasm persisted until we crossed over to the ulnar artery and forearm angiography was performed via the side port of the ulnar sheath (continuous arrow).
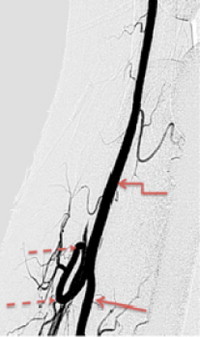
Figure 2.

Rare anatomical variation of the radial artery. Unique anatomical variation of the radial artery trifurcating into three smaller branches a few centimeters proximal to the styloid process of the radius (dashed arrows) making access to the main radial artery via any of these branches extremely difficult. Ulnar artery sheath in place (continuous arrow).
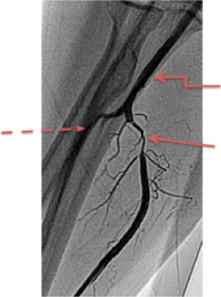
Figure 3.
Radial loop. Complete radial artery loop resulted in crossover to ulnar approach. Radial loop (dashed arrows), ulnar artery (continuous arrow) and brachial artery (curved arrow).
Ulnar pulse intensity was graded as compared to the radial pulse and was found to be good, weaker or absent in 68.8%, 15.6% and 15.6%, respectively. Successful transulnar approach was achieved in 37 patients (82.2%). The eight failed cases (17.8%) were mainly due to absent or weak ulnar pulse and crossed over to right femoral artery. Angiographically documented ulnar artery spasm was seen in eight patients (17.8%, Fig. 4). Diagnostic coronary angiography alone was performed in the majority of cases (62.2%) while PCI was performed in 17 cases (37.8%), eight of which were emergency interventions.
Figure 4.
Ulnar artery spasm. Intense focal ulnar artery spasm few millimeters from its origin (continuous arrow) that was treated with an extra dose of the vasodilatory cocktail 100 mcg of glyceryl trinitrate and 2.5 mg of verapamil through the side arm of the ulnar sheath. Note that the radial artery (dashed arrow) is small in size, most likely due to diffuse spasm. Brachial artery (curved arrow) is normal.
Complications included transient numbness of the hand in seven patients (15.5%), one ulnar artery perforation (2.2%, Fig. 5a) that was conservatively managed successfully and non-significant hematoma in six patients (13.3%, Fig. 5b). One patient experienced post procedural minor stroke that fully resolved three days later. No significant hand ischemia was noted in any of the patients.
Figure 5.
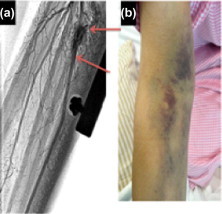
Ulnar artery perforation and superficial hematoma. localized ulnar artery perforation (a) and consequent superficial hematoma (b). The perforation was managed conservatively and the superficial hematoma healed few weeks later.
The procedure times for diagnostic and interventional procedures were 26.4 ± 18.04 and 44.6 ± 25.2 min, respectively. Procedure details are illustrated in Table 2.
Discussion
Radial artery is the default approach for coronary procedures at our institute. Whenever radial access fails (6.2%), femoral approach is the first alternative access, followed by transulnar approach. A single operator experienced in the radial approach performs the vast majority of ulnar accesses.
As we routinely implemented forearm angiography via side port of the ulnar sheath immediately after insertion, we were able to highlight some reasons for failure to access the radial artery. Radial artery spasm was the most common cause of radial access failure (64.4%). Many of these spasms were encountered during radial piercing with the micro-puncture needle where inability to advance the guidewire and sheath placement (Fig. 1) was encountered. In the remaining cases, despite successful puncturing of the radial artery and placement of the hydrophilic sheath, intense radial artery spasm compelled us to crossover to an alternative approach despite extra doses of the vasodilatory cocktail via the sheath. Moreover, many of these patients received pre-procedure sedation of fentanyl 25 mg and midazolam 1 mg intravenously. The radial artery is hypersensitive and spasmogenic as compared to other somatic vessels [14,15], and radial artery spasm is reported to occur in approximately 15% of patients during angiography [16].
The second most common cause of radial access failure was inability to puncture the radial artery (33.4%) due to weak or absent radial pulse. Selective forearm angiography via ulnar sheath enabled us to highlight the reason for radial access failure in three patients: two of these patients had hypoplastic radial artery, and one had a rare anatomic radial artery variation of early bifurcation into three small branches, ∼30 mm from the styloid of radius (Fig. 2). It would have been impossible to insert the radial sheath in any of these tiny branches.
In this study, we completed coronary angiography with or without intervention in 37 out of 45 patients with a success rate of 82.2%, which is a relatively reasonable frequency of success, comparable to other studies [9], and far less than reported by others [13,17,18].
Absent or weak ulnar pulse constituted the most common cause of access failure as the artery is deeply seated underneath the muscles. However, in a few patients who presented with absent or weak ulnar pulse we succeeded in puncturing the artery “blindly” and successfully performing the coronary procedure. On the other hand, despite finding a palpable ulnar pulse in other patients, we could not access the artery.
The incidence of ulnar artery spasm is not mentioned in previous publications. Among the documented ulnar spasms encountered in eight patients (17.7%), all responded to extra doses of vasodilatory cocktail (Fig. 4). It is important to note that many of these patients have also experienced intense radial spasm as well.
We particularly valued the usefulness of the ulnar approach in a patient who had bypass grafts and presented with Acute Coronary Syndrome/Non ST segment Elevation Myocardial Infarction (ACS/NSTEMI). He was loaded with aspirin and clopidogrel, and was given enoxaparin and eptifibatide. Our default approach for these patients was the left radial approach. We failed to access the artery due to intense radial spasm, and consequently crossed over to the right femoral approach. Unfortunately, the patient experienced large right inguinal hematoma that was managed with tight compression dressing. We then re-crossed over successfully to the left ulnar approach.
Transulnar approach in our study was feasible for both elective and urgent diagnostic and interventional procedures. Almost one third of our patients underwent successful PCI (17 patients, 37.8%), eight of whom were emergency cases (ST segment Elevation Myocardial Infarction (STEMI) or NSTEMI).
The chief objective to crossover to transulnar approach whenever transradial access fails is to reduce the anticipated local vascular complications of the transfemoral access. In our study, the reported rate of local vascular complications were 15.5% (seven out of 45 patients); six patients experienced minor hematoma (Fig. 5b) and one procedure was complicated by ulnar artery perforation (Fig. 5a). None of the patients experienced major bleeding requiring blood transfusion. All local vascular complications including perforation were treated conservatively as per recommended protocols [19]. All patients were closely observed for hand ischemia. Short-term clinical follow up as well as Duplex scan excluded compartment syndrome (Fig. 6a and b). All patients left hospital the next day and were asymptomatic, clinically and hemodynamically stable with no evidence of hand ischemia. Seven patients (15.5%) experienced pain and transient numbness during ulnar cannulation. All improved after a short time with no permanent neurological damage. One patient developed minor stroke few hours post procedure that totally resolved three days later. We do not feel that the stroke is attributable to the ulnar access.
Figure 6.
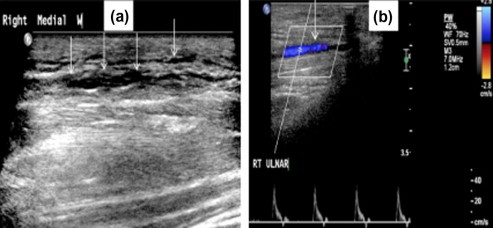
Duplex scan after ulnar artery perforation: (a): Gray scale ultrasound image of right wrist demonstrating diffuse subcutaneous hypo echoic hemorrhage (white arrow). (b): Longitudinal color Doppler image of the right wrist demonstrating normal antegrade flow in ulnar artery with no stenosis or pseudoaneurysm.
In the present study, the procedure time of the diagnostic coronary procedure with or without left ventriculography/aortography/non selective renal angiography was 26.3 ± 18.04 min, which is relatively long. This reflects our early experience in the transulnar approach as well as difficulty in accessing the ulnar artery as compared to the more superficial radial artery. This is consistent with the recently published AURA of ARTEMIS Study recommendations by Hahalis et al. [20].
Our team reported more fluoroscopy time than that reported in the transradial approach [21]. This possibly reflects increased experience and efficiency over time.
Conclusion
Whenever transradial access fails, a transulnar artery approach is a relatively feasible and safe alternative for either elective or emergency coronary diagnostic and interventional procedures. A transulnar artery approach has reasonable success rates and acceptable complication rates. The most frequent cause of transulnar access failure is absent or weak ulnar pulse. Almost all local vascular complications, including perforation, can be treated conservatively.
From our experience, the ulnar artery has a less intense pulse when compared to the radial artery. One third of our patients had impalpable or weak ulnar pulse, which is attributed to deep location of the ulnar artery beneath the muscle. Moreover, the ulnar nerve runs close to the artery and patients may experience brief “lightening” neurological discomfort during the puncture. The transulnar approach, therefore, should not be the first choice if the forearm is chosen for a coronary procedure.
Study limitations
There are several limitations to the current study. This is a single center study with a relatively small sample size. Further, the study represents our early experience in transulnar access in cases where transradial approach has failed. Radial artery spasm played a crucial role in the failure of the transradial approach. Sedation was given before the procedure according to operator discretion, and routine sedation might have reduced the incidence of transradial access failure.
Footnotes
Peer review under responsibility of King Saud University.
References
- 1.Jolly S.S., Yusuf S., Cairns J., Niemelä K., Xavier D., Widimsky P. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomized, parallel group, multicenter trial. Lancet. 2011;377(9775):1409–1420. doi: 10.1016/S0140-6736(11)60404-2. [DOI] [PubMed] [Google Scholar]
- 2.Kiemeneij F., Laarman G.J., Odekerken D., Slagboom T., van der Wieken R. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol. 1997;29(6):1269–1275. doi: 10.1016/s0735-1097(97)00064-8. [DOI] [PubMed] [Google Scholar]
- 3.Louvard Y., Lefèvre T., Allain A., Morice M. Coronary angiography through the radial or the femoral approach: the CARAFE study. Catheter Cardiovasc Interv. 2001;52(2):181–187. doi: 10.1002/1522-726x(200102)52:2<181::aid-ccd1044>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 4.Biondi-Zoccai G., Sciahbasi A., Bodí V., Fernández-Portales J., Kanei Y., Romagnoli E. Right versus left radial artery access for coronary procedures: an international collaborative systematic review and meta-analysis including 5 randomized trials and 3210 patients. Int J Cardiol. 2013;166(3):621–626. doi: 10.1016/j.ijcard.2011.11.100. [DOI] [PubMed] [Google Scholar]
- 5.Valsecchi O., Vassileva A., Musumeci G., Rossini R., Tespili M., Guagliumi G. Failure of transradial approach during coronary interventions: anatomic considerations. Catheter Cardiovasc Interv. 2006;67(6):870–878. doi: 10.1002/ccd.20732. [DOI] [PubMed] [Google Scholar]
- 6.Dehghani P., Mohammad A., Bajaj R., Hong T., Suen C.M., Sharieff W. Mechanism and predictors of failed transradial approach for percutaneous coronary interventions. JACC Cardiovasc Interv. 2009;2(11):1057–1064. doi: 10.1016/j.jcin.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Burzotta F., Trani C., Mazzari M.A., Tommasino A., Niccoli G., Porto I. Vascular complications and access crossover in 10,676 transradial percutaneous coronary procedures. Am Heart J. 2012;163(2):230–238. doi: 10.1016/j.ahj.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 8.Terashima M., Meguro T., Takeda H., Endoh N., Ito Y., Mitsuoka M. Percutaneous ulnar artery approach for coronary angiography: a preliminary report in nine patients. Catheter Cardiovasc Interv. 2001;53(3):410–414. doi: 10.1002/ccd.1192. [DOI] [PubMed] [Google Scholar]
- 9.Agostoni P., Zuffi A., Faurie B., Tosi P., Samim M., Belkacemi A. Same wrist intervention via the cubital (ulnar) artery in case of radial puncture failure for percutaneous cardiac catheterization or intervention: the multicenter SWITCH registry. Int J Cardiol. 2013;169(1):52–56. doi: 10.1016/j.ijcard.2013.08.080. [DOI] [PubMed] [Google Scholar]
- 10.Limbruno U., Rossini R., De Carlo M., Amoroso G., Ciabatti N., Petronio A.S. Percutaneous ulnar artery approach for primary coronary angioplasty: safety and feasibility. Catheter Cardiovasc Interv. 2004;61(1):56–59. doi: 10.1002/ccd.10671. [DOI] [PubMed] [Google Scholar]
- 11.Scanlon P.J., Faxon D.P., Audet A.M., Carabello B., Dehmer G.J., Eagle K.A. ACC/AHA guidelines for coronary angiography. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Coronary Angiography). Developed in collaboration with the Society for Cardiac Angiography and Interventions. J Am Coll Cardiol. 1999;33(6):1756–1824. doi: 10.1016/s0735-1097(99)00126-6. [DOI] [PubMed] [Google Scholar]
- 12.Pancholy S.B., Sanghvi K.A., Patel T.M. Radial artery access technique evaluation trial: randomized comparison of Seldinger versus modified Seldinger technique for arterial access for transradial catheterization. Catheter Cardiovasc Interv. 2012;80(2):288–291. doi: 10.1002/ccd.23445. [DOI] [PubMed] [Google Scholar]
- 13.Aptecar E., Pernes J.M., Chabane-Chaouch M., Bussy N., Catarino G., Shahmir A. Transulnar versus transradial artery approach for coronary angioplasty: the PCVI-CUBA study. Catheter Cardiovasc Interv. 2006;67(5):711–720. doi: 10.1002/ccd.20679. [DOI] [PubMed] [Google Scholar]
- 14.Poynter C.W.M. Congenital anomalies of the arteries and veins of the human body with bibliography. The University Studies of the University of Nebraska, Lincoln. 1922;22:1–106. [Google Scholar]
- 15.He G.W., Yang C.Q. Comparison among arterial grafts and coronary artery. An attempt at functional classification. J Thorac Cardiovasc Surg. 1995;109(4):707–715. doi: 10.1016/S0022-5223(95)70352-7. [DOI] [PubMed] [Google Scholar]
- 16.Ivica K., Josip L. Radial artery spasm during transradial coronary procedures. J Invasive Cardiol. 2011;23(12):527–531. [PubMed] [Google Scholar]
- 17.Mangin L., Bertrand O.F., De La Rochellière R., Proulx G., Lemay R., Barbeau G. The transulnar approach for coronary intervention: a safe alternative to transradial approach in selected patients. J Invasive Cardiol. 2005;17(2):77–79. [PubMed] [Google Scholar]
- 18.de Andrade P.B., Tebet M.A., Nogueira E.F., Esteves V.C., de Andrade M.V., Labrunie A. Transulnar approach as an alternative access site for coronary invasive procedures after transradial approach failure. Am Heart J. 2012;164(4):462–467. doi: 10.1016/j.ahj.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 19.Sallam M.M., Ali M., Al-Sekaiti R. Management of radial artery perforation complicating coronary intervention: a stepwise approach. J Interv Cardiol. 2011;24(5):401–406. doi: 10.1111/j.1540-8183.2011.00649.x. [DOI] [PubMed] [Google Scholar]
- 20.Hahalis G., Tsigkas G., Xanthopoulou I., Deftereos S., Ziakas A., Raisakis K. Transulnar compared with transradial artery approach as a default strategy for coronary procedures: a randomized trial. The Transulnar or Transradial Instead of Coronary Transfemoral Angiographies Study (the AURA of ARTEMIS Study) Circ Cardiovasc Interv. 2013;6(3):252–261. doi: 10.1161/CIRCINTERVENTIONS.112.000150. [DOI] [PubMed] [Google Scholar]
- 21.Sallam M., Al-Hadi H., Rathinasekar S., Chandy S. Comparative study of the radial and femoral artery approaches for diagnostic coronary angiography. Sultan Qaboos Univ Med J. 2009;9(3):272–278. [PMC free article] [PubMed] [Google Scholar]



