Abstract
Background: Comprehensive health care is becoming an important issue; however, little is known about the complex relationships between perceived family support, self-rated health, and psychological distress in mixed middle-aged/older primary care patient samples.
Method: In this cross-sectional and predominantly male sample of 137 patients attending their appointments at a primary care clinic in a Department of Veterans Affairs Medical Center, participants completed several questionnaires including the Family Adaptation, Partnership, Growth, Affection, and Resolve; the General Health Questionnaire-12; the Symptom Checklist-10; and the Primary Care Evaluation of Mental Disorders (PRIME-MD) screening questionnaire and interview. Data were collected in 1998. Eighteen percent of the participants were diagnosed with a mood disorder, and 15% were diagnosed with an anxiety disorder (PRIME-MD diagnoses).
Results: Perceived family support and self-rated health were negatively associated with psychological symptoms and certain psychological disorders, while perceived family support and self-rated health were positively rated. In addition, the interaction between perceived family support and self-rated health was significant (p < .01) in relating to psychological symptoms such that psychological symptoms were most elevated in participants reporting dissatisfying family support combined with poor self-rated health. However, the cross-sectional nature of the study prevents causal conclusions from being made.
Conclusions: Physicians and other health care professionals are encouraged to assess both the perceived family support and self-rated health in an effort to conceptualize their patients' problems in a more comprehensive manner.
Family support is an important factor in conceptualizing primary care patient problems. Numerous examples of how the family system determines the course of chronic illness have been influential in the development of collaborative medical care.1–6 Family factors such as perceived family support and illnesses, either physical or psychological, may influence each other in a bidirectional fashion.4,7 Similarly, negative marital perceptions (e.g., spousal support) have been related to clinical depression.8,9 Thus, the assessment of family support might be used to further assess the risk of psychological distress in primary care. Gathering these data may enhance working relationships with patients, ease patients' acceptance of referrals to mental health services, and help physicians and residents become more skilled in conceptualizing patient problems in a comprehensive manner.
However, before strong recommendations can be made for the assessment of family support in older primary care patients, several issues must be examined. First, it is unclear whether family support relates to some measures of psychological distress but not to others. Some measures only assess psychological distress whereas others include an assessment of somatic symptoms. Measures also differ on the response format (e.g., presence of symptoms vs. severity of symptoms) and timeframe (e.g., last week vs. last month). If a distress measure is not correlated with family support, it is possible for health care professionals to incorrectly assume that patients are at risk for psychological distress because they report that they are unhappy or dissatisfied with the support their family provides to them (i.e., dissatisfying family support). Second, little is known about the relationship between dissatisfying family support and distress in samples consisting of a large proportion of older patients. Perhaps this is a phenomenon that is limited to more youthful samples. Third, the effect of family support on emotional distress may vary depending on patients' self-rated health. Perceptions of good health may buffer the effects of dissatisfying family support, and measures of self-rated health may help physicians make comprehensive judgments of risk.
Research on Family Support and Psychological Distress
A number of studies provide some support for the theoretical relationship between perceived family support and mental health. The quantity and quality of family support are inversely related to psychological symptoms.10,11 Some studies have indicated that persons with psychiatric disorders also report more dissatisfying family support than those without diagnoses.12,13 Other research has shown that family support is not related to psychological symptoms or diagnoses.14 Diverse psychological symptom measures were used across these studies, thereby calling into question whether family support is related to only some types of psychological symptoms. To examine this issue, we used 3 different measures of psychological distress that inquire about different kinds of symptoms with different response formats as well as a diagnostic interview designed to assess clinically significant psychological disorders. Previous findings with these measures have shown that all 3 measures can be used with some degree of accuracy in screening for mental disorders.15
Self-Rated Health
In the present study, we also examined a more complex relationship between perceived family support and psychological distress by including an assessment of self-rated health. Self-rated health is a dynamic representation of overall health that includes the patient's knowledge of current and past medical problems, current frailty, and health changes over time.16–18 Because self-rated health is often measured with a single item, it is an easily administered assessment tool in clinic settings. Poor self-rated health is related to an increased risk of mortality, even when a variety of health indicators are controlled for.19,20 Self-rated health is also an important correlate of mental disorders,21–23 elevated psychological symptoms,24 and dissatisfying family support.16–25
Although self-rated health, family support, and psychological distress have been found to correlate with each other, more complex associations between these variables have not been explored. The risk for psychological distress may increase as one makes negative appraisals about more than one area of life26; in this case, health and family. However, no published studies have tested the hypothesis that family support and self-rated health might interact in relating to psychological distress. Patients with poor self-rated health and dissatisfying family support might report more psychological distress than individuals who are protected by either good self-rated health or satisfying family support.26 Support for this hypothesis would provide health care professionals with an extension of the theoretical and empirical literature, a more comprehensive view of patients, and another way of identifying at-risk patients.
Hypotheses
Following the existing theory and research, we hypothesized that dissatisfying family support would be related to elevated psychological distress and psychiatric diagnoses using several different measures of distress. We also expected that self-ratings of health interact with family support in correlating with psychological symptoms such that dissatisfying family support in the presence of poor self-rated health would be associated with elevated psychological symptoms and diagnoses. Whereas the research on the univariate association between self-rated health and distress in older samples has been extensive,18 only a few studies have shown that family and other social supports are associated with less severe depression, regardless of age.27,28 To date, no studies have been conducted on the interaction between family support and self-rated health in older primary care patients. For this reason, we examine our hypotheses in a cross-sectional, mixed sample of middle-aged and older patients visiting a Veterans Affairs clinic.
METHOD
Participants
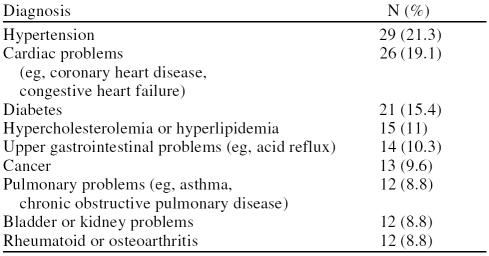
Participants were 137 patients attending primary care appointments at a large upstate New York Department of Veterans Affairs Medical Center (Syracuse, N.Y.). The study was approved by an institutional review board. Data were collected in 1998. The mean age of patient participants was 63.71 years (SD = 12.98). The sample was predominantly male (97.08%; N = 133). In terms of marital status, 58.8% (N = 80) were married at the time of the study, 18.4% (N = 25) were separated or divorced, 12.5% (N = 17) were widowed, and 9.6% (N = 13) were never married. One participant did not disclose marital status. Thirty participants (22.1%) had combat experience, while 2.2% (N = 3) were former prisoners of war (POWs). One paticipant did not give information on combat experience. Combat and POW status were not associated with psychological distress, perceived family support, or self-rated health. One hundred twenty-two participants (89.1%) reported attending at least 1 medical appointment in the year prior to participation, whereas only 14.6% (N = 20) of participants utilized outpatient mental health services in the year prior to participation. Participants' medical diagnoses are shown in Table 1. These medical diagnoses were not necessarily addressed at each of the medical appointments that were attended in the past year.
Table 1.
Medical Problems Recorded in Participants' Charts
Procedure
A full description of the procedure and the measures used can be found in Cano et al.15 A mental health technician approached potential participants while they were awaiting their primary care appointments. Patients who agreed to participate completed a consent form, the Family Adaptation, Partnership, Growth, Affection, and Resolve (APGAR),29,30 the Primary Care Evaluation of Mental Disorders (PRIME-MD) questionnaire,31 the General Health Questionnaire-12 (GHQ-12),32 and the Symptom Checklist-10 (SCL-10).33,34 Patients were administered the PRIME-MD interview by a mental health technician on the basis of their responses on the PRIME-MD questionnaire. Data on health care use and medical diagnoses were obtained from participants' charts. Since no data were collected on the patients who declined to participate in the study, no comparisons could be made between participants and patients who declined to participate.
Measures
Family Adaptation, Partnership, Growth, Affection, and Resolve.
The APGAR is a 5-item measure of perceived family support that was designed as an assessment tool for physicians.29,30 The APGAR was chosen for this study because it measures a theoretically important construct in a brief and easily administered format. Family physicians trained in lengthier methods of assessment (e.g., the McMaster Model of Family Functioning35) are unlikely to use them in actual practice36 and reported that they were simply too busy to use such a protracted and costly approach.37 Even more recent approaches that rely on patient self-report, such as the Family Profile,38 can be time-consuming and therefore less likely to be used than a brief measure such as the APGAR.
The APGAR has distinguished between patients with and without family distress,39 with lower scores indicating less satisfying perceived family support. A sample item of the scale includes the statement “I am satisfied that I can turn to my family for help when something is troubling me.” In this article, we refer to lower scores on this scale as indicating “dissatisfying family support.” “Unsatisfying support” implies that the individual perceives the support in a categorical manner (i.e., unsatisfying vs. satisfying), which is incorrect because of the Likert-type response format. Participants responded to each item using a 5-point rating scale ranging from 0 (never) to 4 (always), as detailed in the research version of the scale.30 The current sample reported a mean APGAR score of 15.28 (SD = 5.09; range, 0–22). The inter-item reliability for the current study was .93, indicating excellent reliability.
General Health Questionnaire-12.
The GHQ-12 was developed to assess psychological symptoms.32 Participants noted the presence or absence of 12 symptoms within the past few weeks. This measure has been used in large cross-cultural studies and is correlated with psychiatric disorders in primary health care settings.32,40 Participants reported a mean of 2.07 (SD = 3.04) symptoms. The current interitem reliability was .90.
Symptom Checklist-10.
The SCL-10 is a 10-item instrument that Nguyen et al.33 derived from the SCL-90.34 Each item describes the psychological distress experienced within the past week using a 0 (not at all) to 5 (extremely distressed) scale. A single global score may be used as an index of psychopathology or psychological distress.33 The interitem reliability of the SCL-10 was excellent in the current study (α = .92), and the mean SCL-10 score was 5.50 (SD = 7.84).
Primary Care Evaluation of Mental Disorders.
The PRIME-MD is a 2-step psychiatric diagnostic instrument designed for use in primary care settings.31 The first step consists of a 26-item screening questionnaire that measures psychological (10 items) and somatic (15 items) symptoms that may be signs of psychological disorders as well as self-rated health (1 item) within the past month. The second step consists of a diagnostic interview conducted by a trained interviewer only if specific clusters of symptoms are endorsed on the questionnaire. The PRIME-MD has been validated in a sample of 1000 patients.31
The mean number of PRIME-MD symptoms reported by participants was 5.24 (SD = 4.31; range, 0–17). The interitem reliability for self-report PRIME-MD symptoms was excellent at .85. Approximately 14.3% (N = 19) of patients were diagnosed with more than 1 psychiatric disorder. Diagnoses were as follows: 18.0% (N = 24) were diagnosed with a mood disorder, 15.0% (N = 20) were diagnosed with an anxiety disorder, 7.5% (N = 10) were diagnosed with a somatoform disorder, and 1.5% (N = 2) were diagnosed with an eating disorder. For ease of interpretation, the terms PRIME-MD symptoms and PRIME-MD questionnaire are used when referring to the continuous measure of symptoms, whereas PRIME-MD diagnosis is used when describing the categorical diagnoses.
Self-rated health was assessed on the PRIME-MD by 1 item asking participants to rate their overall health from 1 (poor) to 5 (excellent) (mean = 2.99, SD = 1.00; range, 1–5). Single item scales of self-rated health are commonly used in the literature with powerful results.16,18,41 The modest correlation between self-rated health and the number of medical diagnoses reported in participants' charts (r = −0.28, p < .001) supports the notion that self-rated health is not solely a reflection of current medical problems.
Analysis Plan
Four participants did not complete every measure used in the study; therefore, N = 133 for all analyses. To test the first hypothesis that family support would be related positively to psychological distress, Pearson product moment correlations were conducted between family support and the 3 psychological distress measures. In addition, analyses of variance were conducted to determine whether patients with PRIME-MD diagnoses perceived less satisfying family support as compared with patients without these diagnoses.
Multiple regression was used in analyses involving the 3 symptom measures (i.e., continuous dependent variables), and logistic regression was used in analyses involving diagnoses (i.e., dichotomous dependent variables). The first step of the regression consisted of the covariate of age, which was correlated with the GHQ-12, SCL-10, and PRIME-MD questionnaire (p < .001 for each comparison). Participants with a PRIME-MD diagnosis were significantly younger than participants without a diagnosis (p < .0001). The second step included the APGAR and self-rated health. The third step included the interaction term between these 2 variables (i.e., APGAR multiplied by self-rated health). Hierarchical regression was used to test whether the interaction term contributed significantly to the variance in psychological distress beyond the main effects of family support and self-rated health. The standard error (SE) was used to calculate a confidence interval around b. Comparisons (t tests) were also run to determine the nature of significant interactions. A more stringent significance level (p < .01) was used to control for type I error in the comparisons. Because the analyses were similar when conducted separately for men and for women, men and women are combined in the following analyses. It should be noted that the analyses cannot prove a causal relationship because the data are cross-sectional.
RESULTS
Family Support and Psychological Distress
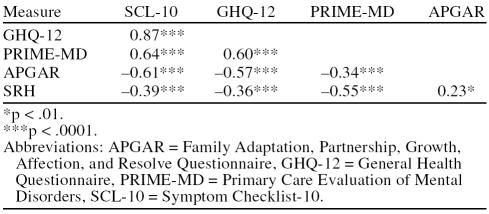
First, we tested the hypothesis that perceptions of dissatisfying family support would be related to elevated psychological symptoms and psychiatric disorders. As expected, correlations showed that dissatisfying family support was associated with elevated psychological symptoms on all 3 symptom measures (Table 2). These results suggest that this relationship is not specific to the measure used. These correlations were not significantly different from one another. Furthermore, poorer self-rated health was related to dissatisfying family support and elevated psychological symptoms (see Table 2).
Table 2.
Pearson Product Moment Correlations Between the GHQ-12, SCL-10, PRIME-MD Questionnaire, APGAR, and Self-Rated Health (SRH)
Analyses of variance showed that patients diagnosed with anxiety disorders reported less family support satisfaction (APGAR; mean = 11.50, SD = 6.45) than patients without anxiety disorders (mean = 16.08, SD = 5.46; F = 15.08, df = 1,131; p < .001). Similarly, patients with mood disorders reported lower APGAR scores (mean = 10.88, SD = 6.82) than patients without mood disorders, (mean = 16.39, SD = 4.06; F = 27.41, df = 1,131; p < .0001). Somatoform disorder was not related to family support (p > .35), possibly due to the low frequency of somatoform disorders. More PRIME-MD diagnoses were also correlated with lower APGAR scores (r = −0.46, p < .0001).
Family Support, Self-Rated Health, and Psychological Distress
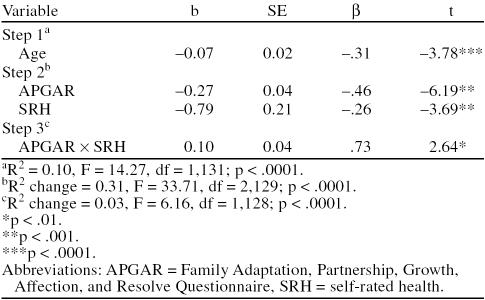
A series of hierarchical regressions were conducted to test the second hypothesis that family support would interact with self-rated health in relating to psychological distress. An examination of the unstandardized coefficients (b) shows how many units of change can be observed in the dependent variable for each unit change in the independent variable. For instance, if age and family support are accounted for, a 1-point decrease in self-rated health will result in a 0.79-point increase in GHQ-12 score (Table 3).
Table 3.
Hierarchical Regression Analyses: General Health Questionnaire-12
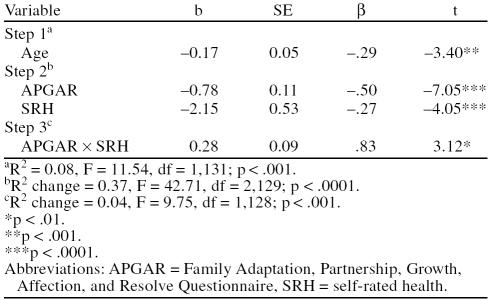
Analyses showed a significant interaction between family support and self-rated health on the GHQ-12 and the SCL-10 psychological distress measures (Tables 3 and 4). T tests showed that participants with dissatisfying family support (i.e., APGAR score lower than the median score of 17) and poor self-rated health (i.e., self-rated health score less than the median score of 3) reported significantly more psychological distress on the GHQ-12 and SCL-10 than participants with (1) satisfying family support and poor self-rated health and (2) satisfying family support and excellent self-rated health (p < .01 for both comparisons).
Table 4.
Hierarchical Regression Analyses: Symptom Checklist-10
In addition, participants who reported poor self-rated health and dissatisfying family support reported significantly more SCL-10 symptoms than participants with dissatisfying family support and excellent self-rated health (p < .01). There was a trend for a similar relationship on the GHQ-12 (p < .03). Among the participants with satisfying family support, self-rated health did not relate to psychological symptoms on the SCL-10 or GHQ-12 (p > .20 for both comparisons). Although the interaction was not significant for PRIME-MD symptoms (p > .20), the main effect of self-rated health was significant (b = −2.23, SE = 0.30, β = −0.52, t = −7.43, p < .001), whereas the main effect of family support approached significance (b = −0.12, SE = 0.06, β = −0.14, t = −1.86, p < .07). These results indicate that poorer self-rated health statistically contributed independently to PRIME-MD symptoms after controlling for age.
With regard to diagnoses, dissatisfying family support and poor self-rated health were related to mood disorders (family support, B = −0.14, SE = 0.05, Wald statistic = 7.38, Exp [B] = 0.87 [CI = 0.79 to 0.96], p < .01; and self-rated health, B = −1.07, SE = 0.34, Wald statistic = 10.14, Exp [B] = 0.35 [CI = 0.18 to 0.66], p < .001), after controlling for age. The Wald statistic is a measure of effect size, and Exp (B) is the odds ratio. Only the main effect for self-rated health was significant for anxiety disorders (b = −0.94, SE = 0.33, Wald statistic = 7.95, Exp [B] = 0.39 [CI = 0.20 to 0.75], p < .01). In other words, dissatisfying family support was positively correlated with mood disorders, and poor self-rated health was positively correlated with mood as well as anxiety disorders. The interaction between APGAR score and self-rated health was not associated with mood or anxiety disorders, indicating that family support did not buffer the effects of poor self-rated health on distress. For mood disorders, the Wald statistic for the interaction was 0.22 (Exp [B] = 0.97 [CI = 0.87 to 1.09], p > .63). For anxiety disorders, the Wald statistic for the interaction was 0.25 (Exp [B] = 1.03 [CI = 0.92 to 1.16], p > .61). Neither main effects nor interactions were significant for somatoform disorders.
DISCUSSION
This study investigated satisfaction with family support as one aspect of family functioning that may be particularly important in conceptualizing patients' problems. As expected, patients' perceptions of dissatisfying family support were significantly related to elevated psychological distress regardless of the symptom measure used. In addition, dissatisfying family support was significantly related to mood and anxiety disorders. These were important findings for 2 reasons. First, the results replicated the findings of previous studies that relied on younger, non-military veteran samples,10–13 suggesting that the link between family support and psychological distress is not dependent on the age or civilian status of the sample. Second, the current findings also show that the relationships between family support and distress are not limited to 1 specific self-report questionnaire or to questionnaires in general. By using 3 psychological distress measures and a diagnostic interview, we were able to show that family support relates to the presence and the severity of psychological and somatic symptoms experienced in a recent time period (e.g., past month vs. past week) as well as clinically significant mood and anxiety disorders. Determining the causal nature of these associations was not a goal of this study; however, it may prove useful to conduct longitudinal research on family support and psychological distress in primary care settings to more fully understand the reciprocal relationships between these variables over time.
We extended existing research that demonstrated the independent statistical contributions of family support and self-rated health to psychological symptoms.10–13,22,23,25 Some might argue that self-rated health is merely another measure of psychological distress or physical health. However, our findings that self-rated health only moderately correlated with medical diagnoses and psychological distress support claims that self-rated health is a cognitive representation or perception of health.16–18
We also found that patients who perceived dissatisfying family support and who rated their health status as poor reported the most psychological distress on the SCL-10 and GHQ-12. However, participants with satisfying family support, regardless of their self-rated health, reported little psychological distress. These results make sense from family function perspectives,4,7 cognitive-behavioral and interpersonal models of depression,8,9 and behavioral medicine perspectives.26 The perception that family members are reliable helpers might minimize the effect of physical illness on psychological distress. Conversely, perceiving deficiencies in health and family support may lead to hopelessness, decreased family interaction, and decreased pleasant activities. These cognitions and behaviors may then lead to distress.
As noted in the Method, there were differences in response time frames (e.g., past month vs. past week), response choices (e.g., presence or absence vs. severity), and types of symptoms (psychological vs. psychological and somatic). Findings with the GHQ-12 and SCL-10 were essentially similar; however, analyses with the more somatic PRIME-MD questionnaire sometimes resulted in different findings. For instance, satisfying family support did not protect participants with poor self-rated health from experiencing elevated somatic complaints. If symptoms on the PRIME-MD reflect physical rather than psychological distress, then the protection offered by family support may be limited to psychological distress.
In sum, we believe that the current study has contributed to the existing knowledge by providing an in-depth analysis of the role of family support and self-rated health in psychological distress. Our results suggest that both perceived family support and health status (i.e., a total of 6 patient-rated items) can be used to assess patients' risk for psychological distress to identify primary care patients for appropriate referrals and provide comprehensive health care. Patients with dissatisfying family support (i.e., research APGAR scores < 17) and poor self-rated health (i.e., self-rated health scores < 3) are particularly at risk. High-risk patients could, then, be administered brief measures of psychological distress (e.g., GHQ-12 or SCL-10) in a stepwise fashion. Alternatively, physicians interested in assessing the context in which older patients' problems occur may administer the APGAR along with psychological distress measures. As shown in one study, nearly half of elderly primary care patients with moderate or severe depression reported no depressive symptoms to their general practitioner, presumably because they felt uncomfortable discussing symptoms with their physicians.42 Collaborative care between medical and mental health service providers in primary care settings may improve older patients' access to psychological help.43 Understanding the context in which health problems occur in this population, including patient perceptions of support from family members and perceptions of their own health, can perhaps enhance these collaborative partnerships by providing physicians the unique opportunity to engage in fruitful discussions with patients about their overall health and well-being.
Footnotes
Corresponding author and reprints: Annmarie Cano, Ph.D., Department of Psychology, Wayne State University, Detroit, MI 48202 (e-mail: acano@wayne.edu).
This research was supported in part by grant R03-MH61569-01from the National Institute of Mental Health, Bethesda, Md. (Dr. Cano).
REFERENCES
- Kriegsman DMW, Penninx BWHJ, van Eijk JTM. A criterion-based literature survey of the relationship between family support and incidence and course of chronic disease in the elderly. Fam Syst Med. 1995;13:39–68. [Google Scholar]
- Doherty WJ, Baird MA. Family Therapy and Family Medicine: Toward the Primary Care of Families. New York, NY: Guilford Press. 1983 [Google Scholar]
- Glenn ML. Collaborative Health Care: A Family-Oriented Model. New York, NY: Praeger. 1987 [Google Scholar]
- Simon FB, Stierlin H, and Wynne LC. Family somatics. In: Simon FB, Stierlin H, Wynne LC, eds. The Language of Family Therapy: A Systemic Vocabulary and Sourcebook. New York, NY: Family Process Press. 1985 141–143. [Google Scholar]
- Taanila A, Larivaara P, and Korpio A. et al. Evaluation of a family-oriented continuing medical education course for general practitioners. Med Educ. 2002 36:248–257. [DOI] [PubMed] [Google Scholar]
- Weihs K, Fisher L, and Baird M. et al. Families, health, and behavior: a section of the commissioned report by the Committee on Health and Behavior: Research, Practice, and Policy Division of Neuroscience and Behavioral Health and Division of Health Promotion and Disease Prevention Institute of Medicine, National Academy of Sciences. Fam Syst Health. 2002 20:7–46. [Google Scholar]
- Minuchin S, Rosman BL, and Baker L. Psychosomatic Families: Anorexia Nervosa in Context. Cambridge, Mass: Harvard University Press. 1978 [Google Scholar]
- Beach SRH, Sandeen EE, and O'Leary KD. Depression in Marriage. New York, NY: Guilford. 1990 [Google Scholar]
- Joiner TE, Coyne JC. eds. The Interactional Nature of Depression: Advances in Interpersonal Approaches. Washington, DC: American Psychological Association. 1999 [Google Scholar]
- Cramer D. Social support and psychological distress in women and men. Br J Med Psychol. 1991;64:147–158. doi: 10.1111/j.2044-8341.1991.tb01652.x. [DOI] [PubMed] [Google Scholar]
- Duer S, Schwenk TL, Coyne JC. Medical and psychosocial correlates of self-reported depressive symptoms in family practice. J Fam Pract. 1988;27:609–614. [PubMed] [Google Scholar]
- Eker D, Arkar H. Perceived social support: psychometric properties of the MSPSS in normal and pathological groups in a developing country. Soc Psychiatry Psychiatr Epidemiol. 1995;30:121–126. doi: 10.1007/BF00802040. [DOI] [PubMed] [Google Scholar]
- Martucci M, Balestrieri M, and Bisoffi G. et al. Evaluating psychiatric morbidity in a general hospital: a two-phase epidemiological survey. Psychol Med. 1999 29:823–832. [DOI] [PubMed] [Google Scholar]
- Mengel M. The use of the Family APGAR in screening for family dysfunction in a family practice center. J Fam Pract. 1987;24:394–398. [PubMed] [Google Scholar]
- Cano A, Sprafkin RP, and Scaturo DJ. et al. Mental health screening in primary care: a comparison of 3 brief measures of psychological distress. Primary Care Companion J Clin Psychiatry. 2001 3:206–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benyamini Y, Leventhal EA, Leventhal H. Self-assessments of health: what do people know that predicts their mortality? Res Aging. 1999;21:477–500. [Google Scholar]
- Ferraro KF, Kelley-Moore JA. Self-rated health and mortality among black and white adults: examining the dynamic evaluation thesis. J Gerontol B Psychol Sci Soc Sci. 2001;56:S195–S205. doi: 10.1093/geronb/56.4.s195. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- Greiner PA, Snowdon DA, Greiner LH. Self-rated function, self-rated health, and postmortem evidence of brain infarcts: findings from the Nun Study. J Gerontol B Psychol Sci Soc Sci. 1999;54:S219–S222. doi: 10.1093/geronb/54b.4.s219. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Wallhagen MI. Self-rated health and mortality over three decades: results from a time-dependent covariate analysis. Res Aging. 1999;21:402–416. [Google Scholar]
- Jackson JL, O'Malley PG, Kroenke K. Clinical predictors of mental disorders among medical outpatients: a validation of the “S4” model. Psychosomatics. 1998;39:431–436. doi: 10.1016/S0033-3182(98)71302-7. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Jackson JL, Chamberlin J. Depressive and anxiety disorders in patients presenting with physical complaints: clinical predictors and outcome. Am J Med. 1997;103:339–347. doi: 10.1016/s0002-9343(97)00241-6. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, and Linzer M. et al. Health-related quality of life in primary care patients with mental disorders. JAMA. 1995 274:1511–1517. [PubMed] [Google Scholar]
- Mulsant BH, Ganguli M, Seaberg EC. The relationship between self-rated health and depressive symptoms in an epidemiological sample of community-dwelling older adults. J Am Geriatr Soc. 1997;45:954–958. doi: 10.1111/j.1532-5415.1997.tb02966.x. [DOI] [PubMed] [Google Scholar]
- Chao J, Zyzanski S, Flocke S. Choosing a family level indicator of family function. Fam Syst Health. 1998;16:367–373. [Google Scholar]
- Turk DC, Meichenbaum D, and Genest M. Pain and Behavioral Medicine: A Cognitive-Behavioral Perspective. New York, NY: Guilford Press. 1983 [Google Scholar]
- Hann D, Baker F, and Denniston M. et al. The influence of social support on depressive symptoms in cancer patients: age and gender differences. J Psychosom Res. 2002 52:279–283. [DOI] [PubMed] [Google Scholar]
- Oxman TE, Hull JG. Social support and treatment response in older depressed primary care patients. J Gerontol B Psychol Sci Soc Sci. 2001;56:35–45. doi: 10.1093/geronb/56.1.p35. [DOI] [PubMed] [Google Scholar]
- Smilkstein G. The Family APGAR: a proposal for a family function test and its use by physicians. J Fam Pract. 1978;6:1231–1239. [PubMed] [Google Scholar]
- Smilkstein G, Ashworth C, Montano MA. Validity and reliability of the Family APGAR as a test of family function. J Fam Pract. 1982;15:303–311. [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, and Kroenke K. et al. The utility of a new procedure for diagnosing mental disorders in primary care. JAMA. 1994 272:1749–1756. [PubMed] [Google Scholar]
- Goldberg D, Williams P. A User's Guide to the General Health Questionnaire: GHQ. Windsor, England: NFER-Nelson Publishing. 1988 [Google Scholar]
- Nguyen TD, Attkisson CC, Stegner BL. Assessment of patient satisfaction: development and refinement of a service evaluation questionnaire. Eval Program Plann. 1983;6:299–313. doi: 10.1016/0149-7189(83)90010-1. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale. A preliminary report. Psychopharmacol Bull. 1973;9:13–28. [PubMed] [Google Scholar]
- Epstein NB, Bishop DA, Levin S. The McMaster Model of Family Functioning. J Marriage Fam Couns. 1978;4:17–31. [Google Scholar]
- Bishop DS, Epstein NB, and Gilbert R. et al. Training family physicians to treat families: unexpected compliance problems. Fam Syst Med. 1984 2:380–386. [Google Scholar]
- Baird MA. Assessing family function in practice. Fam Pract Res J. 1992;12:341–342. [PubMed] [Google Scholar]
- Halvorsen JG. The Family Profile: a new self-report instrument for family assessment. Fam Pract Res J. 1992;12:343–367. [PubMed] [Google Scholar]
- Good MJD, Smilkstein G, and Good BJ. et al. The Family APGAR index: a study of construct validity. J Fam Pract. 1979 8:577–582. [Google Scholar]
- Sartorius N, Üstün TB, and Costa e Silva J-A. et al. An international study of psychological problems in primary care: preliminary report from the World Health Organization Collaborative Project on “Psychological Problems in General Health Care.”. Arch Gen Psychiatry. 1993 50:819–824. [DOI] [PubMed] [Google Scholar]
- Tessler D, Mechanic D. Psychological distress and perceived health status. J Health Soc Behav. 1978;19:254–262. [PubMed] [Google Scholar]
- O'Connor DW, Rosewarne R, Bruce A. Depression in primary care, 1: elderly patients' disclosure of depressive symptoms to their doctors. Int Psychogeriatr. 2001;13:359–365. doi: 10.1017/s1041610201007748. [DOI] [PubMed] [Google Scholar]
- Robb C, Chen H, and Haly WE. et al. Ageism in mental health and health care: a critical review. J Clin Geropsychology. 2002 8:1–12. [Google Scholar]