Abstract
Background: Screening programs for depression often fail to improve care because of lack of adequate communication and follow-up. The purpose of this study was to examine a primary care depression screening program that utilized an electronic medical record (EMR) to improve communication and follow-up.
Method: All adult patients in a family practice office were screened for depression using the Center for Epidemiological Studies Depression Scale (CES-D) during the period March 2000 through March 2001. Screening results were communicated to the primary physician via the EMR, and the physician communicated his or her plan back to the nurse via the EMR. In this retrospective cohort study, we included all persons who screened positive on the CES-D and examined their rate of new psychiatric diagnoses, new psychotropic medications, and change in CES-D scores 3 months after the initial screening.
Results: Of 1092 patients who completed the CES-D, 247 (22.6%) screened positive for depression. Among these, 35% had a new psychiatric diagnosis, 31% were prescribed new psychotropic medications, and 46% had a change in psychotropic medications. The vast majority of these were depression diagnoses and antidepressant medications. For the 94 persons who completed the CES-D at 3-month follow-up, there was a mean decrease in CES-D scores of 2.87 (p < .05).
Conclusion: This study demonstrates a positive impact of a depression screening program that utilized an EMR to facilitate communication and follow-up. Such programs could help to improve detection and treatment of depression in other primary care settings.
Depression is among the most common and debilitating psychiatric conditions, with 1 in 8 individuals requiring treatment for depression during their lifetimes.1 Although almost all cases of depression can be effectively treated with medication, psychotherapy, or a combination of the two,1 many individuals who meet diagnostic criteria for major depression go undiagnosed and untreated.2–4
One way to increase treatment rates for depression is to identify these patients in the primary care setting. While only a minority of depressed patients see a mental health specialist, the majority see their primary care physician. In fact, for persons who do receive care for depression, the majority receive this care from their primary care physician.3,4
One of the difficulties in treating depression in the primary care setting is that many depressed patients are not diagnosed as depressed by their primary care physician.1 The main reason for this is that patients usually present to their primary care physician with vague somatic complaints or with problems completely unrelated to their depression. Studies have shown that primary care physicians are excellent in diagnosing patients who present with typical symptoms of depression.5 However, when patients present with vague somatic symptoms or with unrelated problems, recognition rates are much lower.1,5
In order to increase diagnosis and treatment of depression in primary care, it is often recommended that patients be screened using a standard questionnaire.1 Screening has been shown to increase rates of both diagnosis and treatment of depression.1,6,7 However, in order for screening to work, it is necessary to provide screening results to the physician in a timely and efficient manner. One way to do this is through the use of electronic medical records (EMRs). The EMR makes it easier to record the results of a screening questionnaire, to communicate these results to the patient's primary care physician, and to track the results so that patients who screen positive can receive follow-up.
The purpose of this article is to report the findings of a primary care depression screening program that utilized an EMR. We will describe the operation of the program and discuss its impact on detection and treatment of depression and on changes in depression scores at 3-month follow-up.
METHOD
Setting
The study was conducted at the Family Medicine Center (FMC) of Christiana Care Health Services in Wilmington, Del. The FMC provides comprehensive primary care to patients of all ages and has an average of 15,000 patient visits per year. The FMC functions as the clinical teaching site for the Family Medicine residency teaching program at Christiana Care. The office has 6 faculty and 25 resident physicians, all of whom see patients on a part-time basis. The FMC has used an EMR since July of 1998 (Logician version 5.18). This EMR is a fully automated ambulatory medical record, which includes patient demographics as well as all information that would be included in a traditional medical chart (e.g., medical problems, medications, allergies, laboratory and other test results, office procedures, progress notes, and other medical documentation). The results of all laboratory tests, radiology reports, and all other diagnostic reports are communicated to the physician electronically by placing the document on the physician's computer “desktop.” The physician then reviews and signs the report and can then send an electronic note to the nurse or other staff as needed. For example, the physician could ask the nurse to contact the patient, to start a new medication, or to have the patient come in for a follow-up visit. All physicians routinely check their electronic desktops at least daily.
Depression Screening Program
In March 2000, the FMC began a program to screen all of its adult patients (aged 18 years and over) for depression. They used a questionnaire based on the Center for Epidemiological Studies Depression Scale (CES-D).9 This instrument was chosen because it has been tested and validated in diverse populations10,11 and was already being used in the FMC to screen for peripartum depression.
Patients were screened when they presented to the office to see a physician for any reason. When patients were brought back to the examination room, the nurse assistant handed them a CES-D form. They were asked to complete the form during their visit and to drop the completed form in a box at the check-out desk. They were told that their primary physician would be given the results within 2 days, and they would be contacted if treatment or follow-up was needed. These methods were chosen in order to minimize the disruption to the normal process of care, since most office visits are for problems unrelated to depression, and many times patients were seeing someone other than their regular physician. However, the patients were told that if they would like to discuss their responses on the questionnaire at the current visit, they could bring it up to the treating physician. Also, patients were told that if they had already completed a CES-D form at a previous visit, they did not need to complete another form.
At the end of each day, a transcription clerk collected the CES-D forms. The following morning, all of the forms were transcribed into the EMR. The transcribed document included the 20 questions, the patient's responses to these questions, a total score, and a notation stating that a score of 20 or greater was considered a positive screen. The completed document was sent electronically to the patient's primary physician. Physicians were instructed to review and sign the document and to treat and/or follow-up with the patient as they deemed appropriate. These methods were similar to those used by the FMC for other diagnostic reports, as described above.
While the depression screening program did not direct physicians toward any specific intervention for depressed patients, it did include follow-up of patients who screened positive. All patients who scored 15 or higher on the CES-D were mailed a follow-up questionnaire 3 months after their initial screen. They were instructed to complete the follow-up form and return it to the FMC. Again, patients were told that the result would be communicated to their primary physician within 2 days of receipt, that they would be contacted as needed for treatment or follow-up, and that they could contact their physician if they wanted to discuss their responses on the questionnaire.
The depression screening program at the FMC continued for 1 year, through March of 2001. During that year, there was a change in the methodology for the initial screen. Starting in January of 2001, screening was no longer done when the patient came to the FMC for a physician visit. Rather, a list of adult patients who had come to the FMC was reviewed on a weekly basis, and these patients were mailed a CES-D form if they did not already have a completed CES-D form in their chart. The reason for this change was in response to requests from both patients and nursing staff, in order to minimize the number of CES-D forms that were given to people who had already completed one at a previous visit. In the mailed version, patients were provided written instructions that were identical to the instructions given when the CES-D had been administered in the FMC.
Study Population
Using the EMR database, we determined the number of patients who submitted a completed CES-D form, and we selected all patients who scored positive (i.e., 20 points or greater) on their initial CES-D. From this total study population, we also selected 3 subgroups for the study: subgroup A had no psychiatric diagnoses prior to screening (N = 129), subgroup B had neither a psychiatric diagnosis nor any psychotropic medications prior to screening (N = 101), and subgroup C had both a previous diagnosis and previous medications (N = 94). This information on prior diagnoses and medications was gathered from the EMR database. Note that group B is a subset of group A and that persons in group A may have been on psychotropic medications even though no psychiatric diagnosis was listed.
Data Analysis
The main intent of the study was to determine the impact of screening on diagnosis of psychiatric conditions, on initiation or changes in psychotropic medications, and on CES-D scores. Both descriptive and inferential analyses were performed. For subgroup A we determined the proportion that had a new psychiatric diagnosis within 3 months of screening. For subgroup B we determined the proportion that had new psychiatric medications prescribed within 3 months of screening. For subgroup C we determined the proportion for which changes were made in their psychiatric medications within 3 months of screening. Finally, for those who returned a follow-up CES-D 3 months after the initial screen, we determined changes in CES-D scores.
For the group who returned follow-up CES-D forms, we determined whether depression scores improved from baseline to follow-up. We used a paired-samples t test since the dependent variable demonstrated a normal distribution. However, we also conducted a more conservative nonparametric test (the Wilcoxon test for 2 related samples). For both tests, p < .05 was considered statistically significant.
RESULTS
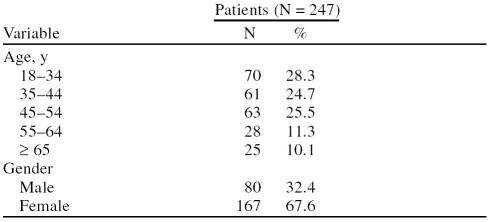
Overall, 1092 patients returned completed CES-D forms during the study period. Of these, 247 (22.6%) screened positive (CES-D score of 20 or greater) and comprised our study population. The age and gender distribution of this population is shown in Table 1.
Table 1.
Age and Gender Distribution of Patients Who Screened Positive for Depression
For subgroup A, 45 persons (35%) had a new psychiatric diagnosis within 3 months of screening. Thirty-nine of these persons had a new diagnosis of depression, 4 had a new diagnosis of an anxiety disorder, and 2 persons were diagnosed with disorders from both categories. For subgroup B, 31 persons (31%) had new psychotropic medications prescribed within 3 months of screening. Twenty-six of these persons had antidepressants prescribed, 2 had anxiolytics prescribed, and 3 persons had both types of psychotropic medications prescribed. For subgroup C, 43 persons (46%) had a change in psychotropic prescriptions. The change involved antidepressant medications for 34 persons, anxiolytics for 3 persons, both antidepressants and anxiolytics for 5 persons, and antipsychotic medication for 1 person.
Of the 247 study patients, 94 returned their 3-month follow-up CES-D. This represents a response rate of 38%. Of these 94 persons, 52.1% had a decrease in CES-D scores, while 38.3% had an increase in scores and 9.6% had no change. On average, the follow-up CES-D scores decreased 2.87 points from the initial screening scores (p < .05 by t test, p = .057 by Wilcoxon test).
DISCUSSION
This study shows a positive impact of a primary care office–based depression screening program that utilized an electronic medical record. Overall, 23% of adult patients screened positive on the CES-D instrument, which is consistent with previous studies of screening in primary care populations.11,12 Over half of these persons had no previous psychiatric diagnosis. For those with no previous diagnosis, over one third were diagnosed with depression or some other psychiatric disorder by their physician. About the same number were prescribed new psychotropic medications, almost all of which were antidepressants.
Perhaps even more important was the change in depression scores. The value of diagnosis and treatment of depression is determined by whether they lead to improvements in patient outcomes. Of the 94 patients who returned their 3-month follow-up CES-D, the majority (52.1%) had a decrease in CES-D scores, and the average CES-D score showed a statistically significant decrease.
The positive results of this study are encouraging given the importance of diagnosing and treating depression in the primary care setting. While depression is a common and debilitating but treatable condition, many depressed persons go undiagnosed or untreated.13 Diagnosis and treatment in the primary setting are recommended, since the majority of depressed patients visit their primary care physician over the course of a year and since treatment for depression can be as effective in primary care settings as it is in specialty settings.1,14 Unfortunately, depression often goes unrecognized in primary care settings.1 This is understandable, since primary care physicians manage multiple complex problems and depressed patients often see their primary care physician for a reason other than depression. Given these barriers to diagnosis in the primary care setting, it makes sense that screening for depression could improve rates of diagnosis and treatment.
While the benefits of screening for depression make intuitive sense, previous studies have shown mixed results. Although some studies have shown improvements in diagnosis and treatment of depression as a result of screening and physician feedback, other studies have shown no significant improvement.4,7 One particular study found that screening improved diagnosis and treatment only when feedback to physicians was selective, i.e., when physicians were notified only when the patient screened positive.7 No previous studies have shown screening to improve depression scores or other clinical outcomes.4,7
In fact, recent guidelines by the U.S. Preventive Services Task Force (USPSTF) recommend screening for depression in primary care.15 However, they qualify this by saying that screening should be done only in settings for which there are systems in place for adequate follow-up and treatment. The present study suggests one possible way to make that happen. In this study, we took advantage of an established EMR. The EMR allowed more rapid and standardized feedback to physicians. It also allowed the physicians an easy way to initiate treatment or follow-up. They did this by sending a note to the nurse or staff to start medications (in cases in which the physician was able to make an appropriate diagnosis based on prior information) or to ask the patient to come in for follow-up. Finally, the EMR allowed easy tracking of patients who had screened positive. This suggests that using electronic charting and communication may be one way to achieve the follow-up recommended by the USPSTF and thereby make depression diagnosis and treatment more successful. Previous studies have also suggested that using the EMR can help to improve detection and treatment of depression in primary care.12
There are several limitations that one must consider when interpreting the results of this study. First, the results cannot be used as valid estimates of the rates of detection and treatment of depression in primary care. That is because our study population was defined by those who scored positive on a screening instrument, rather than by those who are truly depressed by standard diagnostic criteria. Since the screening instrument is not 100% sensitive and specific, it is likely that some persons with depression were missed by the CES-D and that some persons who screened positive are not truly depressed. In fact, studies have suggested that the false-positive rates could be up to 90% depending on what cutoff is chosen to designate a positive screen.16
Also, one must consider that since we did not have a comparison group, we cannot be certain that the persons who were newly diagnosed or treated for depression would not have been thus diagnosed or treated without the screening program. We also cannot be certain that those who improved over 3 months would not have improved without the screening program. It could also be that persons who did return the follow-up survey did so because they had improved (in which case they may feel that follow-up is unnecessary) or because they had worsened (and were less motivated to be treated because of worsening depression). Finally, this study was done in a single family medicine residency teaching practice in Delaware. Results may differ in other settings or for other populations.
Despite these limitations, the results of this study have potential to help improve quality of care for depression. While guidelines encourage primary care physicians to diagnose and treat their depressed patients,1 rates of detection and treatment in primary care settings are still suboptimal. One reason is that screening has not been found to be uniformly effective,7 and physicians are reluctant to initiate screening programs because these programs can be cumbersome and time-consuming.17 This study suggests that using an EMR may make screening and feedback more feasible and therefore may have the potential to improve quality of care for depression.
Acknowledgments
The authors would like to thank Ms. Stephanie Billinski for her assistance with data collection and Mrs. Margaret Lardear for data entry. The authors would also like to thank Wenya Grace Yang, M.S., for assistance with data analysis and Ms. Cheryl Mongillo for assistance with manuscript preparation.
Pretest and Objectives
Instructions and Posttest
Registration and Evaluation
Footnotes
In the spirit of full disclosure and in compliance with all ACCME Essential Areas and Policies, the authors report no financial affiliation or other relationship relevant to the subject matter presented in this article.
REFERENCES
- Depression Guideline Panel. Depression in Primary Care, vol 2: Treatment of Major Depression. Clinical Practice Guideline, no. 5. Rockville, Md: US Dept Health Human Services, Public Health Service, Agency for Health Care Policy and Research. 1993 175. [Google Scholar]
- Unützer J, Katon W, and Callahan CM. et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002 288:2836–2845. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, and Sullivan M. et al. Treating depressed older adults in primary care: narrowing the gap between efficacy and effectiveness. Milbank Q. 1999 77:225–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinkman MS, Okkes I. Mental health problems in primary care: a research agenda. J Fam Pract. 1998;47:379–384. [PubMed] [Google Scholar]
- Carney PA, Dietrich AJ, and Eliassen MS. et al. Recognizing and managing depression in primary care: a standardized patient study. J Fam Pract. 1999 48:965–972. [PubMed] [Google Scholar]
- Valenstein M, Vijan S, and Zeber JE. et al. The cost-utility of screening for depression in primary care. Ann Intern Med. 2001 134:345–360. [DOI] [PubMed] [Google Scholar]
- Gilbody SM, House AO, Sheldon TA. Routinely administered questionnaires for depression and anxiety: systematic review. BMJ. 2001;322:406–409. doi: 10.1136/bmj.322.7283.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logician 4.6. Hillsboro, Ore: MedicaLogic/Medscape, Inc. 1994. [Google Scholar]
- Radloff L. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: evaluation of the Center for Epidemiological Studies Depression Scale. J Psychosom Res. 1999;46:437–443. doi: 10.1016/s0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- Papassotiropoulos A, Heun R. Screening for depression in the elderly: a study on misclassification by screening instruments and improvement of scale performance. Prog Neuropsychopharmacol Biol Psychiatry. 1999;23:431–446. doi: 10.1016/s0278-5846(99)00007-x. [DOI] [PubMed] [Google Scholar]
- Rollman BL, Hanusa BH, and Gilbert T. et al. The electronic medical record: a randomized trial of its impact on primary care physicians' initial management of major depression. Arch Intern Med. 2001 161:189–197. [DOI] [PubMed] [Google Scholar]
- Regier DA, Myers JK, and Kramer M. et al. The NIMH Epidemiologic Catchment Area program: historical context, major objectives, and study population characteristics. Arch Gen Psychiatry. 1984 41:934–941. [DOI] [PubMed] [Google Scholar]
- Schulberg HC, Katon W, and Simon GE. et al. Treating major depression in primary care practice: an update of the Agency for Health Care Policy and Research Practice Guidelines. Arch Gen Psychiatry. 1998 55:1121–1127. [DOI] [PubMed] [Google Scholar]
- Berg AO. US Preventive Services Task Force. Screening for depression: recommendations and rationale. Am Fam Physician. 2002;66:647–650. [PubMed] [Google Scholar]
- Williams JW, Kerber CA, and Mulrow CD. et al. Depressive disorders in primary care: prevalence, functional disability, and identification. J Gen Intern Med. 1995 10:7–12. [DOI] [PubMed] [Google Scholar]
- Solberg LI, Korsen N, and Oxman TE. et al. The need for a system in the care of depression. J Fam Pract. 1999 48:973–979. [PubMed] [Google Scholar]