Abstract
Background:
Multidrug resistance Pseudomonas aeruginosa (MDR-P. aeruginosa) is a worldwide threat for public health. Hyperexpression of efflux pump systems (MexAB-OprM and MexCD-OprJ), which is a well-known mechanisms for MDR emerging, is controlled by regulatory genes, mexR and nfxB, respectively. The aim of this study was to evaluate point mutations in mexR and nfxB genes in MDR- P. aeruginosa isolated from wound infections.
Materials and Methods:
A total of 34 P. aeruginosa cultures obtained from wound infections were analyzed. Among them eight isolates identified as MDR-P. aeruginosa and were subjected to determination of mutations in mexR and nfxB genes.
Results:
We detected eight-point mutations in mexR and 12-point mutations in nfxB. The most common mutations were common G327-A (eight isolates), G384-A (eight isolates), G411-A (eight isolates). Mutations in A371-C and A372-C were the predominant substitution which was seen in nfxB. Amino acid substitutions were also found at position 124 and 126 for NfxB and MexR, respectively.
Conclusions:
P. aeruginosa isolates with mutation in efflux pump regulatory genes such as mexR and nfxB could be a main factor contributed to antibiotic resistance and must be considered in antibiotic treatment.
Keywords: Efflux pump, mexR, nfxB, Pseudomonas aeruginosa
INTRODUCTION
Pseudomonas aeruginosa, which is known as a nonfermentative gram negative opportunistic pathogen, is the leading cause of diverse infections including pneumonia, wound and urinary tract infection (UTI).[1] Because of resistance to many antibiotics, treatment of infections caused by P. aeruginosa is difficult.[2] Several mechanisms have been known for antibiotic resistance, for example, inactivation or modification of the antibiotic, alteration, or modification in the target site of the antibiotic, and decreased intracellular drug concentration by overexpression of efflux pump.[3] Until recently, in P. aeruginosa five super family of efflux pumps including (i) the ATP-binding cassette (ABC) family, (ii) the small multidrug resistance family, (iii) the major facilitator super family, (iv) the resistance-nodulation-division (RND) family, and (v) the multidrug and toxic compound extrusion family have been recognized.[4] Analysis of P. aeruginosa genome showed that all five super families are presented but RND family is predominant.[5] RND pumps consist of three subunit including membrane fusion protein (MFP), an outer membrane factor (OMF), and a cytoplasmic membrane transporter.[5,6] MexAB-OprM and MexCD-OprJ, which are members of RND efflux pumps family, have the wide substrate of antibiotics such as, β-lactam class (aztreonam, ceftazidime) and fluoroquinolones.[7] Active efflux pumps decrease intracellular concentration of drug by pumping it to out. Expression of MexAB-OprM and MexCD-OprJ are regulated by mexR and nfxB, respectively.[7,8,9] MexR consisting of 147 amino acid residues, negatively regulate MexAB-OprM expression.[8] Mutation in mexR (nalB strains) and nfxB compromised regulatory functions and therefore resulting in efflux pumps hyperexpression.[8,9] Several independent studies have revealed that overexpression of mentioned efflux pumps contributed to multi-drug resistance (MDR) phenotype.[10,11,12] MDR P. aeruginosa is defined as resistance to at least three antibiotics belonged to different classes especially, carbapenems, fluoroquinolones, and aminoglycosides.[13] Due to limited choice of effective drug, mortality rates in patients infected with MDR P. aeruginosa is higher in comparison with multiple drugs susceptible P. aeruginosa.[14,15] Therefore, in order to have appropriate therapy for patients infected with P. aeruginosa, identification of multidrug resistance isolates is essential. In this study, our aim was to detect mexR and nfxB mutations in MDR- P. aeruginosa isolated from wound infections.
MATERIALS AND METHODS
Sample collection and identification
This study was conducted between January 2013 and march 2013 at three major hospitals of Isfahan, Iran. During the study, a total of 100 wound samples that were obtained from wound infections were analyzed. P. aeruginosa identification performed based on standard test such as Gram staining, catalase, oxidase, oxidative-fermentative (OF) test, pigment production, and growth at 42°C.[1,16] Subsequently, primary identification confirmed with PCR by using ITS (16s-23s rRNA internal transcribed spacer) gene specific primer.[17]
Antibiotic susceptibility testing
Antibiotic susceptibility of the isolates was ascertained by Kirby-Bauer disk diffusion method according to CLSI (clinical laboratory standard institute) guidelines.[18] In this study, following antibiotic disks (MAST, UK) were used: ceftazidime (30 μg), cefotaxime (30 μg) aztreonam (30 μg), ciprofloxacin (5 μg), imipenem (10 μg), meropenem (10 μg), and amikacin (30 μg). P. aeruginosa ATCC 27853 was used for quality control.
Preparation of genomic DNA
For DNA extraction, two or three colony of fresh culture of P. aeruginosa was dissolved in 300 ml of lysis buffer containing (Tris 100 mmol, Nacl 50 mmol, and EDTA 25 mmol, pH = 7.5) completely. Subsequently, suspension was boiled at 95°C for 15 min. Equal volumes of phenol and chloroform (25:24, pH = 7.5) was added, mixed thoroughly, and centrifuged at 9000 g for 5 min. Aqueous–viscous supernatant was transformed to a fresh micro tube, phenol/chloroform (25:24) was added again and centrifuged at 9000 g for 5 min. To DNA precipitation, 600 μl of cold pure ethanol (Merck, Germany) was added and centrifuged at 13000 g (4°C, 20 min). Obtained DNA after washing with 70% ethanol was stored at –20°C.
mexR and nfxB amplifications and sequencing
PCR for mexR (503bp) and nfxB (731 bp) amplification were carried out in separate 25 μl reaction mixture consist of 10 pmol of each primer (Metabion, Germany), mexR-F (5′-CTGGATCAACCACATTTACA -3′), mexR-R (5′-CTTCGAAAAGAATGTTCTTAAA-3′), nfxB -F (5′-ACGCGAGGCCAGTTTTCT-3′) and nfxB-R (5′-ACTGATCTTCCCGAGTGTCG-3′), 2.5 μl (25 mMol Mgcl2), 200 μM dNTP, 2.5 μl PCR buffer 10X, 1.25 u taq DNApol (Cinna gen, Iran), and 5 μl DNA template.[19,20] Cycling condition performed in 35 cycles including, denaturation at 95°C for 1 min, annealing at 55°C for mexR and 60°C for nfxB, 45 s, extension at 72°C for 1 min and final extension at 72°C for 10 min. PCR products were visualized on 1.5% agarose gel stained with DNA green viewer dye [Figures 1 and 2]. PCR products were sent for BIO NEER (Korea) company for purification and sequencing on both strands. We used Mega4 as multiple sequence alignment software for sequences analyzing.
Figure 1.

Gel image of representative PCR of mexR gene. Line1 Ladder, Lane 2 negative control, line 3 positive, line 4 to 10 clinical specimens
Figure 2.
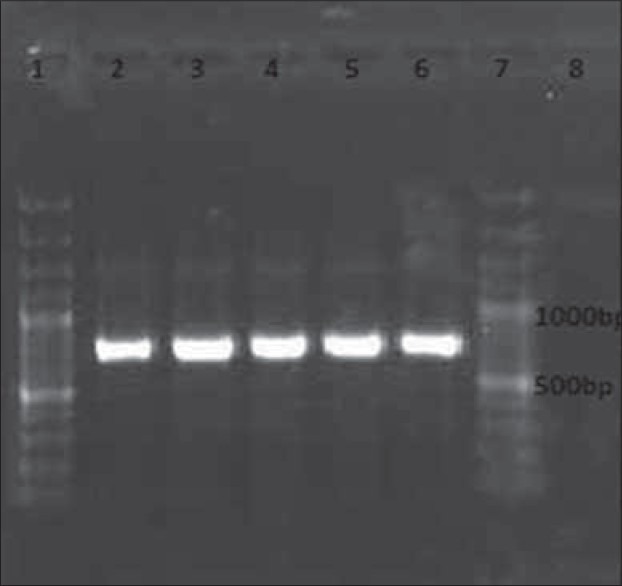
Gel image of representative PCR of nfxB gene. Line1, 7 Ladder, Lane 2 positivecontrol, line 3 to 6 clinical specimens, line 8 negative control
RESULTS
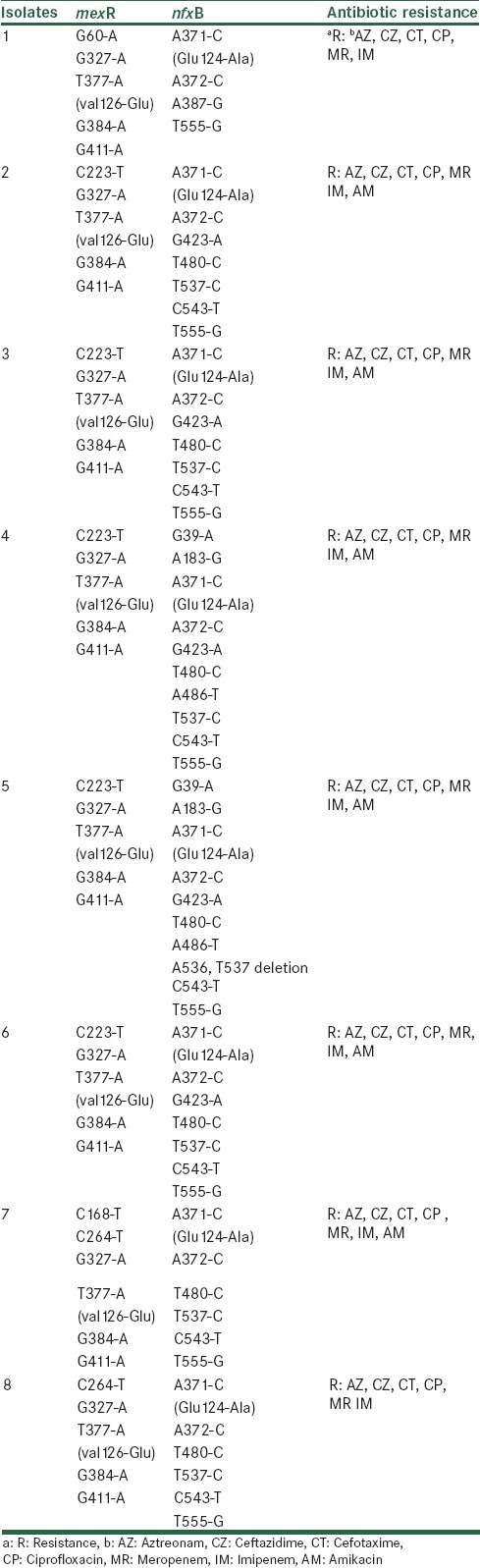
Eight of 34 nonrepetitive P. aeruginosa were identified as MDR-P. aeruginosa. All isolates showed resistance to ceftazidime, cefotaxime, aztreonam, ciprofloxacin, imipenem, and meropenem. Our results showed seven silent mutations including G327-A (eight isolates), G384-A (eight isolates), G411-A (eight isolates), C223-T (five isolates), C264-T (two isolates), G60-A (one isolate), C168-T (one isolate) in mexR gene. Only one missense mutation which changed val 126 to Glu was seen [Table 1]. Four isolates had five different point mutations simultaneously [Table 1]. In nfxB, 12-point mutations were found. Mutations at position A371-C and A372-C were the predominant substitution. We also found missense mutations in codon 124 that changed Glu to Ala [Table 1]. The GenBank accession numbers of mexR and nfxB which determined in this work are as follow: KF675781-88.
Table 1.
Mutations in mexR, nfxB in MDR-Pseudomonas aeruginosa isolated from wound infections
DISCUSSION
Resistance to multiple antibiotics in P. aeruginosa as one of the most common etiological agents of wound infections is well-known property.[21] Treatment of MDR-P. aeruginosa is difficult due to limited choice of antibiotics.[22] Generally, antibiotic resistance mechanism in P. aeruginosa is divided into two categories, intrinsic and acquired resistance. Low permeability of outer membrane protein, constitutive expression of AmpC and efflux pumps is example of intrinsic resistance mechanism.[23,24,25] MexAB-OprM and MexCD-OprJ are two preponderant efflux pumps that contribute to intrinsic resistance of P. aeruginosa to different antibiotics.[3] MexAB-OprM and MexCD-OprJ are negatively regulated by MexR and NfxB, respectively; hence, mutations in these regulatory genes lead to overexpression of mentioned efflux pumps and multiple drug resistance emerging.[19,26] In our study mutations of mexR and nfxB in MDR-P. aeruginosa isolated from wound infections were investigated. In mexR, 8-point mutations were detected, seven of them were silent. Only the mutation in thymine 377 and conversion to adenine leads to substitution of Val with Glu in codon 126. This substitution had related to antibiotic resistance, according to similar studies.[19,27,28] Results of several independent studies revealed different mutations, for example, Suman and colleagues reported 24 silent and four missense mutations in 14 clinical isolates of P. aeruginosa.[29] Different amino acids substitution with relation to antibiotic resistance was seen in codon 21, 95, 30, 79, 106, 114, 78, 107, 53, and 103 of mexR gene.[10,12,29,30] Although mutation in mexR is one of the main cause of MexAB-OprM overexpression but its expression and DNA binding activity in order to prediction of antibiotic effectiveness should be evaluated. Based on our results, mutations in nfxB were relatively high. The nfxB mutations consisted of 11 silent mutations, one missense mutation and a deletion from position 536 to 537. Mutations in position 371 and 372 were the most frequently replacement in all isolates [Table 1]. Analysis of NfxB showed that DNA binding domain is located between amino acid residues 26 and 42.[12] There was not any mutation mentioned region in this study. Missense mutation was seen in Glu 124-Ala of NfxB. Similar study revealed that change in codon 124 was related to ciprofloxacin resistance.[12] Results of another study of Fluoroquinolone resistance P. aeruginosa showed that mutation in codon 82 (Arg to Leu) was the most frequently substitution in nfxB.[31] Hyperexpression of efflux pumps such as MexAB-OprM and MexCD-OprJ are complicated. Isolates of nalC and nalD mutants had mutations in PA-3721 and PA-3574 genes showed overexpression of MexAB-OprM independent from mexR mutations.[32,33] Therefore, expression of MexAB-OprM is not only regulated by MexR but also affected by PA-3721 and PA-3574 genes. In order to know preponderant mutations, further study for evaluation of expression mexB, mexC, oprM and oprJ by realtime PCR is necessary.
ACKNOWLEDGMENT
The authors would like to express their thank to Mr. Sedighi, Mr. Shokri and Mrs. Beigi for their excellent assistance. This research was supported by Isfahan University of Medical Science, Grant No. 392063.
Footnotes
Source of Support: Isfahan University of Medical Science
Conflict of Interest: None declared.
REFERENCES
- 1.Forbes BA, Sahm DF, Weissfeld AS. 12th ed. USA: Elsevier; 2007. Bailey and Scott's Diagnostic Microbiology; pp. 340–350. [Google Scholar]
- 2.Strateva T, Yordanov D. Pseudomonas aeruginosa: A phenomenon of bacterial resistance. J Med Microbiol. 2009;58:1133–48. doi: 10.1099/jmm.0.009142-0. [DOI] [PubMed] [Google Scholar]
- 3.Lister PD, Wolter DG, Hanson ND. Antibacterial-resistant Pseudomonas aeruginosa: Clinical impact and complex regulation of chromosomally encoded resistance mechanisms. Clin Microbiol Rev. 2009;22:582–610. doi: 10.1128/CMR.00040-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schweizer HP. Efflux as mechanism of resistance to antimicrobials in Pseudomonas aeruginosa and related bacteria: Unanswered questions. Genet Mol Res. 2003;2:48–62. [PubMed] [Google Scholar]
- 5.Alekshun MN, Levy SB. Molecular mechanisms of antibacterial multidrug resistance. Cell. 2007;128:1037–150. doi: 10.1016/j.cell.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Ozer B, Duran N, Onlen Y, Savas L. Efflux pump genes and antimicrobial resistance of Pseudomonas aeruginosa strains isolated from lower respiratory tract infections acquired in an intensive care unit. J Antibiot (Tokyo) 2012;65:9–13. doi: 10.1038/ja.2011.102. [DOI] [PubMed] [Google Scholar]
- 7.Llanes L, Hocquet D, Vogne C, Baitich DB, Neuwirth C, Plesiat P. Clinical strains of Pseudomonas aeruginosa overproducing MexAB-OprM and MexXY efflux pumps simultaneously. Antimicrob Agents Chemother. 2004;48:1797–802. doi: 10.1128/AAC.48.5.1797-1802.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poole K, Tetro K, Zhao Q, Neshat S, Heinrichs DE, Bianco N. Expression of the multidrug resistance operon mexA-mexBoprMin Pseudomonas aeruginosa: mexR encodes a regulator of operon expression. Antimicrob Agents Chemother. 1996;40:2021–8. doi: 10.1128/aac.40.9.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeannot K, Elsen S, Kohler T, Delden CV, Plesiat P. Resistance and virulence of Pseudomonas aeruginosa clinical strains overproducing the MexCD-OprJ efflux pump. Antimicrob Agents Chemother. 2008;52:2455–62. doi: 10.1128/AAC.01107-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adewoye L, Sutherland A, Srikumar R, Poole K. The MexR repressor of the mexAB-oprM multidrug efflux operon in Pseudomonas aeruginosa: Characterization of mutations compromising activity. J Bacteriol. 2002;184:4308–12. doi: 10.1128/JB.184.15.4308-4312.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dumas JL, Delden CV, Perron K, Kohler T. Analysisofantibiotic resistance gene expression in Pseudomonas aeruginosa by quantitative real-time-PCR. FEMS Microbiol Lett. 2006;254:217–25. doi: 10.1111/j.1574-6968.2005.00008.x. [DOI] [PubMed] [Google Scholar]
- 12.Higgins PG, Fluit AC, Milatovic D, Verhoef J, Schmitz FJ. Mutations in GyrA, ParC, MexR and NfxB in clinical isolates Pseudomonas aeruginosa. Int J Antimicrob Agents. 2003;21:409–13. doi: 10.1016/s0924-8579(03)00009-8. [DOI] [PubMed] [Google Scholar]
- 13.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 14.Pena C, Zorrilla SG, Oriol I, Tubau F, Dominguez MA, Pujol M. Impact of multidrug resistance on Pseudomonas aeruginosa ventilator-associated pneumonia outcome: Predictors of early and crude mortality. Eur J Clin Microbiol Infect Dis. 2013;32:413–20. doi: 10.1007/s10096-012-1758-8. [DOI] [PubMed] [Google Scholar]
- 15.Morales E, Cots F, Sala M, Comas M, Belvis F, Riu M. Hospital costs of nosocomial multi-drug resistant Pseudomonas aeruginosa acquisition. BMC Health Serv Res. 2012;12:1–8. doi: 10.1186/1472-6963-12-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahon C, Lehman D, Manuselis G. 4th ed. USA: Elsevier; 2011. Text Book of Diagnostic Microbiology; pp. 480–90. [Google Scholar]
- 17.Tyler SD, Strathdee CA, Rozee KR, Johnson WM. Oligonucleotide primers designed to differentiate pathogenic Pseudomonas on the basis of the sequencing of genes coding for 16S-23S rRNA internal transcribed spacers. Clin Diagn Lab Immunol. 1995;2:448–53. doi: 10.1128/cdli.2.4.448-453.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.USA, Wayne, Pa: National Committee for Clinical Laboratory Standards; 2012. National Committee for Clinical Laboratory Standards Ed., “Prefomance standards for antimicrobial disk susceptibility tests,” Approved Standards M100- S22. [Google Scholar]
- 19.Gorgani N, Ahlbrand S, Patterson A, Pourmand N. Detection of point mutations associated with antibiotic resistance in Pseudomonas aeruginosa . Int J Antimicrob Agents. 2009;34:414–8. doi: 10.1016/j.ijantimicag.2009.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jeannot K, Elsen S, Kohler T, Attree I, Delden CV, Plesiat P. Resistance and virulence of Pseudomonas aeruginosa clinical strains overproducing the MexCD-OprJ efflux pump. Antimicrob Agents Chemother. 2008;52:2455–62. doi: 10.1128/AAC.01107-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Breidenstein EB, Nunez CD, Hancock RE. Pseudomonas aeruginosa: All roads lead to resistance. Trends Microbiol. 2011;19:419–26. doi: 10.1016/j.tim.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 22.Hirsch EB, Tam VH. Impact of multidrug-resistant Pseudomonas aeruginosa infection on patient outcomes. Expert Rev Pharmacoecon Outcomes Res. 2010;10:441–51. doi: 10.1586/erp.10.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soto SM. Role of efflux pumps in the antibiotic resistance of bacteria embedded in a biofilm. Virulence. 2013;4:1–7. doi: 10.4161/viru.23724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Livermore DM. Multiple mechanisms of antimicrobial resistance in Pseudomonas aeruginosa: Our worst nightmare.? Clin Infect Dis. 2002;34:634–40. doi: 10.1086/338782. [DOI] [PubMed] [Google Scholar]
- 25.Hooper DC. Efflux pumps and nosocomial antibiotic resistance: A primer for hospital epidemiologists. Clin Infect Dis. 2005;40:1811–7. doi: 10.1086/430381. [DOI] [PubMed] [Google Scholar]
- 26.Anderson C, Jalal S, Aili D, Wang Y, Islam S, Jarl A. Critical biophysical properties in Pseudomonas aeruginosa efflux gene regulator MexR are targeted by mutations conferring multidrug resistance. Protein Sci. 2010;19:680–92. doi: 10.1002/pro.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tomas M, Doumith M, Warner M, Turton JF, Beceiro A, Bou G. Efflux pumps, OprD Porin, AmpC β-Lactamase, and multiresistance in Pseudomonas aeruginosa isolates from cystic fibrosis patients. Antimicrob Agents Chemother. 2010;54:2219–24. doi: 10.1128/AAC.00816-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Henrichfreise B, Wiegand I, Pfister W, Wiedemann B. Resistance mechanisms of multiresistant Pseudomonas aeruginosa strains from germany and correlation with hypermutation. Antimicrob Agents Chemother. 2007;51:4062–70. doi: 10.1128/AAC.00148-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suman G, Khan M, Sabitha K, Jamil K. Mutation in mexR-gene leading to drug resistance in corneal keraitis in human. Indian J Exp Biol. 2006;44:929–36. [PubMed] [Google Scholar]
- 30.Hocquet D, Bertrand X, Kohler T, Talon D, Plesiat P. Genetic and phenotypic variations of a resistant Pseudomonas aeruginosa epidemic clone. Antimicrob Agents Chemother. 2003;47:1887–94. doi: 10.1128/AAC.47.6.1887-1894.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jalal S, Ciofu O, Høiby N, Gotoh N, Wretlind B. Molecular mechanisms of fluoroquinolone resistance in Pseudomonas aeruginosa isolates from cystic fibrosis patients. Antimicrob Agents Chemother. 2000;44:710–2. doi: 10.1128/aac.44.3.710-712.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morita Y, Cao L, Gould VC, Avison MB, Poole K. NalD encodes a second repressor of the MexAB-OprM multidrug efflux operon of Pseudomonas aeruginosa. J Bacteriol. 2006;188:8649–54. doi: 10.1128/JB.01342-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sobel ML, Hocquet D, Cao L, Plesiat P, Poole K. Mutations in PA3574 (nalD) lead to increased MexAB-OprM expression and multidrug resistance in laboratory and clinical isolates of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2005;49:1782–6. doi: 10.1128/AAC.49.5.1782-1786.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]


