Abstract
Background:
Heparin has long been used to prevent thrombosis in the permanent central venous hemodialysis catheters (PermCath). Other alternatives for heparin with fewer side-effects have recently been considered. We compared normal saline (0.9%) with heparin for flushing PermCath with regards to catheter patency and prevention of heparin complications.
Materials and Methods:
Chronic kidney disease patients who were candidate of PermCath placement were randomly assigned into two groups of heparin and saline. In the heparin group, the PermCath was flushed with heparin (1000 IU), and in the saline group, it was flushed with saline 0.9%. Patients were followed for 24 hours, and outcomes included catheter thrombosis, maneuver needed to maintain catheter patency, and bleeding from catheter site.
Results:
Ninety six patients were included (age = 63.1 ± 11.2 years, 54.2% male). No one experienced catheter thrombosis. Two patient (4.2%) in the heparin and three ones (6.1%) in the saline group required catheter manipulation (P = 0.520). Four patients (8.5%) in the heparin and three ones (6.1%) in the saline group experienced bleeding (P = 0.476); differences between heparin and saline groups in the amount of bleeding (225.0 ± 62.4 vs. 200.0 ± 113.5 cc, P = 0.721) and bleeding time (6.5 ± 1.2 vs. 5.3 ± 1.5 min, P = 0.322) were not significant. In the heparin group, no significant increase was observed in PTT over time; baseline 30.9 ± 3.4, 12 h 31.8 ± 3.4, 24 h 31.2 ± 6.6 (P = 0.628).
Conclusions:
Flushing PermCath with normal saline 0.9% is as effective as heparin in maintaining patency of the catheter, while it may reduce the risks associated with heparin.
Keywords: Central venous catheters, hemorrhage, heparin, thrombosis
INTRODUCTION
Chronic kidney disease patients require an appropriate vascular access for hemodialysis with sufficient blood flow. Three general long-term types of access that are currently used for this purpose include arteriovenous fistula, synthetic grafts, and tunneled catheters. Although current guidelines do not recommend the catheters for more than 10% of permanent accesses,[1] in many centers, the percentages of catheters are more than this amount. Furthermore, in patients with recent graft or fistula, these catheters have very important roles in maturation of grafts (about two weeks) and fistulas (about two months). Also, in patients who are undergoing peritoneal dialysis, dialysis is performed through the catheter if peritonitis occurred. According to the statistics, every year, more than 250 thousand tunneled catheters are placed in the United States.[2]
Infection and thrombosis are the most common and important complications related to tunneled catheters. Catheter thrombosis, through venous thrombosis or creating a fibrin sheath, includes up to 40% of catheter complications[3] and cause catheter dysfunction. Additionally, it interferes with organ grafts and fistulas, and fibrin sheaths reduce catheter blood flow and cause disturbances in dialysis function.[2] In many centers, high concentrations of heparin solution (1000 to 10000 IU) are used to lock the catheter for prevention of catheter thrombosis.[4] This method, however, has important complications. Heparin leak into the systemic circulation may cause heparin-induced thrombocytopenia and increase the risk of systemic coagulopathy and bleeding.[5,6,7]
Other alternatives for locking the catheters such as saline solution, sodium citrate, polyethylene gelin, saline, and low heparin concentration rather than high concentrations have recently been considered. Studies have shown that these methods are the same at keeping the hemodialysis catheter open and do not have heparin-induced adverse effects.[6,7,8,9,10] However, few studies have been conducted on this subject, and there are some controversies on this issue. Therefore, this study aimed to compare normal saline 0.9% and heparin for flushing into the permanent central venous hemodialysis catheters (PermCath) with regards to catheter patency and prevention of heparin complications.
MATERIALS AND METHODS
This single-blinded, randomized, controlled trial was conducted on chronic kidney disease patients who were candidate for PermCath placement. The study was done on vascular surgery ward in a university hospital in Isfahan between 2012 and 2013. Patients were consecutively enrolled into the study. They were 18 years and older and had their first permanent catheter insertion through their right or left internal jugular vein. Patients with the following conditions were not included: Patients on anti-coagulants or therapeutic dose of fibrinolytic therapy, coagulopathy, thrombocytopenia (platelets <100000/mcL), history of allergy to heparin, having arteriovenous fistulas at each extremity, and the history of pulmonary hypertension. The study was approved by the Ethics Committee of Isfahan University of Medical Sciences and registered in clinical trials database (clinicaltrials.gov). Patients participating in the study signed a written consent.
Intervention
Based on random allocation numbers, patients were divided into two groups of heparin and saline. A double lumen permanent hemodialysis catheter (model Even-More, USA, 14.5 F, 28 cm on the right or left 32 cm) was placed by an experienced vascular surgeon with the same protocol in the operating room. Ensuring the catheter function aspiration with a 20 cc syringe was done in the operating room after catheter placement, and to ensure the proper placement of the catheter location, post-operative chest X-ray was performed. In the heparin group, the catheters were locked with 1000 IU heparin added to 10 cc isotonic saline,[4] in the saline group, it was locked with saline solution 0.9%.
Assessments
Treatment outcomes included catheter thrombosis (irreversible closure of the catheter), the need to perform any maneuver (lavage, move, etc.) to open the catheter, and bleeding from the catheter site. The first visit was performed in one day after the catheter placement, and surgical site bleeding was investigated by a resident of surgery by counting the number of bloody gases (any gauze around 30 cc).[11] Also, catheter thrombosis (based on unsuccessful hemodialysis, chest X-ray, and maneuver) and the need to perform any maneuver to open the catheter were checked. Coagulation tests including prothrombin time (PT), partial thromboplastin time (PTT), platelets count, and bleeding time (for those with bleeding) were performed by the Hospital laboratory for all patients before operation and immediately after operation, and then 12 hours after the operation for the heparin group.
Data analysis
Data were analyzed using SPSS v. 16 software for windows. The Chi-Square test (for a nominal qualitative variables), independent sample t-Test and paired t-Test (for parametric quantitative variables), and Mann-Whitney and Wilcoxon tests (for qualitative variables bit rate or parametric) were used. A P value of < 0.05 was considered statistically significant.
RESULTS
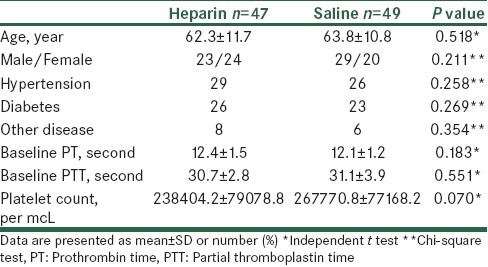
One hundred and twenty nine patients were evaluated during the study period. Twenty nine patients were not eligible to be included into the study, and six patients were excluded from the study after enrolment as their laboratory data indicated platelets count < 100000. Finally, a total of 96 patients were included into the trial (age = 63.1 ± 11.2 years, 54.2% male), Figure 1. The two groups were similar regarding demographic characteristics and baseline laboratory data, except that baseline platelets count was about 29366 platelet/mcL lower in the heparin compared with the saline group (P = 0.070), [Table 1].
Figure 1.
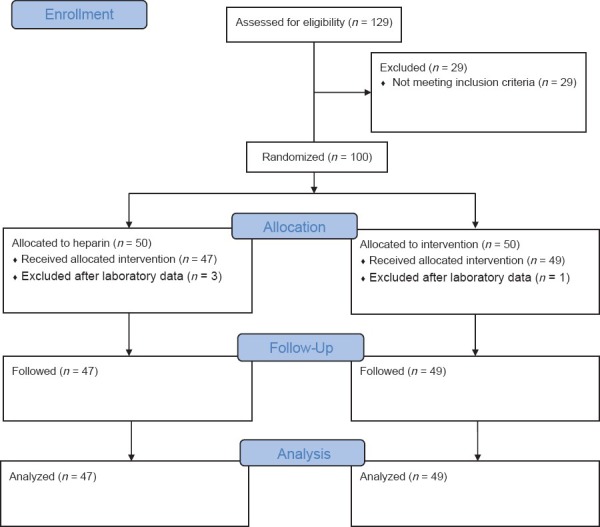
Patients flow diagram
Table 1.
Comparison of demographic characteristics and baseline laboratory data between the two groups
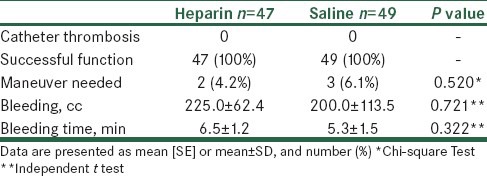
Comparison of outcome variables between the two groups is presented in Table 2. No one experienced catheter thrombosis, and catheter function was successful in all patients. Two patient (4.2%) in the heparin and three ones (6.1%) in the saline group required catheter manipulation to maintain the patency of the catheter (P = 0.520). Four patients (8.5%) in the heparin and three ones (6.1%) in the saline group experienced bleeding (P = 0.476); difference between groups in the amount of bleeding (P = 0.721) and bleeding time (P = 0.322) was not significant [Table 2].
Table 2.
Comparison of outcome variables between the two groups
In the heparin group, no significant increase was observed in PTT over time; baseline 30.9 ± 3.4, 12 h 31.8 ± 3.4, 24 h 31.2 ± 6.6 (P = 0.628). Regarding the difference between the two groups in baseline platelets counts, we conducted a multivariate analysis for evaluating possible predictors of bleeding. After including variables of age, gender, hypertension, diabetes, type of intervention, baseline PT and PTT, and baseline platelet into the linear regression analysis, the baseline PTT was significantly associated with increasing amount of bleeding (unstandardized β =4.066, P = 0.031).
DISCUSSION
This study aimed to compare saline with heparin for locking the hemodialysis permanent central venous catheter. The two methods did not differ in the catheter function and catheter thrombosis, or in the amount of bleeding and bleeding time. Also, in the multivariate analysis, only the baseline PTT was associated with more bleeding. Hence, the saline has not significantly reduced bleeding. However, the dose of heparin can affect the bleeding, and it is likely that if we used higher dose of heparin, more bleeding would occurred. In preserving the catheter function, saline has a similar effect with heparin, which indicates that saline is a good alternative for locking permanent central venous catheter for hemodialysis.
Some of the previous studies have examined the possibility of replacing high-dose heparin with low-dose heparin, and some of the other studies have examined the replacement of other solutions including saline and citrate with heparin. Among the studies, which have compared a lower dose of heparin with the usual dose, Thomson et al. compared 1000 IU of heparin with 5000 IU to lock the catheter.[6] The results showed that the activated partial thromboplastin time (aPTT) increased 22.2%, ten minutes after locking the catheter with 1000 IU of heparin, while aPTT increased 373.7% after locking the catheter with 5000 IU of heparin. However, it was no significant difference between catheter thrombosis and blood flows during dialysis.[6] In another retrospective study by the Yevzlin and colleagues, on patients with tunneled catheters for hemodialysis, the patients were divided to receive 5000 IU or 1000 IU of heparin or citrate for catheter lock.[7] Multivariable analysis showed that the risk of bleeding in patients receiving heparin with higher concentration is about 12 times more than other groups.[7] These studies showed that low-dose heparin has no significant negative effect on catheter function and catheter thrombosis, while the risk of bleeding and coagulopathies were significantly reduced after infusion of low-dose heparin.
Among the studies, which have used some other non-heparin solutions for permanent central venous catheter, the study of Buturović et al. compared the patients in three groups of heparin, citrate, and polygeline.[8] There was no difference between three groups in the duration of catheter use and clot formation. These authors concluded that citrate and polygeline can replace heparin in temporary intravenous catheters for hemodialysis.[8] In the study of Moran and colleagues, on patients undergoing heWmodialysis, central venous catheter was locked with heparin (1000 IU/ml) or gentamicin-citrate solution with 4% saline. The results showed that gentamicin-citrate solution reduced the incidence of infection; however, catheter thrombosis was associated with the size of catheter.[10] Some studies have also examined saline as an alternative for heparin. In the study by Del Cotillo et al., which compared saline with heparin (1 IU/ml), the two different methods had no difference in the duration of catheters being in place and the manipulations required to maintain the patency of the arterial catheter, while patients receiving heparin had longer aPTT (2.1 vs. 1.25).[9] In another study by Pumarola and colleagues, 100 IU/ml heparin was compared with 500 IU/ml heparin and with saline in two separate phases. The results of this study showed that saline solution is as effective as 100 or 500 IU of heparin for maintenance of catheter patency.[12] In another study, Kaneko and colleagues compared daily saline lavage (20 ml) to locking the catheter with saline (20 ml) plus 2 ml heparin (1000 IU) and found no difference between the two methods in catheters thrombosis.[13] In contrast, some other studies have different results. For example, in the study by Rabe et al., high dose heparin (5000 IU) was significantly better in keeping the catheter open compared with vitamin C and saline 0.9%.[14] However, most studies showed that replacing high-dose heparin with low-dose heparin or other solutions makes no changes on catheter thrombosis, while the risk of subsequent bleeding and coagulopathies may be more with high-dose heparin. Therefore, at least in patients who have high risk for bleeding such as the patients with low platelet or prolonged PTT, we can use saline solution instead of heparin for locking the catheter.
Our study also had some limitations. Although patients were randomly divided into two groups, probably because of the small sample size, the two groups were not similar regarding baseline platelet count for which we applied multivariate analysis. Also, given the low incidence of catheter thrombosis, longer follow-up and larger sample size was needed. In this study, we used catheter thrombosis and the need of maneuver to open the catheter to evaluate the catheter function. However, in some previous studies, the catheter blood flow during hemodialysis was examined, which is a more sensitive criteria for evaluating the catheter function[6] and it is better to be studied more in future.
In summary, the present study showed that saline solution is as effective as heparin in maintaining the patency of permanent hemodialysis catheter. Also, the amount and duration of bleeding was not significantly different between heparin and saline lock methods. The equality of heparin and saline in catheter function shows that saline can be a substitute for heparin for locking the permanent hemodialysis catheter at the end of procedure. However, more studies with larger sample sizes and longer fallow-ups and also with more sensitive methods for assessing the function of the catheter are recommended.
ACKNOWLEDGMENTS
This study was supported by the Isfahan University of Medical Sciences. We are thankful to Dr. Ali Gholamrezaei for helping us in editing this report.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.NKF-DOQI clinical practice guidelines for vascular access. National Kidney Foundation-Dialysis Outcomes Quality Initiative. Am J Kidney Dis. 1997;30:S150–91. [PubMed] [Google Scholar]
- 2.Trerotola SO. Hemodialysis catheter placement and management. Radiology. 2000;215:651–8. doi: 10.1148/radiology.215.3.r00jn23651. [DOI] [PubMed] [Google Scholar]
- 3.Liangos O, Gul A, Madias NE, Jaber BL. Long-term management of the tunneled venous catheter. Semin Dial. 2006;19:158–64. doi: 10.1111/j.1525-139X.2006.00143.x. [DOI] [PubMed] [Google Scholar]
- 4.Moran JE, Ash SR. Locking solutions for hemodialysis catheters; heparin and citrate-a position paper by ASDIN. Semin Dial. 2008;21:490–2. doi: 10.1111/j.1525-139X.2008.00466.x. [DOI] [PubMed] [Google Scholar]
- 5.Dreyer G, Lawton P, Jose M. Heparin leak from a hemodialysis catheter causing major bleeding, ultimately leading to transplant rejection and death. Hemodial Int. 2008;12:431–3. doi: 10.1111/j.1542-4758.2008.00306.x. [DOI] [PubMed] [Google Scholar]
- 6.Thomson PC, Morris ST, Mactier RA. The effect of heparinized catheter lock solutions on systemic anticoagulation in hemodialysis patients. Clin Nephrol. 2011;75:212–7. doi: 10.5414/cn106460. [DOI] [PubMed] [Google Scholar]
- 7.Yevzlin AS, Sanchez RJ, Hiatt JG, Washington MH, Wakeen M, Hofmann RM, et al. Concentrated heparin lock is associated with major bleeding complications after tunneled hemodialysis catheter placement. Semin Dial. 2007;20:351–4. doi: 10.1111/j.1525-139X.2007.00294.x. [DOI] [PubMed] [Google Scholar]
- 8.Buturovic J, Ponikvar R, Kandus A, Boh M, Klinkmann J, Ivanovich P. Filling hemodialysis catheters in the interdialytic period: Heparin versus citrate versus polygeline: A prospective randomized study. Artif Organs. 1998;22:945–7. doi: 10.1046/j.1525-1594.1998.06268.x. [DOI] [PubMed] [Google Scholar]
- 9.Del CM, Grane N, Llavore M, Quintana S. Heparinized solution vs. saline solution in the maintenance of arterial catheters: A double blind randomized clinical trial. Intensive Care Med. 2008;34:339–43. doi: 10.1007/s00134-007-0886-6. [DOI] [PubMed] [Google Scholar]
- 10.Moran J, Sun S, Khababa I, Pedan A, Doss S, Schiller B. A randomized trial comparing gentamicin/citrate and heparin locks for central venous catheters in maintenance hemodialysis patients. Am J Kidney Dis. 2012;59:102–7. doi: 10.1053/j.ajkd.2011.08.031. [DOI] [PubMed] [Google Scholar]
- 11.Hughes K, Chang YC, Sedrak J, Torres A. A clinically practical way to estimate surgical blood loss. Dermatol Online J. 2007;13:17. [PubMed] [Google Scholar]
- 12.Pumarola C, Casademont MR, Colomer PM, Cordon BC, Sabench CS, Felez VM, et al. Comparative study of maintenance of patency of triple lumen central venous catheter. Enferm Intensiva. 2007;18:25–35. doi: 10.1016/s1130-2399(07)74386-9. [DOI] [PubMed] [Google Scholar]
- 13.Kaneko Y, Iwano M, Yoshida H, Kosuge M, Ito S, Narita I, et al. Natural saline-flush is sufficient to maintain patency of immobilized-urokinase double-lumen catheter used to provide temporary blood access for hemodialysis. Blood Purif. 2004;22:473–9. doi: 10.1159/000081811. [DOI] [PubMed] [Google Scholar]
- 14.Rabe C, Gramann T, Sons X, Berna M, Gonzalez-Carmona MA, Klehr HU, et al. Keeping central venous lines open: A prospective comparison of heparin, vitamin C and sodium chloride sealing solutions in medical patients. Intensive Care Med. 2002;28:1172–6. doi: 10.1007/s00134-002-1379-2. [DOI] [PubMed] [Google Scholar]


