Abstract
Individual brief motivational intervention (iBMI) is an efficacious strategy to reduce heavy drinking by students who are mandated to receive an alcohol intervention following an alcohol-related event. However, despite the strong empirical support for iBMI, it is unknown if the results from rigorously controlled research on iBMI translate to real-world settings. Furthermore, many colleges lack the resources to provide iBMI to mandated students. Therefore, group-delivered BMI (gBMI) might be a cost-effective alternative that can be delivered to a large number of individuals. The purpose of this study was to conduct a comparative effectiveness evaluation of iBMI and gBMI as delivered by staff at a university health services center. Participants (N = 278) were college students who were mandated to receive an alcohol intervention following an alcohol-related incident. Participants were randomized to receive an individual (iBMI; n = 133) or a Group BMI (gBMI; n = 145). Results indicated that both iBMI and gBMI participants reduced their peak estimated blood alcohol concentration (BAC) and the number of negative alcohol-related consequences at 1-, 3-, and 6-months postintervention. The iBMI and gBMI conditions were not significantly different at follow-up. These findings provide preliminary support for the use of iBMI and gBMIs for college students in real-world settings.
Keywords: brief intervention, personalized feedback, college drinking, mandated students, comparative effectiveness
Alcohol misuse is a major public health concern, and college students are a designated high-risk population for alcohol use disorders (National Institute on Alcohol Abuse and Alcoholism [NIAAA], 2007) because of the association between heavy drinking in college and alcohol use disorders later in life (e.g., National Center on Addiction & Substance Abuse, 2007; Jennison, 2004). Many students are arrested, receive medical attention for alcohol-related incidents, or receive campus citations for violating campus alcohol policy (Hoover, 2003; Nicklin, 2000). Campuses often require that these individuals (referred to as mandated students) receive an alcohol intervention (Lewis & Marchell, 2006; Wechsler et al., 2002).
Rigorously controlled research studies have found that brief motivational intervention (BMI) is an efficacious strategy to reduce alcohol use or negative alcohol-related consequences relative to no-treatment or attention-control conditions (e.g., Barnett et al., 2004; Borsari & Carey, 2005; Carey, Carey, Maisto, & Henson, 2006; White, Mun, Pugh, & Morgan, 2007). In addition, BMI that contain components of the Brief Alcohol Screening and Intervention for College Students (BASICS; Dimeff, Baer, Kivlahan, & Marlatt, 1999) are more effective at reducing alcohol-related harms than other alcohol interventions (Carey, Scott-Sheldon, Carey, & DeMartini, 2007). BASICS is an individual BMI (iBMI) that incorporates motivational interviewing (MI; Miller & Rollnick, 2012) and personalized feedback (PF) about alcohol use patterns (i.e., information about normative perceptions of alcohol use and alcohol-related consequences) to reduce harmful drinking behaviors. MI is defined as “a collaborative conversation style for strengthening a person’s motivation and commitment to change” (Miller & Rollnick, 2012, p. 12) using several strategies, including expressing empathy, developing discrepancy, rolling with resistance, and supporting self-efficacy.
A small but growing body of research has linked Group BMI (gBMI) to reduced alcohol use and/or alcohol-related consequences in mandated college students (Alfonso, Hall, & Dunn, 2013; Fromme & Corbin, 2004; LaBrie, Lamb, Pedersen, & Quinlan, 2006; LaBrie, Thompson, Huchting, Lac, & Buckley, 2007; LaChance, Feldstein Ewing, Bryan, & Hutchison, 2009). However, one study (Cimini et al., 2009) found no significant differences in alcohol use and alcohol-related consequences between gBMI and two active conditions. However the two active conditions, peer performances and group discussions about alcohol-related scenarios and group alcohol education, lack empirical support making these results difficult to interpret due to lack of an assessment-only control group. Collectively, these evaluations of gBMIs for mandated students provide modest support for the efficacy of this delivery method. That said, a meta-analysis indicated that group-delivered alcohol interventions for college students are less efficacious than individually delivered interventions (Carey et al., 2007).
To date, only one study has directly compared iBMI and gBMI using a sample of mandated college students (Alfonso et al., 2013). In this efficacy trial, participants were randomized to receive (a) BASICS, (b) a 120-minute group-delivered and multicomponent intervention that utilizes MI called CHOICES (Parks & Woodford, 2005), or (c) a 15-minute computer intervention that provides PF (Walters, Vader, & Harris, 2007). Of the three groups, only BASICS demonstrated a statistically significant reduction in alcohol use and negative alcohol-related consequences. However, BASICS was not significantly different than CHOICES at follow-up, potentially because of power, attrition, and the lack of a short-term follow-up. Although this study compared an individual to a group delivered intervention, the differential content of BASICS and CHOICES compromised the ability to determine whether delivery format (individual vs. group) influenced outcomes. Therefore, a dose-equivalent comparison of iBMI and gBMI has yet to be conducted with college students.
The degree to which both iBMI and gBMI comparatively impact drinking is an essential step in identifying resource allocation for colleges and universities aimed at reducing harm associated with alcohol. Namely, the results from controlled alcohol intervention strategies, while critically important, may not translate to real-world settings (e.g., university health centers). Therefore, determining the comparative effectiveness of iBMI and gBMI is of particular importance as campuses that seek to deliver individual face-to-face interventions may discover they do not have the space and requisite support staff to deliver and schedule the interventions. As effective alcohol interventions delivered to large numbers of individuals in real-world settings will have a strong public health impact on heavy alcohol use (cf. Abrams et al., 1996; Glasgow, Vogt, & Boles, 1999), there is great need for effective group-delivered interventions that can conserve valuable resources (e.g., staff time and physical space to conduct the intervention).
To this end, the purpose of comparative effectiveness research is to assist with clinical and policy decision making from studies conducted in real-world settings (e.g., Luce et al., 2009). To our knowledge, this is the first study to conduct a preliminary comparative effectiveness evaluation of iBMI and gBMI for mandated college students that has the identical content and is delivered by university health center staff. We posit two hypotheses in the context of three commonly used alcohol outcome measures (drinks per week, peak estimated blood alcohol concentration [pBAC], and alcohol-related consequences). First, mandated students will reduce their alcohol use and consequences following a campus-initiated alcohol intervention regardless of the intervention modality. Second, iBMI participants will demonstrate greater reductions in alcohol use and consequences than participants receiving gBMI.
Method
Design
This study used a two-group design where participants were randomly assigned to receive an iBMI or gBMI following the completion of a 60-min baseline assessment. Both interventions were one session. The gBMI (M = 55.47 minutes; SD = 7.91) was significantly longer in length than the iBMI (M = 42.8 minutes; SD = 10.88; t(134) = −6.10; p < .001). Participants completed follow-up assessments at 1-, 3- and 6-month postintervention. All study procedures were approved by the university’s Institutional Review Board.
Participants
Prospective participants were undergraduate students at a 4-year, state-related university with an enrollment of over 44,000 students. Eligible students were mandated to receive an alcohol intervention after they violated campus alcohol policy, received medical attention for alcohol-related issues, or were arrested by police on campus or in the surrounding area. Students were referred to the campus’s heath center to receive the alcohol intervention and paid the campus-required $200 program fee.
Participants (N = 278) were 68% male, 81% Caucasian, 52% freshman, and they had an average age of 19.08 (SD = 1.19). Participants were referred for an alcohol intervention for the following offenses (students can be referred for multiple offenses): underage drinking (N = 146; 52%), presence of alcohol (N = 69; 25%), medical complications treated at the local Emergency Department (N = 39; 14%), public drunkenness (N = 33; 12%), hosting people in his or her residence hall room and alcohol and underage people are present (N = 8; 3%), driving under the influence (N = 7; 3%), and supplying alcohol to minors (N = 6; 2%). Sample demographics can be found in Table 1.
Table 1.
Group Comparisons at Baseline for iBMI (n = 133) and gBMI (n = 145)
| iBMI N (%) | gBMI N (%) | χ2 | p | |
|---|---|---|---|---|
| Male gender | 81 (61%) | 105 (72%) | 4.15 | 0.04 |
| Year in school | 1.10 | 0.77 | ||
| Freshman | 71 (53%) | 74 (51%) | ||
| Sophomore | 27 (20%) | 34 (23%) | ||
| Junior | 25 (19%) | 23 (16%) | ||
| Senior | 10 (8%) | 14 (10%) | ||
| Caucasian | 119 (89%) | 120 (83%) | 2.59 | 0.11 |
| iBMI M (SD)
|
gBMI M (SD)
|
Wilcoxon Two-Sample Statistic
|
p
|
|
| Age | 18.94 (1.06) | 19.08 (1.23) | 1,8097.50 | 0.47 |
| Freq. of drinking past month | 5.91(3.30) | 5.36 (3.87) | 1,9767.00 | 0.07 |
| Heavy drinking days | 1.26 (1.87) | 1.23 (1.69) | 1,8342.50 | 0.74 |
| Typical drinks per drinking day | 5.15 (2.80) | 5.09 (3.13) | 1,8618.50 | 0.92 |
| Peak drinks | 8.42 (5.23) | 8.18 (4.78) | 1,8507.50 | 0.94 |
| Typical BAC | 0.08 (0.06) | 0.07 (0.06) | 1,9215.00 | 0.39 |
| Peak BAC | 0.14 (0.10) | 0.13 (0.09) | 1,8963.00 | 0.54 |
| Drinks per week | 11.36 (8.55) | 11.41 (10.24) | 1,8703.00 | 0.82 |
| Alcohol-related consequences | 6.19 (5.00) | 5.59 (4.94) | 1,9057.00 | 0.45 |
| AUDIT | 7.72 (3.58) | 8.19 (3.66) | 1,7777.00 | 0.24 |
Note. Wilcoxon two-sample test used to test for group differences for continuous variables and a chi-square test was used for categorical variables. iBMI = Individual (one-on-one) brief motivational intervention; gBMI = group-delivered brief motivational intervention; BAC = estimated blood alcohol concentration; Alcohol-related consequences = the summed score of the Young Adult Alcohol Consequences Questionnaire (YAACQ); AUDIT = Alcohol Use Disorders Identification Test.
Recruitment
Recruitment started September 15, 2010 and ended November 19, 2010. Mandated students were approached by staff after they arrived for their initial scheduled appointment. Students were asked to complete a screening questionnaire lasting approximately 5 minutes to verify eligibility. Students were eligible to participate in this research study if they were 18 years old or older, an undergraduate, had an Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993) score of less than 16 which was consistent with campus policy and which has been demonstrated to be indicative of low-to-hazardous alcohol misuse (Bradley, McDonell, Kivlahan, Diehr, & Fihn, 1998), and did not report suicidal ideation on the Patient Health Questionnaire (PHQ-9; Spitzer, Kroenke, & Williams, 1999; consistent with campus policy). Eligible students were told that completion of the research study would satisfy the campus mandate and that they would be randomly assigned to receive a group or an individual session to discuss alcohol. Students were also told that participation in this study was not required, that they could drop out of the study at any time without penalty, and the alternative was to complete an identical baseline survey, receive an individual BASICS session (standard care at the host site), and complete a 1-month follow-up consistent with the campus mandate.
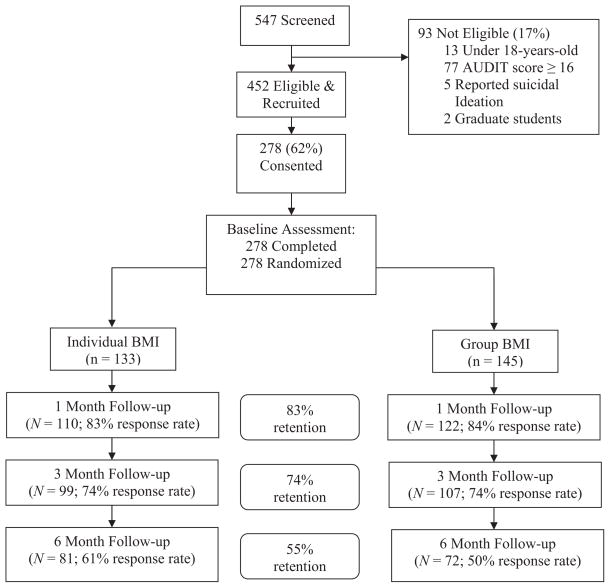
As can be seen in Figure 1, 547 students were screened for the study. All students who were not eligible to participate (n = 93) received an iBMI. All students who reported suicidal ideation or had AUDIT score of 16 or greater were referred to receive a more intensive intervention for alcohol use consistent with campus policy. Of the 452 remaining students, 278 (62%) consented to participate in the research and received an overview of the research procedures and consent form. Participants received a $10, $20, and $25 gift card for completing the 1-, 3-, and 6-month surveys, respectively.
Figure 1.
Participant flow diagram.
Follow-up assessments
Participants completed the 1-month postintervention survey on a computer at the health services center in order to complete their sanction. Participants were then contacted by e-mail to complete the 3- and 6-month follow-ups over the Internet at a location of their choice. Up to three reminder e-mails were sent to participants to complete the 3- and 6-month follow-ups. All surveys were computer administered using DatStat Illume™.
Measures
Demographics
Demographic information included gender, age, ethnicity, and year in school.
Screening
The PHQ-9 (Spitzer et al., 1999) is a 10-item questionnaire that was used to screen for suicidal ideation. The AUDIT (Saunders et al., 1993) is a brief (10-item) and widely used screening measure for hazardous alcohol use. AUDIT scores of 16 or more may be indicative of high or very high alcohol problem severity or alcohol dependence (Babor & Higgins-Biddle, 2001; Saunders et al., 1993). The mean AUDIT score for this sample was 7.98 (SD = 3.62). The AUDIT was used to screen for eligibility and for descriptive purposes.
Alcohol consumption
A modified version (Borsari & Carey, 2000) of the Daily Drinking Questionnaire (Collins, Parks, & Marlatt, 1985) was used to assess alcohol use during a typical and heavy drinking occasion and drug use over the past 30 days, and has been used with college students. Participants reported the amount of time spent drinking during a typical and peak drinking episode, along with their weight in order to estimate typical and peak blood alcohol concentration (BAC) using an equation (Matthews & Miller, 1979). Estimated peak BAC obtained from this equation using retrospective self-report data is significantly related to actual breath alcohol concentration (e.g., Hustad & Carey, 2005). Participants recorded the number of drinks consumed on an average day for each day of the week. The number of drinks consumed per week was obtained by adding the number of standard drinks consumed per day during a typical week during the past month.
Alcohol-related consequences
The Young Adult Alcohol Consequences Questionnaire (YAACQ; Read, Kahler, Strong, & Colder, 2006) is a 48-item inventory that was used to assess the total number of negative alcohol-related consequences in the past 30 days. This measure was specifically created to measure a diverse range of alcohol-related consequences (yes/no dichotomy) in college-aged students and is sensitive to changes in alcohol consumption in longitudinal studies (Kahler, Hustad, Barnett, Strong, & Borsari, 2008). The YAACQ had acceptable internal consistency in this sample at all assessment periods (Cronbach’s αs = 0.85–0.93).
Intervention fidelity
Sessions were coded using the Motivational Treatment Integrity Code, Version 3.0 (Moyers, Martin, Manuel, Hendrickson, & Miller, 2005). The MITI evaluates how well therapists implement MI. Randomly selected 20-min segments of the session are coded. The MITI contains two components: global ratings and behavior counts. The global ratings are (a) evocation; (b) collaboration; (c) autonomy/support; (d) direction; (e) empathy; (f) acknowledging change talk; and (g) inviting change talk. The behavior counts assess (a) MI adherent (e.g., emphasizing self-efficacy) and MI nonadherent (e.g., confronting) behaviors; (b) the types of questions (closed, open); and (c) types of reflections (simple, complex). This measure was used to evaluate MI fidelity.
Intervention Conditions
The interventions are both based on a widely disseminated and efficacious iBMI for volunteer (Borsari & Carey, 2000; Carey et al., 2006) and mandated students (Borsari & Carey, 2005; Borsari et al., 2012; Carey, Carey, Henson, Maisto, & DeMartini, 2011). This iBMI was a modification of BASICS (Dimeff et al., 1999). The interventions were delivered approximately 1 week after the baseline assessment. Sessions were audio recorded for supervision and fidelity purposes.
Interventionist training
Interventionists consisted of four full-time staff members and one graduate student in College Student Affairs. All staff members had a master’s degree in social work, counselor education, education, or exercise science (this person also completed all coursework for a master’s in counseling education). Four of the five interventionists had prior experience with substance use interventions. Interventionists received a BMI manual, participated in a 2-day training event that provided training on MI and BASICS, received an hour-long training on the use of MI in a group setting and group facilitation strategies (from Velasquez, Gaddy-Maurer, Crouch, & DiClemente, 2001), participated in and received feedback from several role-plays, and received weekly supervision. Interventionists completed an average of 2.55 (SD = 1.01) BMIs with mandated students prior to the start of the study. Each interventionist received 1 hour of individual and 1 hour of staff (i.e., group) supervision each week. During supervision, the audio-recorded sessions were reviewed and discussed focusing on MI strategies and PF delivery.
Individual BMI (iBMI)
In the iBMI condition, participants met one-on-one with the interventionist and received a gender-specific, computer-generated PF that was based on the responses to the baseline survey. PF included descriptive information about the participant’s drinking patterns (number of drinking days, number of drinks consumed in a typical and peak drinking occasion, amount of time spent consuming alcohol on a typical and peak drinking occasion), the campus-specific and gender-specific average number of drinks consumed during the four most common drinking days of the week (Wednesday, Thursday, Friday, and Saturday) with a campus-specific and gender-specific normative comparison, estimated typical and peak BAC, estimated amount of money spent on alcohol, estimated number of calories consumed from alcohol, the participant’s AUDIT score, biphasic effects of alcohol, family history of alcohol misuse, use of tobacco and other drugs, higher-risk behaviors (e.g., pregaming, playing drinking games, drinking alcohol with energy drinks), alcohol-related consequences, protective behaviors (e.g., drinking slowly), readiness and confidence to change, an overview of harm reduction, and a list of local resources. Participants also completed a decisional balance exercise where they described the pros and cons of changing and not changing their alcohol use.
Group BMI (gBMI)
The gBMI was an adaptation of the iBMI and was delivered by the same four interventionists who delivered the iBMI (one interventionist per group). To adapt the iBMI for the group setting, interventionists were instructed to facilitate the session by interacting with an individual student using MI strategies and then opening the discussion to other members of the group using open-ended questions or reflections. Each participant in the group received individually tailored PF and was discussed using MI strategies. The interventionists were also instructed to address the same topics during gBMI as during the iBMI, and also conducted a decisional balance exercise. There were 32 group sessions and groups ranged from two to seven participants (M = 4.34, SD = 1.89). Participants (n = 3) who were unable to attend one of the gBMIs due to a scheduling conflict received an iBMI. These three individuals were included in the gBMI condition using an intent-to-treat analysis.1
Data Analysis Plan
Generalized estimating equations method (GEE; Hardin & Hilbe, 2003) were used to evaluate the impact of the intervention conditions on the three outcome variables: estimated peak blood alcohol concentration (BAC), total number of alcoholic beverages consumed in a typical week, and the total number of alcohol-related consequences. Since we focused on evaluating population-averaged (i.e., group averages) versus individual-level (i.e., for each individual) trajectories, we chose GEE over mixed models (Zhang et al., 2011). Compared to mixed models, GEE does not require the distributional assumption on the outcome variable and the resultant estimators are robust to misspecification of correlation structure. We implemented GEE using PROC GENIMOD (SAS 9.3) to account for the correlation between repeated measures within the subjects. An unstructured correlation matrix was specified to allow unique estimates for each dependent variable across time (Kleinbaum, Kupper, Nizam, & Muller, 2008). In addition, peak BAC was analyzed using normal distribution and identity link; drinks per week and alcohol-related consequences were analyzed using a Poisson distribution, which is often used with count data, and a log link. The covariates included in the regression models are time (0 = baseline, 1 = 1-month, 3 = 3-month, 6 = 6-month) treated as categorical variable, gender (0 = male, 1 = female), condition (0 = iBMI, 1 = gBMI), and interaction between time and condition, which evaluated whether the intervention effects varied at each follow-up. When the interactions were not significant, we refitted the models excluding the interaction terms. If the overall time effect was significant, we evaluated the time effect through pairwise comparisons with the baseline value to determine how outcome variables changed after the intervention. Coefficient estimates (Est) and incidence rate ratios (IRR) were reported for linear regression and Poisson regression models, respectively. All available data were included in these analyses and all analyses were performed at a significance level of 0.05. Within-subjects effect sizes at each of the follow-ups were obtained using Cohen’s d (using pooled standard deviations), where 0.2 is classified as a small effect, 0.5 is a medium effect, and 0.8 is a large effect (Cohen, 1988).
Results
Preliminary Analyses
The distributional properties of these data were examined after data cleaning. Peak BACs greater than 0.40g/dL (n = 10) were recoded to 0.40g/dL as these BACs approached the median lethal dose.
Success of randomization
Conditions were compared at baseline using Wilcoxon’s two-sample (a nonparametric test for two independent samples that is used when the dependent variables are not normally distributed) and chi-square tests. The gBMI group had a larger percentage of male participants compared to the iBMI group (61% to 72%; χ2 = 4.15, p = .04). Participants in these two conditions did not differ on other demographic or alcohol use variables (see Table 1).
Attrition analysis
Regarding the completion rates for the follow-up assessments, 49% of the sample completed each of the three follow-up assessments; 22% completed 2 out of 3, 21% completed 1 out of 3, and only 8% missed every follow-up assessment. In light of the missing data, attrition analyses for all outcome and demographic variables were conducted to compare participants who completed all of the surveys (n = 137) to those who missed at least one follow-up (n = 141) using a series of Wilcoxon’s two-sample tests for continuous variables and chi-square tests for categorical variables. The only significant difference between the groups was that older participants were less likely to complete all follow-up assessments (p =.01). However, age was not significantly related to key outcomes and was dropped from these analyses. Furthermore, there were no significant differences between the intervention conditions according to the number of missed assessments ( , p =.29). Collectively, these results suggest that there is little indication of an attrition bias.
Intervention fidelity
In total, 26 iBMI sessions (out of 133) and six gBMI sessions (out of 32) were coded using the Motivational Interviewing Treatment Integrity Code (MITI; Moyers et al., 2005). This sample is consistent with other research in which a random 20% of sessions are selected for fidelity assessment. In the current study, fidelity assessment also included double-coding 20% of coded iBMI (n = 6) and 100% of selected gBMI (n = 6) with intraclass correlation (ICC) scores ranging from 0.52 to 0.98 identifying overall good coder reliability. The global scores and therapist behavior counts for the coded sessions are presented in Table 2. In addition, we conducted exploratory analyses using independent t tests to compare iBMI and gBMI on global scores and behavior counts. Generally, the two conditions were not significantly different on global ratings and therapist behaviors; however, interventionists provided information significantly more in the iBMI condition than during the gBMI (p < .001). Regarding overall competency of MI, the global ratings and the ratings for open-ended questions and the reflections-to-questions ratio are lower than competency levels (using a 3.5 cutoff for global scores; Miller & Rollnick, 2012). Some of the behavior counts were also below competency levels (e.g., ratio of questions to reflections, percent MI-consistent), but other ratings were consistent with MITI codings of MI fidelity in other trials with utilizing community mental health clinicians (Baer et al., 2004), peer counselors in the college setting (Mastroleo, Turrisi, Carney, Ray, & Larimer, 2010), and trauma center staff (Zatzick et al., 2013). In sum, the global ratings and behavior counts indicate that interventionists implemented MI with modest fidelity and the two conditions were relatively equivalent.
Table 2.
Comparison of Interventionist Behaviors Between Individual and Group Sessions
| Individual (N = 26) M (SD) | Group (N = 6) M (SD) | t | p | |
|---|---|---|---|---|
| Interventionist global scores | ||||
| Evocation | 2.90 (0.90) | 2.50 (0.55) | 1.03 | 0.31 |
| Collaboration | 2.76 (0.74) | 2.50 (0.55) | 0.81 | 0.43 |
| Autonomy | 3.00 (0.54) | 3.00 (0.00) | 0.00 | 1.00 |
| MI Spirit | 2.95 (0.77) | 2.67 (0.37) | 0.90 | 0.38 |
| Direction | 4.90 (0.41) | 5.00 (0.00) | −0.61 | 0.55 |
| Empathy | 3.14 (0.88) | 2.83 (0.75) | 0.79 | 0.43 |
| Acknowledging change talk | 2.66 (0.86) | 2.50 (0.55) | 0.42 | 0.68 |
| Inviting change talk | 2.93 (0.75) | 2.50 (0.84) | 1.26 | 0.22 |
| Interventionist behavior counts | ||||
| Giving information | 31.17 (9.05) | 15.83 (3.66) | 4.05 | <0.001 |
| MI-adherent statements | 2.48 (1.48) | 2.33 (1.03) | 0.24 | 0.82 |
| MI-inconsistent statements | 1.14 (1.93) | 0.17 (0.41) | 1.26 | 0.22 |
| Open-ended questions | 9.28 (5.91) | 10.00 (4.60) | −0.28 | 0.78 |
| Close-ended questions | 14.07 (7.04) | 16.83 (8.38) | −0.85 | 0.40 |
| Simple reflections | 11.10 (7.52) | 13.50 (10.08) | −0.67 | 0.51 |
| Complex reflections | 3.41 (2.63) | 3.67 (4.08) | −0.20 | 0.85 |
| Total questions asked | 23.24 (11.25) | 26.83 (11.05) | −0.71 | 0.48 |
| Total reflections | 14.52 (9.27) | 17.17 (13.96) | −0.58 | 0.56 |
Main Outcomes
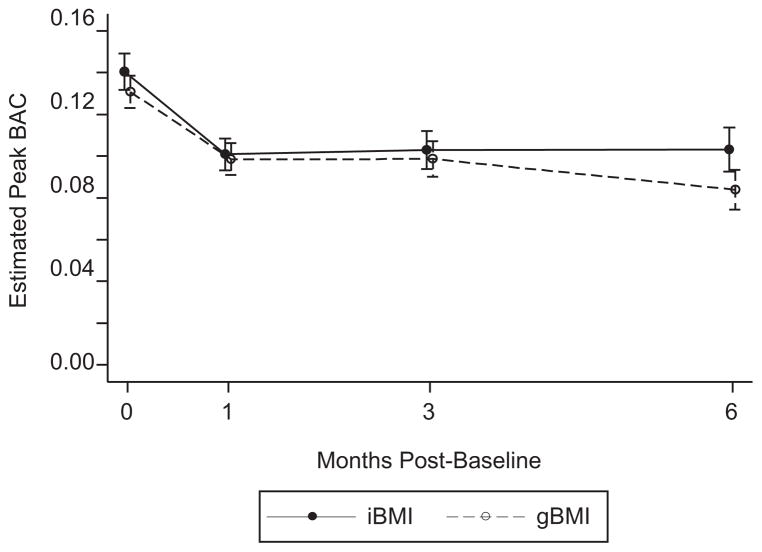
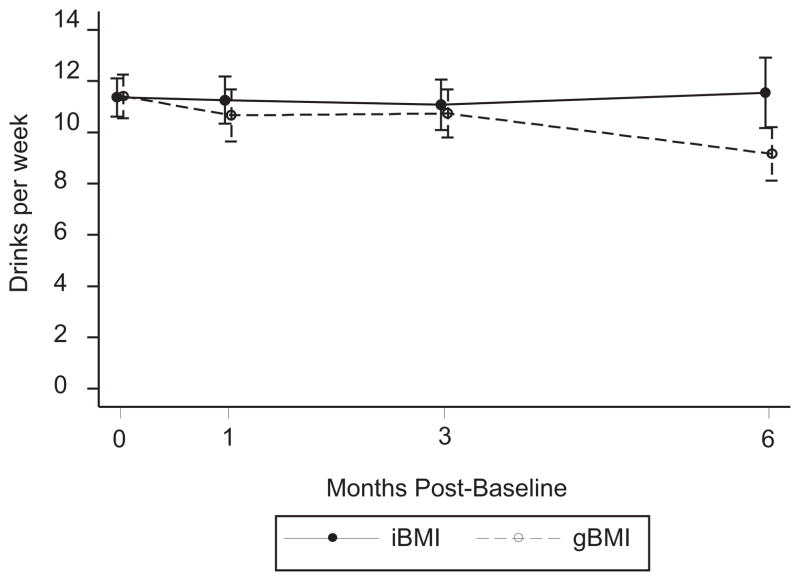
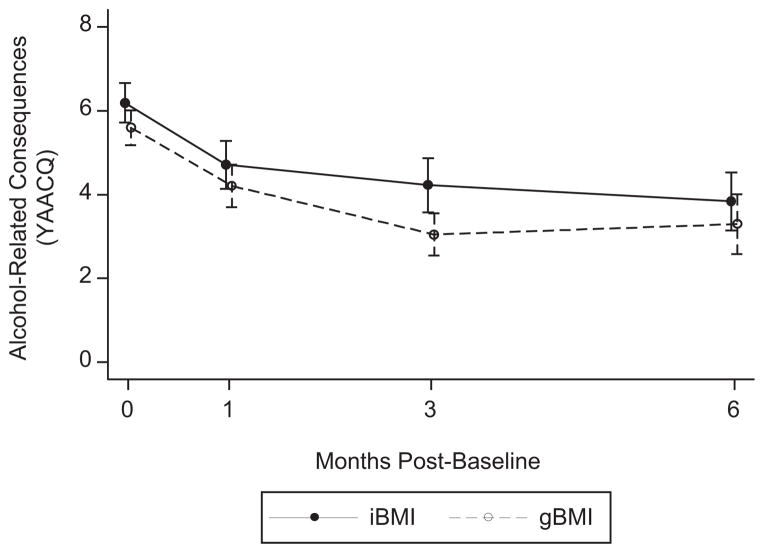
The raw means, standard deviations, and within-group effect sizes at each follow-up for the three outcome variables by group and across time are presented in Table 3. In addition, Figures 2, 3, and 4 show the primary outcomes at baseline, 1 month, 3 months, and 6 months for the iBMI and gBMI conditions.
Table 3.
Alcohol Use Variables at Baseline and Follow-Up and Magnitude of Change
| Measure | iBMI (n = 133) M (SD) | gBMI (n = 145) M (SD) | Effect size at 1 month (w/in-group change) | Effect size at 3 month (w/in-group change) | Effect size at 6 month (w/in-group change) |
|---|---|---|---|---|---|
| Peak BAC | |||||
| Baseline | 0.14 (0.10) | 0.13 (0.09) | iBMI = 0.44 | iBMI = 0.42 | iBMI = 0.40 |
| 1-month | 0.10 (0.08) | 0.10 (0.08) | gBMI = 0.35 | gBMI = 0.33 | gBMI = 0.59 |
| 3-month | 0.10 (0.09) | 0.10 (0.09) | Avg = 0.40 | Avg = 0.37 | Avg = 0.44 |
| 6-month | 0.10 (0.10) | 0.08 (0.08) | |||
| Ave. no. of drinks/week | |||||
| Baseline | 11.36 (8.55) | 11.41 (10.24) | iBMI = 0.01 | iBMI = 0.03 | iBMI = 0.02 |
| 1-month | 11.25 (9.65) | 10.66 (11.14) | gBMI = 0.07 | gBMI = 0.07 | gBMI = 0.24 |
| 3-month | 11.08 (9.81) | 10.73 (9.72) | Avg = 0.04 | Avg = 0.05 | Avg = 0.09 |
| 6-month | 11.54 (12.38) | 9.16 (8.85) | |||
| No. negative alcohol consequences | |||||
| Baseline | 6.19 (5.41) | 5.59 (4.94) | iBMI = 0.25 | iBMI = 0.33 | iBMI = 0.40 |
| 1-month | 4.71 (5.97) | 4.20 (5.57) | gBMI = 0.26 | gBMI = 0.50 | gBMI = 0.42 |
| 3-month | 4.22 (6.45) | 3.05 (5.21) | Avg = 0.26 | Avg = 0.41 | Avg = 0.41 |
| 6-month | 3.84 (6.41) | 3.30 (6.01) | |||
Note. iBMI = Individual (one-on-one) brief motivational intervention; gBMI = group-delivered brief motivational intervention; BAC = estimated blood alcohol concentration (g/dl). Alcohol consequences measured by the Young Adult Alcohol Consequence Questionnaire. Within-subjects effect size calculated using Cohen’s d. Avg = within-subjects effect size for both conditions.
Figure 2.
Estimated peak blood alcohol concentration over time. Bars represent standard error. iBMI = individual brief motivational intervention; gBMI = group brief motivational intervention.
Figure 3.
Number of drinks consumed in a typical week over time. Bars represent standard error. iBMI = individual brief motivational intervention; gBMI = group brief motivational intervention.
Figure 4.
Number of negative alcohol-related consequences over time. Bars represent standard error. iBMI = individual brief motivational intervention; gBMI = group brief motivational intervention; YAACQ = Young Adult Alcohol Consequences Questionnaire.
For peak BAC, the time by intervention condition interaction was not significant, indicating that the outcomes for peak BAC did not differ over time according to intervention condition (p = .62). There was a within-group effect evident: In both the iBMI and gBMI, peak BAC at the 1-, 3-, and 6-month follow-ups were significantly lower than baseline values (Ests = 0.04, ps ≤ 0.001). Peak BACs were not significantly different by gender (Est = −0.012, p = .20). The main effect for intervention condition was not significantly different on peak BAC (Est = −0.009, p = .33).
Regarding drinks per week, although the time by intervention condition interaction was not significant (p = .91), male participants reported consuming more alcohol in a typical week than female students (IRR = 1.87, p ≤ .0001). The main effects for the overall effect for time (p = .94) and intervention condition on drinks per week (IRR = 0.92, p = .38) were not significant.
In terms of alcohol-related consequences, the time by intervention condition interaction (p = .83) and the main effect for gender were not significant (IRR = 1.13, p = .28). Alcohol-related consequences at the 1-, 3- and 6-month follow-up assessments were significantly lower than baseline values, indicating that participants reduced their alcohol-related harms after the iBMI and gBMI (IRRs = 0.62–0.77, ps ≤ 0.001). iBMI and gBMI participants were not significantly different at the 1-month follow-up for alcohol-related consequences (IRR = 0.81, p = .20). The main effect for intervention condition on alcohol-related consequences was not significantly different (IRR = 0.87, p = .19).
Effect Sizes
The average and condition-specific magnitude of within-subjects change (Cohen’s d) for each follow-up was calculated for the three outcome variables and is presented in Table 3. A small-to-medium within-group effect size for peak BAC (d = 0.40) and a small effect size for alcohol related-consequences (d = 0.26) was observed for both conditions at the 1-month follow-up.
Discussion
This study evaluated the comparative effectiveness of individual and group brief motivational interventions with PF delivered in a university health center, allowing for a real-world setting evaluation. Results indicate that participants in both the iBMI and gBMI exhibited similar reductions in peak BAC and alcohol-related consequences. These findings are in contrast with previous research (Alfonso et al., 2013) and a meta-analysis (Carey et al., 2007) indicating that iBMI is more efficacious than gBMI. As previous research indicates that iBMIs are a cost-effective method to reduce college student alcohol use (Cowell, Brown, Mills, Bender, & Wedehase, 2012), the current results lend preliminary support for gBMI as an additional cost-effective approach to reduce high-risk college student drinking behaviors, as implementing gBMI holds promise to efficiently reach larger numbers of mandated students with fewer resources than iBMI. For example, the gBMI implemented in this project resulted in a mean saving of over 3 hours of interventionist time per group, providing support for the cost-savings related to interventionist time for gBMI when compared to iBMI. Thus, gBMI may produce a large public health impact on peak BAC and alcohol-related consequences given these results and the broad reach of this approach.
It should be highlighted that this study was not designed to evaluate the efficacy of gBMI. Due to a lack of a no-treatment comparison group, it is impossible to determine whether these interventions were primarily responsible for the observed changes in alcohol use and consequences. However, it is possible to place these results in the context of previous peer-reviewed research on alcohol interventions using the within-subjects effect sizes for the gBMI and iBMI conditions (see Table 3). Specifically, the within-subjects effect sizes for this study for peak BAC and alcohol-related consequences are similar to the mean within-subjects effect size for alcohol interventions that were similar to BASICS that also included a follow-up less than or equal to 4.33 weeks postintervention (Cohen’s d+peak BAC = 0.40 (range = 0.27–0.52); Cohen’s d+alcohol-related consequences = 0.22 [range = 0.15–0.29]; Lori Scott-Sheldon, personal communication, May 10, 2012). Thus, the overall magnitude of within-subject change in this sample for peak BAC and alcohol-related consequences is consistent with similar studies. While visually comparing effect sizes is no substitute for rigorous randomized controlled trials, these results provide preliminary support for the effectiveness of gBMI to reduce peak BAC and alcohol-related consequences in real-world settings, which is an important, and often uninvestigated standard used to evaluate the impact of interventions (Glasgow et al., 1999).
One initially counterintuitive finding was the lack of an overall intervention effect for either intervention on drinks per week, yet reductions were observed for peak BAC and alcohol-related consequences. In contrast, the majority of studies on BASICS have consistently demonstrated that college students who receive an alcohol intervention like BASICS demonstrate a significant reduction in the total number of drinks consumed per week (Carey et al., 2007). One explanation could be the difference in the variables assessed; although alcohol use and alcohol-related consequences are correlated (e.g., Borsari, Neal, Collins, & Carey, 2001), previous longitudinal research has identified that individual characteristics moderate the relationship between alcohol use and alcohol-related consequences (e.g., D’Lima, Pearson, & Kelley, 2012; Hustad, Carey, Carey, & Maisto, 2009). Therefore, while it is possible to observe a reduction in both alcohol use and associated harms, it is also possible to see a reduction in only one of those variables. An alternate explanation for the observed outcomes has to do with the content of the iBMI and gBMI. Specifically both intervention modalities placed a particularly strong emphasis on reducing negative alcohol-related consequences. This focus may have led to a reduction in the heavy alcohol use (captured by peak BAC), which in turn reduced negative consequences. It should also be noted that two other studies implementing this iBMI with mandated students demonstrated a reduction in alcohol-related consequences yet found no effect for drinks per week (Borsari & Carey, 2005; Borsari et al., 2012).
Although the purpose of the current study was to explore the comparative effectiveness of iBMI and gBMI, we evaluated whether these interventions were delivered with fidelity using MITI scores and behavior counts. Results indicated that interventionists were able to similarly deliver both interventions; however, iBMI resulted in significantly more information giving when compared to the gBMI. It is possible that iBMI may be more conducive to personal questions and concerns that might lead to giving information due to the one-on-one nature of the session when compared to gBMI. Notably, these analyses have a few limitations. First, these exploratory analyses conducted with a small sample (20%) of coded sessions. Second, the MITI analyzes a random 20-minute sample and it is possible that these fidelity scores and behavior counts would be differ with full session evaluations. Second, no client language was evaluated so although there is more information giving in iBMI, it is unclear if it is a direct result of student questions, the interventionist, or some combination. Finally, future research is needed to evaluate the direct link between information giving to drinking outcomes. In addition, future research is needed to identify methodological and intervention-specific mechanisms of change for alcohol use and alcohol-related consequences.
Collectively, these results indicate that the intervention delivery format (individual vs. group) may not be a critical component of BMI effectiveness. In light of the positive findings for BMIs in both individual and group format for college student drinking, it is likely that certain intervention components will be more likely to develop discrepancy and motivate individuals to change their behavior. However, the active components of BMIs are currently unknown (e.g., DiClemente, Marinilli, Singh, & Bellino, 2001; Miller & Rose, 2009; White, 2006). PF alone has the ability to reduce alcohol use and related consequences (e.g., Neighbors et al., 2010), and more recent research has identified the advantage of including PF as a component of individual interventions (Walters, Vader, Harris, Field, & Jouriles, 2009). Understanding the active components of an effective “treatment package” can allow researchers to focus on and seek to improve the subset of empirically supported components while eliminating ineffective components. For example, it is not clear whether MITI scores are predictive of clinical improvement. Future research will explore whether certain therapist and client utterances may be more predictive of outcomes than MITI scores.
The results of this study should be interpreted in the context of several limitations. First, due to the design of this study, we are not able to compare alcohol use and alcohol-related consequences that occurred before and after the citation incident. Previous studies suggest that mandated students demonstrated a modest reduction in alcohol use following an alcohol-related incident (Carey, Henson, Carey, & Maisto, 2009; Hustad et al., 2011; Morgan, White, & Mun, 2008), and it is possible that the incident might also motivate students to minimize the harms associated with their drinking. Second, the two conditions differ with respect to contact time and it is possible that this difference may have biased these results. Third, ethical considerations precluded the use of an assessment-only control group with college students mandated to receive treatment for alcohol use. Therefore, we are unable to be certain that the observed reductions were due solely to the iBMI and gBMI as naturalistic examinations of college student drinking (Del Boca, Darkes, Greenbaum, & Goldman, 2004; Hoeppner et al., 2012), albeit with nonmandated students, have demonstrated modest reductions in the amount of alcohol consumed during the first semester. Since participants were recruited during the course of one semester, it is possible that these results might differ with a longer recruitment period. That said, the magnitude of the reductions in peak BAC and alcohol-related consequences are similar to previous studies on BMI. Fourth, we excluded students with high or very high alcohol problem severity scores on the AUDIT (Babor & Higgins-Biddle, 2001; Saunders et al., 1993) or suicidal ideation; therefore, these results may not generalize to these groups. It is expected that students with high AUDIT scores would also benefit from an alcohol intervention and it is plausible that low-risk drinkers might benefit from a stepped-care approach (Borsari et al., 2012), where individuals receive one or more intervention according to their alcohol use severity or their response to an intervention. Future research should also evaluate other screening measures for both inclusion and stepped-care approaches to intervention assignment. Fifth, we relied on self-reported outcome variables. However, self-report is generally considered valid and reliable (Del Boca & Darkes, 2003). Sixth, exploratory comparisons of MITI scores by condition indicated that MI global and specific behaviors were consistent across the iBMI and gBMI. That said, future research utilizing formal process coding measures (e.g., the Motivational Interviewing Skills Code; Miller, Moyers, Ernst, & Amrhein, 2008) with larger samples will be able to identify mechanisms of behavior change in iBMI and gBMI. Finally, because this study was conducted at one university, these results may not generalize to all universities and health centers.
In summary, these results provide preliminary support for the comparative effectiveness and adoption of iBMI and gBMI in a university health center. However, group-delivered interventions are more efficient than individually delivered interventions as gBMI conserve valuable resources (professional staff time and physical space), factors that greatly influence the speed and delivery of an intervention. Thus, gBMI appears to be a viable option for universities interested in supplying services to a larger population of mandated students. The results have the potential to make a considerable impact on the risky drinking of mandated college students.
Acknowledgments
The project described was supported by the National Center for Advancing Translational Sciences, Grants UL1 TR000127 and KL2 TR000126. Brian Borsari’s contribution to this article was supported by National Institute on Alcohol Abuse and Alcoholism Grants R01-AA015518 and R01-AA017874. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. We thank everyone who contributed significantly to the work, including the participants, Liz Barton, Kate Carey, Andrea Dowhower, Lisa Glynn, Rochelle Holmes, Michelle Loxley, David Mallen, Jessica Nabozny, Colleen Peterson, Lori Scott-Sheldon, Steve Shephard, Damon Sims, Margaret Spears, and Katie Tenny for their assistance with this project.
Footnotes
We conducted a series of follow-up analyses where these three individuals who were assigned to the gBMI group and received iBMI were analyzed in the iBMI condition. Results from these analyses were virtually identical to the results when these participants were analyzed according to the random assigned condition.
Contributor Information
John T. P. Hustad, Pennsylvania State University College of Medicine
Nadine R. Mastroleo, Brown University
Lan Kong, Pennsylvania State University College of Medicine.
Rachel Urwin, University Health Services, The Pennsylvania State University.
Suzanne Zeman, University Health Services, The Pennsylvania State University.
Linda LaSalle, University Health Services, The Pennsylvania State University.
Brian Borsari, Providence VA Medical Center, Providence, Rhode Island and Brown University.
References
- Abrams DB, Orleans CT, Niaura RS, Goldstein MG, Prochaska JO, Velicer W. Integrating individual and public health perspectives for treatment of tobacco dependence under managed health care: A combined stepped-care and matching model. Annals of Behavioral Medicine. 1996;18:290–304. doi: 10.1007/BF02895291. [DOI] [PubMed] [Google Scholar]
- Alfonso J, Hall TV, Dunn ME. Feedback-based alcohol interventions for mandated students: An effectiveness study of three modalities. Clinical Psychology & Psychotherapy. 2013;20:411–423. doi: 10.1002/cpp.1786. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC. Brief intervention for hazardous and harmful drinking: A manual for use in primary care. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- Baer JS, Rosengren DB, Dunn CW, Wells EA, Ogle RL, Hartzler B. An evaluation of workshop training in motivational interviewing for addiction and mental health clinicians. Drug and Alcohol Dependence. 2004;73:99–106. doi: 10.1016/j.drugalcdep.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Barnett NP, Tevyaw TO, Fromme K, Borsari B, Carey KB, Corbin WR, Monti PM. Brief alcohol interventions with mandated or adjudicated college students. Alcoholism: Clinical and Experimental Research. 2004;28:966–975. doi: 10.1097/01.ALC.0000128231.97817.C7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology. 2000;68:728–733. doi: 10.1037/0022-006X.68.4.728. [DOI] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Two brief alcohol interventions for mandated college students. Psychology of Addictive Behaviors. 2005;19:296–302. doi: 10.1037/0893-164X.19.3.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Hustad JTP, Mastroleo NR, Tevyaw TO, Barnett NP, Kahler CW, Monti PM. Addressing alcohol use and problems in mandated college students: A randomized clinical trial using stepped care. Journal of Consulting and Clinical Psychology. 2012;80:1062–1074. doi: 10.1037/a0029902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Neal DJ, Collins SE, Carey KB. Differential utility of three indexes of risky drinking for predicting alcohol problems in college students. Psychology of Addictive Behaviors. 2001;15:321–324. doi: 10.1037/0893-164X.15.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley KA, McDonell MB, Kivlahan DR, Diehr P, Fihn SD. The AUDIT alcohol consumption questions: Reliability, validity and responsiveness to change in older male primary care patients. Alcoholism: Clinical & Experimental Research. 1998;22:1842–1849. doi: 10.1111/j.1530-0277.1998.tb03991.x. [DOI] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Henson JM, Maisto SA, DeMartini KS. Brief alcohol interventions for mandated college students: Comparison of face-to-face counseling and computer-delivered interventions. Addiction. 2011;106:528–537. doi: 10.1111/j.1360-0443.2010.03193.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Maisto SA, Henson JM. Brief motivational interventions for heavy college drinkers: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74:943–954. doi: 10.1037/0022-006X.74.5.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, Maisto SA. Computer versus in-person intervention for students violating campus alcohol policy. Journal of Consulting and Clinical Psychology. 2009;77:74–87. doi: 10.1037/a0014281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32:2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimini MD, Martens MP, Larimer ME, Kilmer JR, Neighbors C, Monserrat JM. Assessing the effectiveness of peer-facilitated interventions addressing high-risk drinking among judicially mandated college students. Journal of Studies on Alcohol and Drugs. 2009;16:57–66. doi: 10.15288/jsads.2009.s16.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- Cowell AJ, Brown JM, Mills MJ, Bender RH, Wedehase BJ. Cost-effectiveness analysis of motivational interviewing with feedback to reduce drinking among a sample of college students. Journal of Studies on Alcohol and Drugs. 2012;73:226–237. doi: 10.15288/jsad.2012.73.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: State of the science and challenges for research. Addiction. 2003;98(Suppl 2):1–12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J, Greenbaum PE, Goldman MS. Up close and personal: Temporal variability in the drinking of individual college students during their first year. Journal of Consulting and Clinical Psychology. 2004;72:155–164. doi: 10.1037/0022-006X.72.2.155. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Marinilli AS, Singh M, Bellino LE. The role of feedback in the process of health behavior change. American Journal of Health Behavior. 2001;25:217–227. doi: 10.5993/AJHB.25.3.8. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief alcohol screening and intervention for college students (BASICS): A harm reduction approach. New York, NY: Guilford Press; 1999. [Google Scholar]
- D’Lima GM, Pearson MR, Kelley ML. Protective behavioral strategies as a mediator and moderator of the relationship between self-regulation and alcohol-related consequences in first-year college students. Psychology of Addictive Behaviors. 2012;26:330–337. doi: 10.1037/a0026942. [DOI] [PubMed] [Google Scholar]
- Fromme K, Corbin W. Prevention of heavy drinking and associated negative consequences among mandated and voluntary college students. Journal of Consulting and Clinical Psychology. 2004;72:1038–1049. doi: 10.1037/0022-006X.72.6.1038. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health. 1999;89:1322–1327. doi: 10.2105/AJPH.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardin JW, Hilbe JM. Generalized estimating equations. Boca Raton, FL: Chapman and Hall/CRC; 2003. [Google Scholar]
- Hoeppner BB, Barnett NP, Jackson KM, Colby SM, Kahler CW, Monti PM, Corriveau D. Daily college student drinking patterns across the first year of college. Journal of Studies on Alcohol and Drugs. 2012;73:613–624. doi: 10.15288/jsad.2012.73.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoover E. Drug and alcohol arrests increased on campuses in 2001. Chronicle of Higher Education. 2003 May 16; Retrieved from http://chronicle.com/article/DrugAlcohol-Arrests/32868.
- Hustad JTP, Carey KB. Using calculations to estimate blood alcohol concentrations for naturally occurring drinking episodes: A validity study. Journal of Studies on Alcohol. 2005;66:130–138. doi: 10.15288/jsa.2005.66.130. [DOI] [PubMed] [Google Scholar]
- Hustad JTP, Carey KB, Carey MP, Maisto SA. Self-regulation, alcohol consumption and consequences in college student heavy drinkers: A latent growth analysis. Journal of Studies on Alcohol and Drugs. 2009;70:373–382. doi: 10.15288/jsad.2009.70.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustad JTP, Eaton Short E, Borsari B, Barnett NP, Tevyaw TO, Kahler CW. College alcohol citations result in modest reductions in student drinking. Journal of Substance Abuse Treatment. 2011;40:281–286. doi: 10.1016/j.jsat.2010.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennison KM. The short-term effects and unintended long-term consequences of binge drinking in college: A 10-year follow-up study. The American Journal of Drug and Alcohol Abuse. 2004;30:659–684. doi: 10.1081/ADA-200032331. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Hustad JTP, Barnett NP, Strong DR, Borsari B. Validation of the 30-Day version of the Brief Young Adult Alcohol Consequences Questionnaire for use in longitudinal studies. Journal of Studies on Alcohol and Drugs. 2008;69:611–615. doi: 10.15288/jsad.2008.69.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinbaum DG, Kupper LL, Nizam A, Muller KE. Applied regression analysis and other multivariable methods. Belmont, CA: Duxbury; 2008. [Google Scholar]
- LaBrie JW, Lamb TF, Pedersen ER, Quinlan T. A group motivational interviewing intervention reduces drinking and alcohol-related consequences in adjudicated college students. Journal of College Student Development. 2006;47:267–280. doi: 10.1353/csd.2006.0031. [DOI] [Google Scholar]
- LaBrie JW, Thompson AD, Huchting K, Lac A, Buckley K. A group motivational interviewing intervention reduces drinking and alcohol-related negative consequences in adjudicated college women. Addictive Behaviors. 2007;32:2549–2562. doi: 10.1016/j.addbeh.2007.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaChance H, Feldstein Ewing SW, Bryan AD, Hutchison KE. What makes group MET work? A randomized controlled trial of college student drinkers in mandated alcohol diversion. Psychology of Addictive Behaviors. 2009;23:598–612. doi: 10.1037/a0016633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis DK, Marchell TC. Safety first: A medical amnesty approach to alcohol poisoning at a U.S. university. International Journal of Drug Policy. 2006;17:329–338. doi: 10.1016/j.drugpo.2006.02.007. [DOI] [Google Scholar]
- Luce BR, Kramer JM, Goodman SN, Connor JT, Tunis S, Whicher D, Schwartz JS. Rethinking randomized clinical trials for comparative effectiveness research: The need for transformational change. Annals of Internal Medicine. 2009;151:206–209. doi: 10.7326/0003-4819-151-3-200908040-00126. [DOI] [PubMed] [Google Scholar]
- Mastroleo NR, Turrisi R, Carney JV, Ray AE, Larimer ME. Examination of posttraining supervision of peer counselors in a motivational enhancement intervention to reduce drinking in a sample of heavy-drinking college students. Journal of Substance Abuse Treatment. 2010;39:289–297. doi: 10.1016/j.jsat.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews DB, Miller WR. Estimating blood alcohol concentration: Two computer programs and their applications in therapy and research. Addictive Behaviors. 1979;4:55–60. doi: 10.1016/0306-4603(79)90021-2. [DOI] [PubMed] [Google Scholar]
- Miller WR, Moyers TB, Ernst D, Amrhein P. Manual for the motivational interviewing skills code (MISC) Version 2.1. Albuquerque, NM: Center on Alcoholism, Substance Abuse, and Addictions, The University of New Mexico; 2008. Retrieved from http://casaa.unm.edu/download/misc.pdf. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. 3. New York, NY: Guilford Press; 2012. [Google Scholar]
- Miller WR, Rose GS. Toward a theory of motivational interviewing. American Psychologist. 2009;64:527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan TJ, White HR, Mun EY. Changes in drinking before a mandated brief intervention with college students. Journal of Studies on Alcohol and Drugs. 2008;69:286–290. doi: 10.15288/jsad.2008.69.286. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- National Center on Addiction and Substance Abuse at Columbia University. Wasting the best and brightest: Substance abuse at America’s colleges and universities. New York, NY: Author; 2007. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. What colleges need to know now: An update on college drinking research. Washington DC: National Institutes of Health; 2007. [Google Scholar]
- Neighbors C, Lewis MA, Atkins DC, Jensen MM, Walter T, Fossos N, Larimer ME. Efficacy of web-based personalized normative feedback: A two-year randomized controlled trial. Journal of Consulting and Clinical Psychology. 2010;78:898–911. doi: 10.1037/a0020766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicklin JL. Arrests at colleges surge for alcohol and drug violations. The Chronicle of Higher Education. 2000 Jun 9; Retrieved from http://chronicle.com/article/Arrests-at-Colleges-Surge-for/23670.
- Parks GA, Woodford MS. CHOICES about alcohol: A brief alcohol abuse prevention and harm reduction program for college students. In: Walz GR, Yep RK, editors. Vistas: Compelling perspectives on counseling. Alexandria, VA: American Counseling Association; 2005. pp. 171–174. [Google Scholar]
- Read JP, Kahler CW, Strong DR, Colder CR. Development and preliminary validation of the young adult alcohol consequences questionnaire. Journal of Studies on Alcohol. 2006;67:169–177. doi: 10.15288/jsa.2006.67.169. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA: Journal of the American Medical Association. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Velasquez MM, Gaddy-Maurer G, Crouch C, DiClemente CC. Group treatment for substance abuse: A stages of change therapy manual. New York, NY: The Guilford Press; 2001. [Google Scholar]
- Walters ST, Vader AM, Harris TR. A controlled trial of web-based feedback for heavy drinking college students. Prevention Science. 2007;8:83–88. doi: 10.1007/s11121-006-0059-9. [DOI] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR, Field CA, Jouriles EN. Dismantling motivational interviewing and feedback for college drinkers: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77:64–73. doi: 10.1037/a0014472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993–2001. Journal of American College Health. 2002;50:203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- White HR. Reduction of alcohol-related harm on United States college campuses: The use of personal feedback interventions. International Journal of Drug Policy. 2006;17:310–319. doi: 10.1016/j.drugpo.2006.02.006. [DOI] [Google Scholar]
- White HR, Mun EY, Pugh L, Morgan TJ. Long-term effects of brief substance use interventions for mandated college students: Sleeper effects of an in-person personal feedback intervention. Alcoholism: Clinical and Experimental Research. 2007;31:1380–1391. doi: 10.1111/j.1530-0277.2007.00435.x. [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Donovan DM, Dunn C, Jurkovich GJ, Wang J, Russo J, Gentilello LM. Disseminating Organizational Screening and Brief Intervention Services (DO-SBIS) for alcohol at trauma centers study design. General Hospital Psychiatry. 2013;35:174–180. doi: 10.1016/j.genhosppsych.2012.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H, Xia Y, Chen R, Gunzler D, Tang W, Tu X. Modeling longitudinal binomial responses: Implications from two dueling paradigms. Journal of Applied Statistics. 2011;38:2373–2390. doi: 10.1080/02664763.2010.550038. [DOI] [Google Scholar]