Abstract
Background
Although lung transplantation improves quality of life, most psychosocial research focuses on adverse psychological and social functioning outcomes. Positive effects, particularly in the late-term years as physical morbidities increase, have received little attention. We provide the first data on a psychological benefit—posttraumatic growth (PTG)—and we focused on long-term (>5 year) survivors.
Methods
Among 178 patients from a prospective study of mental health during the first two years posttransplant, we re-contacted survivors 6–11 years posttransplant. We assessed PTG (i.e., positive psychological change resulting from the transplant) and examined its relationship to other patient characteristics with multivariable regression analyses.
Results
64 patients (86% of survivors) were assessed (M=8.1 years posttransplant, SD=1.2). Mean PTG exceeded the scale’s midpoint (M=38.6, SD=10.0; scale midpoint=25). Recipients experiencing greater PTG were female (p=.022), less educated (p=.014), and had a history of posttransplant panic disorder (p=.005), greater friend support (p=.048), and better perceived health (p=.032). Neither other pre- or posttransplant mood and anxiety disorders nor transplant-related morbidities (acute rejection, bronchiolitis obliterans syndrome) predicted PTG.
Conclusions
PTG exceeded levels observed in other chronic disease populations, suggesting that lung transplantation may uniquely foster positive psychological change in long-term survivors. PTG occurs despite physical and psychiatric morbidities. Whether PTG promotes other positive posttransplant psychosocial outcomes deserves attention.
Keywords: lung transplantation, posttraumatic growth, psychological outcomes
Introduction
For individuals with advanced lung disease, lung transplantation can extend survival and improve quality of life. These gains, however, are accompanied by the development of new morbidities (e.g., acute and chronic graft rejection) and other chronic stressors, including the need to adhere to a multi-component medical regimen, transplant-related financial strains, and requirements for ongoing or new medical care. Moreover, lung recipients face life expectancies that are not only shorter than normal for their chronological ages but also lag behind those of other organ recipients.(1,2) In turn, although some studies considering psychosocial outcomes focus on general pre- to posttransplant improvements with lung transplantation,(3–5) most such research has focused on adverse posttransplant outcomes, including somatic, psychological, behavioral, and social functioning problems.(6–13) Positive consequences of lung transplantation, especially in the long-term years as transplant-related morbidities become more common, have received little attention. In particular, psychological benefits, such as posttraumatic growth (PTG), have yet to be examined in long-term survivors of lung transplantation or any other solid organ transplantation.
PTG refers to positive psychological change conferred after a major life event or traumatic experience.(14,15) It has been observed in other patient groups confronted with potentially life-threatening acute and chronic illnesses, including cancer, heart disease, and HIV.(16–21) Although such patients frequently acknowledge the fear and psychological distress associated with learning of their condition and undergoing treatment, they often also report positive psychological outcomes from both their acute illness experience and subsequent life with chronic illness. Organ transplantation presents a different scenario: receiving a transplant, while stressful, is typically viewed by patients as life-giving rather than life-threatening.(22,23) Whether this would lead to greater or lesser PTG relative to that observed in other populations is unknown. Furthermore, although it is known that some transplant recipients experience posttraumatic stress disorder related to the transplant experience (PTSD-T) or other mood and anxiety disorders in the aftermath of transplantation,(7,9,12, 22,24) there are no data on whether having developed psychiatric disorder affects the transplant recipient’s potential for achieving psychological growth in the long-term posttransplant. Finally, with respect to lung transplantation in particular, the rising medical burden in the years following lung transplantation may also affect the degree of PTG that patients experience, although whether a higher burden level would accentuate or undermine PTG is not clear.
We sought to examine these issues in a cohort of long-term (>5 year) survivors after lung transplantation. Our goals were (a) determine if, and to what degree, these recipients experienced PTG, (b) examine whether any such growth was affected by the experience of early posttransplant PTSD-T or other mood and anxiety disorders, and (c) identify psychosocial and medical burden-related predictors and correlates of long-term PTG. With respect to our third goal, we focused on variables known or hypothesized from conceptual models of stressor exposure to be linked to psychological outcomes.(15,22,25–27)
Methods
Study Participants
Participants were 64 lung recipients who participated in our earlier study during the first two years posttransplant.(7) We originally enrolled 178 adults (aged ≥18) shortly after hospital discharge after their first lung transplant. They received transplants at the University of Pittsburgh Medical Center between November, 1999 and August, 2004 (95% of all lung recipients during this timeframe; we could identify no demographic or transplant-related differences between those who did vs. did not enroll(7)). Of the 74 alive at the time of the current follow-up study (conducted from August 2010 through May 2011), three could not be contacted (4%). Of those contacted, three refused, two were too ill to participate, and two consented but withdrew before the study interview due to illness (response rate among those contacted, 90%).
Procedure
The University of Pittsburgh Institutional Review Board approved the study. All participants provided verbal informed consent for the current long-term follow-up telephone interviews. Participants had previously provided written informed consent for medical record reviews and for earlier interviews to assess psychiatric disorder conducted during the first two years post-transplant.
The current long-term follow-up interviews collected data on recipients’ PTG, perceived health and psychosocial status. The interviews involved fully structured, closed-ended questions and were conducted by a trained bachelor’s degree-level interviewer. The interviewer was trained to reliability and monitored throughout the study by a senior clinician researcher. Transplant-related information and information on morbidities with onsets since transplant were obtained from recipients’ medical records.
The procedures for conducting earlier mental health interviews during the first two years post-transplant have been described previously.(7) In brief, the lung recipients were interviewed at 2-, 7-, 12-, 18-, and 24-months posttransplant to assess the presence and history of mood and anxiety disorders, as described further below. Interviewers conducting these psychiatric interviews were mental health professionals with advanced degrees who were trained and monitored to maintain reliability by a senior clinician researcher, as detailed previously.(7)
Measures
In addition to collecting standard demographic data, measures were obtained in four domains. For measures that consisted of multi-item scales, descriptive information is presented in Table 1.
Table 1.
Multi-item measures administered to lung transplant recipients at the long-term follow-up assessment.
| Measure | Mean (SD) or percent of sample |
Possible range |
Internal consistency reliability, α |
|---|---|---|---|
| PTGI-SF (higher = more growth)a | 38.6 (10.0) | 0 – 50 | .88 |
| QLTP Respiratory subscale (higher = more symptoms) | 5.8 (2.4) | 0 – 10 | n/ac |
| SF-36 Physical functioning (higher = better) | 67.0 (26.3) | 0 – 100 | .93 |
| SF-36 General health (higher = better) | 53.7 (25.8) | 0 – 100 | .77 |
| LOT: Optimism (higher = less)a | 8.0 (4.7) | 0 – 24 | .72 |
| Sense of mastery (higher = more)a | 3.2 (0.5) | 1 – 4 | .81 |
| Caregiver Support, % lowa | 35.9d | 1 – 5 | .92 |
| Friend Support Scale, % lowb | 30.6d | 1 – 4 | .90 |
Abbreviations: PTGI-SF, Posttraumatic Growth Inventory-Short Form; QLTP, Questionnaire for Lung Transplant Patients; SF-36, Short-Form 36; LOT, Life Orientation Test.
One respondent was missing a score on this variable.
Two respondents were missing scores on this variable.
This measure is a count; Cronbach’s alpha is not applicable.
This measure’s distribution was skewed; scores were dichotomized to identify respondents with the low support; see text for additional explanation.
PTG at Long-term Follow-up
PTG was assessed with the 10-item Posttraumatic Growth Inventory-Short Form (PTGI-SF).(28) The PTGI-SF measures positive life changes after a trauma or major life event, and its psychometric properties have been documented (28). Participants rated the degree to which they had experienced each item as a result of their lung transplantation. Items are rated on a 6-point scale (ranging from 0 to 5); they are summed to yield a total score, which represents growth occurring across five areas: appreciation of life, new possibilities, personal strength, relating to others, and spiritual change.
Psychiatric Disorder Early Posttransplant and Pretransplant Lifetime History
Mood and anxiety disorders were assessed in our original study prospectively during the first two years post-transplant. Specifically, we used the mood and anxiety modules from the Structured Clinical Interview for DSM-IVR (SCID) to determine the presence of PTSD-T, panic disorder, generalized anxiety disorder (GAD) and major depressive disorder (MDD).(7) The 2-month posttransplant interview assessed disorders from the time of transplant; subsequent interviews at 7-, 12- and 24-months covered the period since last assessment. For the present study, we examined whether each disorder occurred or not at any time during the 2-year time frame. Because posttransplant GAD was rare (prevalence, 4%), there were too few cases to consider it in the present analyses. At the 2-month interview, we also determined whether respondents had a pretransplant lifetime history of either panic disorder, GAD or MDD using the SCID.
Transplant-Related Medical Characteristics and Morbidities
We obtained standard information from recipients’ medical records on such characteristics as indication for transplant. We also obtained information on factors associated with the transplant that might indicate a more difficult recovery, including length of hospitalization following transplant and days in the intensive care unit (ICU). Further, we collected information on major transplant-related physical morbidities developing at any point from transplant to the time of our follow-up assessment including whether recipients had (a) experienced acute graft rejection at grade ≥A2, assigned according to standard criteria at the time that samples were graded,(29,30) and (b) developed Bronchiolitis Obliterans Syndrome (BOS) at grade ≥1 utilizing standard criteria.(31) BOS is the clinical manifestation of chronic graft rejection, and is formally defined as graft deterioration secondary to persistent airflow obstruction.(31)
At the long-term follow-up assessment, we measured current respiratory symptoms with the self-report Questionnaire for Lung Transplant Patients (QLTP) respiratory subscale.(32) We measured recipients’ perceptions of general health and physical functioning at the follow-up assessment with the SF-36 general health and physical functioning subscales.(33)
Psychosocial Characteristics at Long-term Follow-up
We assessed recipients’ intrapersonal resources with two measures: the Life Orientation Test assessed dispositional optimism,(34) and the Sense of Mastery Scale assessed perceptions of self-mastery or control over one’s circumstances.(35) We also assessed two elements of recipients’ interpersonal resources. First, we measured social support from their primary family caregiver (i.e., the individual who provided the most support and assistance if needed) with the Caregiver Support Scale, a short version adapted from Spanier’s Dyadic Adjustment Scale(35,36) and used previously with transplant populations.(37–39) This measure was skewed. In addition, some individuals reported that they had no caregiver (n=20). Because we reasoned that having poor caregiver support was worse than having either no family caregiver or good caregiver support (consistent with our own and others’ observations in other patient populations(40,41–44)), we created a dichotomous variable identifying those scoring in the lowest third of the caregiver support scale vs. all other respondents (i.e., vs. those with higher caregiver support as well as those with no caregiver). Second, we administered the Friend Support Scale to measure perceived emotional and instrumental support from friends.(45) This measure was also skewed; scores were dichotomized to identify recipients with the poorest support (lower third of the distribution) relative to remaining individuals.
Data Analysis
We used descriptive statistics to determine the sample’s demographic and transplant-related profile and to address our first study aim regarding the nature and extent of PTG. To examine whether some PTG scale items were endorsed more strongly than others, we considered item scores in two ways. First, we considered the mean on each PTGI-SF item’s 0 to 5-point rating scale concerning the degree of growth experienced. Second, because past studies have reported the distribution of scores in terms of clinically significant growth we examined the percentage of the sample endorsing each item at a moderate degree or above (≥3).
We calculated t-tests to address our second study aim regarding whether PTG levels differed among recipients who did vs. did not have diagnosable psychiatric disorder early posttransplant (as well as pretransplant). To identify the unique demographic, transplant-related, psychiatric, and psychosocial predictors and correlates of PTG (our third study aim), we utilized linear regression analysis. Given our sample size, we limited the number of variables in the regression analysis by requiring that variables have a simple bivariate correlation with PTG of at least modest size (r≥0.20).(46,47) Before conducting statistical tests, we examined variables’ distributions and their interrelationships for evidence of multicollinearity in order to determine that analytic assumptions were met.(48) Because PTGI scores were skewed, we applied a log transformation to normalize the scores before performing statistical tests.
Results
Sample Description
Demographic and transplant-related characteristics are shown in Table 2. The sample is similar to the national distribution of lung recipients transplanted during the same time period in terms of gender, age, indication for transplant, and type of lung transplant.(2)
Table 2.
Demographic and transplant-related characteristics in 64 lung transplant recipients
| Characteristic | Descriptive Statistic |
|---|---|
| Demographic | |
| Age (years), mean (SD) | 58.1 (10.4) |
| Gender, % male | 46.9 |
| Race/ethnicity, % European American | 95.3 |
| Education, % | |
| High school graduate or less | 35.9 |
| Some college or college graduate | 40.6 |
| Post-graduate education | 23.4 |
| Employed, % yes | 21.9 |
| Occupation (when last employed), % nonprofessional | 21.4 |
| Marital status, % married or living with a partner | 67.2 |
| Transplant-related | |
| Indication for transplant, % | |
| COPD/emphysema | 34.4 |
| Idiopathic pulmonary fibrosis | 18.8 |
| Cystic fibrosis | 18.8 |
| Other | 28.1 |
| Age (years) at transplant, mean (SD) | 49.7 (10.3) |
| Years since transplant, mean (SD) | 8.1 (1.2) |
| Type of lung transplant, % | |
| Single | 46.9 |
| Bilaterala | 53.1 |
| Days hospitalized post-transplant, mean (SD) | 24.3 (16.9) |
| median (IQR) | 17 (12–34) |
| Days in ICU post-transplant, mean (SD) | 7.5 (9.5) |
| median (IQR) | 3 (1–8) |
| Retransplant, % yes | 7.8 |
| Developed acute graft rejection, % yes | 65.6 |
| Developed BOS (chronic rejection), % yes | 46.9 |
Includes one heart – lung recipient
COPD, chronic obstructive pulmonary disease
ICU, intensive care unit
BOS, bronchiolitis obliterans syndrome
Lung recipients were an average of 8.1 years posttransplant at the time of the long-term follow-up assessment (SD=1.2, median=8.0, range: 6.5–11.0). The 64 individuals in our sample were demographically indistinguishable from surviving members of the original cohort of 178 recipients who were not re-enrolled at follow-up.
Level and Nature of PTG at Follow-up
The mean PTG levels in the sample was above the midpoint of the 50-point scale (M=38.6, SD=10.0). The median of 40, a value slightly higher than the mean, reflects the fact that the distribution of total scores was somewhat negatively skewed, i.e., the bulk of the sample scored on the upper end of the scale, indicating more growth (interquartile range, 34–45, absolute range, 10–50).
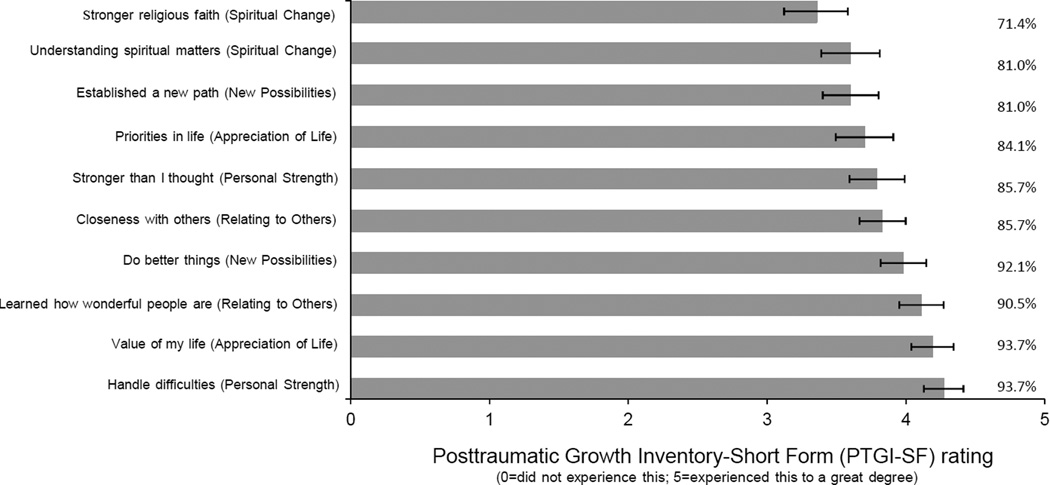
The distributions of PTGI-SF item means and the percentage of respondents endorsing each item at a level indicating clinically significant growth are presented in Figure 1. “I know better that I can handle difficulties,” one of the two personal strength items, was most strongly endorsed (M=4.3, SD=1.0), and it was endorsed at or above a moderate degree by 93.7% of the sample. A second item (“I have a greater appreciation for the value of my own life”) was also very commonly endorsed (Figure 1). The two spiritual change items were endorsed less frequently and at lower degrees than most other items. Overall, respondents rated an average of 8.4 of the 10 items at a moderate degree or higher, and 50.8% of the sample endorsed all 10 items at least at a moderate degree.
Figure 1.
Mean item scores (and SE bars), and percent of the sample endorsing each item at a moderate degree or higher (> 3).
PTG Levels at Follow-up in Recipients With vs. Without Early Posttransplant or Lifetime History of Mood and Anxiety Disorders
Table 3 compares PTG levels in recipients who did vs. did not experience diagnosable disorders either during the first two years posttransplant or at any point in their lifetime before transplant. With respect to posttransplant disorder, there were no differences in PTG related to either PTSD-T or posttransplant MDD. However, recipients who experienced panic disorder in the early years posttransplant reported significantly higher PTG than those without posttransplant panic disorder. Table 3 shows that there were no statistically reliable differences in recipients’ PTG as a function of pretransplant lifetime history of mood or anxiety disorder.
Table 3.
Levels of post-traumatic growth at long-term follow-up in lung recipients with and without mood and anxiety disorders during the first two years post-transplant or before transplant.
| PTGI level, Mean (SD)a |
t-test | p | |
|---|---|---|---|
| Disorder during the first two years posttransplant | |||
| PTSD-T,b yes (n=8) | 39.8 (9.4) | 0.41 | .683 |
| no (n=50) | 39.1 (9.7) | ||
| Panic disorder,c yes (n=12) | 43.3 (9.8) | 3.09 | .003 |
| no (n=50) | 37.4 (9.9) | ||
| Major depression,c yes (n=12) | 38.8 (11.6) | 0.51 | .611 |
| no (n=50) | 39.2 (9.8) | ||
| Lifetime mood or anxiety disorder pretransplant, yes (n=35) | 37.2 (11.0) | 0.87 | .388 |
| no (n=27) | 40.3 (8.7) |
Note. Of the 12 posttransplant cases of panic disorder, 6 had a pretransplant history of this disorder. Of the 12 posttransplant cases of major depression, 10 had a pretransplant history of this disorder. PTSD-T was specific to the transplant experience and thus could only be determined posttransplant.
PTGI was log transformed prior to analyses to reduce skewness in its distribution. Means and SDs are presented in original units to facilitate interpretation. One respondent was missing data on the PTGI.
6 recipients were missing data on this variable.
2 recipients were missing data on this variable.
Factors Associated with PTG
As shown in the first column of Table 4, six variables met our entry criterion for the regression analysis (bivariate associations with PTG of ≥.20) and were included in the regression model. The table also displays standardized regression coefficients for variables included in the model. Recipients who were female, had less education, experienced panic disorder early posttransplant, and had higher social support from friends at the long-term follow-up assessment had significantly higher PTG. Individuals with poorer perceived general health at the follow-up assessment experienced less PTG.
Table 4.
Associations of posttraumatic growth with demographic, health, and psychosocial characteristics.a
| Posttraumatic growth | ||||
|---|---|---|---|---|
| Correlation Coefficient, r |
Regression Resultsb | |||
| b | t | p | ||
| Demographics | ||||
| Age, years | .12 | — | — | — |
| Gender, female | .38 | .27 | 2.35 | .022 |
| Level of education (1= high school or less, 3=post-graduate education) | −.22 | −.28 | 2.55 | .014 |
| Employed, yes | −.10 | — | — | — |
| Occupation, nonprofessional | −.09 | — | — | — |
| Marital status, married or living with a partner | .02 | — | — | — |
| Transplant-related characteristics and morbidities | ||||
| Type of transplant, double lung | −.09 | — | — | — |
| Indication for transplant, COPD/emphysema | .22 | .11 | 0.93 | .358 |
| Hospitalized post-transplant, days | .11 | — | — | — |
| In ICU post-transplant, days | .14 | — | — | — |
| Time since transplant, years | −.02 | — | — | — |
| Developed acute graft rejection, yes | .07 | — | — | — |
| Developed BOS, yes | .03 | — | — | — |
| Respiratory symptoms at long-term follow-up (0=less, 10=more) | −.17 | — | — | — |
| SF-36 Physical functioning at long-term follow-up (0=poorer, 100=better) | .04 | — | — | — |
| SF-36 General health at long-term follow-up (0=poorer, 100=better) | −.21 | −.25 | 2.20 | .032 |
| Psychiatric disorder pre- or early post-transplant | ||||
| Posttransplant occurrence of PTSD-T, yes | −.06 | — | — | — |
| Posttransplant occurrence of panic disorder, yes | .37 | .33 | 2.95 | .005 |
| Posttransplant occurrence of major depression, yes | .07 | — | — | — |
| Lifetime pretransplant history of mood or anxiety disorder, yes | −.11 | — | — | — |
| Psychosocial characteristics assessed at long-term follow-up | ||||
| Optimism (0=more, 10=less) | .09 | — | — | — |
| Mastery (1=less, 4=more) | .08 | — | — | — |
| Support from family caregiver, higher | .01 | — | — | — |
| Support from friends, higher | .30 | .22 | 2.02 | .048 |
| R for model | .65 | |||
| F (6, 55) | 6.62 | < .001 | ||
PTGI, days hospitalized post-transplant, and days in ICU post-transplant were log transformed prior to analyses to reduce skewness in their distributions.
Correlations between the 6 variables entered into the regression model ranged from 0.02 to .38, mean=.17, median=.17. There was thus no evidence of multicollinearity between the variables.(48)
Discussion
Perhaps because survival rates are poorer after lung transplantation than other forms of organ transplantation, there is a dearth of literature on psychosocial outcomes in lung recipients in the late-term (≥5 years) posttransplant. The few reports consider only very small samples (n’s <30) and document declines in emotional and social functioning (relative to either their well-being earlier posttransplant or relative to normative data), in parallel with increasing physical morbidities.(49,50) Whether long-term survivors feel they have achieved psychological benefits from the transplant, especially as they face declining health, is unknown.
Our sample of 64 lung recipients, who averaged 8 years posttransplant, ranging up to 11 years, reported on whether or not they had achieved psychological growth due to the transplant experience. Their levels of growth appear to exceed that observed in other patient groups. Specifically, although it is challenging to make comparisons across studies because they vary in whether they use the PTGI-SF or the longer 21-item version of the scale, when we convert all studies’ PTGI scores from total scores (sum of items) to mean scores (sum divided by number of items asked), the mean in our sample (3.86) is higher than levels observed in studies of other chronic disease groups include patients with cancer, HIV disease, and heart disease (means ranging from 2.25 to 3.61).(16–21,51–53)
We may have observed higher PTG in part because our sample was many years posttransplant, and the Tedeschi and Calhoun theory of PTG(14,15) suggests that growth increases with time. Most studies of other chronic illness populations have assessed growth only within months to a few years after the onset of health problems or treatment.(26) However, even among the few chronic disease studies with very long follow-up (e.g., 5–15 years),(16,26) PTG levels are lower than in our sample. Thus, factors other than time may have contributed to degree of PTG in our sample. In particular, the fact that transplantation is typically viewed as a positive, life-giving event—as opposed to a life-threatening process—may have contributed to the high levels growth we observed. Qualitative studies show that lung recipients (and, indeed, all types of deceased donor organ recipients) report a new-found appreciation of their lives because it is from another person’s loss that they have been able to receive the new organs; they may feel that they have a responsibility, and a desire, to make the most of their lives after transplant.(23,54,55)
With respect to correlates and predictors of PTG, our findings are generally consistent with those reported across the PTG literature in that demographic factors such as female gender and lower education were associated with greater PTG in our sample.(14,26,53) We also observed that greater friend support at long-term follow-up was associated with greater PTG. However, because support was assessed at the same timepoint as PTG, it is not clear if social support promotes PTG or if social relationships are strengthened by the presence of PTG, as Koutrouli et al.(26) noted in their review of PTG studies in breast cancer patients.
We found that poorer perceived general health reported at the long-term follow-up was a significant correlate of reduced PTG (regression coefficient, −.25), while objective indicators of health status including the presence of BOS were not reliably related to PTG. Similar differences in the impact of perceived vs. objective health indicators on PTG have been noted in other chronic disease populations,(16,51) supporting the conclusion that clinicians should carefully attend to patients’ own appraisals of their health because these appraisals are more intimately linked to other psychological reactions than are actual illness parameters.
The finding that development of BOS, in particular, was not reliably related to PTG is noteworthy, given multiple studies showing BOS to be associated with poorer general quality of life after lung transplantation (as recently reviewed by Yusen (56)). If BOS is related to quality of life, why would it not be associated with PTG? We suggest that it may be because PTG represents a fundamentally different outcome from those typically conceptualized under the rubric of quality of life.(11,12,24,33,50) Indeed, PTG may be experienced no matter whether concurrent quality of life is high or low.(14,15) This may also explain why our measure of physical functional quality of life showed minimal association with PTG in the present sample.
Although PTSD-T and other psychiatric conditions including panic disorder and major depression are relatively common in the early years after lung transplantation and are themselves strongly predicted by a pretransplant history of mood and anxiety disorders (7), we found only limited evidence that these disorders affected lung recipients’ likelihood of achieving PTG by the late-term years posttransplant. Namely, a history of panic disorder early posttransplant led to heightened PTG, while neither PTSD-T nor major depression early posttransplant (nor lifetime pretransplant history of mood or anxiety disorder) predicted PTG levels. Links between PTSD, depression, and PTG have also been difficult to document in other studies.(26,51,57,58) With respect to posttransplant panic disorder, we have previously suggested that lung recipients’ heightened propensity for this problem may be linked to a conditioned fear response and/or a pattern of catastrophic thinking in the presence of symptoms related to their respiratory disease.(7,59,60) Fearing the worst in the aftermath of lung transplantation and, indeed, in the face of other difficult life experiences may ultimately be a key ingredient to experiencing PTG: such intense emotional responses are the factors that shake individuals’ assumptions about their lives and put into motion a rebuilding or restructuring of how they view themselves.(15,61)
Interestingly, we found no indication that psychological dispositional characteristics—namely optimism and sense of mastery assessed at the long-term follow-up—were associated with lung recipients’ degree of PTG. This is an encouraging finding, suggesting that even individuals who are not by nature optimistic or do not perceive themselves to have high levels of control over their lives are still capable of achieving PTG in relation to the transplant. It also is consistent with the view that the capacity to develop PTG is not a dispositional characteristic. Instead, as theory suggests (14,15), it develops in response to specific life experiences, and lung transplantation appears to have a powerful impact in this regard.
Our study has limitations. First, our sample is small and comes from a single site, thus potentially limiting generalizability. Second, considerable time passed between our previous assessment at two years posttransplant and our long-term follow-up assessment when PTG was evaluated. Our lung recipients’ interim psychosocial and mental health profiles are unknown, which limits our ability to connect long-term PTG with psychosocial status across the entire posttransplant period. Third, we could not examine some transplant-related health parameters such as rehospitalizations and occurrence of infections as predictors of PTG because, as time passes posttransplant, ascertainment of these factors is likely to be incomplete since patients may receive care locally rather than return for diagnosis and care at the transplant center. However, we were able to examine the predictive role of major, highly prevalent transplant-related parameters that are closely monitored through routine, lifelong evaluation at our center, including the development of BOS. Fourth, some lung recipients did not participate in our follow-up assessment due to illness and they may not have achieved the level of PTG noted in study participants. These nonparticipants constituted only 5% of eligible individuals and thus their exclusion may have had minimal impact on our findings. Finally, our focus at follow-up was on long-term survivors. Whether individuals whose survival times were shorter also achieved PTG, and when PTG begins to occur during the posttransplant trajectory, remain unknown.
In conclusion, long-term survivors of lung transplantation experience PTG at levels that appear higher than those observed in other chronic disease populations. From a clinical standpoint, it is encouraging PTG is not precluded by the presence of transplant-related morbidities or by past occurrences of psychiatric disorder. Because PTG has been linked to a reduced risk of subsequent morbidity and mortality in cancer, HIV, and heart disease patients,(17,62,63) future study of its role as a risk moderator for health outcomes and ability to manage chronic illness after lung transplantation is warranted.
Acknowledgments
Preparation of this article was supported in part by Grant R01 MH072718 from the National Institute of Mental Health, Rockville, MD and a grant from the North American Transplant Coordinators Organization (NATCO).
Footnotes
Author Contributions
Fox, Dew, Posluszny: research conceptualization/design; data collection, analysis and interpretation; manuscript preparation and final approval. Dew: obtaining funding. DiMartini, DeVito Dabbs: design, interpretation of analysis, manuscript revision and final approval. Zomak: research conceptualization, interpretation of analysis, manuscript revision and final approval. Bermudez: data collection, interpretation of analysis, manuscript revision and final approval.
References
- 1.Christie JD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: 29th adult lung and heart-lung transplant report - 2012. J Heart Lung Transplant. 31(10):1073–1086. doi: 10.1016/j.healun.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR) Rockville, MD: Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation; 2012. [Last accessed July 30, 2013]. OPTN/SRTR 2011 Annual Data Report. ( http://srtr.transplant.hrsa.gov/annual_reports/2011/Default.aspx). [Google Scholar]
- 3.Lanuza DM, Lefaiver C, McCabe M, Farcas GA, Garrity E., Jr Prospective study of functional status and quality of life before and after lung transplantation. Chest. 2000;18:115–122. doi: 10.1378/chest.118.1.115. [DOI] [PubMed] [Google Scholar]
- 4.Goetzmann L, Ruegg L, Stamm M, et al. Psychosocial profiles after transplantation: A 24-month follow-up of heart, lung, liver, kidney and allogeneic bone-marrow patients. Transplantation. 2008;86:662–668. doi: 10.1097/TP.0b013e3181817dd7. [DOI] [PubMed] [Google Scholar]
- 5.Santana MJ, Feeny D, Jackson K, Weinkauf J, Lien D. Improvement in health-related quality of life after lung transplantation. Canadian Respir J. 2009;16(5):153–158. doi: 10.1155/2009/843215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bosma OH, Vermuelen KM, Verschurren EA, et al. Adherence to immunosuppression in adult lung transplant recioients: Prevalence and risk factors. J Heart Lung Transplant. 2011;30:1275–1280. doi: 10.1016/j.healun.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 7.Dew MA, DiMartini AF, DeVito Dabbs AJ, et al. Onset and risk factors for anxiety and depression during the first 2 years after lung transplantation. Gen Hosp Psychiatry. 2012;34:127–138. doi: 10.1016/j.genhosppsych.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dew MA, DiMartini AF, DeVito Dabbs A, et al. Adherence to the medical regimen during the first two years after lung transplantation. Transplantation. 2008;85(2):193–202. doi: 10.1097/TP.0b013e318160135f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fusar-Poli P, Lazzaretti M, Ceruti M, et al. Depression after lung transplantation: Causes and treatment. Lung. 2007;185(2):55–65. doi: 10.1007/s00408-006-0093-1. [DOI] [PubMed] [Google Scholar]
- 10.Goetzmann L, Klaghofer R, Wagner-Huber R, et al. Psychosocial vulnerability predicts psychosocial outcome after an organ transplant: results of a prospective study with lung, liver, and bone-marrow patients. J Psychosom Res. 2007;62(1):93–100. doi: 10.1016/j.jpsychores.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 11.Kugler C, Fischer S, Gottlieb J, et al. Symptom experience after lung transplantation: Impact on quality of life and adherence. Clin Transplant. 2007;21(5):590–596. doi: 10.1111/j.1399-0012.2007.00693.x. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberger EM, Dew MA, DiMartini AF, DeVito Dabbs AJ, Yusen RD. Psychosocial issues facing lung transplant candidates, recipients and family caregivers. Thorac Surg Clin. 2012;22:517–529. doi: 10.1016/j.thorsurg.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu J, Adeboyejo O, Wagley E, et al. Daily burdens of recipients and family caregivers after lung transplant. Prog Transplant. 2012;22(1):41–47. doi: 10.7182/pit2012815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J Trauma Stress. 1996;9:455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- 15.Tedeschi RG, Calhoun LG. Posttraumatic growth: Conceptual foundations and empirical evidence. Psycholog Inquiry. 2004;15:1–18. [Google Scholar]
- 16.Lelorain S, Tessier P, Florin A, Bonnaud-Antignac A. Posttraumatic growth in long term breast cancer survivors: Relation to coping, social support and cognitive processing. J Health Psychol. 2012;17(5):627–639. doi: 10.1177/1359105311427475. [DOI] [PubMed] [Google Scholar]
- 17.Leung YW, Alter DA, Prior PL, et al. Posttraumatic growth in coronary artery disease outpatients: Relationship to degree of trauma and health service use. J Psychosom Res. 2012;72(4):293–299. doi: 10.1016/j.jpsychores.2011.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nightingale VR, Sher TG, Hansen NB. The impact of receiving an HIV diagnosis and cognitive processing on psychological distress and posttraumatic growth. J Trauma Stress. 2010;23(4):452–460. doi: 10.1002/jts.20554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Posluszny DM, Baum A, Edwards RP, Dew MA. Posttraumatic growth in women one year after diagnosis for gynecologic cancer or benign conditions. J Psychosoc Oncol. 2011;29(5):561–572. doi: 10.1080/07347332.2011.599360. [DOI] [PubMed] [Google Scholar]
- 20.Rand KL, Cripe LD, Monahan PO, et al. Illness appraisal, religious coping, and psychological responses in men with advanced cancer. Support Care Cancer. 2012;20(8):1719–1728. doi: 10.1007/s00520-011-1265-y. [DOI] [PubMed] [Google Scholar]
- 21.Sheikh AI. Posttraumatic growth in the context of heart disease. J Clin Psychol Medical Settings. 2004;11(4):265–273. [Google Scholar]
- 22.Dew MA, DiMartini AF. Transplantation. In: Friedman HS, editor. Health Psychology. NY: Oxford University Press; 2011. [Google Scholar]
- 23.Simmons RG, Marine SK, Simmons RL. Gift of life: The effect of organ transplantation on individual, family, and societal dynamics. New Brunswick, NJ: Transaction Publishers, Inc.; 1987. [Google Scholar]
- 24.Cupples SA, Dew MA, Grady KL, et al. The present status of research on psychosocial outcomes in cardiothoracic transplantation: Review and recommendations for the field. J Heart Lung Transplant. 2006;25:716–725. doi: 10.1016/j.healun.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 25.Hammen C. Stress and depression. Ann Rev Clin Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 26.Koutrouli N, Anagnostopoulos F, Potamianos G. Posttraumatic stress disorder and posttraumatic growth in breast cancer patients: a systematic review. Women Health. 2012;52(5):503–516. doi: 10.1080/03630242.2012.679337. [DOI] [PubMed] [Google Scholar]
- 27.Zuckerman M. Vulnerability to psychopathology: A biosocial model. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- 28.Cann A, Calhoun LG, Tedeschi RG, et al. A short form of the Posttraumatic Growth Inventory. Anxiety Stress Coping. 2010;23(2):127–137. doi: 10.1080/10615800903094273. [DOI] [PubMed] [Google Scholar]
- 29.Stewart S, Fishbein MC, Snell GI, et al. Revision of the 1996 working formulation for the standardization of nomenclature in the diagnosis of lung rejection. J Heart Lung Transplant. 2007;26:1229–1242. doi: 10.1016/j.healun.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 30.Yousem SA, Berry GJ, Cagle PT, et al. Revision of the 1990 working formulation for the classification of pulmonary allograft rejection. Lung Rejection Study Group. J Heart Lung Transplant. 1996;15:1–15. [PubMed] [Google Scholar]
- 31.Estenne M, Maurer JR, Boehler A, et al. Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria. J Heart Lung Transplant. 2002;21:297–310. doi: 10.1016/s1053-2498(02)00398-4. [DOI] [PubMed] [Google Scholar]
- 32.DeVito Dabbs A, Kim Y, Vensak J, Studer S, Iacono A. Validation and refinement of the Questionnaire for Lung Transplant Patients. Prog Transplant. 2004;14(4):338–345. doi: 10.1177/152692480401400409. [DOI] [PubMed] [Google Scholar]
- 33.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey: Manual and interpretation guide. Boston: The Health Institute, New England Medical Center; 1993. [Google Scholar]
- 34.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4(3):219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 35.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19:2–21. [PubMed] [Google Scholar]
- 36.Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J Marriage Family. 1976;38:15–30. [Google Scholar]
- 37.Dew MA, Simmons RG, Roth LH, Schulberg HC, Thompson ME, Armitage JM, Griffith BP. Psychosocial predictors of vulnerability to distress in the year following heart transplantation. Psychological Med. 1994;24:929–945. doi: 10.1017/s0033291700029020. [DOI] [PubMed] [Google Scholar]
- 38.Dew MA, Kormos RL, DiMartini AF, et al. Prevalence and risk of depression and anxiety-related disorders during the first three years after heart transplantation. Psychosomatics. 2001;42:300–313. doi: 10.1176/appi.psy.42.4.300. [DOI] [PubMed] [Google Scholar]
- 39.Dew MA, Myaskovsky L, DiMartini AF, et al. Onset, timing and risk for depression and anxiety in family caregivers to heart transplant recipients. Psychological Med. 2004;34:1065–1082. doi: 10.1017/s0033291703001387. 53–55. [DOI] [PubMed] [Google Scholar]
- 40.Dew MA, Becker JT, Sanchez J, et al. Prevalence and predictors of depressive, anxiety, and substance use disorders in HIV-infected and uninfected men: A longitudinal evaluation. Psychological Med. 1997;27:395–409. doi: 10.1017/s0033291796004552. [DOI] [PubMed] [Google Scholar]
- 41.Dew MA, Ragni MV, Nimorwicz P. (1990). Infection with Human Immunodeficiency Virus and vulnerability to psychiatric distress: A study of men with hemophilia. Arch Gen Psychiatry. 1990;47:737–744. doi: 10.1001/archpsyc.1990.01810200045006. [DOI] [PubMed] [Google Scholar]
- 42.Rook KS. Investigating the positive and negative sides of personal relationships: Through a glass darkly? In: Spitzberg BH, Cupach WR, editors. The dark side of close relationships. Mahwah, NJ: Erlbaum; 1995. pp. 437–463. [Google Scholar]
- 43.Newsom JT, Nishishiba M, Morgan DL, Rook KS. The relative importance of three domains of positive and negative social exchanges: A longitudinal model with comparable measures. Psychol aging. 2003;18:746–754. doi: 10.1037/0882-7974.18.4.746. [DOI] [PubMed] [Google Scholar]
- 44.Taylor SE. Social support: A review. In: Friedman HS, editor. Oxford handbook of health psychology. New York: Oxford University Press; 2011. [Google Scholar]
- 45.Moos RH. Evaluating correctional and community settings. NY: Wiley; 1975. [Google Scholar]
- 46.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale NJ: Erlbaum; 1988. [Google Scholar]
- 47.Hemphill JF. Interpreting the magnitudes of correlation coefficients. Am Psychologist. 2003;58:78–79. doi: 10.1037/0003-066x.58.1.78. [DOI] [PubMed] [Google Scholar]
- 48.Tabachnick BG, Fidell LS. Using multivariate statistics. 5th edition. Needham Heights, MA: Pearson/Allyn & Bacon; 2007. [Google Scholar]
- 49.Rutherford RM, Fisher AJ, Hilton C, et al. Functional status and quality of life in patients surviving 10 years after lung transplantation. Am J Transplant. 2005;5:1099–1104. doi: 10.1111/j.1600-6143.2004.00803.x. [DOI] [PubMed] [Google Scholar]
- 50.Vermeulen KM, Ouwens JP, van der Bij W, et al. Long-term quality of life in patients surviving at least 55 months after lung transplantation. Gen Hosp Psychiatry. 2003;25:95–102. doi: 10.1016/s0163-8343(03)00007-0. [DOI] [PubMed] [Google Scholar]
- 51.Andrykowski MA, Bishop MM, Hahn EA, et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J Clin Oncol. 2005;23(3):599–608. doi: 10.1200/JCO.2005.03.189. [DOI] [PubMed] [Google Scholar]
- 52.Mols F, Vingerhoets AJ, Coebergh JW, van de Poll-Franse LV. Well-being, posttraumatic growth and benefit finding in long-term breast cancer survivors. Psychol Health. 2009;24(5):583–595. doi: 10.1080/08870440701671362. [DOI] [PubMed] [Google Scholar]
- 53.Widows MR, Jacobsen PB, Booth-Jones M, Fields KK. Predictors of posttraumatic growth following bone marrow transplantation for cancer. Health Psychol. 2005;24(3):266–273. doi: 10.1037/0278-6133.24.3.266. [DOI] [PubMed] [Google Scholar]
- 54.Evangelista LS, Doering L, Dracup K. Meaning and life purpose: The perspectives of post-transplant women. Heart Lung. 2003;32(4):250–257. doi: 10.1016/s0147-9563(03)00042-6. [DOI] [PubMed] [Google Scholar]
- 55.Thomsen D, Jensen BO. Patients' experiences of everyday life after lung transplantation. J Clin Nurs. 2009;18(24):3472–3479. doi: 10.1111/j.1365-2702.2009.02828.x. [DOI] [PubMed] [Google Scholar]
- 56.Yusen RD. Survival and quality of life of patients undergoing lung transplant. Clin Chest Med. 2011;32:253–264. doi: 10.1016/j.ccm.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 57.Cordova MJ, Giese-Davis J, Golant M, et al. Breast cancer as trauma: Posttraumatic stress and posttraumatic growth. J Clin Psychol Med Settings. 2007;14(4):308–319. [Google Scholar]
- 58.Tomich PL, Helgeson VS. Posttraumatic growth following cancer: Links to quality of life. J Trauma Stress. 2012;25(5):567–573. doi: 10.1002/jts.21738. [DOI] [PubMed] [Google Scholar]
- 59.Livermore N, Sharpe L, McKenzie D. Panic attacks and panic disorder in chronic obstructive pulmonary disease: A cognitive behavioral perspective. Respir Med. 2010;104(9):1246–1253. doi: 10.1016/j.rmed.2010.04.011. 2010. [DOI] [PubMed] [Google Scholar]
- 60.Katon WJ. Panic disorder. N Engl J Med. 2006;354:2360–2367. doi: 10.1056/NEJMcp052466. [DOI] [PubMed] [Google Scholar]
- 61.Bellizzi KM, Blank TO. Predicting posttraumatic growth in breast cancer survivors. Health Psychol. 2006;25:47–56. doi: 10.1037/0278-6133.25.1.47. [DOI] [PubMed] [Google Scholar]
- 62.Dunigan JT, Carr BI, Steel JL. Posttraumatic growth, immunity and survival in patients with hepatoma. Dig Dis Sci. 2007;52(9):2452–2459. doi: 10.1007/s10620-006-9477-6. [DOI] [PubMed] [Google Scholar]
- 63.Bower JE, Kemeny ME, Taylor SE, Fahey JL. Cognitive processing, discovery of meaning, CD4 decline, and AIDS-related mortality among bereaved HIV-seropositive men. J Consult Clin Psychol. 1998;66(6):979–986. doi: 10.1037//0022-006x.66.6.979. [DOI] [PubMed] [Google Scholar]