Abstract
Background
We evaluated whether computerized counseling about contraceptive options and screening for contraindications increased women’s subsequent knowledge and use of hormonal contraception.
Methods
For the study 814 women aged 18 to 45 years were recruited from the waiting rooms of three emergency departments and an urgent care clinic staffed by non-gynecologists and asked to use a randomly-selected computer module before seeing a clinician.
Results
Women in the intervention group were more likely to report receiving a contraceptive prescription when seeking acute care than women in the control group (16% vs 1%, p=0.001). Women who requested contraceptive refills were not less likely than women requesting new prescriptions to have potential contraindications to estrogen (75% of refills vs. 52% new, p=0.23). Three months after visiting the clinic, women in the intervention group tended to be more likely to have used contraception at last intercourse (71% vs 65%, p=0.91) and to correctly answer questions about contraceptive effectiveness, but these differences were not statistically significant.
Conclusion
Patient-facing computers appear to increase access to prescription contraception for women seeking acute care.
Keywords: Contraceptive counseling, primary care, urgent care, acute care, computer information technology
1. Introduction
As nearly 50% of US pregnancies are unplanned [1], there is a need to improve knowledge of and access to effective contraception. Because prescription contraceptives are typically more effective than barrier or behavioral methods [2], women who have limited access to health care may experience higher rates of unintended pregnancy. Indeed, in the US, low-income women frequently have limited access to routine health care [3], and experience higher rates of unintended pregnancy [4]
Acute care settings (such as emergency departments and urgent care clinics) serve as a primary source of health care for many low-income, uninsured, and younger women [5]. In prior work, we found that although the large majority (68%) of women surveyed in two urgent care clinics reported they were trying to avoid pregnancy, 32% reported recent unprotected sex [6]. However, urgent care clinicians rarely provide contraceptive prescriptions [6], due in part to time constraints [7], inadequate knowledge of available contraceptive options, and limited experience screening women for contraindications to contraceptive use or managing potential side effects. Prior research suggests that there is little need for direct physician involvement in the provision of hormonal contraception, as women can use a checklist to self-screen for contraindications to use of hormonal contraception, manage side effects, and determine an appropriate initiation date [8,9].
Thus, we developed a patient-facing computer program (a computer “kiosk”) to facilitate access to prescription contraception for women seeking acute care from emergency departments or urgent care clinics staffed by non-gynecologists. We assessed whether this program was acceptable to women and increased the number of women receiving contraceptive prescriptions when they sought acute care. As secondary outcomes, we explored the effects of this intervention on women’s knowledge and use of prescription contraception three months after they sought acute care.
2. Materials and methods
Between January and July of 2011, women were consecutively recruited from the waiting rooms of four urban acute care settings (three emergency departments and one urgent care center staffed by non-gynecologists) in Western Pennsylvania. All four locations were part of the same large health system. Women aged 18–45 years were invited by an on-site research assistant to use an interactive computer program in English or Spanish while waiting to see a clinician. At each location, the kiosk program randomized women to use either an interactive computer module that provided information about contraceptives and the opportunity to request a prescription, or a control module that provided information about screening for chlamydia infection. The computer modules’ content was adapted from evidence-based sources of information [2,10]. To overcome potential health literacy barriers, headphones were provided so that women could chose to either listen to or read the information presented. Informed consent and patient contact information were recorded by the computer. Women received no compensation for using the computer on the day they visited the clinic, however, participants received $10 on completion of a follow-up survey three months after their visit. This study was approved by the Institutional Review Board of the University of Pittsburgh (#PRO0806023) on September 12, 2008, and registered on clinicaltrials.gov. On the basis of our prior work in urgent care clinics in San Francisco [11,12], we anticipated that no more than 1% of women in the control group would receive a contraceptive prescription when seeking acute care and that 3 months after women enrolled in this study, 30% of women in the control group would report using hormonal contraception. We powered this study to have an 80% chance of detecting a significant difference at a two-sided alpha of 0.05 if 45% of women in the intervention group (a difference of 15%) were using hormonal contraception at the 3-month follow-up, with 175 women in each group. Because we anticipated that 45% of women would have no need for a new contraceptive prescription (i.e., they would be happy with a previously provided contraceptive), we planned to enroll 318 women in each group to ensure that half might benefit from the offer of a new contraceptive prescription. In addition, as women seeking acute care are a transient population, we anticipated 15% loss to follow-up and aimed to enroll a total of 824 subjects.
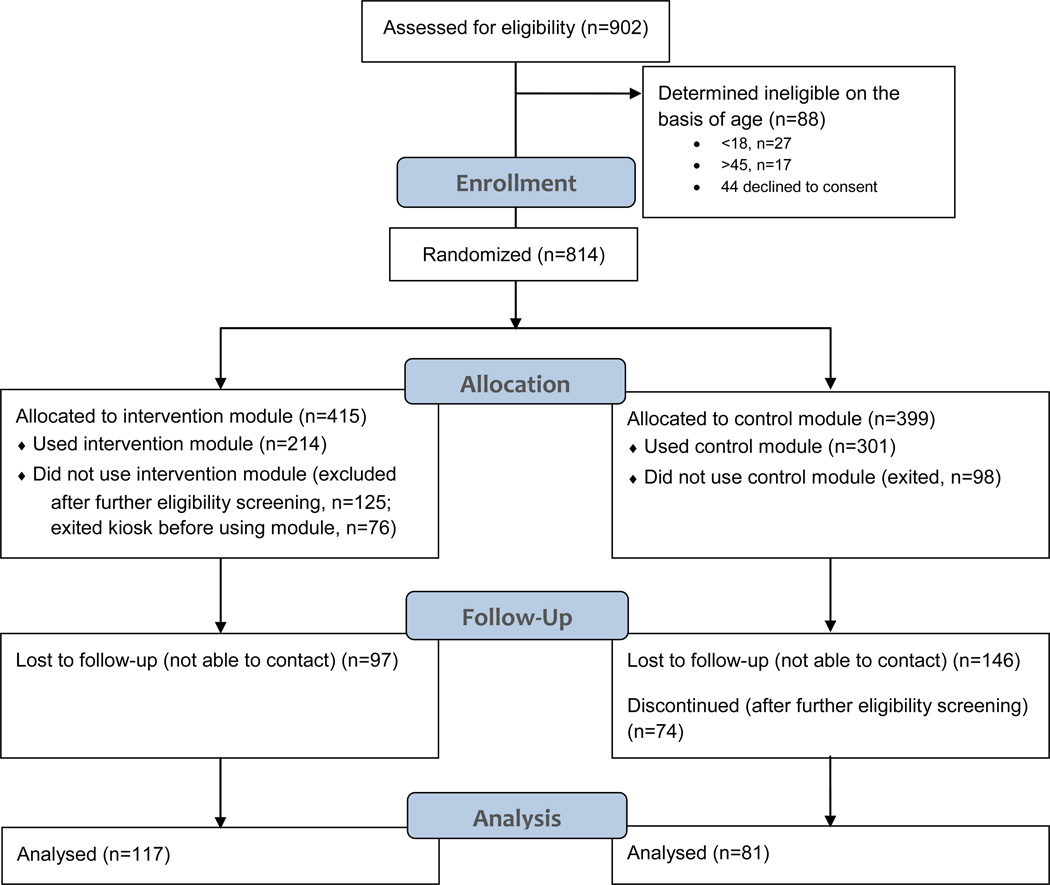
Women randomized to the intervention were screened by the computer for eligibility (Fig. 1). Women were excluded from this intervention if they were not in need of contraception (because they were currently pregnant, trying to become pregnant, had undergone a hysterectomy or tubal ligation, had an intrauterine device or implant in place, had a partner who had undergone vasectomy, or reported only having sex with women). Eligible participants were offered educational information about commonly used methods of reversible contraception (Fig. 2). Participants were able to choose which contraceptives they wanted to learn about, and were given the opportunity to request a prescription for a combined oral contraceptive, progestin-only pill, contraceptive ring, or patch. Women who requested an estrogen-containing contraceptive were screened by the computer for 14 potential contraindications to estrogen use considered category “3” or “4” according to the World Health Organization and US Centers for Disease Control [13,14] (Table 1); if none were identified, a prescription was printed and then signed by a study clinician who had reviewed the patient’s medical record for any hypertension. Prior to March 2011, women who reported one or more potential contraindications to the use of estrogen-containing contraception were told that the computer had identified a potential contraindication to the contraceptive they had selected and encouraged them to discuss birth control options with their doctor. Starting in March 2011, the computer program was modified so that women with potential contraindications to estrogen were offered a prescription for the progestin-only pill in addition to being advised to discuss birth control options with their clinician. On the day women used the computer, the intervention module assessed women’s satisfaction with the intervention and reasons for exiting the program. Women entered their phone number and e-mail address for follow-up into the computer kiosk. We did not require women to enter demographic or other personal information prior to using the kiosk out of concern that early attempts to collect this information would deter women from using the kiosk.
Figure 1. Flow of participants through trial.
Figure 2. Sample Screenshots from Intervention.
Two examples of what the intervention module looks like – choice of method to learn about next, and the first page of information about the contraceptive ring.
Table 1.
Potential contraindications to estrogen identified by computerized screening
| Contraindications reported | MECa category [15,16] |
N (%)b |
|---|---|---|
| Migrainesc | 4 | 17 (7.9) |
| Smoker and over 35 years of age | 4 | 2 (0.9) |
| Had baby in last 3 weeks | 3 | 2 (0.9) |
| High blood pressured | 4 | 2 (0.9) |
| Gallbladder disease | 3 | 2 (0.9) |
| Blood clot | 4 | 0 (0) |
| Heart attack or stroke | 4 | 0 (0) |
| Heart disease | 4e | 0 (0) |
| Diabetes | 4 | 0 (0) |
| Medication for high cholesterol | 3 | 0 (0) |
| Liver disease/cancer | 4 | 0 (0) |
| Breast cancer | 4 | 0 (0) |
| Breastfeeding an infant under 6 months of age | 3 (4)f | 0 (0) |
| Medication for seizures/tuberculosis | 3 | 0 (0) |
Medical eligibility criteria; 4 “A condition which represents an unacceptable health risk if the contraceptive method is used”; 3 “A condition where the theoretical or proven risks usually outweigh the advantages of using the method.”
The family planning module was used by 214 women who could identify more than one potential contraindication to the use of estrogen.
The computer did not ask women to specify whether they had migraines with or without aura.
An additional 2 women were identified as having hypertension on clinician chart review and thus received a progestin-only pill instead of the estrogen-containing contraceptive they had initially requested.
e.g. peripartum cardiomyopathy, or moderately or severely impaired cardiac function
US MEC = 3, WHO MEC = 4.
Three months after women used the kiosk, they were contacted and asked to answer questions about their current knowledge and use of contraception. Women could complete this survey by phone or the Internet. Women were asked whether they remembered what topic the computer had addressed, about their satisfaction with the computer kiosk, and whether they received a contraceptive prescription or referral for family planning services the day they sought acute care. Participants were also asked about their current pregnancy intentions, and contraceptive knowledge with the following questions: “Typically, when using condoms for birth control, how many women will get pregnant within one year?” with the following response options: ‘none’, ’1 in 7’, 1 in 100’ or ‘1 in 10,000’. On the basis of the existing literature [2], we considered the correct answer to be “1 in 7.” Participants were then asked “How well do IUDs and implants work?” and “How well do the ring and the patch work?” with response options which included: ‘the same effectiveness as a condom’, ‘the same effectiveness as a birth control pill’, ‘the same effectiveness as surgical sterilization (having your tubes tied)’. Because women randomized to the control group were screened only for age criteria on the day they sought acute care, at follow up these women were further screened to confirm that they would have been eligible to use the family planning module at the time they sought acute care.
Using the data collected at the time women used the computer programs, we calculated the percentage of women in the intervention group who requested a contraceptive prescription, the types of contraceptives requested, and whether a potential contraindication to estrogen was identified. Using follow-up survey data, we calculated the percentage reporting receipt of a contraceptive prescription the day they used the computer program, reporting use of contraception at last intercourse, and reporting that they were unintentionally pregnant. Secondary outcomes included knowledge of contraceptive effectiveness at the 3-month follow-up. Categorical outcomes were compared using chi squared tests and Fisher’s exact tests, and continuous outcomes were compared using t-tests for independent samples. In addition, we used multivariable logistic regression to control for women’s pregnancy intentions and demographic characteristics when examining the intervention effect on contraceptive use at 3 months. All analyses were performed using Stata 10 IC (StataCorp, College Station, TX).
3. Results
Over the 7 months of this study, approximately half of women invited to use the kiosk consented and enrolled in this study; of these 814 women, 415 were randomized to the intervention and 399 to the control group (Fig. 1). At baseline, there was no significant difference in the mean age of women randomized to each group (p=0.27). Of those randomized to the intervention group, 125 were ineligible, either because they were pregnant or trying to conceive (n=76), had been sterilized or had a partner with a vasectomy (n=17), had an IUD (n=25), or only had sex with women (n=7); an additional 76 women exited the module before completing screening, leaving 214 women who used the intervention module. In total, of the 515 women eligible for follow-up, 53% (n=272) completed the follow-up survey (211 by email and 61 over the phone). Additional screening found that 74 women randomized to the control group would have been ineligible for the intervention, and so they were excluded from further analyses, leaving n=117 in the intervention group and n=81 in the control group for the final analysis (Fig. 1). Among women in the intervention group, age was not associated with likelihood of completing follow-up (p=0.81); however, women who “did not know” whether they wanted to become pregnant were less likely to complete follow-up (p=0.05).
The average mean age ± standard deviation of women who completed the follow-up survey was 26.1±5.3 years. The majority (66%) was white, three-quarters had private insurance and 85% reported completing at least some college. There were no significant demographic differences between women in the intervention and control groups at follow-up (Table 2).
Table 2.
Characteristics of study participants who completed follow-up
| Participant characteristics | Intervention N = 117 N (%) |
Control N = 81 N (%) |
p-value |
|---|---|---|---|
| Age | 0.97 | ||
| 18–21 | 19 (16.4) | 13 (16.1) | |
| 22–30 | 77 (66.4) | 52 (64.2) | |
| 31–45 | 20 (17.2) | 16 (19.8) | |
| Race | |||
| White | 77 (67.0) | 51 (63.8) | 0.64 |
| Black | 30 (26.1) | 26 (32.5) | |
| Other | 8 (7.0) | 3 (3.8) | |
| Education level | |||
| High school education (or less) | 16 (13.7) | 13 (16.1) | 0.91 |
| Some college | 31 (26.5) | 24 (29.6) | |
| Graduated college | 29 (24.8) | 18 (22.2) | |
| More than 4-year degree | 40 (34.2) | 26 (32.1) | |
| Health insurance | 0.62 | ||
| Private | 79 (67.5) | 54 (66.7) | |
| Public | 20 (17.1) | 19 (23.5) | |
| None | 13 (11.1) | 6 (7.4) | |
| Religious objection to birth control | 0.65 | ||
| Yes | 4 (3.4) | 3 (3.7) | |
| Relationship status | 0.64 | ||
| Currently married | 14 (12.0) | 13 (16.1) | |
| Not married, in committed relationship | 59 (50.4) | 35 (43.2) | |
| Actively dating, not committed | 13 (11.1) | 8 (9.9) | |
| Divorced/Separated/Widowed | 2 (1.8) | 2 (2.5) | |
| Single, not in relationship | 29 (24.8) | 22 (27.2) | |
| Household income range | 0.76 | ||
| Under $20,000 | 22 (18.8) | 19 (23.5) | |
| $20,000 to $39,999 | 31 (26.5) | 17 (21.0) | |
| $40,000 to $59,999 | 18 (15.4) | 13 (16.1) | |
| Over $60,000 | 31 (26.5) | 19 (23.5) | |
| Don’t know/Missing data | 15 (12.8) | 13 (16.1) | |
| Pregnancy intentions | 0.14 | ||
| Trying or would not mind pregnancy | 11 (9.8) | 13 (17.1) | |
| Trying to avoid pregnancy | 101 (90.2) | 63 (82.9) | |
| Satisfaction with module | 0.88 | ||
| Very satisfied | 23 (26.4) | 18 (26.5) | |
| Satisfied | 47 (54.0) | 40 (58.8) | |
| Somewhat satisfied | 14 (16.1) | 8 (11.8) | |
| Not satisfied | 3 (3.5) | 2 (2.9) |
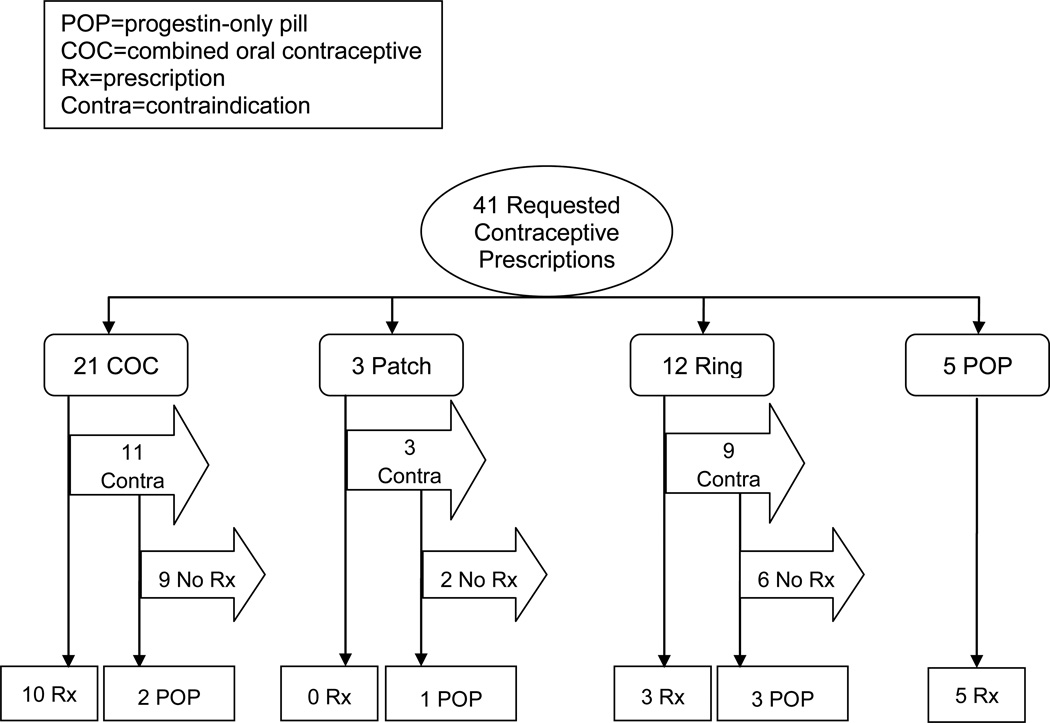
Among women who used the family planning module, 19% (41/214) requested a contraceptive prescription. Of these 41 women, 59% (24/41) ultimately received a prescription for hormonal contraception (Fig. 3). Potential contraindications to the use of estrogen were identified for 23 women, with migraine headaches the most commonly identified potential contraindication; other potential contraindications are shown in Table 1. Twenty percent (8/41) of the contraceptive prescription requests were for refills (Table 3). The eight women who requested a contraceptive refill were not less likely (and tended to be more likely) than women requesting new contraceptive prescriptions to be identified as having a potential contraindication to the use of estrogen (75% vs. 52%, p=0.23). Interestingly, 12% (5/41) of women who requested a contraceptive prescription initially requested a progestin-only pill, and an additional 15% (6/41) of women who requested a contraceptive prescription switched to progestin-only pills after being notified of a potential contraindication to the use of estrogen. None of the 11 women who received prescriptions for progestin-only pills had used an oral contraceptive at last intercourse; rather, most had used condoms, withdrawal, or no method of birth control the last time they had sex; one reported using a contraceptive injection (Table 3). Over half (57%) of women who received contraceptive prescriptions reported that since their last menses they had sex one or more times without a condom or other form of birth control.
Figure 3. Requests for contraceptive prescriptions.
Flowchart of prescriptions requested, contraindicated, and received. Arrows indicate participants being removed from consideration for a prescription, due to choice or contraindication (as stated).
POP=progestin-only pill
COC=combined oral contraceptive
Rx=prescription
Contra=contraindication
Table 3.
Relationship between contraceptive use prior to kiosk use and prescription request
| Prescription Initially Requested | |||||
|---|---|---|---|---|---|
| Method last used prior to visiting kiosk |
Ring N (%) |
Patch N (%) |
COCa N (%) |
POPb N (%) |
None N (%) |
| Ring (N=10) | 2 (20) | 0 (0) | 0 (0) | 0 (0) | 8 (80) |
| Patch (N=1) | 0 (0) | 1 (100) | 0 (0) | 0 (0) | 0 (0) |
| Combined Pill (N=89) | 0 (0) | 0 (0) | 5 (6) | 0 (0) | 84 (94) |
| Progestin-only Pill (N=0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| DMPAc (N=16) | 1 (6) | 0 (0) | 3 (19) | 0 (0) | 12 (75) |
| No method (N=23) | 5 (22) | 2 (9) | 3 (13) | 1 (4) | 12 (52) |
| Condoms (N=57) | 4 (7) | 0 (0) | 9 (16) | 3 (5) | 41 (72) |
| Withdrawal (N=5) | 0 (0) | 0 (0) | 1 (20) | 1 (20) | 3 (60) |
| Other (N=3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 3 (100) |
| Abstinence/never had sex (N=10) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 10 (100) |
| Total (N=214) | 12 (6) | 3 (1) | 21 (10) | 5 (2) | 173 (81) |
Combined oral contraceptive.
Progestin-only pill.
Depot medroxyprogesterone acetate.
3.1. Acceptability of computer-assisted provision of hormonal contraception
The majority (95%) of women who requested a contraceptive prescription said the program was easy to use, and 85% said they would recommend the computer module to a friend; however, 65% said that they would prefer to discuss their family planning needs with a health care provider. Of those participants who gave one or more reasons for exiting without requesting a prescription, nearly three quarters (115/160) said they already had birth control; 13% (20/160) said they did not have enough time to finish the module, and 3% (4/160) said they wanted an IUD, implant, or injection, instead of the methods offered by the kiosk. The study clinician spent less than 2 min reviewing the blood pressure measurements recorded in each woman’s medical record and ordering requested prescriptions.
3.2. Intervention effects at 3-month follow-up
Three months after visiting the study clinic, women in the intervention group were more likely to report they had received a contraceptive prescription the day they sought acute care (16% vs. 1%, p=0.001) (Table 4). Non-white women (34% non-white vs. 8% white, p<0.001), and less educated women (31% high school or less vs. 23% some college vs. 10% Bachelor’s degree or more, p=0.07) were more likely to have used the computer to request a contraceptive prescription than white or more educated women, respectively. At 3-month follow-up, more women in the intervention than control groups reported they used any form of birth control the last time they had sex (71% vs. 65%), but this difference was not statistically significant (p=0.91); similarly, women in the intervention group were more likely to report use of prescription contraception, but this difference was not statistically significant (Table 4). Women in the intervention group were also slightly more likely to answer each of the knowledge questions correctly, but these differences were not statistically significant (Table 4). Among women who reported having sex in the 3 months since they sought urgent care, four experienced an unintended pregnancy: 0.9% (1/117) of women in the intervention group vs. 3.8% (3/80) of women in the control group, but again, this difference was not statistically significant. In multivariable models, the strongest predictors of contraceptive use at 3-month follow-up were a woman’s pregnancy intentions and education (Table 5); women in the intervention group tended to be more likely to report use of prescription contraceptive (OR=1.41, 95% CI 0.62 – 3.19) or any contraception (OR1.37, 95% CI 0.33 – 5.68) at 3-month follow-up, but these findings did not reach statistical significance.
Table 4.
Knowledge, access to, and use of contraception at 3-month follow-up
| Reported at follow-up | Intervention N=117 N (%) |
Control N=80a N (%) |
p-value |
|---|---|---|---|
| Received a contraceptive Rx the day they used the computer | 19 (16.2) | 1 (1.3) | 0.001 |
| Had sex in 3 months after seeking urgent care | 94 (80.3) | 61 (76.3) | 0.49 |
| Unintended pregnancy at time of 3-month follow-up | 1 (0.9) | 3 (3.8) | 0.31 |
| Used any contraception at last intercourseb | 83 (70.9) | 52 (65.0) | 0.91 |
| Used prescription contraceptionc at last intercourseb | 55 (47.0) | 35 (43.8) | 0.95 |
| Correctly answered knowledge questions: | |||
| Knew IUDsd and implants are as effective as tubal ligation | 25 (21.4) | 12 (15.0) | 0.26 |
| Knew ring and patch are as effective as birth control pills | 101 (86.3) | 63 (78.8) | 0.16 |
| Knew 1 in 7 women using condoms typically becomes pregnant within first year of use | 33 (28.2) | 19 (23.8) | 0.49 |
One woman reporting current intended pregnancy was excluded from this analysis.
Four women reporting current pregnancy were excluded from these analyses.
Prescription contraception includes pills, patch, ring, injection, intrauterine devices (IUDs), and subdermal contraceptive implants. No new sterilization (vasectomy or tubal ligation) was reported.
Intrauterine device.
Table 5.
Association of participant characteristics with use of contraception at last sex (n=146)
| Participant characteristics | Use of any contraception at last sex |
Use of prescription contraception at last sex |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Intervention module | 1.37 (0.33 – 5.68) | 1.41 (0.62 – 3.19) |
| Age category, years | ||
| 18–21 | ---- Referent ---- | ---- Referent ---- |
| 22–30 | 1.51 (0.25 – 9.20) | 2.51 (0.71 – 8.84) |
| 31–45 | 0.67 (0.08 – 5.55) | 0.33 (0.07 – 1.54) |
| Race | ||
| Nonwhite | ---- Referent ---- | ---- Referent ---- |
| White | 3.02 (0.64 – 14.19) | 2.60 (1.11 – 6.06) |
| Education category | ||
| High school or less | ---- Referent ---- | ---- Referent ---- |
| Some college | 1.45 (0.27 – 7.70) | 4.01 (0.99 – 16.22) |
| Bachelors degree or more | 5.96 (0.69 – 51.35) | 5.92 (1.46 – 20.84) |
| Pregnancy intentions | ||
| Would novvt mind pregnancy | ---- Referent ---- | ---- Referent ---- |
| Trying to avoid pregnancy | 12.98 (2.93 – 57.55) | 4.23 (1.28 – 14.02) |
4. Discussion
This randomized controlled trial found that women were more likely to receive a contraceptive prescription when seeking acute care if they had access to computerized contraceptive education and screening for contraindications to use of estrogen; close to one fifth of women who used the kiosk while seeking acute care requested a contraceptive prescription. Over half the women who received contraceptive prescriptions reported recent unprotected intercourse and were thus at high risk of unintended pregnancy. Of note, minority and less-educated women were most likely to request a contraceptive prescription, likely reflecting their more limited access to contraceptive prescriptions.
Importantly, women who requested contraceptive refills, who had previously been screened by a clinician for contraindications to estrogen, were not less likely than women requesting new prescriptions to be identified as having a potential contraindication to estrogen. Thus, such technology may allow as much protection as the screening offered by most practicing clinicians. In addition, this intervention was implemented with minimal burden on busy clinicians and, thus, has the potential for widespread dissemination.
We were surprised to find that so many women requested prescriptions for progestin-only pills, even before they were notified of a potential contraindication to estrogen, as these are rarely prescribed by US clinicians [15]. Clinician counseling is known to affect women’s contraceptive choices [16–18] and contraceptive use [19]; however, there has been little attention to potential clinician bias against the use of progestin-only pills. In contrast to estrogen-containing contraceptives, the prevalence of contraindications to progestin-only pills, which pose less risk of thromboembolic disease [20], is very low [21].
We have previously shown that women who received computerized education about emergency contraception [22] and folic acid supplementation [23] while waiting for urgent care had increased knowledge and use of these medications. Likewise, computers have been used by family planning clinics to assist with contraceptive decision-making [24]. However, this is the first study to extend the use of kiosks to provision of contraceptive prescriptions in acute care settings. Our 3-month follow-up of women who used this kiosk while seeking acute care showed that compared to women in the control group, women in the intervention group tended to have more accurate knowledge of the effectiveness of available contraceptives, more frequently reported contraceptive use, and fewer had experienced an unintended pregnancy. The trends we found in improved knowledge of contraceptive effectiveness in the intervention group at follow-up were similar to the effect sizes reported by studies that have had more power [16]; however, this study would have had to enroll five to seven times as many women to show these difference to be statistically significant. In addition, as the intervention module allowed women to choose which methods of birth control they wanted to learn about and the computer did not collect information about how much time a woman spent reviewing the computer’s educational offerings, we are unable to measure how much educational information each woman actually received; as we did not evaluate women’s contraceptive knowledge at baseline, we do not know if the intervention actually increased any of the women’s contraceptive knowledge. All outcomes were self-reported and women identified as having potential contraindications to the use of estrogen by the computer may not have had clinically-relevant contraindications. For example, the computer did not ask women to specify whether they had migraines with or without aura, and therefore likely over-identified women with headaches as having potential contraindications to the use of estrogen. Finally, we do not have data on how women who agreed to participate in this study may differ from those who did not. Likewise, women who completed the follow-up survey may not be fully representative of the women who enrolled in the study. We suspect that women who completed follow-up are more educated than the average woman seeking acute care, as 85% of women who completed follow-up had at least some college education.
In conclusion, the use of an interactive, patient-facing computer kiosk appears to be a feasible and acceptable way to increase women’s access to contraceptive prescriptions outside of traditional family planning settings. This approach offers advantages over websites that allow women to purchase hormonal contraception because such websites currently provide little or no screening for contraindications to the use of estrogen [25]; in contrast, this kiosk provides women with actionable information immediately prior to a clinical encounter with blood pressure measurement. Acute care settings frequently serve women at high risk of unintended pregnancy; thus, the implementation of such technology in settings with long waits for service may be particularly useful.
Acknowledgements
This study was funded by grant SFP2-8 from by the Society for Family Planning. Dr. Gonzales was supported by a grant from the California Health Care Foundation, and Dr. Tebb and the Chlamydia module were supported in part by grant R40MC08719 through the U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Research Program.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
A poster describing a preliminary analysis of this study data was presented at the North American Forum on Family Planning in Washington, DC on October 23, 2011, and a 15-min oral presentation of these findings was presented to the US Food and Drug Administration OTC Technologies public meeting on March 23, 2012.
References
- 1.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84:478–485. doi: 10.1016/j.contraception.2011.07.013. Epub 2011/10/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404. doi: 10.1016/j.contraception.2011.01.021. Epub 2011/04/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones RK, Darroch JE, Henshaw SK. Patterns in the socioeconomic characteristics of women obtaining abortions in 2000–2001. Perspect Sex Reprod Health. 2002;34:226–235. [PubMed] [Google Scholar]
- 4.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. Epub 2006/06/15. [DOI] [PubMed] [Google Scholar]
- 5.Walls CA, Rhodes KV, Kennedy JJ. The emergency department as usual source of medical care: estimates from the 1998 National Health Interview Survey. Acad Emerg Med. 2002;9:1140–1145. doi: 10.1111/j.1553-2712.2002.tb01568.x. Epub 2002/11/05. [DOI] [PubMed] [Google Scholar]
- 6.Schwarz EB, Gerbert B, Gonzales R. Need for emergency contraception in urgent care settings. Contraception. 2007;75:285–288. doi: 10.1016/j.contraception.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Akers AY, Gold MA, Borrero S, Santucci A, Schwarz EB. Providers' perspectives on challenges to contraceptive counseling in primary care settings. J Womens Health (Larchmt) 2010;19:1163–1170. doi: 10.1089/jwh.2009.1735. Epub 2010/04/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grossman D, Ellertson C, Abuabara K, Blanchard K, Rivas FT. Barriers to contraceptive use in product labeling and practice guidelines. Am J Public Health. 2006;96:791–799. doi: 10.2105/AJPH.2004.040774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grossman D, Fernandez L, Hopkins K, Amastae J, Garcia SG, Potter JE. Accuracy of self-screening for contraindications to combined oral contraceptive use. Obstet Gynecol. 2008;112:572–578. doi: 10.1097/AOG.0b013e31818345f0. Epub 2008/09/02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Curtis KM, Jamieson DJ, Peterson HB, Marchbanks PA. Adaptation of the World Health Organization's medical eligibility criteria for contraceptive use for use in the United States. Contraception. 2010;82:3–9. doi: 10.1016/j.contraception.2010.02.014. Epub 2010/08/05. [DOI] [PubMed] [Google Scholar]
- 11.Schwarz EB, Gerbert B, Gonzales R. Computer-assisted provision of emergency contraception: a randomized controlled trial. J Gen Intern Med. 2008 doi: 10.1007/s11606-008-0609-x. forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwarz EB, Gonzales R, Gerbert B. Computerized counseling about folate: a randomized trial. Contraception. 2007;76:170. [Google Scholar]
- 13.Centers for Disease C, Prevention. Peterson HB, Curtis KM, Jamieson D, et al. U S. Medical Eligibility Criteria for Contraceptive Use, 2010. MMWR Recomm Rep. 2010;59(RR-4):1–86. [PubMed] [Google Scholar]
- 14.World Health Organization. Medical eligibility criteria for contraceptive use. 4th edition. Geneva: Department of Reproductive Health and Research, World Health Organization; 2010. Reproductive Health and Research; p. 125. [Google Scholar]
- 15.Mosher WD, Jones J. Use of contraception in the United States, 1982–2008. Vital Health Stat 23. 2010;(29):1–44. Epub 2010/10/14. [PubMed] [Google Scholar]
- 16.Merki-Feld GS, Gruber IM. Intention to use a combined contraceptive method and decision after counselling in Switzerland - Swiss data from the European CHOICE study. Eur J Contracept Reprod Health Care. 2011 doi: 10.3109/13625187.2011.630114. Epub 2011/12/28. [DOI] [PubMed] [Google Scholar]
- 17.Merckx M, Donders GG, Grandjean P, Van de Sande T, Weyers S. Does structured counselling influence combined hormonal contraceptive choice? Eur J Contracept Reprod Health Care. 2011;16:418–429. doi: 10.3109/13625187.2011.625882. Epub 2011/11/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bitzer J, Gemzell-Danielsson K, Roumen F, Marintcheva-Petrova M, van Bakel B, Oddens BJ. The CHOICE study: Effect of counselling on the selection of combined hormonal contraceptive methods in 11 countries. Eur J Contracept Reprod Health Care. 2011;17:65–78. doi: 10.3109/13625187.2011.637586. Epub 2012/01/14. [DOI] [PubMed] [Google Scholar]
- 19.Lee JK, Parisi SM, Akers AY, Borrero S, Schwarz EB. The impact of contraceptive counseling in primary care on contraceptive use. J Gen Intern Med. 2011;26:731–736. doi: 10.1007/s11606-011-1647-3. Epub 2011/02/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lidegaard O, Nielsen LH, Skovlund CW, Skjeldestad FE, Lokkegaard E. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001–9. BMJ. 2011;343:d6423. doi: 10.1136/bmj.d6423. Epub 2011/10/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.White K, Potter JE, Hopkins K, Fernandez L, Amastae J, Grossman D. Contraindications to progestin-only oral contraceptive pills among reproductive-aged women. Contraception. 2012 doi: 10.1016/j.contraception.2012.01.008. Epub 2012/03/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwarz EB, Gerbert B, Gonzales R. Computer-assisted provision of emergency contraception a randomized controlled trial. J Gen Intern Med. 2008;23(6):794–799. doi: 10.1007/s11606-008-0609-x. Epub 2008/04/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwarz EB, Sobota M, Gonzales R, Gerbert B. Computerized counseling for folate knowledge and use: a randomized controlled trial. Am J Prev Med. 2008;35:568–571. doi: 10.1016/j.amepre.2008.06.034. Epub 2008/11/13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garbers S, Meserve A, Kottke M, Hatcher R, Ventura A, Chiasson MA. Randomized controlled trial of a computer-based module to improve contraceptive method choice. Contraception. 2012 doi: 10.1016/j.contraception.2012.01.013. Epub 2012/03/10. [DOI] [PubMed] [Google Scholar]
- 25.Memmel LM, Miller L, Gardner J. Over-the-internet availability of hormonal contraceptives regardless of risk factors. Contraception. 2006;73:372–375. doi: 10.1016/j.contraception.2005.10.001. Epub 2006/03/15. [DOI] [PubMed] [Google Scholar]