Abstract
In Asian populations, diabetes mellitus is increasing and has become an important health problem in recent decades. Cardiovascular disease (CVD) is one of the most important complications and the most common cause of death in diabetic patients. Among the risk factors of CVD, elevated low-density lipoprotein cholesterol has been a major concern. Studies suggested that serum triglyceride may also play a role in predicting CVD in patients with type 2 diabetes mellitus, but the association is still debated. In this review, we summarized published studies focusing on the relationship between serum triglyceride and CVD disease in Asian diabetic patients. Ten studies conducted in six different Asian countries (three from Hong Kong, two from Taiwan, tow from Japan, one from Indonesia, one from South India, and one from South Korea) were summarized and discussed. CVD was subdivided into coronary heart disease, stroke, and peripheral arterial disease. Of the ten studies analyzed, one focused on CVD, five on coronary heart disease, three on stroke, three on peripheral arterial disease, and one on mortality from CVD. Studies from Hong Kong, Taiwan, and Japan suggested that triglyceride is a significant and independent risk factor for coronary heart disease, but not a significant risk factor for stroke (studies conducted in Japan and South Korea) or peripheral arterial disease (studies conducted in Taiwan, Indonesia, and South India). Although serum triglyceride may be a significant risk factor for coronary heart disease in Asian diabetic patients, clinical trials evaluating whether lowering triglycerides using fibrates can reduce the risk of coronary heart disease in these patients need to be initiated.
Keywords: Asian populations, cardiovascular disease, coronary heart disease, fibrates, triglyceride, type 2 diabetes
Abbreviations: ACCORD - Action to Control Cardiovascular Risk in Diabetes; Apo C-III - apolipoprotein C3; CHD - coronary heart disease; CI - confidence interval; CVD - cardiovascular disease; FIELD - Fenofibrate Intervention and Event Lowering in Diabetes; HDL-C - high-density lipoprotein cholesterol; LDL - low-density lipoprotein; LDL-C - low-density lipoprotein cholesterol; NCEP-ATP III - National Cholesterol Education Program Adult Treatment Panel III; PAD - peripheral artery disease; sd-LDL-C - small-dense low-density lipoprotein cholesterol; T2DM - type 2 diabetes mellitus; TG - triglyceride; TRL - triglyceride-rich lipoprotein; VLDL - very low-density lipoprotein
1. Introduction
Type 2 diabetes mellitus (T2DM) is now a global health problem with more than 60% of global diabetes appearing in the Asian population [1]. According to the prediction of the International Diabetes Federation, the number of T2DM cases in Western Pacific and Southeast Asia will increase to more than 179,000,000 by 2025 [1]. In Western countries, cardiovascular disease (CVD), including coronary heart disease (CHD), cerebral vascular disease, and other peripheral arterial disease (PAD), is a major complication and cause of mortality in patients with diabetes. In Taiwan, diabetic patients suffer from an overall 63% higher risk of mortality than the general population, and CVD remains the major cause of death in these patients [2]. The incidence of type 2 diabetes has been on the rise over the past decades in Taiwan. The optimal cutoff value for body mass index in the development of common chronic diseases including diabetes, hypertension, and dyslipidemia in Taiwan is approximately 23 kg/m2. This is much lower than the currently recommended cutoff value of 30 kg/m2 for obesity defined by the World Health Organization [3, 4].
The prevalence of CVD in the Asian diabetes population was known to be lower than in Caucasians [5, 6]. In the early 1970s, renal failure and stroke were the leading causes of death in diabetic patients in China, Japan, and Pima India, compared with ischemic heart disease in Caucasian patients [6]. However, with continuing globalization, diet and lifestyle have changed rapidly in developing countries in Asia in recent decades [1]. In a report from the Asia Pacific Cohort Studies Collaboration, the relative effect of diabetes on the risks of CVD in Asian populations is about the same as for Caucasians [7]. In a recent questionnaire survey of 18,385 diabetics in Japan, the frequency of cause of death from CAD and cerebrovascular disease (10.2% and 9.8%, respectively) were similarly higher than from renal failure (6.8%) [8].
Dyslipidemia is a major risk factor for CVD [9]. In patients with T2DM, dyslipidemia is characterized by high serum triglyceride (TG), low high-density lipoprotein cholesterol (HDL-C), and increased small-dense low-density lipoprotein cholesterol (sd-LDL-C) [10]. Serum TG is considered a risk factor for CVD in the general population and in diabetic patients, especially for those with high non-HDL-C [11, 12]. Studies conducted in Taiwan have also suggested that triglyceride is associated with hypertension in patients with T2DM and may also be associated with the progression of albuminuria [13, 14]. Indeed, in the Asian population, hypertriglyceridemia may be more important than LDL-C as a risk factor for CVD in diabetic patients and non-diabetic patients [15-17]. In this article, we review the role of TG in CVD in patients with T2DM in Asian populations.
2. Literature search
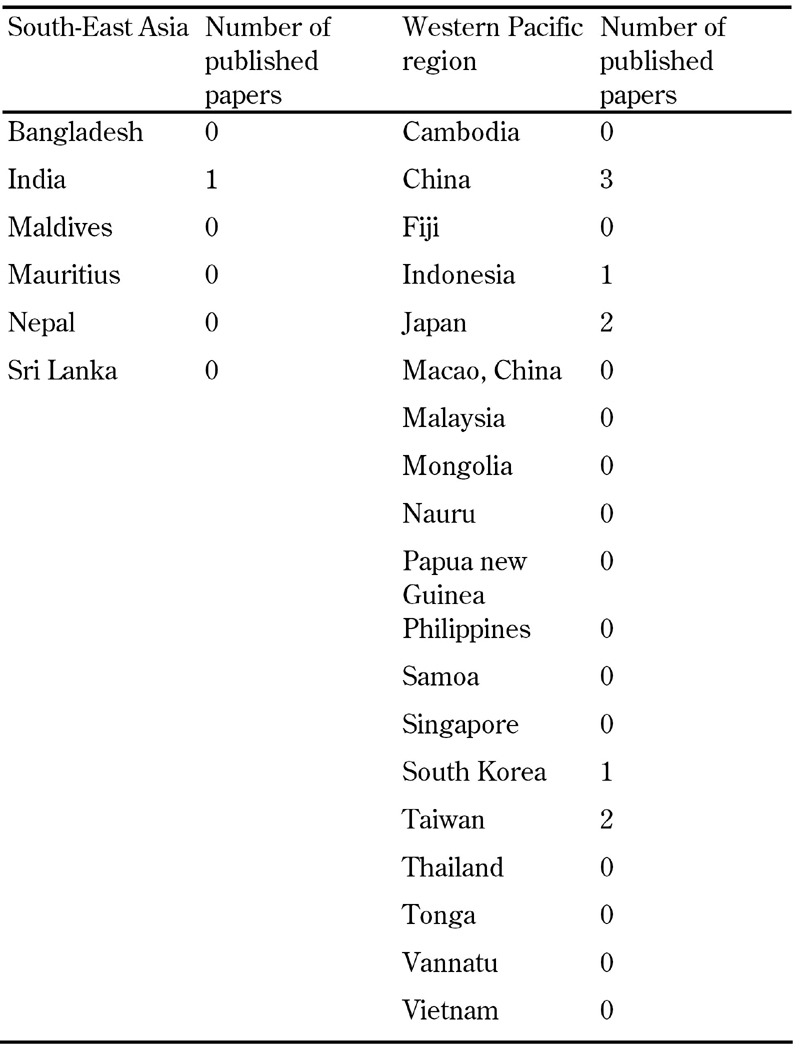
We searched MEDLINE (Ovid) using the terms "diabetes mellitus" or "type2 diabetes" and other relevant keywords, including "cardiovascular disease", "coronary heart disease", "stroke", "triglycerides", and "triacylglycerol". Separate queries were performed for the countries of the South-East Asian region and the Western Pacific region, as defined by the International Diabetes Federation (Table 1) [18, 19]. The South-East Asian region included Bangladesh, India, Maldives, Mauritius, Nepal, and Sri Lanka. The Western Pacific region included Australia, Cambodia, China, Fiji, Indonesia, Japan, Macao China, Malaysia, Mongolia, Nauru, New Zealand, Papua New Guinea, Philippines, Samoa, Singapore, South Korea, Taiwan, Thailand, Tonga, Vanuatu, and Vietnam. The queries were limited to English articles. The publication year was not limited. We excluded studies from Australia and New Zealand because these populations are largely Caucasian.
Table 1. Number of studies in different countries of the South-East Asian and the Western Pacific region (excluding Australia and New Zealand).
Publications on type 1 diabetes and studies simply comparing serum TG levels in controls and disease groups without multivariate analysis were also excluded. We abstracted the following information to a fixed protocol:
- Ethnicity
- Year of publication
- Name of the first author
- Recruitment period
- Follow-up duration
- Age
- Total case number
- Cardiovascular outcome
- Case number of cardiovascular outcome
- Average serum TG level in the disease group
- Hazard ratio
- Odds ratio or relative risk for total cholesterol, TG, HDL-C and LDL-C
- Variables adjusted in the modeling
3. Findings
We initially found 41 studies in fifteen different countries in the South-East Asian and Western Pacific regions. Among them, 14 studies were considered relevant to the topic. We further excluded 4 papers due to the lack of multivariate analysis [20-23]. As a result, a total of ten papers were included in the analysis, and the numbers of papers per country are shown in Table 1 (three from Hong Kong, two from Japan, two from Taiwan, one from South India, one from Indonesia, and one from South Korea). The abstracted data from the 10 studies are listed in Tables 2 and 3 according to the fixed protocol. In these ten studies, five focused on CHD, three on stroke, three on PAD, one on CVD, and one on CVD related mortality [15, 16, 24-31]. The findings on the association of TG and CVD are discussed as follows.
Table 2. Findings from clinical studies on the association between triglyceride and cardiovascular disease in Chinese patients with diabetes.
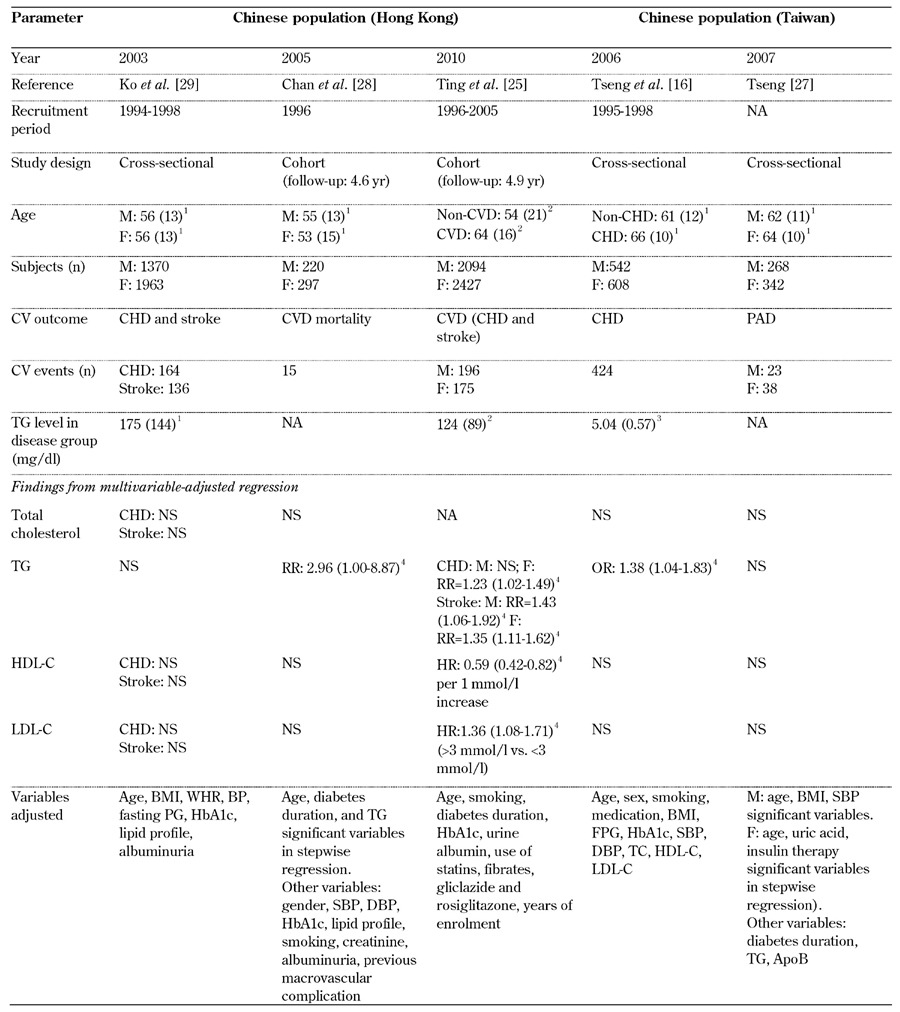
Legend: 1 Mean (standard deviation). 2 median (interquartile range). 3 Ln(TG) shown as mean (SD). 4 95% confidence interval. Abbreviations: BMI – body mass index, CHD – coronary heart disease, CVD – cardiovascular disease, DBP – diastolic blood pressure, F – female, FPG – fasting plasma glucose, HDL-C – high-density lipoprotein cholesterol, HR – hazard ratio, LDL-C – low-density lipoprotein cholesterol, M – male, NA – not available, NS – not significant, OR – odds ratio, PAD – peripheral arterial disease, RR – relative risk, SBP – systolic blood pressure, SD – standard deviation, TC – total cholesterol, TG – triglycerides. References [16, 25, 27-29].
Table 3. Findings from clinical studies on the association between triglyceride and cardiovascular disease in diabetic subjects from the Asian-Pacific region.
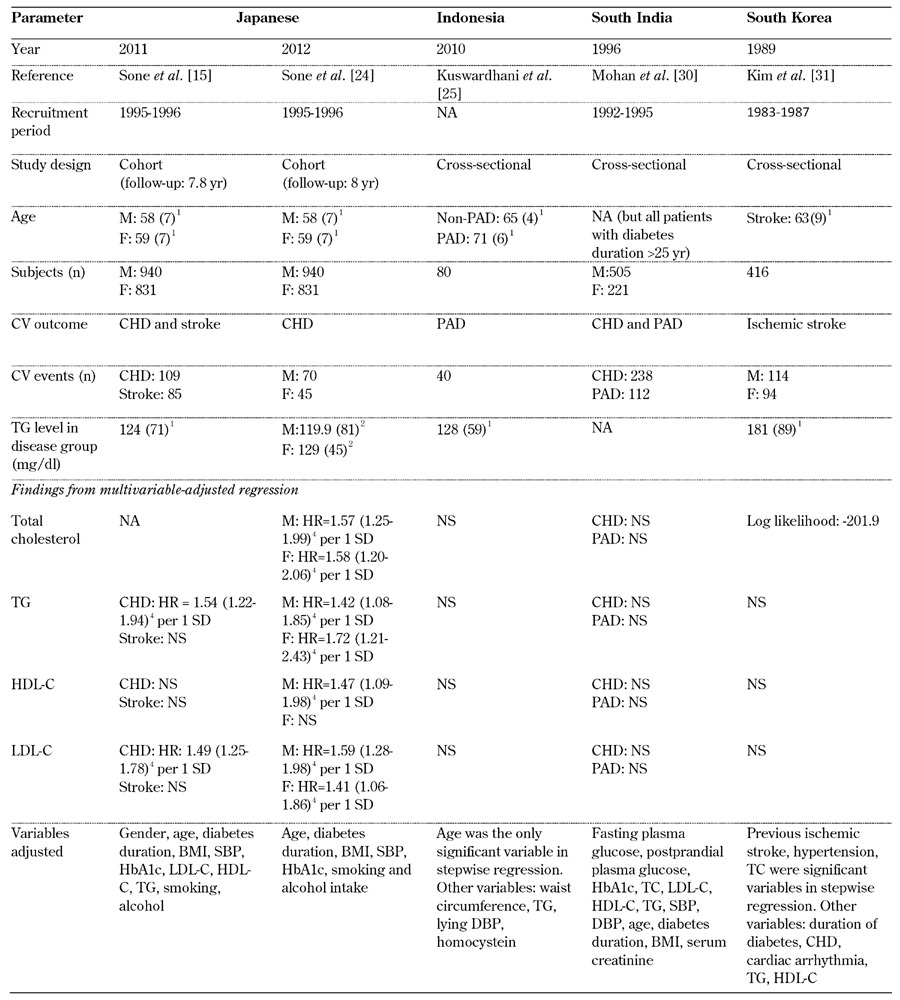
Legend: 1 Mean (standard deviation). 2 median (interquartile range). 3 Ln(TG) shown as mean (SD). 4 95% confidence interval. Abbreviations: BMI – body mass index, CHD – coronary heart disease, CVD – cardiovascular disease, DBP – diastolic blood pressure, F – female, FPG – fasting plasma glucose, HDL-C – high-density lipoprotein cholesterol, HR – hazard ratio, LDL-C – low-density lipoprotein cholesterol, M – male, NA – not available, NS – not significant, OR – odds ratio, PAD – peripheral arterial disease, RR – relative risk, SBP – systolic blood pressure, SD – standard deviation, TC – total cholesterol, TG – triglycerides. References [16, 25, 27-29].
3.1 Triglyceride and coronary heart disease
In four studies, increased serum TG level was an independent risk factor for CHD (Tables 2 and 3). TG appeared to play a more important role in the development of CHD than LDL-C, HDL-C, or total cholesterol [15, 16, 24, 29], and was more obvious in female than male patients in two studies [24, 29]. The only study that did not indicate a role for TG in CHD was conducted in South India [30]. This study recruited only subjects who had diabetes for more than 25 years. Therefore, the study had limitations, and the findings cannot be generalized as applicable to the average diabetic patient.
3.2 Triglyceride and stroke
In three studies referring to stroke, none of the following were found to be significant risk factors: total cholesterol, HDL-C, or LDL-C. As for TG, the results were equivocal. In one study in Hong Kong, the relative risk (95% confidence interval, CI) was 1.43 (1.06-1.92) in males and was 1.35 (1.11-1.62) in females (Table 2) [29]. However, in studies from Japanese and South Koreans, TG was not a significant risk factor for stroke [15, 31].
3.3 Triglyceride and peripheral arterial disease
For PAD, the conclusions were consistent. In studies conducted in Taiwan, Indonesia, and South India, neither total cholesterol, HDL-C, LDL-C, nor TG were associated with PAD in multivariate regression models (Tables 2 and 3) [26, 27, 30].
3.4 Triglyceride and cardiovascular disease
In a recent study in Hong Kong, low HDL-C, and high LDL-C were significant predictors for CVD (including CHD and stroke), but TG was not a significant risk factor [25]. In contrast, another study from Hong Kong showed that increased levels of TG were the only significant predictor for cardiovascular mortality [28].
4. Discussion
4.1 Triglyceride and cardiovascular disease in a non-diabetic population
Unlike LDL-C, which is well-established as a major predictor for CVD in global populations, the independent relationship of TG on predicting CVD has long been controversial [11]. Although some studies do not favor hypertriglyceridemia as an independent risk factor for CVD, two recent meta-analysis studies have suggested that TG is independently associated with myocardial infection, CHD, CVD and CVD death [12, 32-34]. There is one meta-analysis study focusing on the Asia Pacific region. This study analyzed the results from 25 cohort studies in six countries including Japan, China, Taiwan, Thailand, South Korea, and Singapore. The results supported serum TG as a better predictor than total cholesterol, HDL-C, and LDL-C for CHD mortality and CVD mortality [35]. Another Japanese cohort study also showed an independent relationship between hypertriglyceridemia and ischemic stroke and myocardial infarction [36]. In contrast to studies in Western populations, hypertriglyceridemia appeared to be more important than LDL-C for CVD in Asians.
4.2 Triglyceride and cardiovascular disease in diabetic patients
Hypertriglyceridemia, low HDL-C, and increased sd-LDL-C are typical presentations of dyslipidemia in patients with T2DM. The pathogenesis of hyperlipidemia is characterized by increased very low density lipoprotein (VLDL) production and defective removal of chylomicrons and its remnants [11]. In the United Kingdom Prospective Diabetes Study, LDL-C was the strongest predictor for CVD, and hypertriglyceridemia was not a predictor [37]. In contrast, in other case-control studies, the results were conflicting [9, 38, 39]. In one study, hypertriglyceridemia was an independent risk factor for CVD only in the high non-HDL-C group [12].
Since the pattern of dyslipidemia and its association with CVD may differ between diabetic and non-diabetic subjects, and studies conducted in Asian diabetic patients are rare, we reviewed the role of hypertriglyceridemia for CVD in diabetic patients in the South-East Asian and Western Pacific regions (excluding Australia and New Zealand). We found that the serum TG level is a major and independent risk factor for CHD in most studies except the one conducted in South India (Table 2). However, the results in the study from South India could not be applied to the general diabetic population because it recruited only patients who had diabetes for more than 25 years. In our review, serum LDL-C is not a predictor nor is it as good as TG for predicting CHD. The reason may be that the level of LDL-C cannot represent the amount of all real atherogenic lipoproteins in diabetic patients [40]. Besides, in studies from Japan and Hong Kong, the association between TG and CHD is stronger in female diabetics. The reason for such a gender difference has yet to be clarified. In patients with stroke, the role of TG is equivocal. Systolic blood pressure is a leading predictor of stroke in Western or Asian populations [15, 31, 41]. Thus, when compared with blood pressure, the influence of TG may be concealed.
PAD is common in diabetic patients [42-44]. In our review, hypertriglyceridemia was not an independent risk factor on PAD in multivariate analysis. However, the role of hypertriglyceridemia in the development of PAD remains controversial. In some case-control studies conducted in Asian, there were significant differences in the serum TG levels between disease and control groups [21, 22], although in another study conducted in Taiwanese diabetic patients, TG was not a significant risk factor for PAD, assessed by both univariate and multivariate analysis [43]. As a result, hypertriglyceridemia may not be a significant risk factor for PAD.
Two studies in Hong Kong focused on CVD events and CVD mortality, with contradictory results. In 2005, Chan et al. showed that hypertriglyceridemia is the only a predictor for cardiovascular mortality and the relative risk (95% CI) is 2.97 (1.00-8.77) (Table 2) [28]. In contrast, Ting et al. (2010) showed that low HDL-C and high LDL-C were risk factors for cardiovascular events, including ischemic heart disease and stroke, and that hypertriglyceridemia was not a significant predictor of CVD events and mortality (Table 2) [25]. However, in this study, CVD was not divide into subgroups. As we know, the prevalence of hemorrhagic stroke is higher in Asian populations and hypertension is a major risk factor leading to hemorrhagic stroke [45]. Therefore, the effect of TG may be attenuated in this population. Further exploration is needed to clarify the evolution of TG and LDL-C as risk factors for CVD in the Asian population.
4.3 Pathophysiology of triglyceride in cardiovascular disease
Currently, TG is considered a biomarker for CVD, although there is no strong evidence that TG can cause atherogenesis directly [46]. Hypertriglyceridemia is known to be associated with increased levels of prothrombotic factors, such as fibrinogen and plasminogen activator inhibitors, and is related to the size and density of the LDL particle [47, 48]. More importantly, hypertriglyceridemia is associated with some atherogenic remnant particles and apo C-III [46]. In addition to sd-LDL, triglyceride-rich lipoprotein (TRL), TRL remnant and apo C-III are also associated with atherosclerosis [11]. In subjects with insulin resistance, increased TG-rich VLDL and apo C-III formation from liver are observed, along with the excretion of TRL and a resulting decrease in its remnant. TRL remnant can pass through the endothelial cell and be taken up by macrophages, forming foam cells and leading to fatty streak formation. Furthermore, postprandial TRL has been shown to stimulate several proinflammatory genes, such as interleukin-6, intercellular adhesion molecule-1, etc. [49]. Apo C-III is a proinflammatory and proatherogenic protein. VLDL that have apo C-III can activate monocytes and endothelial cells to induce tumor necrosis factor-α, interleukin-1, nuclear factor-κB, etc. [50]. This may explain the findings that hypertriglyceridemia is a risk factor for CVD in diabetes.
4.4 Evidence of triglyceride control for preventing CVD in diabetes
According to the Adult Treatment Panel III of the National Cholesterol Education Program (NCEP ATP III), LDL-C is the primary target for dyslipidemia control in different cardiovascular risk categories. Although there is controversy in the practice of lowering TG for the prevention of CVD, NCEP ATP III recommends using non-HDL-C as a secondary treatment target for subjects having serum TG > 200 mg/dl [51]. Fibrates are useful for lowering hypertriglyceridemia. Currently, the FIELD (Fenofibrate Intervention and Event Lowering in Diabetes) and ACCORD (Action to Control Cardiovascular Risk in Diabetes) studies are both attempting to establish the role of TG lowering agents in primary prevention for CVD in diabetic patients [52, 53]. Both studies failed to demonstrate the lowering of CVD events by lowering TG. However, the subgroup analysis in the ACCORD study showed that fibrates were implicated in decreased CVD incidence in patients with TG ≥ 204 mg/dl and HDL-C ≤ 34 mg/dl [54].
In 2010, Jun et al. performed a meta-analysis including 18 trials, and reported a 10% relative risk reduction in major CVD events for subjects taking fibrates, especially in hypertriglyceridemia alone or in subjects with hypertriglyceridemia and low HDL-C [55]. The current consensus from the American Diabetes Association also favored the recommendation of the NCEP ATPIII to use non-HDL-C goals for patients with TG > 200 mg/dl [56]. In 2010, the Hong Kong Diabetes Registry reported a prospective study about fibrate use for preventing CHD. The hazard ratio was 0.34 with low significance [25]. Since hypertriglyceridemia is a major concern in Asian population, further explorations of the use of fibrates for lowering TG in Asian diabetic subjects are needed.
5. Limitations
There are several limitations in our review. First, the number of studies examining the relationship between TG and CVD in Asian populations is still small and studies from many countries such as Malaysia, Philippines, Thailand, Nepal, etc. are still lacking. Second, the authors in these studies used different statistical models adjusting for different sets of confounders; therefore comparisons are unreliable or inaccurate. The results may be influenced by choosing different confounders such as HDL-C, which is highly associated with TG [11]. Third, most studies did not take concomitant medical treatment such as statins or fibrates into consideration and could not demonstrate the influence of these lipid-lowering agents. Finally, many studies are cross-sectional, and the cause-effect relationship cannot be easily identified.
5. Conclusions
In Asian diabetic patients, the association between TG and CHD is strong, probably even stronger than LDL-C and CHD. For stroke and PAD, the role of hypertriglyceridemia is still controversial. Further studies with larger sample size and standard protocol are needed to clarify the role of TG in the development of CVD among Asian populations.
Disclosures: The authors report no conflict of interests.
Acknowledgments
The authors thank the Department of Health (DOH89-TD-1035; DOH97-TD-D-113-97009) and the National Science Council (NSC102-2314-B-002-067) of Taiwan for their continuous support of epidemiologic studies in diabetes.
References
- 1.Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, Hu FB. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301:2129–2140. doi: 10.1001/jama.2009.726. [DOI] [PubMed] [Google Scholar]
- 2.Tseng CH. Mortality and causes of death in a national sample of diabetic patients in Taiwan. Diabetes Care. 2004;27:1605–1609. doi: 10.2337/diacare.27.7.1605. [DOI] [PubMed] [Google Scholar]
- 3.Tseng CH, Tseng CP, Chong CK, Huang TP, Song YM, Chou CW, Lai SM, Tai TY, Cheng JC. Increasing incidence of diagnosed type 2 diabetes in Taiwan: analysis of data from a national cohort. Diabetologia. 2006;49:1755–1760. doi: 10.1007/s00125-006-0314-4. [DOI] [PubMed] [Google Scholar]
- 4.Tseng CH, Chong CK, Chan TT, Bai CH, You SL, Chiou HY, Su TC, Chen CJ. Optimal anthropometric factor cutoffs for hyperglycemia, hypertension and dyslipidemia for the Taiwanese population. Atherosclerosis. 2010;210:585–589. doi: 10.1016/j.atherosclerosis.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 5.Chi ZS, Lee ET, Lu M, Keen H, Bennett PH. Vascular disease prevalence in diabetic patients in China: standardised comparison with the 14 centres in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia. 2001;44(Suppl 2):S82–S86. doi: 10.1007/pl00002944. [DOI] [PubMed] [Google Scholar]
- 6.Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H. Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia. 2001;44(Suppl 2):S14–S21. doi: 10.1007/pl00002934. [DOI] [PubMed] [Google Scholar]
- 7.Woodward M, Zhang X, Barzi F, Pan W, Ueshima H, Rodgers A, MacMahon S. The effects of diabetes on the risks of major cardiovascular diseases and death in the Asia-Pacific region. Diabetes Care. 2003;26:360–366. doi: 10.2337/diacare.26.2.360. [DOI] [PubMed] [Google Scholar]
- 8.Hotta N, Nakamura J, Iwamoto Y, Ohno Y, Kasuga M, Kikkawa R, Toyota T. Causes of death in Japanese diabetics: A questionnaire survey of 18,385 diabetics over a 10-year period. J Diabetes Invest. 2010;1:66–76. doi: 10.1111/j.2040-1124.2010.00019.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arsenault BJ, Boekholdt SM, Kastelein JJ. Lipid parameters for measuring risk of cardiovascular disease. Nat Rev Cardiol. 2011;8:197–206. doi: 10.1038/nrcardio.2010.223. [DOI] [PubMed] [Google Scholar]
- 10.Mooradian AD. Dyslipidemia in type 2 diabetes mellitus. Nat Clin Pract Endocrinol Metab. 2009;5:150–159. doi: 10.1038/ncpendmet1066. [DOI] [PubMed] [Google Scholar]
- 11.Miller MM, Stone NJ, Vice C, Ballantyne CM, Bittner VM, Criqui MH, Ginsberg HN, Goldberg AC, Howard WJ. et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–2333. doi: 10.1161/CIR.0b013e3182160726. [DOI] [PubMed] [Google Scholar]
- 12.Bos G, Dekker JM, Nijpels G, de Vegt F, Diamant M, Stehouwer CD, Bouter LM, Heine RJ. A combination of high concentrations of serum triglyceride and non-high-density-lipoprotein-cholesterol is a risk factor for cardiovascular disease in subjects with abnormal glucose metabolism - The Hoorn Study. Diabetologia. 2003;46:910–916. doi: 10.1007/s00125-003-1141-5. [DOI] [PubMed] [Google Scholar]
- 13.Tseng CH, Tai TY. Correlating factors associated with hypertension among non-insulin-dependent diabetes - a cross-sectional study of an epidemiological cohort in Taipei City. Chinese J Family Med. 1991;1:53–62. [Google Scholar]
- 14.Tseng CH. Differential dyslipidemia associated with albuminuria in type 2 diabetic patients in Taiwan. Clin Biochem. 2009;42:1019–1024. doi: 10.1016/j.clinbiochem.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Sone H, Tanaka S, Tanaka S, Iimuro S, Oida K, Yamasaki Y, Oikawa S, Ishibashi S, Katayama S, Ohashi Y. et al. Serum level of triglycerides is a potent risk factor comparable to LDL cholesterol for coronary heart disease in Japanese patients with type 2 diabetes: subanalysis of the Japan Diabetes Complications Study (JDCS) J Clin Endocrinol Metab. 2011;96:3448–3456. doi: 10.1210/jc.2011-0622. [DOI] [PubMed] [Google Scholar]
- 16.Tseng CH, Tseng CP, Chong CK, Cheng JC, Tai TY. Independent association between triglycerides and coronary artery disease in Taiwanese type 2 diabetic patients. Int J Cardiol. 2006;111:80–85. doi: 10.1016/j.ijcard.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 17.Iso H, Naito Y, Sato S, Kitamura A, Okamura T, Sankai T, Shimamoto T, Iida M, Komachi Y. Serum triglycerides and risk of coronary heart disease among Japanese men and women. Am J Epidemiol. 2001;153:490–499. doi: 10.1093/aje/153.5.490. [DOI] [PubMed] [Google Scholar]
- 18.member associations in Western Pacific area. International diabetes federation; http://www.idf.org/member-associations/WP. Accessed on November 21, 2012. [Google Scholar]
- 19.member associations in Western Pacific area. International diabetes federation; http://www.idf.org/member-associations/SEA. Accessed on November 21, 2012. [Google Scholar]
- 20.Sasaki A, Horiuchi N, Hasegawa K, Uehara M. Mortality from coronary heart disease and cerebrovascular disease and associated risk factors in diabetic patients in Osaka District, Japan. Diabet Res Clin Pract. 1995;27:77–83. doi: 10.1016/0168-8227(94)01018-u. [DOI] [PubMed] [Google Scholar]
- 21.Thomas GN, Critchley JA, Tomlinson B, Cockram CS, Chan JC. Peripheral vascular disease in Type 2 diabetic Chinese patients: associations with metabolic indices, concomitant vascular disease and genetic factors. Diabet Med. 2003;20:988–995. doi: 10.1046/j.1464-5491.2003.01046.x. [DOI] [PubMed] [Google Scholar]
- 22.Rhee SY, Guan H, Liu ZM, Cheng SW, Waspadji S, Palmes P, Tai TY, Suwanwalaikorn S, Kim YS, Group P. Multi-country study on the prevalence and clinical features of peripheral arterial disease in Asian type 2 diabetes patients at high risk of atherosclerosis. Diabetes Res Clin Pract. 2007;76:82–92. doi: 10.1016/j.diabres.2006.07.029. [DOI] [PubMed] [Google Scholar]
- 23.Sone H, Tanaka S, Ishibashi S, Yamasaki Y, Oikawa S, Ito H, Saito Y, Ohashi Y, Akanuma Y, Yamada N. et al. The new worldwide definition of metabolic syndrome is not a better diagnostic predictor of cardiovascular disease in Japanese diabetic patients than the existing definitions: additional analysis from the Japan Diabetes Complications Study. Diabetes Care. 2006;29:145–147. doi: 10.2337/diacare.29.1.145. [DOI] [PubMed] [Google Scholar]
- 24.Sone H, Tanaka S, Tanaka S, Iimuro S, Ishibashi S, Oikawa S, Shimano H, Katayama S, Ohashi Y, Akanuma Y. et al. Comparison of various lipid variables as predictors of coronary heart disease in Japanese men and women with type 2 diabetes: subanalysis of the Japan Diabetes Complications Study. Diabetes Care. 2012;35:1150–1157. doi: 10.2337/dc11-1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ting RZ, Yang X, Yu LW, Luk AO, Kong AP, Tong PC, So WY, Chan JC, Ma RC. Lipid control and use of lipid-regulating drugs for prevention of cardiovascular events in Chinese type 2 diabetic patients: a prospective cohort study. Cardiovasc Diabetol. 2010;9:77. doi: 10.1186/1475-2840-9-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuswardhani RA, Suastika K. Age and homocystein were risk factor for peripheral arterial disease in elderly with type 2 diabetes mellitus. Acta Medica Indonesiana. 2010;42:94–99. [PubMed] [Google Scholar]
- 27.Tseng CH. Sex difference in the distribution of atherosclerotic risk factors and their association with peripheral arterial disease in Taiwanese type 2 diabetic patients. Circ J. 2007;71:1131–1136. doi: 10.1253/circj.71.1131. [DOI] [PubMed] [Google Scholar]
- 28.Chan WB, Tong PC, Chow CC, So WY, Ng MC, Ma RC, Osaki R, Cockram CS, Chan JC. Triglyceride predicts cardiovascular mortality and its relationship with glycaemia and obesity in Chinese type 2 diabetic patients. Diabetes Metab Res Rev. 2005;21:183–188. doi: 10.1002/dmrr.497. [DOI] [PubMed] [Google Scholar]
- 29.Ko GT, Chan JC, Chow CC, Yeung VT, Chan WB, So WY, Ma RC, Ozaki R, Cockram CS. Triglyceride, albuminuria and blood pressure are the major associations of non-fatal cardiovascular disease in Chinese type 2 diabetes. Acta Diabetol. 2003;40:80–84. doi: 10.1007/s005920300009. [DOI] [PubMed] [Google Scholar]
- 30.Mohan V, Vijayaprabha R, Rema M. Vascular complications in long-term south Indian NIDDM of over 25 years’ duration. Diabetes Res Clin Pract. 1996;31:133–140. doi: 10.1016/0168-8227(96)01215-6. [DOI] [PubMed] [Google Scholar]
- 31.Kim JS, Sunwoo IN. Risk factors of ischemic brain stroke in Korean diabetic patients - a retrospective study. Yonsei Med J. 1989;30:288–293. doi: 10.3349/ymj.1989.30.3.288. [DOI] [PubMed] [Google Scholar]
- 32.Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, Thompson A, Wood AM, Lewington S, Sattar N, Packard CJ. et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302:1993–2000. doi: 10.1001/jama.2009.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murad MH, Hazem A, Coto-Yglesias F, Dzyubak S, Gupta S, Bancos I, Lane MA, Erwin PJ, Berglund L, Elraiyah T. et al. The association of hypertriglyceridemia with cardiovascular events and pancreatitis: a systematic review and meta-analysis. BMC Endocr Disord. 2012;12:2. doi: 10.1186/1472-6823-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, Boekholdt SM, Khaw KT, Gudnason V. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007;115:450–458. doi: 10.1161/CIRCULATIONAHA.106.637793. [DOI] [PubMed] [Google Scholar]
- 35.Barzi F, Patel A, Woodward M, Lawes CM, Ohkubo T, Gu D, Lam TH, Ueshima H. A comparison of lipid variables as predictors of cardiovascular disease in the Asia Pacific region. Ann Epidemiol. 2005;15:405–413. doi: 10.1016/j.annepidem.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 36.Okamura T, Kokubo Y, Watanabe M, Higashiyama A, Ono Y, Miyamoto Y, Yoshimasa Y, Okayama A. Triglycerides and non-high-density lipoprotein cholesterol and the incidence of cardiovascular disease in an urban Japanese cohort: the Suita study. Atherosclerosis. 2010;209:290–294. doi: 10.1016/j.atherosclerosis.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 37.Turner RC, Millns H, Neil HA, Stratton IM, Manley SE, Matthews DR, Holman RR. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23) BMJ. 1998;316:823–828. doi: 10.1136/bmj.316.7134.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fontbonne A, Eschwege E, Cambien F, Richard JL, Ducimetiere P, Thibult N, Warnet JM, Claude JR, Rosselin GE. Hypertriglyceridaemia as a risk factor of coronary heart disease mortality in subjects with impaired glucose tolerance or diabetes. Results from the 11-year follow-up of the Paris Prospective Study. Diabetologia. 1989;32:300–304. doi: 10.1007/BF00265546. [DOI] [PubMed] [Google Scholar]
- 39.Tohidi M, Hatami M, Hadaegh F, Safarkhani M, Harati H, Azizi F. Lipid measures for prediction of incident cardiovascular disease in diabetic and non-diabetic adults: results of the 8.6 years follow-up of a population based cohort study. Lipids Health Dis. 2010;9:6. doi: 10.1186/1476-511X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chan JC, Chan SP, Deerochanawong C, Go RT, Lee KO, Ma RC, Pan CY, Sheu WH, Barter P. Diabetic dyslipidaemia in Asian populations in the Western Pacific Region: what we know and don't know. Diabetes Res Clin Pract. 2011;94:1–13. doi: 10.1016/j.diabres.2011.05.034. [DOI] [PubMed] [Google Scholar]
- 41.Mulnier HE, Seaman HE, Raleigh VS, Soedamah-Muthu SS, Colhoun HM, Lawrenson RA, De Vries CS. Risk of stroke in people with type 2 diabetes in the UK: a study using the General Practice Research Database. Diabetologia. 2006;49:2859–2865. doi: 10.1007/s00125-006-0493-z. [DOI] [PubMed] [Google Scholar]
- 42.Tseng CH. Lipoprotein(a) is an independent risk factor for peripheral arterial disease in Chinese type 2 diabetic patients in Taiwan. Diabetes Care. 2004;27:517–521. doi: 10.2337/diacare.27.2.517. [DOI] [PubMed] [Google Scholar]
- 43.Tseng CH. Prevalence and risk factors of peripheral arterial obstructive disease in Taiwanese type 2 diabetic patients. Angiology. 2003;54:331–338. doi: 10.1177/000331970305400309. [DOI] [PubMed] [Google Scholar]
- 44.Tseng CH. Independent association of uric acid levels with peripheral arterial disease in Taiwanese patients with Type 2 diabetes. Diabet Med. 2004;21:724–729. doi: 10.1111/j.1464-5491.2004.01239.x. [DOI] [PubMed] [Google Scholar]
- 45.Jia Q, Liu LP, Wang YJ. Stroke in China. Clin Exp Pharmacol Physiol. 2010;37:259–264. doi: 10.1111/j.1440-1681.2009.05290.x. [DOI] [PubMed] [Google Scholar]
- 46.Talayero BG, Sacks FM. The role of triglycerides in atherosclerosis. Curr Cardiol Rep. 2011;13:544–552. doi: 10.1007/s11886-011-0220-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Georgieva AM, Cate HT, Keulen ET, van Oerle R, Govers-Riemslag JW, Hamulyak K, van der Kallen CJ, Van Greevenbroek MM, De Bruin TW. Prothrombotic markers in familial combined hyperlipidemia: evidence of endothelial cell activation and relation to metabolic syndrome. Atherosclerosis. 2004;175:345–351. doi: 10.1016/j.atherosclerosis.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 48.Koba S, Hirano T, Yoshino G, Sakai K, Sakaue T, Adachi M, Katagiri T. Remarkably high prevalence of small dense low-density lipoprotein in Japanese men with coronary artery disease, irrespective of the presence of diabetes. Atherosclerosis. 2002;160:249–256. doi: 10.1016/s0021-9150(01)00580-9. [DOI] [PubMed] [Google Scholar]
- 49.Norata GD, Grigore L, Raselli S, Redaelli L, Hamsten A, Maggi F, Eriksson P, Catapano AL. Post-prandial endothelial dysfunction in hypertriglyceridemic subjects: molecular mechanisms and gene expression studies. Atherosclerosis. 2007;193:321–327. doi: 10.1016/j.atherosclerosis.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 50.Kawakami A, Aikawa M, Alcaide P, Luscinskas FW, Libby P, Sacks FM. Apolipoprotein CIII induces expression of vascular cell adhesion molecule-1 in vascular endothelial cells and increases adhesion of monocytic cells. Circulation. 2006;114:681–687. doi: 10.1161/CIRCULATIONAHA.106.622514. [DOI] [PubMed] [Google Scholar]
- 51.Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC Jr, Stone NJ. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 52.Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, Forder P, Pillai A, Davis T, Glasziou P. et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet. 2005;366:1849–1861. doi: 10.1016/S0140-6736(05)67667-2. [DOI] [PubMed] [Google Scholar]
- 53.Ginsberg HN, Elam MB, Lovato LC, Crouse JR 3rd, Leiter LA, Linz P, Friedewald WT, Buse JB, Gerstein HC, Probstfield J. et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010;362:1563–1574. doi: 10.1056/NEJMoa1001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Saely CH, Rein P, Drexel H. Combination lipid therapy in type 2 diabetes. N Engl J Med. 2010;363:692. doi: 10.1056/NEJMc1006407. [DOI] [PubMed] [Google Scholar]
- 55.Jun M, Foote C, Lv J, Neal B, Patel A, Nicholls SJ, Grobbee DE, Cass A, Chalmers J, Perkovic V. Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet. 2010;375:1875–1884. doi: 10.1016/S0140-6736(10)60656-3. [DOI] [PubMed] [Google Scholar]
- 56.Brunzell JD, Davidson M, Furberg CD, Goldberg RB, Howard BV, Stein JH, Witztum JL. Lipoprotein management in patients with cardiometabolic risk: consensus statement from the American Diabetes Association and the American College of Cardiology Foundation. Diabetes Care. 2008;31:811–822. doi: 10.2337/dc08-9018. [DOI] [PubMed] [Google Scholar]


