Abstract
Traumatic Brain Injury (TBI) continues to be one of the leading causes of death and disability in the pediatric population. Although the literature on neurocognitive outcomes is relatively rich, studies vary significantly in the methods used to group subjects on several moderating variables, including age at injury, injury severity, and time since injury, making it difficult to combine and summarize the data for comparison. Further complicating this effort is the wide range of measures used to document functional outcomes in key neurocognitive domains. In this meta-analytic review, 28 publications (1988 to 2007) that met inclusion criteria were summarized based on three distinct injury severity and time post injury groups for 14 key neurocognitive domains. Effect sizes were calculated to reflect the extent to which the above groups differed in case-control and case-case studies, as well as address recovery based on longitudinal studies. To the best of our knowledge, this is the first published quantitative summary of the literature on neurocognitive outcomes after pediatric TBI. Limitations of the current state of the literature as well as recommendations for future studies are discussed.
Keywords: traumatic brain injury, pediatric, meta analysis, neurocognitive outcomes
Traumatic Brain Injury (TBI) is the single most common cause of death and disability in children and adolescents (CDC, 2000). A major cause of the significant disability frequently associated with pediatric TBI is acquired neurocognitive impairments that adversely affect academic, behavioral, and interpersonal functioning. Numerous studies have examined the neurocognitive sequelae after a brain injury in childhood. There are often striking inconsistencies among studies about the nature and extent of neurocognitive impairment and recovery following TBI. These inconsistencies in part result from several intrinsic characteristics of TBI, including the heterogeneity of injuries (e.g., location of lesion, mechanism of injury) and the influence of social and developmental processes (e.g., age at injury, premorbid status, and family resources) on the injured brain’s capacity to recover neurocognitive functioning. The variability in reported neurocognitive outcomes among studies also reflects methodological differences among studies (e.g., sample characteristics such as injury severity, age at injury and time since injury, as well within subject over time vs. cross-sectional study designs). For example, some studies of mild TBI have reported significant functional impairments (Boll, 1983) whereas others have reported minimal functional morbidity once premorbid status has been accounted for (Asarnow et al., 1995). Further complicating attempts at integrating the extant data are the wide range of measures used to assess key domains of neurocognitive outcome. Such methodological differences among studies and the heterogeneity of injuries need to be systematically taken into account when summarizing the available data on neurocognitive outcomes after pediatric TBI.
We conducted a meta-analytic review of studies that examined the effects of injury severity and time since injury on neurocognitive outcomes and recovery after pediatric TBI using crosssectional and longitudinal reports. By definition, a meta-analysis uses effect size as the metric to delineate the magnitude of the difference between groups. In this report, the analyses were designed to answer the following three separate, but related, questions regarding outcomes and recovery of key neurocognitive domains after a pediatric TBI:
What is the magnitude of the effect of injury severity over the course of three time bands following injury? (Case-control studies)
What is the magnitude of the difference among severity groups over the course of three time bands following injury? (Case-case studies)
What is the magnitude of change over time (i.e., recovery) in key neurocognitive domains across severity groups? (Longitudinal studies)
There have been a number of excellent reviews on neurocognitive outcomes after pediatric TBI. They have, however, focused on a subsample of this population (e.g., mild injuries [Satz et al., 1997]) or on a specific cognitive domain (e.g., executive function [Levin & Hanten, 2005]). Further, to the best of our knowledge, there has not been a systematic meta-analytic review of neurocognitive outcomes across domains, accounting for time post injury, injury severity, and age at injury. In this review, we attempted to provide a systematic, quantitative summary of the literature.
Method
We attempted to identify all studies that reported neurocognitive outcomes subsequent to pediatric TBI. Studies were included that either directly reported neurocognitive outcomes as a primary objective or reported data on neurocognitive outcomes for a related objective (e.g., imaging study). Studies published in English reporting neurocognitive outcomes after a TBI were identified using the PubMed database. Search terms included combinations of neuropsychology/cognition/neurocognition, head injury/TBI, child/pediatric. Studies of inflicted injuries on infants and children were not included, because nonaccidental head trauma patients are unique in their presentation and their prognoses, tend to be younger (Gilles, 1999), and the neuropathology and neurophysiology of nonaccidental trauma is different from accidental brain injury (Geddes, Hackshaw, Vowles, Nickols, & Whitwell, 2001). The search yielded 115 publications. To calculate effect sizes, only studies that reported descriptive group statistics or group difference statistics were included, thereby excluding 25 studies, many of them pivotal. These studies described growth curve analyses or statistical associations between neurocognitive variables and other factors (e.g., imaging correlates). Of the remaining studies, an additional 25 were excluded because injury severity was unclear (N = 7) or severity groups were combined (N = 18), leaving 65 studies. There were only a few studies using other injury controls instead of healthy controls and because these comparisons were different in nature and few in number, they were not included in the analyses. An effort was also made to identify and exclude studies using duplicate subject pools (e.g., same lab and same recruitment period), except when the reported outcomes were different, thereby excluding an additional eight studies. Despite our best efforts, there may be some subject overlap, which we were unable to identify from the study descriptions provided. An additional 29 were excluded because they did not include data on the discrete neurocognitive domains we were interested in for this meta analysis. The resulting final database included a total of 28 publications, dating from 1988 to 2007.
To answer the questions posed by this review, one would ideally include only longitudinal studies with clearly defined injury severity, age at injury, and narrow time since injury bands. Unfortunately, many studies were not organized in this manner. Consequently, we attempted to verify the results from the relatively few longitudinal studies of children with TBI by examining the same neurocognitive domains at similar times post injury in crosssectional reports. To group the studies, we set cut points for each of the following key moderating variables: (1) injury severity, (2) time since injury, and (3) age at injury.
In a majority of the studies, acute injury severity was based on Glasgow Coma Scale (GCS) score and frequently confirmed by clinical findings (e.g., presence/length of loss of consciousness and posttraumatic amnesia, and/or positive neuroimaging findings). Consistent with convention, most studies used the following GCS score ranges to group samples based on injury severity: mild (GCS 13–15), moderate (GCS 9–12), and severe (GCS 3–8). We used the severity groups published in the studies to designate the injury severity groups used in our analyses.
Three mean time post injury intervals were defined using the following cutoffs: Time 1: 0–5 months post injury; Time 2: 6–23 months post injury, and Time 3: 24+ months post injury. In general, Time 1 represents the postacute period, where the greatest functional impairments are observed. Time 2 represents the period when the greatest recovery is observed. Time 3 is the chronic stage, when most of the recovery has already taken place and relatively little change is expected thereafter. We used the mean time post injury for a study when assigning it to one of the three time post injury categories. We are fully aware that there were several studies that included patients with time post injury spanning across these three time bands. We attempted to minimize the overlap as much as possible by carefully selecting our cutoffs.
Finally, the following two age at injury groupings were created based on the group means reported in studies: Injury age 1: 0–5 years and Injury age 2: 6–16 years. This cutpoint was chosen for several related reasons: (1) in general, different types of neurocognitive measures are used for these two age groupings, (2) by 6 years, most children have begun formal education, significantly affecting their development, and (3) by about 6 years, children begin to show a greater functional utilization of language and metacognitive skills, which separates them from their younger counterparts. There were several studies that included patients with age at injury ranges spanning across our two age at injury groupings. Again, we chose our cutoff to minimize this overlap as much as possible.
The statistics extracted from publications included the minimal descriptive data necessary to calculate effect sizes. These included: (1) mean and standard deviation (when standard deviation was not reported, it was calculated using confidence intervals or standard errors of the means), (2) sample size and t-value, (3) difference in means and common standard deviation, or (4) sample size and p value. Rosenthal and DiMatteo (2001) review the mathematical calculations used to derive effect sizes from the above descriptive data (Rosenthal & DiMatteo, 2001). The extracted descriptive and group difference statistics were entered into a database in the software program Comprehensive Meta Analysis (Borenstein, Hedges, Higgins, & Rothstein, 2005). Hedge’s g was used as the estimate of effect because it is adjusted for sample size (McCartney & Rosenthal, 2000). Random instead of fixed effects models were chosen because effect sizes were expected to vary across studies depending on the sample characteristics and the neurocognitive measures used, and the weights assigned to each study were balanced based on study sample size (Borenstein, Hedges, & Rothstein, 2007). A general interpretive guide to effect sizes includes: large effects (.8), moderate effects (.5), and small effects (.2) (Cohen, 1988). We calculated effect sizes for subgroups based on injury severity and time since injury. Although separate statistics were not calculated for the age at injury variable (because relatively few studies were identified that fit the lower age at injury band), studies were tracked on this variable to make it possible to identify effect sizes that were driven by study samples including younger groups for post hoc discussion.
There were very few longitudinal studies, which would ideally be used to describe recovery of functions over time. For this reason, when possible, scores from the same measure but using a different cohort of patients were matched to form comparable “within-subject” data. These analyses were used to compliment the true within subject analyses and not replace them. Statistics using this combination approach are reported separately and clearly identified in the tables. (These statistics are always presented on the right side of “/” in the tables). Further, for the “within-subject” longitudinal studies, we only included studies reporting standard scores in the analyses and excluded all reported data using raw scores. We decided to do so because we could not account for normal developmental changes that may, in part or in full, explain changes in raw scores. Further, we are aware that in cases where more than one measure of a function (e.g., attention) were reported, we did not observe the independent observations prerequisite for inclusion in the effect size calculations. We decided to include multiple measures of the same neurocognitive domain within the same study because we believe that each measure contributes uniquely to the study of a given neurocognitive domain (e.g., sustained vs. divided attention) and that eliminating measures may bias the results. We also had no basis of eliminating one subskill wihin a given domain in favor of another.
The following neurocognitive domains were included in the analyses: General Intellectual Functioning (FSIQ or its equivalent; Verbal IQ; and Performance IQ); Attention/Executive Functions (working memory, processing speed/reaction time, attention, fluency, inhibition, and problem solving); Memory (verbal/visual immediate/delayed); and Visual Perceptual/Motor skills. Although there were several pivotal studies of language functions, academic skills, and motor skills, we focused on more traditional neurocognitive domains to simplify our analyses. Global measures of functioning were also excluded (e.g., combined visual and verbal memory composites) because they provided redundant information and potentially erroneously combined skill areas that are uniquely affected after injury.
Results
Twenty-three of the 28 studies included in the meta-analysis used exclusion criteria that were similar across studies and included, in large part, prior neurological (including previous head injury), developmental, learning/attention, and psychiatric diagnoses, penetrating injuries, injuries secondary to abuse, and in some cases, nonfluent English speaking patients and/or parents. Three of the studies did not indicate whether exclusion criteria were used. The remaining two explicitly stated that all patients who met inclusion criteria were recruited. Interestingly, one of the latter two studies of severe TBI outcomes showed the largest case-control effects across many neurocognitive domains (Parry et al., 2004).
In Table 1, effect sizes, an estimate of the associated standard error (SE), the statistical significance of the associated statistic (p), and the number of individual studies or individual reports from a given study (N) are reported. The specific studies from which descriptive statistics are extracted from are also identified as references. Of note, in a few domains, there are more observations than studies because more than one measure of a given neurocognitive domain was included. The three sets of analyses for each neurocognitive domain correspond to the three questions posed in this meta-analysis, addressing magnitude of (a) the effect of injury severity over the course of three time bands post injury, (b) the difference among severity groups over the course of three time bands post injury, and (c) change over time (recovery) in key neurocognitive domains across severity groups. The first two sets of questions are addressed by the cross-sectional case-control and cross-sectional case-case reports, respectively. Corresponding to these analyses, the first two sets of effect sizes presented in Table 1 (sections 1a-14a and 1b-14b) reflect the magnitude of effects listed separately by injury severity and by time post injury. The third question is addressed using longitudinal within group data reflecting the magnitude of change over time, also listed separately by injury severity and time post injury. The effect sizes derived from the three sets of analyses provide complimentary findings and a unique perspective on neurocognitive outcomes and recovery after pediatric TBI that none of the analyses can do independently.
Table 1. Effect Sizes and Associated Statistics for Each Neurocognitive Domain by Severity and Time Post Injury Group.
| FSIQ | Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1a | Mild vs. Ctrl | −.209 | .19(1) | (1) | −.171 | .20(1) | (2) | −.298 | .16(3) | (3–5) | |||
| Mod vs. Ctrl | −.917 | .29(1) | * | (1) | −.487 | .28(1) | (2) | −.599 | .20(3) | * | (3–5) | ||
| Sev vs. Ctrl | −.786 | .32(1) | * | (1) | −1.086 | .20(4) | * | (2,6,7) | −1.106 | .23(5) | * | (3–5,8,9) | |
| 1b | Mild vs. Mod | −.656 | .14(4) | * | (1,10,11) | −.564 | .14(4) | * | (2,10,11) | −.430 | .13(6) | * | (2–5,10,11) |
| Mod vs. Sev | −.792 | .16(4) | * | (1,10,11) | −.479 | .16(4) | * | (2,10,11) | −.469 | .14(6) | * | (2–5,10,11) | |
| Mild vs. Sev | −1.348 | .17(4) | * | (1,10,11) | −.998 | .17(4) | * | (2,10,11) | −.778 | .17(6) | * | (3–5,10,11) |
| Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1c | Mild | −.129 | .13(4) | (1,2,10,11) | −.019 | .14(4) | (2,3,10,11) | −.148 | .14(4) | (1,3,10,11) | |||
| Mod | −.213 | .13(4) | (1,2,10,11) | −.004 | .14(4) | (2,3,10,11) | −.204 | .40(4) | (1,3,10,11) | ||||
| Sev | −.438 | .14(5) | (1,2,10–12) | −.084/−.145 | .14/.11(5/8) | (2,3,10–12)/(2–7, 10–13) |
−.507 | .14(5) | * | (1,3,10–12) |
| VIQ | Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2a | Mild vs. Ctrl | −.143 | .19(1) | (1) | −.053 | .20(1) | (2) | −.358 | .16(3) | (3–5) | |||
| Mod vs. Ctrl | −.665 | .29(1) | * | (1) | −.416 | .28(1) | (2) | −.464 | .20(3) | * | (3–5) | ||
| Sev vs. Ctrl | −.523 | .32(1) | (1) | −.393 | .31(1) | (2) | −.903 | .36(5) | * | (3–5,8,9) | |||
| 2b | Mild vs. Mod | −.421 | .16(4) | * | (1,10,14) | −.547 | .16(3) | * | (2,10) | −.292 | .17(5) | (3–5,10) | |
| Mod vs. Sev | −.556 | .17(4) | * | (1,10,14) | −.418 | .19(3) | * | (2,10) | −.428 | .15(5) | * | (3–5,10) | |
| Mild vs. Sev | −.915 | .17(4) | * | (1,10,14) | −.923 | .19(3) | * | (2,10) | −.606 | .19(5) | * | (3–5,10) |
| Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2c | Mild | −.016 | .15(3) | (1,2,10) | .102 | .16(3) | (2,3,10) | .070/.127 | .15/.14(3/4) | (1,3,10)/(4,14) | |||
| Mod | −.025 | .16(3) | (1,2,10) | .084 | .16(3) | (2,3,10) | .066/.157 | .16/.17(3/4) | (1,3,10)/(1,3,4,10,14) | ||||
| Sev | −.350 | .15(4) | * | (1,2,10,12) | −.105 | .15(4) | (2,3,10,12) | −.376/−.253 | .20/.20(4.5) | (1,3,9,10,12,14) |
| PIQ | Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3a | Mild vs. Ctrl | −.216 | .19(1) | (1) | −.237 | .20(1) | (2) | −.106 | .16(3) | (3–5) | |||
| Mod vs. Ctrl | −.830 | .29(1) | * | (1) | −.464 | .28(1) | (2) | −.579 | .20(3) | * | (3–5) | ||
| Sev vs. Ctrl | −.892 | .33(1) | * | (1) | −.787 | .32(1) | * | (2) | −.846 | .20(5) | * | (3–5,8,9) | |
| 3b | Mild vs. Mod | −.635 | .15(4) | * | (1,10,14) | −.396 | .16(3) | * | (2,10) | −.450 | .14(5) | * | (3–5,10) |
| Mod vs. Sev | −.791 | .18(4) | * | (1,10,14) | −.586 | .20(3) | * | (2,10) | −.561 | .16(5) | * | (3–5,10) | |
| Mild vs. Sev | −1.394 | .18(4) | * | (1,10,14) | −.962 | .19(3) | * | (2,10) | −.867 | .19(5) | * | (3–5,10) |
| Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3c | Mild | −.249 | .15(3) | (1,2,10) | −.189 | .16(3) | (2,3,10) | −.414/.175 | .19/.55(3/4) | */ | (1,3,10)/(5,14) | ||
| Mod | −.434 | .16(3) | * | (1,2,10) | −.024 | .16(3) | (2,3,10) | −.458/−.385 | .16/.16(3/4) | */* | (1,3,4,10,14) | ||
| Sev | −.664 | .15(4) | * | (1,2,10,12) | −.055 | .15(4) | (2,3,10,12) | −.692/−.643 | .15/.14(4/5) | */* | (1,3,9,10,12,14) |
| Processing speed |
Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4a | Mild vs. Ctrl | −.331 | .19(1) | (1) | −.508 | .21(1) | * | (2) | −.336 | .19(3) | * | (3-5) | |
| Mod vs. Ctrl | −.629 | .29(1) | * | (1) | −.221 | .28(1) | (2) | −.731 | .21(3) | * | (3–5) | ||
| Sev vs. Ctrl | −1.181 | .34(1) | * | (1) | −.645 | .32(1) | * | (2) | −.925 | .23(4) | * | (3–5,8) | |
| 4b | Mild vs. Mod | −.545 | .13(5) | * | (1,2,10,11,14) | −.255 | .20(4) | (2,10,11) | −.385 | .13(6) | * | (3–5,10,11) | |
| Mod vs. Sev | −.692 | .15(5) | * | (1,2,10,11,14) | −.659 | .16(4) | * | (2,10,11) | −.503 | .14(6) | * | (3–5,10,11) | |
| Mild vs. Sev | −1.188 | .15(5) | * | (1,10,11,14) | −.877 | .19(4) | * | (2,10,11) | −.607 | .15(8) | * | (3–5,10,11,15) |
| Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4c | Mild | −.187 | .13(4) | (1,2,10,11) | −.114 | .19(4) | (2,3,10,11) | −.354 | .15(4) | * | (1,3,10,11) | ||
| Mod | −.475 | .15(4) | * | (1,2,10,11) | .119 | .14(4) | (2,3,10,11) | −.331 | .14(4) | * | (1,3,10,11) | ||
| Sev | −.554 | .18(4) | * | (1,2,10,11) | −.048 | .18(4) | (2,3,10,11) | −.570 | .18(4) | * | (1,3,10,11) |
| Attention | Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | 17,27 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5a | Mild vs. Ctrl | .011 | .19(1) | (1) | −.165 | .20(1) | (2) | −.347 | .20(5) | (3,4) | |||
| Mod vs. Ctrl | −.373 | .28(1) | (1) | −.374 | .28(1) | (2) | −.316 | .14(5) | * | (3,4) | |||
| Sev vs. Ctrl | −.662 | .32(1) | * | (1) | −.507 | .32(1) | (2) | −.710 | .14(6) | * | (3,4,9) | ||
| 5b | Mild vs. Mod | −.334 | .13(4) | * | (1,11) | −.201 | .16(6) | (2,11,16) | −.246 | .11(8) | * | (3,4,11) | |
| Mod vs. Sev | −.509 | .15(4) | * | (1,11) | −.652 | .19(6) | * | (2,11,16) | −.390 | .11(8) | * | (3,4,11) | |
| Mild vs. Sev | −.878 | .16(4) | * | (1,11) | −.800 | .15(6) | * | (2,11,16) | −.570 | .11(9) | * | (3,4,11,15) |
| Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5c | Mild | −.016 | .20(1) | (1,2) | −.171 | .21(1) | (2,3) | −.168 | .21(1) | (1,3) | |||
| Mod | −.344 | .28(1) | * | (1,2) | .410 | .31(1) | (2,3) | −.052 | .31(1) | (1,3) | |||
| Sev | −.254 | .31(1) | (1,2) | −.213 | .34(1) | (2,3) | −.484 | .34(1) | (1,3) |
| Working memory |
Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6a | Mild vs. Ctrl | −.019 | .16(2) | (1,17) | −.050 | .17(2) | (2,17) | −.092 | .10(7) | (3–5,17–19) | |||
| Mod vs. Ctrl | −.050 | .18(2) | (1,17) | −.183 | .18(2) | (2,17) | −.194 | .21(4) | (3–5,17) | ||||
| Sev vs. Ctrl | −.305 | .20(2) | (1,17) | −.254 | .20(2) | (2,17) | −.453 | .15(8) | * | (3–5,17,19,20) | |||
| 6b | Mild vs. Mod | −.309 | .17(5) | (1,10,11,17) | −.319 | .12(6) | * | (2,10,11,16,17) | −.181 | .09(9) | * | (3–5,10,11,17,21) | |
| Mod vs. Sev | −.230 | .13(5) | (1,10,11,17) | −.043 | .13(6) | (2,10,11,16,17) | −.124 | .09(9) | (3–5,10,11,17,21) | ||||
| Mild vs. Sev | −.549 | .19(5) | * | (1,10,11,17) | −.391 | .14(6) | * | (2,10,11,16,17) | −.388 | .08(13) | * | (3–5,10,11,17,19–21) |
| Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6c | Mild | .049 | .13(4) | (2,3,10,11) | −.016/.088 | .14/.13(4/5) | (2,3,10,11)/ (2,3,5,10,11,16) |
.035 | .14(4) | (1,3,10,11) | |||
| Mod | −.018 | .13(4) | (1,2,10,11) | −.075/−.125 | .14/.13(4/5) | (2,3,10,11)/ (2,3,5,10,11,16) |
−.087 | .14(4) | (1,3,10,11) | ||||
| Sev | −.228 | .18(4) | (1,2,10,11) | −.146/−.166 | .18/.16(4/5) | (2,3,10,11)/ (2,3,5,10,11,16) |
−.360 | .18(4) | * | (1,3,10,11) |
| Fluency | Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 7a | Mild vs. Ctrl | −.139 | .31(1) | (17) | −.419 | .32(1) | (17) | −.572 | .32(1) | (17) | |||
| Mod vs. Ctrl | −.152 | .23(1) | (17) | −.099 | .23(1) | (17,22) | −.403 | .14(3) | * | (17,23) | |||
| Sev vs. Ctrl | −.288 | .27(1) | (17) | −.410 | .27(1) | (17) | −1.115 | .29(3) | * | (17,23) | |||
| 7b | Mild vs. Mod | −.340 | .37(2) | (14,17) | .272 | .30(1) | (17) | .316 | .35(1) | (17) | |||
| Mod vs. Sev | −.172 | .22(2) | (14,17) | −.279 | .25(1) | (17) | −.395 | .14(3) | * | (17,23) | |||
| Mild vs. Sev | −.592 | .44(2) | (14,17) | −.014 | .33(1) | (17) | −.348 | .24(2) | (15,17) |
| Inhibition | Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 8a | Mod vs. Ctrl | −.725 | .25(1) | * | (23) | ||||||||
| Sev vs. Ctrl | −.389 | .20(2) | * | (9,23) | |||||||||
| 8b | Mod vs. Sev | .096 | .24(1) | (23) |
| Problem solving |
Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 9a | Mild vs. Ctrl | −.150 | .19(1) | (1) | −.165 | .20(1) | (2) | .180 | .22(1) | (3) | |||
| Mod vs. Ctrl | −.325 | .28(1) | (1) | −.342 | .28(1) | (2) | −.402 | .13(4) | * | (3,23) | |||
| Sev vs. Ctrl | −.052 | .31(1) | (1) | −.024 | .13(5) | (2,6) | −.701 | .14(6) | * | (3,8,9,23) | |||
| 9b | Mild vs. Mod | −.183 | .24(1) | (1) | −.397 | .24(1) | (2) | −.740 | .29(1) | * | (3) | ||
| Mod vs. Sev | −.284 | .30(1) | (1) | −.347 | .30(1) | (2) | −.180 | .13(4) | (3,23) | ||||
| Mild vs. Sev | −.503 | .26(1) | * | (1) | −.729 | .27(1) | * | (2) | −.305 | .16(3) | * | (3,15) |
| Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 9c | Mild | −.440 | .20(1) | * | (1,2) | −.343 | .21(1) | (2,3) | −.775 | .22(1) | * | (1,3) | |
| Mod | −.211 | .28(1) | (1,2) | .064 | .31(1) | (2,3) | −.134 | .31(1) | (1,3) | ||||
| Sev | −.139 | .31(1) | (1,2) | −.259 | .34(1) | (2,3) | −.385 | .34(1) | (1,3) |
| Verbal immediate |
Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10a | Mild vs. Ctrl | −.327 | .17(2) | * | (1,17) | −.313 | .17(2) | (2,17) | −.061 | .15(3) | (3,17) | ||
| Mod vs. Ctrl | −.098 | .18(2) | (1,17) | −.624 | .41(3) | (2,17,22) | −.224 | .19(2) | (3,17) | ||||
| Sev vs. Ctrl | −.521 | .18(3) | * | (1,17,24) | −.809 | .14(6) | * | (1,2,6,7,17) | −.552 | .23(7) | * | (17,18,20) | |
| 10b | Mild vs. Mod | −.130 | .33(3) | (1,14,17) | .118 | .19(2) | (2,17) | −.122 | .30(2) | (5,17) | |||
| Mod vs. Sev | −.338 | .18(3) | * | (1,14,17) | −.332 | .19(2) | (2,17) | −.434 | .18(3) | * | (3,5,17) | ||
| Mild vs. Sev | −.613 | .45(3) | (1,14,17) | −.215 | .21(2) | (2,17) | −.545 | .15(5) | * | (3,5,17,20,25) |
| Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10c | Mild | /.151 | /.21(/1) | /(14,25) | |||||||||
| Mod | |||||||||||||
| Sev | /−.289 | /.28(4) | /(6,7,14,20,25,26) | /−.384 | /.29(1) | /(6,14) |
| Verbal delayed |
Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 11a | Mild vs. Ctrl | −.355 | .19(1) | (1) | −.180 | .20(1) | (2) | −.085 | .22(1) | (3) | |||
| Mod vs. Ctrl | −.492 | .28(1) | (1) | −.669 | .34(2) | * | (2,22) | −.263 | .34(1) | (3) | |||
| Sev vs. Ctrl | −.671 | .23(2) | * | (1,24) | −.861 | .18(3) | * | (2,6) | −.878 | .45(3) | * | (3,8,26) | |
| 11b | Mild vs. Mod | −.342 | .21(2) | (1,14) | −.172 | .24(1) | (2) | −.167 | .35(1) | (5) | |||
| Mod vs. Sev | −.401 | .25(2) | (1,14) | −.316 | .30(1) | (2) | −.559 | .26(2) | * | (3,5) | |||
| Mild vs. Sev | −.801 | .21(2) | * | (1,14) | −.491 | .26(1) | (2) | −.653 | .15(3) | * | (3,5,25) |
| Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 11c | Mild | /.120 | /.21(1) | /(14,25) | |||||||||
| Mod | /−.688 | /.36(1) | /(5,22) | ||||||||||
| Sev | /.138 | /.39(1) | /(6,14) | /−.039 | /.42(1) | /(6,14) |
| Visual immediate |
Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 12a | Mild vs. Ctrl | .278 | .19(1) | (1) | −.132 | .20(1) | (2) | .000 | .22(1) | (3) | |||
| Mod vs. Ctrl | −.895 | .29(1) | * | (1) | −.694 | .50(2) | (2,22) | .061 | .34(1) | (3) | |||
| Sev vs. Ctrl | −.346 | .31(1) | (1) | −.907 | .17(3) | * | (2,7) | −.338 | .39(3) | (3,8,9) | |||
| 12b | Mild vs. Mod | −.316 | .24(1) | (1) | −.173 | .24(1) | (2) | −.029 | .17(3) | (3,5) | |||
| Mod vs. Sev | −.289 | .30(1) | (1) | −.238 | .30(1) | (2) | −.455 | .26(2) | (3,5) | ||||
| Mild vs. Sev | −.636 | .27(1) | (1) | −.495 | .26(1) | (2) | −.525 | .23(2) | * | (3,5) |
| Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 12c | Mild | ||||||||||||
| Mod | /−.584 | /.36(1) | /* | /(5,22) | |||||||||
| Sev |
| Visual delayed |
Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 13a | Sev vs. Ctrl | −.836 | .37(1) | * | (8) | ||||||||
| 13b | Mild vs. Mod | .031 | .22(2) | (3,5) | |||||||||
| Mod vs. Sev | −.596 | .40(1) | (5) | ||||||||||
| Mild vs. Sev | −.831 | .33(1) | * | (5) |
| Visual perceptual |
Severity | Time 1 | SE(N) | Sig | Ref | Time 2 | SE(N) | Sig | Ref | Time 3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 14a | Mild vs. Ctrl | .173 | .19(1) | (1) | −.045 | .20(1) | (2) | −.156 | .18(2) | (3,5) | |||
| Mod vs. Ctrl | −.033 | .28(1) | (1) | .000 | .28(1) | (2) | −.171 | .26(2) | (3,5) | ||||
| Sev vs. Ctrl | −.464 | .31(1) | (1) | −.750 | .19(3) | * | (1,27) | −.382 | .16(6) | * | (3,5,9,27) | ||
| 14b | Mild vs. Mod | −.326 | .16(4) | * | (1,10,14) | −.338 | .16(3) | * | (2,10) | −.264 | .15(4) | (3,5,10) | |
| Mod vs. Sev | −.575 | .18(4) | * | (1,10,14) | −.294 | .23(3) | (2,10) | −.279 | .20(4) | (3,5,10) | |||
| Mild vs. Sev | −.891 | .25(4) | * | (1,10,14) | −.608 | .21(3) | * | (2,10) | −.448 | .09(6) | * | (3,5,10,15,28) |
| Visual perceptual |
Severity | T1 vs. T2 | SE(N) | Sig | Ref | T2 vs. T3 | SE(N) | Sig | Ref | T1 vs. T3 | SE(N) | Sig | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 14c | Mild | −.099 | .23(2) | (10) | −.037 | .23(2) | (10) | −.129 | .23(2) | (10) | |||
| Mod | −.257 | .19(2) | (10) | −.007 | .19(2) | (10) | −.265 | .19(2) | (10) | ||||
| Sev | −.594 | .30(2) | * | (10) | −.051 | .27(2) | (10) | −.602 | .43(2) | (10) |
Note. 1 (Jaffe et al., 1992); 2 (Jaffe et al., 1993); 3 (Fay et al., 1994); 4 (Catroppa et al., 2007) 5 (Hawley et al., 2004); 6 (Levin et al., 1994); 7 (Ong et al., 1998); 8 (Parry et al., 2004); 9 (Verger et al., 2000); 10 (Anderson et al., 2005); 11 (Catroppa & Anderson, 2005); 12 (Ewing-Cobbs et al., 1997); 13 (Ayr et al., 2005); 14 (Kinsella et al., 1995); 15 (Brookshire et al., 2000); 16 (Kaufmann et al., 1993); 17 (Anderson et al., 2004); 18 (Chapman et al., 2004); 19 (Levin et al., 2002); 20 (Chapman et al., 2006); 21 (Roncadin et al., 2004); 22 (Lowther & Mayfield, 2004); 23 (Levin et al., 1993); 24 (Roman et al., 1998); 25 (Di Stefano et al., 2000); 26 (Hanten et al., 2000); 27 Lehnung et al., 2003); 28 (Levin et al., 2001).
In subsequent paragraphs, the findings for each severity group is reviewed with references made to the corresponding summary statistic tables. The tables include three sets of statistics. Crosssectional studies summarizing case-control and case-case (more severe compared to less severe) studies are presented in the “a” and “b” rows of Table 1, respectively. In these analyses, a negative case-control effect size indicates that the cases performed more poorly than the controls. Similarly, a negative case-case effect size indicates that the more severe groups performed more poorly than the less severe group. The magnitude of these differences is reflected in the respective weighted mean effect sizes listed in corresponding sections in Table 1. Further, summaries from longitudinal studies addressing recovery over time are presented in the corresponding “c” rows of Table 1, and compare the more proximal evaluation to a later evaluation. For example, a negative effect size comparing the Time 1 and Time 2 data points from longitudinal analyses indicate that the Time 2 scores are comparatively higher. The magnitude of the effect sizes provides a standardized measure of the degree of the differences, which we have interpreted as recovery. Table 2 lists all of the neurocognitive measures contributing to the effect sizes tabulated by domain.
Table 2. List of Measures Used in Meta-Analysis for Each Neurocognitive Domain.
| Domain | Measures |
|---|---|
| Intelligence | Editions of the the Wechsler Scales of Intelligence (Preschool, Child, Adult), Stanford-Binet Intelligence Scales, and the respective composite scores derived from these measures (e.g., FSIQ, VIQ, PIQ). |
| Processing speed/reaction time | Tests of reaction time (e.g., CANTAB) or the Processing Speed Index (PSI) of the Wechsler Scales (or subtest scores comprising the PSI when PSI not reported). |
| Attention |
Paper/pencil measures: Trails A and B, Letter Cancellation Test, subtests of the TEA-Ch, and contingency naming tests. |
| Computerized measures: versions of the Continuous Performance Tests. | |
| Working memory | Versions of verbal and visual span tests and n-back tests, Wechsler Scales Working Memory (WMI) or Freedom from Distractibility (FDI) Indices (or subtest scores comprising the latter when WMT or FDI not reported). |
| Fluency | Timed verbal fluency tests (category or letter). |
| Inhibition | Versions of the Go-No Go test and the Interference subtest of the Stroop. |
| Problem solving | Measures of planning and problem solving, including WCST, the Category Test, Stockings of Cambridge (CANTAB), delayed alternation tasks, Tower of London Test, and the 20 Questions Test. |
| Memory | Subtests and composites from various batteries of verbal/nonverbal, immediate/delayed memory, including CMS, CVLT, TOMAL, WRAML, Rivermead Behavioral Memory Test, Rey-O, RAVLT, and several nonpublished/experimental list learning tasks. |
| Visual spatial | Measures of visual motor and visual perceptual processing, including the Perceptual Organization Index from Wechsler Scales, Tactual Performance Location trial, copy trial of the Rey-Osterrieth Complex Figure, Benton’s Line Orientation Test, and various versions of the Mazes test (Kiel Locomotor Maze, Austin Maze, Porteus Maze). |
Outcomes After Mild TBI
Case-control studies (Table 1, rows 1–14a) showed negligible or small differences between the Mild and Control groups at all time points for FSIQ, PIQ, working memory, problem solving, visual immediate memory, and visual perceptual functioning. Negligible differences were also noted for VIQ and attention through Time 2, but small effects were noted at Time 3. The apparent effect size increase in VIQ was present even if only the single study contributing to all three time points was considered. The small effect noted for attention at Time 3, on the other hand, was due largely to a study of a younger age at injury cohort (not in earlier analyses). Small group differences were apparent up to 2 years post injury in verbal immediate and delayed memory, which resolved by Time 3. Small to moderate effects were noted for processing speed at all time points. Finally, generally negligible differences in fluency were noted at Time 1. This difference, however, appeared to get larger over time and was in the moderate range by Time 3. (The single study contributing to this statistic was also based on data from a younger age at injury cohort).
Case-case studies (Table 1, rows 1–14b) showed no differences between the Mild and Moderate groups at any time point in verbal immediate memory and fluency, and at Time 3 for visual delayed memory. Although no meaningful group differences in problem solving were apparent at Time 1, the groups are better differentiated over time, with a large effect size noted by Time 3. Across all three time points, small (and frequently negligible) effects were apparent for attention, working memory, and verbal delayed memory whereas small to moderate effects were noted for VIQ (resolved by Time 3), PIQ, processing speed, and visual perceptual functioning. For visual immediate memory, a moderate effect size (although inconsistent across studies) was apparent at Time 1, with groups less differentiated over time.
Longitudinal studies (Table 1, rows 1-14c) did not show changes in VIQ, FSIQ, attention, working memory, or visual perceptual functioning. There were no longitudinal studies addressing fluency, memory, or inhibition that met study inclusion criteria. However, in both verbal immediate and delayed memory, combining cross-sectional data from studies that used the same measure at Time 1 and Time 3 suggested unremarkable change over time. Small changes for processing speed were noted, with considerable improvements in problem by Time 3.
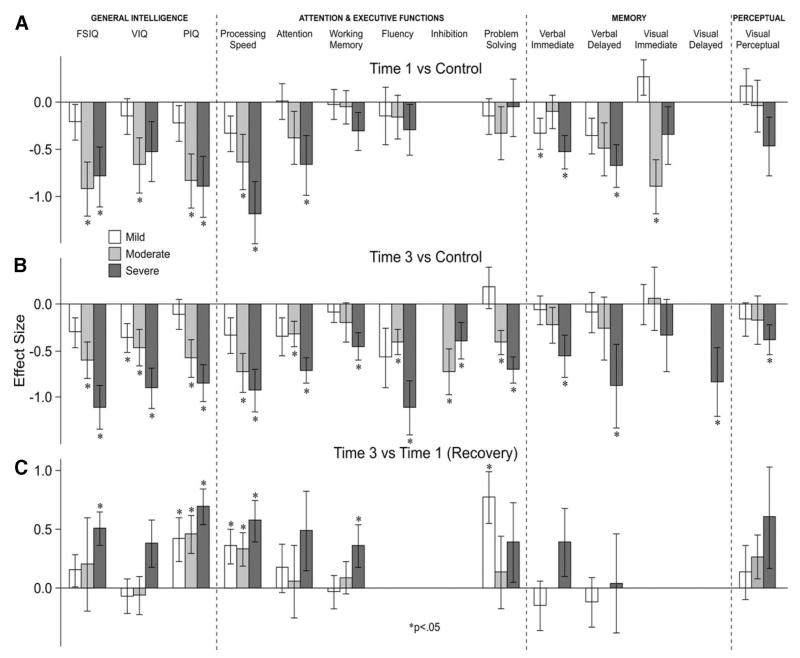
Figure 1 summarizes the effect sizes for three key findings (case-control postacute and chronic studies, and longitudinal studies) from the analyses discussed above. Effect sizes from casecontrol studies show that postacutely (Time 1), the majority of the neurocognitive domains reviewed were either not affected or were minimally affected (see Figure 1A). By Time 3 (chronic phase), some of the impairments apparent at earlier time points had resolved. In several cases, however, increasing case-control differences were apparent by Time 3 (chronic phase) (see Figure 1B). With the exception of VIQ, however, many of the effects were not statistically significant because of relatively large standard errors indicating inconsistency across study results. Of note, large effects in some domains (e.g., fluency) were apparent in studies of a younger age at injury cohort (2–7 at injury) (Anderson, Morse, Catroppa, Haritou, & Rosenfeld, 2004). With few impairments noted postacutely, little, if any, recovery was observed in longitudinal studies by Time 3, with some noteworthy exceptions, including problem solving, PIQ, and processing speed (see Figure 1C).
Figure 1.
Summary of effects between TBI and control groups for each neurocognitive domain in the postacute (Time 1) and chronic (Time 3) phases, and recovery trends. (A) Time 1 (acute/post-acute) versus Control effect sizes by injury severity and domain in cross-sectional studies. (B) Time 3 (chronic) versus Control effect sizes by injury severity and domain in cross-sectional studies. (C) Time 3 versus Time 1 (Recovery) effect sizes by injury severity and domain in longitudinal studies.
Of all the measures administered, problem solving may be one of the more likely domains to be affected by practice effects. Assuming so, the Mild group appears to gain substantially from these effects while the Moderate and Severe groups gain comparably less. Also of interest, the Mild group appears to make notable gains in PIQ and processing speed (factored into the PIQ on Wechsler Scales). Because all scores used in the meta-analysis were standard scores (accounting for age related development), significant changes in performance from Time 1 to Time 3 suggest that the groups made improvements above and beyond that expected during normal development. This finding is somewhat surprising because PIQ and processing speed are typically not prone to practice effects. Also of note, the Mild and Moderate groups, particularly with regard to measures of intelligence, processing speed, attention, and working memory, appear to show the same pattern of “recovery,” despite the Mild group’s smaller discrepancy from Controls. In summary, the Mild TBI group showed generally few, if any, impairments in aspects of general intelligence, attention/executive skills, and memory, as well as some recovery in these areas at around two years post injury.
Outcomes After Moderate TBI
Case-control studies (Table 1, rows 1–14a) showed negligible overall differences between the Moderate and Control groups in visual perceptual functioning, working memory, and verbal immediate memory (with significant inconsistency across studies) at any time point. Generally negligible differences were noted for fluency by Time 2, with a larger discrepancy apparent by Time 3. Small but consistent effects were noted for attention and problem solving at all time points. Small to moderate effects for verbal delayed memory and moderate to large effects for visual immediate memory were apparent through Time 2, with this difference significantly decreasing by Time 3. Finally, large effects for FSIQ, VIQ, and PIQ were present at Time 1, which decreased some by later time points. Large effects for were noted for processing speed and inhibition at Time 3.
Case-case studies (Table 1, rows 1–14b) show negligible differences between the Moderate and Severe groups in working memory at all three time points, as well as inhibition and fluency at Time 3 (no earlier studies were available). Small, and in some cases, negligible, effects were noted at all three time points for verbal and visual immediate memory, problem solving, and fluency. Small to moderate differences were noted for VIQ and processing speed (all three time points), and verbal and visual delayed memory at Time 3. Moderate to large effects were apparent for FSIQ, PIQ, visual perceptual functioning, and attention, initially, with this difference decreasing in magnitude over time.
There were no longitudinal studies of memory, fluency, or inhibition. However, in both verbal delayed and visual immediate memory, combining cross-sectional data from studies using the same measures at Time 2 and Time 3 suggested moderate changes over time. Longitudinal studies of FSIQ, PIQ, processing speed, attention, problem solving, and visual perceptual functioning showed some improvement (small to moderate) in the first 2 years post injury, with no observable changes thereafter. Further, no improvements in VIQ or working memory were apparent. These results are presented in Table 1 (rows 1–14c).
The summary graphs show significant case-control effects postacutely, although in some cases inconsistent across studies, in several neurocognitive domains, including general intellectual functioning, processing speed, attention, problem solving, as well as visual immediate and verbal delayed memory. No impairments in verbal immediate memory and visual perceptual functioning were observed (see Figure 1A). By the chronic phase (Time 3), deficits in intellectual functioning persisted, although considered smaller in magnitude compared to postacute studies (see Figure 1B). There were also significant impairments in executive skills, including processing speed, attention, fluency, inhibition, and problem solving. In contrast, working memory, memory, and visual perceptual skills appeared largely commensurate with the Controls (see Figure 1B). Although few longitudinal studies were available for review, substantial improvement in intellectual functioning (specifically PIQ) and processing speed were apparent, with no changes in VIQ, attention, working memory, problem solving, or visual perceptual functioning noted (see Figure 1C).
Outcomes After Severe TBI
Case-control studies (Table 1, rows 1–14a) showed small group differences at Time 1 for fluency and problem solving, with this difference appearing substantially larger over time (in the very large range by Time 3). Small to moderate effects were noted for working memory and visual immediate memory, with the largest difference noted for working memory at Time 3 and visual immediate memory at Time 2. Small but statistically significant effects were apparent for inhibition at Time 3. Moderate effects were apparent for VIQ at Time 1, with the effect size almost doubling by Time 3, suggesting that the gap between the groups expands over time. Moderate to large effects were observed for attention, verbal immediate and delayed memory, and visual perceptual functioning. The latter differences persisted even at Time 3 and, in some cases (e.g., verbal delayed memory), increased over time. Large effects were noted for FSIQ, PIQ, and processing speed across all three time points, with significant increases in group differences by Time 2 for FSIQ. Large effects were also evident for visual delayed memory at Time 3.
Case-case analyses are presented in Table 1 (rows 1–14b). There were no meaningful differences between the Moderate and Severe groups for working memory at any time point or inhibition at Time 3. There were, however, moderate differences in working memory and fluency between the Severe and Mild groups at Time 1, which diminished over time. Small to moderate differences were noted at all time points for verbal and visual immediate memory. Moderate to large effects between the Severe and both the Mild and Moderate groups were also apparent for FSIQ, VIQ, attention, problem solving, and visual perceptual functioning (all of which decreased over time), verbal delayed memory (consistent over time), and visual delayed memory at Time 3. Large to very large differences were noted for PIQ and processing speed, with both effect sizes decreasing over time. In all analyses, the Severe group was better differentiated from the Mild than the Moderate group.
There were no longitudinal studies of memory, inhibition, or fluency. However, combining cross-sectional data from various studies using the same measures from different time points suggested a small amount of improvement in verbal immediate memory, with no such improvements observed for verbal delayed memory. No improvements in problem solving were noted. Small changes in VIQ, working memory, attention, and visual perceptual functioning were noted over time. In contrast, moderate to large improvements were apparent in FSIQ, PIQ, processing speed, and visual perceptual functioning by Time 2, with no changes observed thereafter. Longitudinal study results are presented in Table 1 (rows 1–14c).
The summary graphs indicate significant impairments in general intellectual functioning (in PIQ more so than in VIQ), aspects of executive functioning (especially processing speed and attention), as well as verbal memory (immediate and delayed) in the Severe TBI group compared to Controls (see Figure 1A). Deficits in working memory, fluency, and visual perceptual skills were also apparent, but studies did not report impairments in these domains on a consistent basis (see Figure 1A). In contrast, by the chronic phase (Time 3), significant impairments in almost all neurocognitive domains were noted, with effect sizes that were significantly larger than the effect sizes derived from comparable postacute studies (see Figure 1B). Specifically, substantial deficits were apparent in general intellectual functioning (large to very large effects), verbal memory (moderate to large effects), and visual perceptual skills (small effects). Impairments were also noted for all aspects of executive skills, with the most impacted domains (large to very large effect sizes) observed for fluency, processing speed, attention, and problem solving. The effect sizes for working memory and inhibition were in the small to moderate range, but consistent enough across studies to achieve statistical significance (see Figure 1B). Longitudinal studies of severe TBI indicated substantial recovery in intellectual functioning, which was especially true for PIQ relative to VIQ. Small to moderate recovery in several aspects of executive functioning, processing speed, and working memory, were also observed. There was moderate improvement in visual perceptual skills, but due to considerable variability in reported outcomes, statistical significance was not reached. (see Figure 1C). Of interest, one of the largest case-control effect sizes in the Severe TBI analyses across several domains was in one of two studies where reportedly no exclusion criteria were implemented (Parry et al., 2004). Although this may have resulted in larger effects than the remaining studies, it is unlikely that premorbid neurocognitive status explained the full extent of the case-control differences observed.
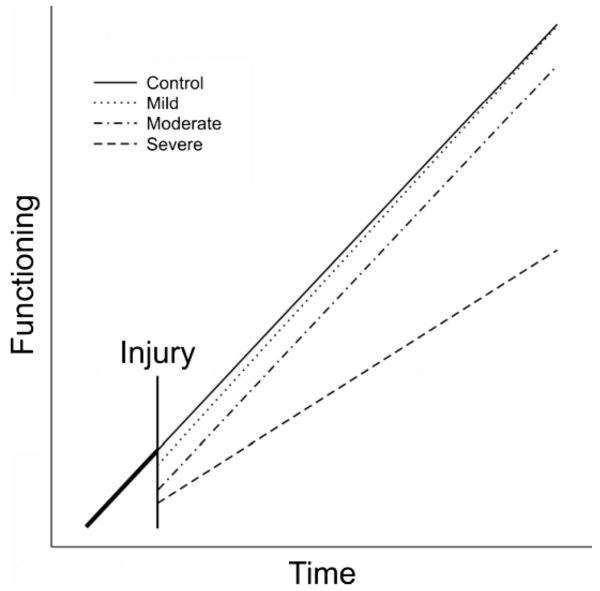
Figure 2 indicates a theoretical summary model of recovery after pediatric TBI by severity group generalized across all neurocognitive domains reviewed. Although recovery trends are based on patterns emerging from this meta analysis, the slopes are only a summary model and not based on raw data. The emerging pattern of recovery suggests that the little impairment, if any, observed in the Mild TBI group resolves over time so that this group ultimately resembles the Controls. In contrast, there are notable deficits in the Moderate group and although this group shows recovery relative to their acute functioning, they do not catch up to the Control group. The Severe TBI group, however, despite some improvements relative to functioning in the acute stage, shows a slower rate of development so that the gap between the Severe and Control groups expands over time.
Figure 2.
Summary diagram of trends in neurocognitive outcomes and recovery over time.
Discussion
One of the striking findings from this review is that despite the relatively large volume of studies addressing functional outcomes and recovery following pediatric TBI, there are remarkably few studies with well defined and discrete severity groups, time points post injury, and age bands at the time of injury. This, in addition to the necessity for having descriptive statistical data to conduct a meta-analytic review, substantially reduced the number of studies that could be summarized. Nonetheless, data from available studies that met inclusion criteria were systematically summarized and reviewed in this paper, yielding empirically and clinically useful information regarding injury outcomes by neurocognitive domain at various defined time points post injury (cross-sectional studies), as well as the time course of recovery (longitudinal studies).
Studies of mild TBI included in the analyses showed few, if any, impairments in the neurocognitive domains reviewed at any time point, including postacute outcomes. This is consistent with previous literature (Bijur, Haslum, & Golding, 1990; Satz et al., 1997). Of note, however, there were some studies reporting substantial impairments in the mild TBI group, even at Time 3. For example, data from one study of a relatively younger TBI sample (2-7 years at injury and 5 years post injury) contributed effect sizes in the moderate to large range (with one exception) on four different paper and pencil measures of attention (Catroppa, Anderson, Morse, Haritou, & Rosenfeld, 2007). Conversely, a study of comparatively older children (6–15 years at injury and 3 years post injury) resulted in no notable differences between cases and controls (Fay et al., 1994). Further, a large British cohort of mild head injury in children found no differences between cases and healthy controls or other nonhead injury orthopedic controls in any aspect of neurocognitive ability or behavioral functioning (Bijur et al., 1990). Although most studies found no statistically significant effects of mild TBI on neurocognitive functioning as a group, some suggested that there may be a subset of children with mild TBI who show adverse outcomes in some domains. The inconsistencies across studies in the outcomes of mild TBI may be due to several factors.
First, differences in outcome may be because of the age at injury ranges included in studies. Although we could not statistically capture the effects of age at injury in this meta-analysis because of the small number of studies on the younger age at injury group, prior studies have shown poorer outcome in younger age at injury groups, despite greater plasticity (Anderson & Moore, 1995; Anderson et al., 2004; Dennis, 2000). Second, there were marked methodological differences in the studies reviewed, which may have contributed to the relatively wide range of outcomes. These differences included how severity groups were defined and the source of patient referrals (prospective vs. convenience/clinic samples). Methodological differences in outcome studies of mild TBI in children have been previously reviewed (Lee, 2007; Satz et al., 1997). Further, perhaps children with mild TBI showing adverse outcomes were misdiagnosed. Third, effect sizes for most of the domains where some case-control differences were observed were quite small, generally ranging between .2 and .3, with one exception (.57 for fluency at Time 3). Consequently, the Mild TBI group did not show a level of impairment post-TBI where it would be implausible that their functioning changed from premorbid levels. Indeed, preinjury AD/HD and behavioral problems are present at higher rates (13–22%) in children with TBI, albeit in more severe injury groups (Bloom et al., 2001; Max et al., 1998) than in the general pediatric population (APA, 1994). Further, these premorbid symptoms help predict post injury neurobehavioral outcomes (Schachar, Levin, Max, Purvis, & Chen, 2004). Hyperactivity and attentional deficits may result in children’s behavior being a risk factor for their injury (Max et al., 2004). In addition, some studies have reported a high rate of premorbid learning disabilities or poor academic performance in individuals who suffer a mild TBI, with rates as high as 50% (Dicker, 1992). Therefore, although many of the studies excluded children with known premorbid neurological problems or prior head injuries, the rate of premorbid neurocognitive and neurobehavioral deficits, albeit subtle, may potentially have contributed to adverse post injury outcomes. Because of the relatively high prevalence of preinjury neurocognitive and neurobehavioral problems, the extent to which the presence of these factors are excluded from analyses is of concern when studying the mild TBI population. When evaluating the effect of mild TBI on neurocognitive functioning, it is critically important to control for the preinjury levels of cognitive functioning (Asarnow, Satz, Light, Lewis, & Neumann, 1991). Alternatively, a subgroup of the mild TBI population, the “miserable few,” may experience neurocognitive impairments chronically post mild TBI, in the absence of premorbid difficulties. Differentiating between these two groups is critical, especially in any efforts to elucidate the underlying pathological processes, frequently opaque on conventional neuroimaging studies, that explain morbidity in a select group.
In general, the Moderate TBI group performed more poorly than the Mild group and better than the Severe group, consistent with a dose-response relationship between severity of injury and outcome. The Moderate group was more similar to the Severe than the Mild injury group, especially on measures of intellectual functioning and processing speed at Time 1. In general, memory skills and visual perceptual skills were similar to Controls by Time 3. Despite modest recovery in intellectual functioning and attention, the deficits in children with Moderate TBI persist even after 2 years post injury compared to controls, suggesting that they do not fully catch up to their demographically matched peers.
Studies of the neurocognitive outcomes and recovery after a severe TBI revealed robust and significant impairments, with moderate to very large effects noted for intellectual functioning (primarily PIQ), executive functioning (processing speed and attention), as well as verbal immediate and delayed memory at Time 1. By Time 3, however, impairments in all of the neurocognitive domains reviewed emerged. Small effects were noted for visual perceptual functioning, visual immediate memory, and inhibition; moderate effects were noted for verbal immediate memory; and large to very large effects were noted for general intellectual functioning (VIQ and PIQ), executive functions (processing speed, attention, fluency, problem solving), and verbal delayed memory. Although it is not surprising that the Severe group showed large effects overall (i.e., was most discrepant from control groups), the comparatively larger effects observed at Time 3 relative to the Time 1 period are particularly noteworthy. It appears that there are significant and persistent neurocognitive impairments in a subset of children with severe TBI. Despite some recovery over the course of the first 2 years post injury, the Severe TBI group, across most neurocognitive domains, not only fails to catch up to its peers, but also appears to fall farther behind over time. Because this finding was somewhat unexpected and intriguing, we looked across studies to see if the effect sizes increased with longer post injury interval in the severe TBI group. Consistent with our initial analyses, with few exceptions, there were relatively larger effect sizes noted for studies with longer mean post injury intervals. This finding, however, was somewhat confounded by age at injury, with younger age at injury groups showing larger discrepancies compared to controls versus older groups. Children with severe TBI may not make developmentally appropriate gains. This reduced rate of normal developmental progress has been described as a “double hazard” injury model (i.e., severe TBI and younger age at injury) (Anderson, Catroppa, Morse, Haritou, & Rosenfeld, 2005; Kriel, Krach, & Panser, 1989). Similar findings have been reported in academic outcomes after severe TBI (Anderson et al., 2006; Ewing-Cobbs et al., 2004). This interference in normal development may be due to injury consequences, which disrupt existing neural networks and impede the process of learning (Hebb, 1942). In addition, other factors may, in part, account for the decline in the rate of development in this group, including lack of exposure to learning opportunities (e.g., missing school because of hospitalizations and treatments) as well as medical treatments/procedures (including physical rehabilitation). Regardless, the findings from this review on the outcomes of severe TBI highlight the importance of focused and specific interventions to mitigate this problem in children with severe TBI.
Across severity groups and post injury time points, meta-analytic findings suggest that the neurocognitive domain most resistant to the impact of injury is visual perceptual functioning, and to some degree visual immediate memory. At Time 1, the least affected domains across severity groups included aspects of executive skills (fluency, problem solving, and to some degree working memory). Although the effect sizes for these domains at Time 3 were relatively larger compared to Time 1, the effects for working memory, visual immediate memory, and visual perception were among the smallest across severity groups. In contrast, domains that appeared most sensitive to TBI across severity groups, including both Time 1 and Time 3 evaluations, were intellectual functioning (PIQ more than VIQ in most cases), processing speed, attention, and, to a lesser degree, verbal memory. At Time 3 only, fluency and problem solving also appeared sensitive to TBI (especially for the Severe group). Finally, the longitudinal analyses suggested that the domains showing the most recovery include intellectual functioning (primarily PIQ) and processing speed (frequently factored into PIQ). It is important, however, to consider the psychometric properties of the measures used to evaluate the neurocognitive domains reviewed in this study. It is possible that the apparent differential sensitivity of neurocognitive domains to the effects of TBI partially reflects the relative psychometric properties of the tests used to assess the domain. The fact that some domains appear to be minimally affected by TBI while others are significantly affected may be because of poor measurement and not necessarily reflective of impairment or lack thereof in a given skill set (Strauss & Allred, 1987).
Limitations and Future Directions
A significant limitation of this meta-analysis was that many published studies could not be included because they did not have discrete intervals post injury and severity ratings for which effect sizes could be derived. Also excluded were studies that did not report scores in a form from which effect sizes could be calculated. The unfortunate consequence was that there were, at times, a small number or single studies used to derive the statistics in certain domains. In some instances, it was difficult to know precisely how to assign a value for a moderating variable (e.g., injury severity and/or time post injury) in a given study. This may have introduced error when examining the effects of those moderator variables.
There are few studies that report on injury severity outcomes separately within well-defined time spans. There are even a smaller number that report on longitudinal outcomes. For a better understanding of the course of recovery, we need more longitudinal studies with well-defined severity indicators and discrete time points post injury. In addition, longitudinal studies with smaller and better defined age at injury time bands are necessary so that the effects of normal development and its interruption because of a head injury can be adequately evaluated. Finally, in an attempt to control for premorbid variables contributing to outcome, the control group for comparison should be carefully chosen. There were only a handful of studies that used an other injury control group instead of healthy control groups.
Acknowledgments
Support for this work was funded by an NIH/NINDS fellowship (F32NS053169) and a fellowship through the Della Martin Foundation awarded to the primary author.
References
References marked with an asterisk indicate studies included in the meta-analysis.
- Anderson VA, Catroppa C, Dudgeon P, Morse SA, Haritou F, Rosenfeld JV. Understanding predictors of functional recovery and outcome 30 months following early childhood head injury. Neuropsychology. 2006;20:42–57. doi: 10.1037/0894-4105.20.1.42. [DOI] [PubMed] [Google Scholar]
- *.Anderson VA, Catroppa C, Morse S, Haritou F, Rosenfeld J. Functional plasticity or vulnerability after early brain injury? Pediatrics. 2005;116:1374–1382. doi: 10.1542/peds.2004-1728. [DOI] [PubMed] [Google Scholar]
- Anderson VA, Moore C. Age at injury as a predictor of outcome following pediatric head injury. Child Neuropsychology. 1995;1:187–202. [Google Scholar]
- *.Anderson VA, Morse SA, Catroppa C, Haritou F, Rosenfeld JV. Thirty month outcome from early childhood head injury: A prospective analysis of neurobehavioural recovery. Brain. 2004;127(Pt 12):2608–2620. doi: 10.1093/brain/awh320. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Asarnow RF, Satz P, Light R, Lewis R, Neumann E. Behavior problems and adaptive functioning in children with mild and severe closed head injury. Journal of Pediatrics Psychology. 1991;16:543–555. doi: 10.1093/jpepsy/16.5.543. [DOI] [PubMed] [Google Scholar]
- Asarnow RF, Satz P, Light R, Zaucha K, Lewis R, McCleary C. The UCLA study of mild closed head injury in children and adolescents. In: Broman SH, Michel ME, editors. Traumatic brain injury in children. Oxford University Press; New York: 1995. pp. 117–146. [Google Scholar]
- *.Ayr LK, Yeates KO, Enrile BG. Arithmetic skills and their cognitive correlates in children with acquired and congenital brain disorder. Journal of the International Neuropsychological Society. 2005;11:249–262. doi: 10.1017/S1355617705050307. [DOI] [PubMed] [Google Scholar]
- Bijur PE, Haslum M, Golding J. Cognitive and behavioral sequelae of mild head injury in children. Pediatrics. 1990;86:337–344. [PubMed] [Google Scholar]
- Bloom DR, Levin HS, Ewing-Cobbs L, Saunders AE, Song J, Fletcher JM, et al. Lifetime and novel psychiatric disorders after pediatric traumatic brain injury. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:572–579. doi: 10.1097/00004583-200105000-00017. [DOI] [PubMed] [Google Scholar]
- Boll TJ. Minor head injury in children: Out of sight but not out of mind. Journal of Clinical Child Psychology. 1983;12:74–80. [Google Scholar]
- Borenstein M, Hedges L, Higgins H, Rothstein H. Comprehensive meta analysis (Version Second) Biostat; Englewood, NJ: 2005. [Google Scholar]
- Borenstein M, Hedges L, Rothstein H. Meta-analysis fixed effect vs. random effects. 2007 doi: 10.1002/jrsm.12. Unpublished manuscript, www.Meta-Analysis.com. [DOI] [PubMed]
- *.Brookshire BL, Chapman SB, Song JB, Levin HS. Cognitive and linguistic correlates of children’s discourse after closed head injury: A 3-year follow-up. Journal of International Neuropsychological Society. 2000;6:741–751. doi: 10.1017/s1355617700677019. [DOI] [PubMed] [Google Scholar]
- *.Catroppa C, Anderson V. A prospective study of the recovery of attention from acute to 2 years following pediatric traumatic brain injury. Journal of the International Neuropsychological Society. 2005;11:84–98. doi: 10.1017/S1355617705050101. [DOI] [PubMed] [Google Scholar]
- *.Catroppa C, Anderson VA, Morse SA, Haritou F, Rosenfeld JV. Children’s attentional skills 5 years post-TBI. Journal of Pediatrics Psychology. 2007;32:354–369. doi: 10.1093/jpepsy/jsl019. [DOI] [PubMed] [Google Scholar]
- CDC Traumatic brain injury in the United States: Assessing outcomes in children. 20002008 from http://www.cdc.gov/ncipc/tbi_report/09_Appendix_B.htm.
- *.Chapman SB, Sparks G, Levin HS, Dennis M, Roncadin C, Zhang L, et al. Discourse macrolevel processing after severe pediatric traumatic brain injury. Developmental Neuropsychology. 2004;25:37–60. doi: 10.1080/87565641.2004.9651921. [DOI] [PubMed] [Google Scholar]
- *.Chapman SB, Gamino JF, Cook LG, Hanten G, Li X, Levin HS. Impaired discourse gist and working memory in children after brain injury. Brain Language. 2006;97:178–188. doi: 10.1016/j.bandl.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Academic Press; New York: 1988. [Google Scholar]
- Dennis M. Childhood medical disorders and cognitive impairment: Biological risk, time, development, and reserve. In: Yeates KO, Ris MD, Taylor HG, editors. Pediatric neuropsychology: Research, theory, and practice. 3-22. Guilford Press; New York: 2000. [Google Scholar]
- Dicker BG. Profile of those at risk for minor head injury. Journal of Head Trauma Rehabilitation. 1992;7:83–91. [Google Scholar]
- *.Di Stefano G, Bachevalier J, Levin HS, Song JX, Scheibel RS, Fletcher JM. Volume of focal brain lesions and hippocampal formation in relation to memory function after closed head injury in children. Journal of Neurology, Neurosurgery, & Psychiatry. 2000;69:210–216. doi: 10.1136/jnnp.69.2.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing-Cobbs L, Barnes M, Fletcher JM, Levin HS, Swank PR, Song J. Modeling of longitudinal academic achievement scores after pediatric traumatic brain injury. Developmental Neuropsychology. 2004;25:107–133. doi: 10.1080/87565641.2004.9651924. [DOI] [PubMed] [Google Scholar]
- *.Ewing-Cobbs L, Fletcher JM, Levin HS, Francis DJ, Davidson K, Miner ME. Longitudinal neuropsychological outcome in infants and preschoolers with traumatic brain injury. Journal of the International Neuropsychological Society. 1997;3:581–591. [PubMed] [Google Scholar]
- *.Fay GC, Jaffe KM, Polissar NL, Liao S, Rivara JB, Martin KM. Outcome of pediatric traumatic brain injury at three years: A cohort study. Archives of Physical Medicine and Rehabilitation. 1994;75:733–741. [PubMed] [Google Scholar]
- Geddes JF, Hackshaw AK, Vowles GH, Nickols CD, Whitwell HL. Neuropathology of inflicted head injury in children. I. Patterns of brain damage. Brain. 2001;124(Pt. 7):1290–1298. doi: 10.1093/brain/124.7.1290. [DOI] [PubMed] [Google Scholar]
- Gilles EE. Nonaccidental head injury. In: Swaiman KF, Ashwal S, editors. Pediatric neurology: Principles and practice. Mosby; St. Louis, MO: 1999. pp. 898–914. [Google Scholar]
- *.Hanten G, Bartha M, Levin HS. Metacognition following pediatric traumatic brain injury: A preliminary study. Developmental Neuropsychology. 2000;18:383–398. doi: 10.1207/S1532694206Hanten. [DOI] [PubMed] [Google Scholar]
- *.Hawley CA, Ward AB, Magnay AR, Mychalkiw W. Return to school after brain injury. Archives of Disease in Children. 2004;89:136–142. doi: 10.1136/adc.2002.025577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hebb D. The effect of early and late brain injury upon test scores, and the nature of normal adult intelligence. Proceedings of the American Philosophical Society. 1942;85:265–292. [Google Scholar]
- *.Jaffe KM, Fay GC, Polissar NL, et al. Severity of pediatric traumatic brain injury and early neurobehavioral outcome: A cohort study. Archives of Physical Medicine and Rehabilitation. 1992;73:540–547. [PubMed] [Google Scholar]
- *.Jaffe KM, Fay GC, Polissar NL, Martin KM, Shurtleff HA, Rivara JM, et al. Severity of pediatric traumatic brain injury and neurobehavioral recovery at one year: A cohort study. Archives of Physical Medicine and Rehabilitation. 1993;74:587–595. doi: 10.1016/0003-9993(93)90156-5. [DOI] [PubMed] [Google Scholar]
- *.Kaufmann PM, Fletcher J, Levin H, Miner M, Ewing-Cobbs L. Attentional disturbance after pediatric closed head injury. Journal of Child Neurology. 1993;8:348–353. doi: 10.1177/088307389300800410. [DOI] [PubMed] [Google Scholar]
- Kinsella G, Prior M, Sawyer M, Murtagh D, Eisenmajer R, Anderson V, et al. Neuropsychological deficit and academic performance in children and adolescents following traumatic brain injury. Journal of Pediatric Psychology. 1995;20:753–767. doi: 10.1093/jpepsy/20.6.753. [DOI] [PubMed] [Google Scholar]
- Kriel RL, Krach LE, Panser LA. Closed head injury: Comparison of children younger and older than 6 years of age. Pediatric Neurology. 1989;5:296–300. doi: 10.1016/0887-8994(89)90021-0. [DOI] [PubMed] [Google Scholar]
- *.Lee LK. Controversies in the sequelae of pediatric mild traumatic brain injury. Pediatric Emergency Care. 2007;23:580–583. doi: 10.1097/PEC.0b013e31813444ea. quiz 584-586. [DOI] [PubMed] [Google Scholar]
- Lehnung M, Leplow B, Ekroll V, Benz B, Ritz A, Mehdorn M, et al. Recovery of spatial memory and persistence of spatial orientation deficits after traumatic brain injury during childhood. Brain Injury. 2003;17:855–869. doi: 10.1080/0269905031000089369. [DOI] [PubMed] [Google Scholar]
- *.Levin HS, Hanten G. Executive functions after traumatic brain injury in children. Pediatric Neurology. 2005;33:79–93. doi: 10.1016/j.pediatrneurol.2005.02.002. [DOI] [PubMed] [Google Scholar]
- *.Levin HS, Culhane KA, Fletcher JM, Mendelsohn DB, Lilly MA, Harward H, et al. Dissociation between delayed alternation and memory after pediatric head injury: Relationship to MRI findings. Journal of Child Neurology. 1994;9:81–99. doi: 10.1177/088307389400900121. [DOI] [PubMed] [Google Scholar]
- *.Levin HS, Hanten G, Chang CC, Zhang L, Schachar R, Ewing-Cobbs L. Working memory after traumatic brain injury in children. Annals of Neurology. 2002;52:82–88. doi: 10.1002/ana.10252. [DOI] [PubMed] [Google Scholar]
- *.Levin HS, Culhane KA, Mendelsohn D, Lilly MA, Bruce D, Fletcher JM, et al. Cognition in relation to MRI in head-injured children and adolescents. Archives of Neurology. 1993;50:897–905. doi: 10.1001/archneur.1993.00540090008004. [DOI] [PubMed] [Google Scholar]
- *.Levin HS, Song J, Ewing-Cobbs L, Roberson G. Porteus Maze performance following traumatic brain injury in children. Neuropsychology. 2001;15:557–567. doi: 10.1037//0894-4105.15.4.557. [DOI] [PubMed] [Google Scholar]
- Lowther JL, Mayfield J. Memory functioning in children with traumatic brain injuries: A TOMAL validity study. Archives of Clinical Neuropsychology. 2004;19:105–118. doi: 10.1016/s0887-6177(02)00222-6. [DOI] [PubMed] [Google Scholar]
- Max JE, Koele SL, Smith WL, Jr., Sato Y, Lindgren SD, Robin DA, et al. Psychiatric disorders in children and adolescents after severe traumatic brain injury: A controlled study. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:832–840. doi: 10.1097/00004583-199808000-00013. [DOI] [PubMed] [Google Scholar]
- Max JE, Lansing AE, Koele SL, Castillo CS, Bokura H, Schachar R, et al. Attention deficit hyperactivity disorder in children and adolescents following traumatic brain injury. Developmental Neuropsychology. 2004;25:159–177. doi: 10.1080/87565641.2004.9651926. [DOI] [PubMed] [Google Scholar]
- *.McCartney K, Rosenthal R. Effect size, practical importance, and social policy for children. Child Development. 2000;71:173–180. doi: 10.1111/1467-8624.00131. [DOI] [PubMed] [Google Scholar]
- *.Ong LC, Chandran V, Peng R. Outcome of closed head injury in Malaysian children: Neurocognitive and behavioral sequelae. Journal of Paediatrics and Child Health. 1998;34:363–368. doi: 10.1046/j.1440-1754.1998.00239.x. [DOI] [PubMed] [Google Scholar]
- *.Parry L, Shores A, Rae C, Kemp A, Waugh MC, Chaseling R, et al. An investigation of neuronal integrity in severe paediatric traumatic brain injury. Child Neuropsychology. 2004;10:248–261. doi: 10.1080/09297040490909279. [DOI] [PubMed] [Google Scholar]
- *.Roman MJ, Delis DC, Willerman L. Impact of pediatric traumatic brain injury on components of verbal memory. Journal of Clinical and Experimental Neuropsychology. 1998;20:245–258. doi: 10.1076/jcen.20.2.245.1168. [DOI] [PubMed] [Google Scholar]
- Roncadin C, Guger S, Archibald J, Barnes M, Dennis M. Working memory after mild, moderate, or severe childhood closed head injury. Developmental Neuropsychology. 2004;25:21–36. doi: 10.1080/87565641.2004.9651920. [DOI] [PubMed] [Google Scholar]
- Rosenthal R, DiMatteo MR. Meta-analysis: Recent developments in quantitative methods for literature reviews. Annual Review of Psychology. 2001;52:59–82. doi: 10.1146/annurev.psych.52.1.59. [DOI] [PubMed] [Google Scholar]
- Satz P, Zaucha K, McCleary C, Light R, Asarnow R, Becker D. Mild head injury in children and adolescents: A review of studies (1970-1995) Psychological Bulletin. 1997;122:107–131. doi: 10.1037/0033-2909.122.2.107. [DOI] [PubMed] [Google Scholar]
- Schachar R, Levin HS, Max JE, Purvis K, Chen S. Attention deficit hyperactivity disorder symptoms and response inhibition after closed head injury in children: Do preinjury behavior and injury severity predict outcome? Developmental Neuropsychology. 2004;25:179–198. doi: 10.1080/87565641.2004.9651927. [DOI] [PubMed] [Google Scholar]
- *.Strauss ME, Allred LJ. Measurement of differential cognitive deficits after head injury. In: Levin HS, Grafman J, Eisenberg HM, editors. Neurobehavioral recovery from head injury. Oxford University Press; New York: 1987. [Google Scholar]
- Verger K, Junqué C, Jurado MA, Tresserras P, Bartumeus F, Nogues P, et al. Age effects on long-term neuropsychological outcome in pediatric traumatic brain injury. Brain Injury. 2000;14:495–503. doi: 10.1080/026990500120411. [DOI] [PubMed] [Google Scholar]