Abstract
Background Informal care givers support disabled stroke patients at home but receive little training for the caregiving role.
Objective To evaluate the effectiveness of training care givers in reducing burden of stroke in patients and their care givers.
Design A single, blind, randomised controlled trial.
Setting Stroke rehabilitation unit.
Subjects 300 stroke patients and their care givers.
Interventions Training care givers in basic nursing and facilitation of personal care techniques.
Main outcome measures Cost to health and social services, caregiving burden, patients' and care givers' functional status (Barthel index, Frenchay activities index), psychological state (hospital anxiety and depression score), quality of life (EuroQol visual analogue scale) and patients' institutionalisation or mortality at one year.
Results Patients were comparable for age (median 76 years; interquartile range 70-82 years), sex (53% men), and severity of stroke (median Barthel index 8; interquartile range 4-12). The costs of care over one year for patients whose care givers had received training were significantly lower (£10 133 v £13 794 ($18 087 v $24 619; €15 204 v €20 697); P = 0.001). Trained care givers experienced less caregiving burden (care giver burden score 32 v 41; P = 0.0001), anxiety (anxiety score 3 v 4; P = 0.0001) or depression (depression score 2 v 3; P = 0.0001) and had a higher quality of life (EuroQol score 80 v 70; P = 0.001). Patients' mortality, institutionalisation, and disability were not influenced by caregiver training. However, patients reported less anxiety (3 v 4.5; P < 0.0001) and depression (3 v 4; P < 0.0001) and better quality of life (65 v 60; P = 0.009) in the caregiver training group.
Conclusion Training care givers during patients' rehabilitation reduced costs and caregiver burden while improving psychosocial outcomes in care givers and patients at one year.
Introduction
It is estimated that 25-74% of stroke survivors require help with activities for daily living from informal care givers, often family members.1-3 Although the physical, psychological, emotional, and social consequences of care giving and its economic benefit to society are well recognised,4-7 care givers' needs are often given low priority in the management of stroke.8 Advances in stroke rehabilitation have successfully reduced severe disability and institutionalisation, which has increased the number of disabled patients living at home and being supported by care givers who feel inadequately trained, poorly informed, and dissatisfied with the extent of support available after discharge.9,10
Interventions to support stroke care givers by providing education, counselling, emotional support, or help with accessing services by using information packages, social workers, specialist nurses, or family support workers have shown little impact on patients and only modest improvements in psychological and social measures in care givers.11-15 This lack of effect may be because few interventions took into account the physical demands of caring for disabled patients,16 or because the outcome measures used were not sensitive to the effects of such interventions.17 Training care givers in skills essential for the day to day management of disabled stroke survivors is likely to have a role in reducing the burden of care but has not been investigated. We evaluated the effectiveness of caregiver training in reducing stroke costs and improving patient and caregiver outcomes. We describe clinical outcomes; economic analyses are described in an accompanying paper.18
Methods
Subjects
We undertook the study in stroke patients admitted to a stroke rehabilitation unit and their care givers. A care giver was defined as the main person (other than health, social, or voluntary care provider) helping with activities of daily living and advocating on behalf of the patient. Patients were included if they were independent in daily living activities before the stroke, medically and neurologically stable at the time of baseline assessments, and expected to return home with residual disability (defined as the need for supervision or physical assistance for core activities of daily living). Care givers were required to have no notable disability (defined as a Rankin score of 0-2) and be willing and able to provide support after discharge. We obtained informed consent from patients and care givers.
Baseline assessments and randomisation procedures
Researchers undertook baseline assessments before randomisation. Patients' assessments included demographics, stroke subtype,19 Barthel index,20 and estimations of premorbid function and quality of life; we used the Frenchay activity index20 and the EuroQol visual analogue scale.21 Caregiver assessments included details of demographics and accommodation, health profile, functional status, and quality of life assessments.
We used block randomisation procedures; each block included 10 subjects. We used computer generated random numbers to prepare the allocation schedule in advance. Allocation codes were held in a central office remote from the study environment. After baseline assessment the responsible assessor telephoned the randomisation office with patients' identification details only. A clerical worker entered these details on a computer database in strict referral order and was given patient allocation, which was relayed to the assessor.
Interventions
All patients were managed on a stroke rehabilitation unit with established multidisciplinary practice and received conventional care in accordance with existing guidelines.
Conventional care
This consisted of
Information on stroke and its consequences, prevention, and management options
Involvement in goal setting for rehabilitation and discharge planning
Encouragement to attend nursing and therapy activities to learn about patients' abilities and informal instruction on facilitating transfers, mobility, and activities of daily living tasks, and
Advice on community services, benefits, and allowances, including contact information for voluntary support services for care givers.
Care giver training
In addition to conventional support, care givers allocated to caregiver training received
Instruction by appropriate professionals on common stroke related problems and their prevention, management of pressure areas and prevention of bed sores, continence, nutrition, positioning, gait facilitation, and advice on benefits and local services, and
“Hands-on” training in lifting and handling techniques, facilitation of mobility and transfers, continence, assistance with personal activities of daily living and communication, tailored to the needs of individual patients.
Training started when patients' rehabilitation needs had stabilised and discharge was contemplated. Care givers received three to five sessions depending on need; each session lasted 30-45 minutes. We assessed care givers' competencies at the end of training. In addition the hospital team conducted a “follow through” session at home to adapt skills learnt to the home environment.
Assessment of outcome
An observer who did not participate in allocation or management of patients assessed outcome at three and 12 months after stroke onset. Most assessments were undertaken at home; patients and care givers were assessed separately wherever possible, and participants were encouraged to complete questionnaires themselves without prompts. Care givers were allowed to help patients who were unable to complete questionnaires without help.
Outcome measures for patients included death or institutionalisation, modified Rankin scale, Barthel index and Frenchay activities index for function, hospital anxiety and depression scale20 for mood, and EuroQol visual analogue scale for quality of life. We used the Frenchay activities index for function and social activities, hospital anxiety and depression scale and caregiver burden scale22 for emotional health, and EuroQol visual analogue scale for quality of life to measure outcomes for care givers. The modified Rankin score at one year was dichotomised to good outcome (score 0-2) and poor outcome (3-6). The Barthel index was similarly dichotomised; scores of > 18 were considered good. Patients and care givers were asked to complete a satisfaction questionnaire at 12 months.
Sample size calculation
The primary outcome measure for the study was the cost to health and social services during the first year of stroke. Sample size calculations were based on data indicating the cost of stroke care from the surveys of disability of the Office for Population Censuses and Surveys.23 The mean weekly cost for support at home after discharge varied between £89.15 (SD £11.15) ($158.99; €133.78) and £68.37 (SD £7.70), depending on the extent of caregiver support.23 The inclusion of 300 subjects would give the study 80% power to detect a 30% reduction in cost at the 5% significance level for unpaired comparisons. This sample size could also detect differences of 1 point in the Barthel index, 1.5 points in the Frenchay activities index, 1.5 points in the hospital anxiety and depression scale, 2.5 points in the EuroQol visual analogue scale, and 1 point in the caregiver burden scale.
Data analysis and statistical methods
We analysed the data on an intention to treat basis. For patients who had died or were lost to follow up we used the last completed datasets in further analyses. We calculated means, standard deviations, medians, and interquartile ranges as appropriate. We used the Mann-Whitney test to compare differences in medians of age, length of stay, therapy input, Barthel index, Frenchay activities index, and EuroQol. We used the χ2 test for discrete variables (for example, stroke subtype, mortality, institutionalisation, and the dichotomised modified Rankin scale and Barthel index). We used prospective and retrospective techniques described in the accompanying paper to collect data on use of resources from health and social services over one year.18 We report all costs as mean values, and we used the t test to undertake comparisons.
We undertook sensitivity analyses to examine the effects if all the missing values for carer burden and quality of life assessments were at the lower limit (worse outcome) and the higher limit (better outcome) of the interquartile range. Seventy five patients in each group received caregiver support consisting of a family worker who provided information on services, link with social agencies, advocacy, and emotional support for up to six months after discharge. We used regression analyses to assess the confounding effect of this and other baseline variables (such as age or extent of disability) on outcome.
Results
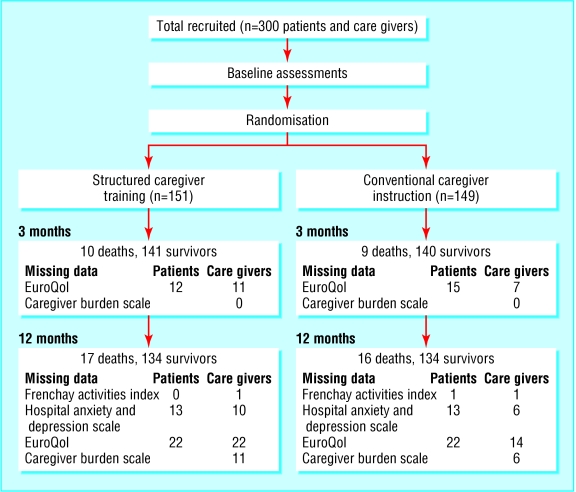
The figure shows the flowchart for the study. Of the 300 patients randomised, 33 patients died before completing the study. Deaths were distributed equally between allocations. Mortality, institutionalisation, and disability data were available for all patients. Data on the assessments according to the Frenchay activities index, hospital anxiety and depression scale, EuroQol, and caregiver burden scale were missing or incomplete in some, but not the same, patients and care givers. Reasons for non-completion of assessments included communication problems in patients and perceived lack of relevance, lack of time, fatigue, or disinclination in patients and care givers. We included in the analyses only completed assessments at each time point (figure).
Figure 1.
Flow of participants through the trial
Baseline characteristics were similar between patients randomised to caregiver training and control groups (table 1). The spouse was the main care giver in two thirds of patients; 95% of patients had additional family support. Eighty per cent of patients owned their homes, and < 5% had input from social services before stroke. The median score on the Barthel index at one week placed both groups above moderately disabled level.
Table 1.
Baseline characteristics of 300 patients and controls randomised to caregiver training and no training in the study
| Patients (n=151) | Controls (n=149) | |
|---|---|---|
| Participants' characteristics | ||
| Median age in years (interquartile range) | 76 (70-80) | 76 (70-82) |
| Male sex | 86 | 74 |
| Median Barthel index at 1 week (interquartile range) | 8 (4-12) | 8 (4-12) |
| No with stroke subtype | ||
| Lacunar syndrome | 51 | 52 |
| Total anterior circulation syndrome | 74 | 73 |
| Partial anterior circulation syndrome | 16 | 14 |
| Posterior circulation syndrome | 10 | 10 |
| Premorbid functional status | ||
| Median Frenchay activities index (interquartile range): | ||
| In patients | 25 (20-29) | 24 (21-29) |
| In care givers | 27 (24-32) | 28 (25-32) |
| Median EuroQol score (interquartile range): | ||
| In patients | 85 (75-90) | 85 (75-95) |
| In care givers | 90 (80-95) | 85 (80-90) |
| Environment and support (No of patients) | ||
| Social services | 6/151 | 8/149 |
| Home owner | 116/151 | 122/149 |
| Main care giver—spouse | 98/151 | 97/149 |
| Additional family support | 143/151 | 142/149 |
We found no significant differences in mortality, institutionalisation, or functional abilities between the training and control group (table 2). Patients whose care givers had received training reported significantly improved quality of life and mood outcomes, both at three and at 12 months. Burden of care was reduced significantly and quality of life and mood in care givers improved significantly at three and 12 months. Functional activities (Frenchay activities index) were not affected (table 3). Regression analyses showed that training care givers had a highly significant effect on caregiver burden score, EuroQol, and hospital anxiety and depression score at 12 months, which was independent of age, stroke severity, extent of disability, and caregiver support. Sensitivity analyses for different assumptions of carer burden and quality of life outcomes showed a relatively small effect on median caregiver burden and EuroQol scores, but the difference between the training and non-training groups remained significant. The proportion of care givers who were satisfied with rehabilitation (45% v 58%; P = 0.001) and instruction in looking after the patient (75% v 36%; p = 0.001) was higher in those receiving training.
Table 2.
Health outcomes for patients included in the study.
| Outcome measure | Range (bad to good) | Training (n=151) | Missing data | No training (n=149) | Missing data | P value |
|---|---|---|---|---|---|---|
| Mortality: | ||||||
| 3 months | — | 9 | 0 | 9 | 0 | 0.98 |
| 12 months | — | 16 | 0 | 16 | 0 | 0.88 |
| Institutionalisation: | ||||||
| 3 months | — | 4 | 0 | 9 | 0 | 0.076 |
| 12 months | — | 2 | 0 | 6 | 0 | 0.071 |
| Mortality or institutionalisation: | ||||||
| 3 months | — | 13 | 0 | 18 | 0 | 0.21 |
| 12 months | — | 18 | 0 | 22 | 0 | 0.38 |
| Modified Rankin score 0-2: | ||||||
| 3 months | — | 80 | 1 | 63 | 0 | 0.054 |
| 12 months | — | 100 | 1 | 87 | 0 | 0.18 |
| Barthel index >18: | ||||||
| 3 months | — | 77 | 0 | 52 | 0 | 0.007 |
| 12 months | — | 93 | 0 | 75 | 0 | 0.074 |
| Median Frenchay activities index at 1 year (interquartile range) | 0-45 | 15 (9-23) | 0 | 16 (8-22) | 1 | |
| Median hospital anxiety and depression score at 1 year (interquartile range): | ||||||
| Anxiety | 21-0 | 3 (2-4) | 13 | 4.5 (4-6) | 13 | 0.0001 |
| Depression | 21-0 | 3 (2-4) | 13 | 4 (2-5.5) | 13 | 0.0001 |
| Median score on EuroQol visual analogue scale (interquartile range): | ||||||
| 3 months | 0-100 | 60 (42-70) | 12 | 50 (40-90) | 15 | 0.019 |
| 1 year | 0-100 | 65 (55-80) | 22 | 60 (41-80) | 22 | 0.009 |
Table 3.
Outcomes for care givers allocated to training and no training groups
| Outcome measure | Range (bad to good) | Training (n=151) | Missing data | No training (n=149) | Missing data | P value |
|---|---|---|---|---|---|---|
| Caregiver burden scale: | 88-22 | |||||
| 3 months | 43 (36-54) | 0 | 51 (41-62) | 0 | 0.0001 | |
| 12 months | 32 (27-41) | 11 | 41 (36-50) | 6 | 0.0001 | |
| Median Frenchay activities index at 1 year (interquartile range) | 0-45 | 27 (23-30) | 1 | 26 (24-30) | 1 | 0.43 |
| Median hospital anxiety and depression score at 1 year (interquartile range): | ||||||
| Anxiety | 21-0 | 3 (2-4) | 10 | 4 (3-6) | 6 | 0.0001 |
| Depression | 21-0 | 2 (1-3) | 10 | 3 (2-5) | 6 | 0.0001 |
| Median EuroQol visual analogue score (interquartile range): | ||||||
| 3 months | 0-100 | 80 (71-90) | 11 | 70 (60-80) | 7 | 0.0001 |
| 1 year | 0-100 | 80 (70-90) | 22 | 70 (60-80) | 14 | 0.0001 |
Caregiver training was associated with significant cost reductions over one year (£10 133 (SD £8676) v £13 794 (SD £10 510); P = 0.001), mainly because of lower hospital costs (£8987 (SD £7368) v £12 383 (SD £9104)). Although non-hospital costs in the 12 months after stroke (£1145 (SD £2553) v £1411 (SD £2742)) were similar, a trend towards lesser use of personal, domestic, and respite care became obvious in the training group. Detailed cost analyses have been presented in the accompanying paper.18
Discussion
Training care givers in basic skills of moving and handling, facilitation of activities of daily living, and simple nursing tasks reduces burden of care and improves quality of life in patients and care givers. Improvements in care givers' emotional health and quality of life with training have been described with education and family support12-15 and seem to be a generic response to most caregiver interventions. Caregiver training has additional advantages of reducing the costs of stroke care and improving patients' quality of life. A higher proportion of patients achieved independence at an earlier stage (table 2), which contrasts with previous reports of no, or even adverse, effects on patients.14,15
An important aspect of stroke rehabilitation is to bridge the gap between patients' or care givers' expectations of recovery and residual disability to promote overall wellbeing of patients and their families. One method of capturing wellbeing is to assess quality of life and several different measures have been used, all with various limitations.24 Although the practical importance of the effects of any intervention on quality of life can be difficult to interpret, moderate differences in average scores can mask large biological effects.15,25 The significant improvements in quality of life scores associated with caregiver training are likely to indicate an important effect that has implications for clinical practice.
Limitations of the study
The findings of the study need to be interpreted in the context of its limitations. It is not possible to blind observers in such trials fully because interactions during assessment with patients or care givers, who are aware of the training received, may disclose allocation. We kept observer bias to a minimum by using observers not involved with allocation, interventions, or patients' care. In addition we used robust, well validated, and objective outcome measures (Rankin scale, Barthel index, Frenchay activities index) and encouraged self completion of various subjective assessments (caregiver burden scale, hospital anxiety and depression scale, EuroQol) without prompts. This may have contributed to missing data on some assessments (tables 2 and 3), which is another potential source of bias. Sensitivity analyses to examine the effects of missing data showed that findings remained robust for worse or better outcome assumptions.
Generalisability of results
The study was undertaken in a largely middle class suburban area, and an interaction between the acceptability of interventions and education, affluence, living accommodation, informal support, and cultural beliefs is possible. Patients and care givers who chose to participate were likely to be fit, motivated, and enthusiastic, and hence most likely to benefit from these interventions. The generalisability of these interventions to other settings where the structures of the population, health and social care, and the economy are different, needs to established.
Outlook
It is common practice to involve care givers in setting goals and planning discharge in stroke rehabilitation. The time may be ripe to use a structured programme of activities under professional supervision during inpatient rehabilitation, to empower consenting informal care givers in their future role by teaching them appropriate skills.
What is already known on this topic
Interventions to support stroke care givers by using information packages, specialist nurses, or family support workers have little impact on patients and modest psychological or social benefits for care givers
What this study adds
Training care givers in basic nursing, moving, and handling and facilitation of activities of daily living is feasible during stroke rehabilitation
Training care givers significantly reduces their burden, anxiety, and depression and improves quality of life and satisfaction with care among care givers at three and 12 months
Patients whose care givers received training reported better quality of life and psychological outcomes at three and 12 months
Patients' mortality, institutionalisation, and disability were not influenced by caregiver training
Supplementary Material
 The CONSORT table is on bmj.com
The CONSORT table is on bmj.com
We acknowledge the contributions made by all hospital, general practice, community health, and social services staff to the project. Particular thanks are owed to Shirley Law and Caroline Oates of the Carer Information and Support Services in Bromley and to Jayne Steadman, Judith Eade, and Magreet Whittink, who participated in the caregiver training programme.
Contributors: LK was responsible for the conception, design, initiation, and overall coordination of the study; and for analysis and interpretation of data, drafting of the paper, and its intellectual content. AE and AP were responsible for analysis and interpretation of data and writing of the paper. IP and AM were involved with data collection, collation, and writing of the paper. MK was involved in the conception and design of the study, interpretation of data and critical review of the paper. ND provided statistical input to the design, data analysis, interpretation and writing of the paper. LK is the guarantor.
Funding: NHS R&D Executive's Primary Secondary Interface Priority Programme (Project No: F-4/1997).
Competing interests: None declared.
Ethical approval: Bromley Research Ethics Committee (LREC/106).
References
- 1.Anderson CS, Linto J, Stewart-Wynne EG. A population based assessment of the impact and burden of care-giving for long-term stroke survivors. Stroke 1995;26: 843-9. [DOI] [PubMed] [Google Scholar]
- 2.Bosanquet N, Franks P. Stroke care: reducing the burden of disease. London: Stroke Association, 1998.
- 3.Dewey HM, Thrift AG, Mihalopoulos C, Carter R, Macdonell RA, McNeil JJ, et al. Informal care for stroke survivors: results from the North East Melbourne stroke incidence study (NEMESIS). Stroke 2002;33: 1028-33. [DOI] [PubMed] [Google Scholar]
- 4.Wade DT, Legh-Smith J, Hewer RL. Effects of living with and looking after survivors of a stroke. BMJ 1986;293: 418-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scholte op Reimer WJ, de Haan RJ, Rijnders PT, Limburg M, van den Bos GA. The burden of caregiving in partners of long-term stroke survivors. Stroke 1998;29: 1605-11. [DOI] [PubMed] [Google Scholar]
- 6.Low JT, Payne S, Roderick P. The impact of stroke on informal carers: a literature review. Soc Sci Med 1999. Sep;49: 711-25. [DOI] [PubMed] [Google Scholar]
- 7.Persson U, Silverberg R, Lindgren B, Norrving B, Jadback G, Johansson B, et al. Direct costs of stroke for a Swedish population. Int J Technol Assess Health Care 1990;6: 125-37. [DOI] [PubMed] [Google Scholar]
- 8.Kerr SM, Smith LN. Stroke: an exploration of the experience of informal caregiving. Clin Rehabil 2001;15: 428-36. [DOI] [PubMed] [Google Scholar]
- 9.Wellwood I, Dennis MS, Warlow CP. Patients' and carers' satisfaction with acute stroke management. Age Ageing 1995;24: 519-24. [DOI] [PubMed] [Google Scholar]
- 10.Simon C, Kendrick T. Community provision for informal live-in carers of stroke patients. Br J Community Nurs 2002;7: 292-8. [DOI] [PubMed] [Google Scholar]
- 11.Friedland JF, McColl M. Social support interventions after stroke: results of a randomised trial. Arch Phys Med Rehabil 1992;73: 573-81. [PubMed] [Google Scholar]
- 12.Forster A, Smith J, Young J, Knapp P, House A, Wright J. Information provision for stroke patients and their caregivers. Cochrane Database Syst Rev 2001;(3): CD001919. [DOI] [PubMed]
- 13.Forster A, Young J. Specialist nurse support for patients with stroke in the community: a randomised controlled trial. BMJ 1996;312: 1642-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dennis M, O'Rourke S, Slattery J, Staniforth T, Warlow C. Evaluation of a stroke family care worker: results of a randomised controlled trial. BMJ 1997;314: 1071-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mant J, Carter C, Wade DT, Winner S. Family support for stroke: a randomised controlled trial. Lancet 2000;356: 808-13. [DOI] [PubMed] [Google Scholar]
- 16.van den Heuvel ET, de Witte LP, Schure LM, Sanderman R, Meyboom-de Jong B. Risk factors for burn-out in caregivers of stroke patients, and possibilities for intervention. Clin Rehabil 2001;15: 669-77. [DOI] [PubMed] [Google Scholar]
- 17.Duncan PW, Jorgensen HS, Wade DT. Outcome measures in acute stroke trials: A systematic review and some recommendations to improve practice. Stroke 2000;31: 1429-38. [DOI] [PubMed] [Google Scholar]
- 18.Patel A, Knapp M, Evans A, Perez I, Kalra L. Training care givers of stroke patients: economic evaluation. BMJ 2004;328: 1102-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 1991;337: 1521-6. [DOI] [PubMed] [Google Scholar]
- 20.Wade DT. Measurement in neurological rehabilitation. Oxford: Oxford University Press, 1992.
- 21.The EuroQol Group. EuroQol: a new facility for the measurement of health related quality of life. Health Policy 1990;16: 199-208. [DOI] [PubMed] [Google Scholar]
- 22.Robinson BC. Validation of a caregiver strain index. J Gerontol 1983;38: 344-8. [DOI] [PubMed] [Google Scholar]
- 23.Kavanagh S, Knapp M, Patel A. Costs and disability among stroke patients. J Public Health Med 1999;21: 385-94. [DOI] [PubMed] [Google Scholar]
- 24.Higginson IJ, Carr AJ. Measuring quality of life: using quality of life measures in the clinical setting. BMJ 2001;322: 1297-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guyatt GH, Juniper EF, Walter SD, Griffith LE, Goldstein RS. Interpreting treatment effects in randomised trials. BMJ 1998;316: 690-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.