Abstract
Purpose
To study the effects of long-term treatment with potassium magnesium citrate and vitamin B-6 prophylaxis (Urikind-KM6; 1,100-mg potassium citrate, 375-mg magnesium citrate, and 20-mg pyridoxine hydrochloride/5 mL) every 8 hours over 3 years.
Materials and Methods
A total of 247 patients with recurrent idiopathic hypocitraturia with or without hyperuricosuria and randomized controls were studied prospectively for 3 years. The total patients were divided into three groups. Control group 1 consisted of 61 patients (24.7%) who had moderate to severe hypocitraturia with or without hyperuricosuria and were recurrent stone formers but discontinued prophylaxis because of drug intolerance within 1 month of therapy. Control group 2 constituted 53 patients (21.5%) who were first-time stone formers and who had mild hypocitraturia with or without hyperuricosuria and were not put on prophylactic therapy and were followed for 3.16±0.08 years. Control group 3 constituted 133 patients (54.8%) who were recurrent stone formers who had moderate to severe hypocitraturia with or without hyperuricosuria and were put on prophylaxis therapy and were followed for 3.16±0.08 years. All patients were followed up at 6-month intervals.
Results
Potassium magnesium citrate prophylaxis produced a sustained increase in 24-hour urinary citrate excretion from initially low values (221.79±13.39 mg/dL) to within normal to high limits (604.04±5.00 mg/dL) at the 6-month follow-up. Urinary pH rose significantly from 5.62±0.2 to 6.87±0.01 and was maintained at 6.87±0.01. The stone recurrence rate declined from 3.23±1.04 per patient per year to 0.35±0.47 per patient per year.
Conclusions
Potassium magnesium citrate prophylaxis was effective in reducing the recurrence of calcium oxalate and phosphate urolithiasis.
Keywords: Calcium oxalate, Potassium-magnesium citrate, Pyridoxine, Urolithiasis
INTRODUCTION
Urolithiasis is a major health problem with a worldwide prevalence of between 2% and 20% [1]. International epidemiological data suggest that the incidence and prevalence of stone disease is increasing [2]. It is estimated that almost 50% of stone formers will experience recurrence within 10 years [3]. More specifically, high fructose consumption, which promotes obesity; reduced fluid intake; and increased calcium, oxalate, sodium, and animal protein intake have all been identified as risk factors for kidney stones [4,5,6,7]. The risk of urolithiasis is greater in individuals with a family history of stone disease [8]. The risk in those individuals is estimated to be more than 2.5 times that in persons without a family history of stone disease [9]. Primary hyperparathyroidism may be found in 5% of stone formers [10]. Different theories as to the pathophysiological mechanisms of lithogenesis have been proposed, including free and fixed particle theories and Randal's plaque hypothesis [11]. The main types of renal stones are calcium oxalate (59%), calcium phosphate (10%), uric acid (17%), struvite (12%), and cystine (2%) [12]. The overall incidence of calcium-containing stones, that is, those containing calcium oxalate and calcium phosphate, is 70% to 80%. More specifically, urine contains inorganic and organic molecules that may inhibit or promote lithogenesis [13]. Hypocitraturia is a common physiologic disturbance in urolithiasis that affects from 19% to 63% of patients with stones. In stone patients with idiopathic hypocitraturia, the hypocitraturia occurs as either a sole disturbance or in association with other physiologic disturbances, which is termed complicated hypocitraturia.
We report the results of a 3.16±0.08-year clinical trial with potassium magnesium citrate and vitamin B-6 prophylaxis (Urikind-KM6, Gena Pharmaceutical Ltd., Kolkata, India) in patients with hypocitraturia- and hyperuricosuria-induced recurrent calcium oxalate and calcium phosphate urolithiasis.
MATERIALS AND METHODS
Between January 2005 and December 2010, a total of 247 patients (193 men [78.2%] and 54 women [21.8%] aged 26-68 years with a mean age of 37 years), who were either first-time, recurrent, or multiple stone formers constituted the subjects of this study. Our study was a prospective, randomized case-control study that was approved by an institutional ethics committee. We used Urikind-KM6 solution (potassium magnesium citrate and vitamin B-6), which is manufactured by Gena Pharmaceuticals Limited. Informed consent was obtained from patients before enrollment in the study.
Urinary estimation of promoters and inhibitors (calcium, magnesium, sodium, potassium, uric acid, citrate, oxalate, and phosphorus) of stone formation was done before and 24 hours after treatment. Urinary pH and volume were also estimated. Serum analysis was done for calcium, phosphorus, uric acid, albumin-globulin ratio, sodium, potassium, and bicarbonate.
Ambulatory 24-hour urinary analysis was done on 2 consecutive days. The first 24-hour urinary collection for analysis of urinary calcium and oxalate was done in a container with 10 mL of 6 mmol of hydrochloric acid to prevent precipitation of calcium and oxalate salts and also to prevent oxidation of ascorbic acid to oxalate. The collection on the second day for urinary pH, uric acid, citrate, magnesium, and creatinine was done in a container with 10 mL of 0.3 mmol of sodium azide to prevent bacterial growth. Urinary volume was calculated, and the urinary volume collected on the 2 consecutive days was averaged. There were no dietary restrictions and 24-hour urine samples were collected while the patients consumed their regular diets at home.
All stones or fragments that were retrieved after use of the available institutional modalities of treatment (e.g., extracorporeal shock wave lithotripsy, percutaneous cutaneous nephro lithotomy, ureterorenoscopy, incision surgery, or spontaneous passage of calculi) were analyzed chemically and crystallographically by using a polarizing microscope. A total of 247 patients were selected for the study. Among these, 61 patients (24.7%) who had moderate to severe hypocitraturia or hyperuricosuria or both and who were known multiple or recurrent stone formers discontinued prophylaxis because of drug intolerance within 1 month of therapy. These patients were given placebo and were followed at 6-month intervals and formed the untreated control group 1. Control group 2 constituted 53 patients (21.5%) who were first-time stone formers with mild hypocitraturia with or without hyperuricosuria who were not put on prophylactic therapy and were followed with conservative treatment with placebo at 6-month intervals for the same period of 3.16±0.08 years. Group 3 constituted 133 patients (54.8%) who were known multiple or recurrent stone formers who were treated (Urikind-KM6) with 1,100-mg potassium citrate, 375-mg magnesium citrate, and 20-mg pyridoxine hydrochloride/5 mL every 8 hours and were followed at 6-month intervals for 3.16±0.08 years.
Careful history was taken for evidence of new stone formation before and during treatment. Patients with Addison's disease, uncontrolled diabetes, or severe heart disease were excluded from the study. Patients on antispasmodics, angiotensin-converting enzyme inhibitors like lisinopril, angiotensin blockers like losartan, corticosteroids, and nasal decongestants (e.g., amphetamine, pseudoephedrine) were also excluded from the study. New stone formation represented spontaneous passage of stones in the absence of preexisting stones, stone passage occurring without a change in the number of stones, appearance of new stones on roentgenograms, or surgical removal or other therapies for newly formed stones. Metabolic evaluation was postponed in surgically active stone formers with renal colic, obstruction, or infection for at least 4 weeks after surgical therapy.
Among the 247 patients, 201 patients (81.4%) were in the idiopathic hypocitraturia group, and 46 patients (18.6%) were in the hypocitraturia and hyperuricosuria group. All patients were encouraged to increase their fluid intake (>3 L/d) to ensure an equal amount of output. Only patients with calcium oxalate, calcium phosphate, or mixed calcium oxalate and phosphate stones were included in this study.
A total of 133 patients (54.8%) received liquid potassium magnesium citrate and vitamin B-6 prophylaxis (Urikind-KM6) in a dosage of 1,100-mg potassium citrate, 375-mg magnesium citrate, and 20-mg pyridoxine hydrochloride/5 mL dose every 8 hours. Patients with diabetes received sorbitol base. The maximum period of follow-up was 38 months. Twenty-four-hour urinary estimation of promoters and inhibitors (calcium, magnesium, sodium, potassium, uric acid, citrate, oxalate, and phosphorus), urinary pH, and volume was also performed. Serum analysis was done for calcium, phosphorus, uric acid, albumin-globulin ratio, sodium, potassium, and bicarbonate during each visit at 6 months, 12 months, 18 months, 24 months, 36 months, and 38 months and the values were compared with baseline data.
The results are represented as least square mean±standard error. To test the mean difference between the three groups and to test the covariation between the three groups, analysis of variance test and analysis of covariance with post hoc tests was used for statistical analysis. All computations were performed by using SAS 9.2 (SAS Institute Inc., Cary, NC, USA) and IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA). A p-value of less than 0.05 was considered statistically significant.
RESULTS
The mean treatment period was 3.16±0.08 years. Pretreatment mean serum and 24-hour urinary parameters are recorded in Table 1. In all patients who received potassium magnesium citrate and vitamin B-6 prophylaxis therapy, there were significant and sustained rises in urinary pH and citrate and potassium levels (Table 2).
TABLE 1.
Pretreatment and control group values of serum and 24-hour urinary variables
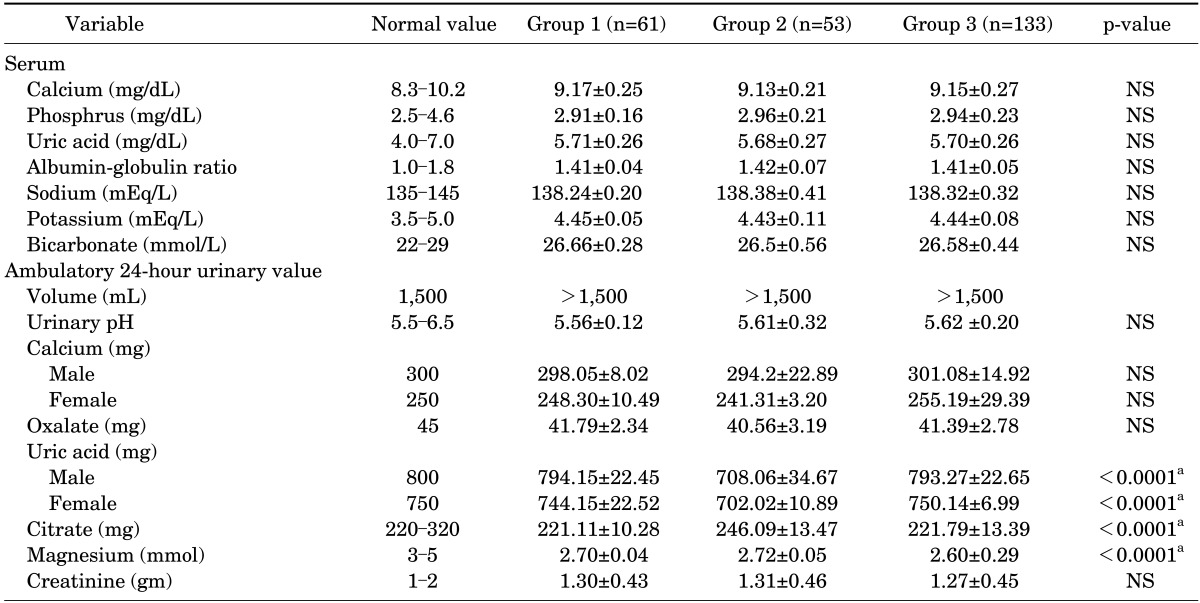
Values are presented as mean±standard deviation.
NS, not significant.
a:Significant.
TABLE 2.
Comparison of treatment values of serum and 24-hour urinary variables in three groups (result of ANCOVA)
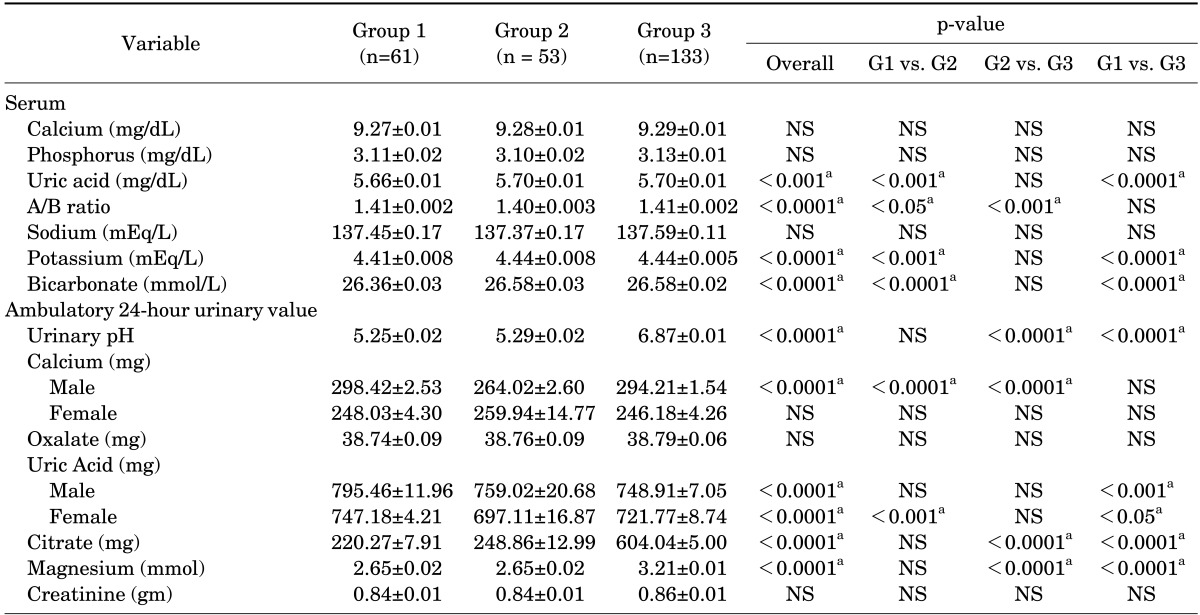
Values are presented as mean±standard error.
ANCOVA, analysis of covariance; NS, not significant.
a:Significant.
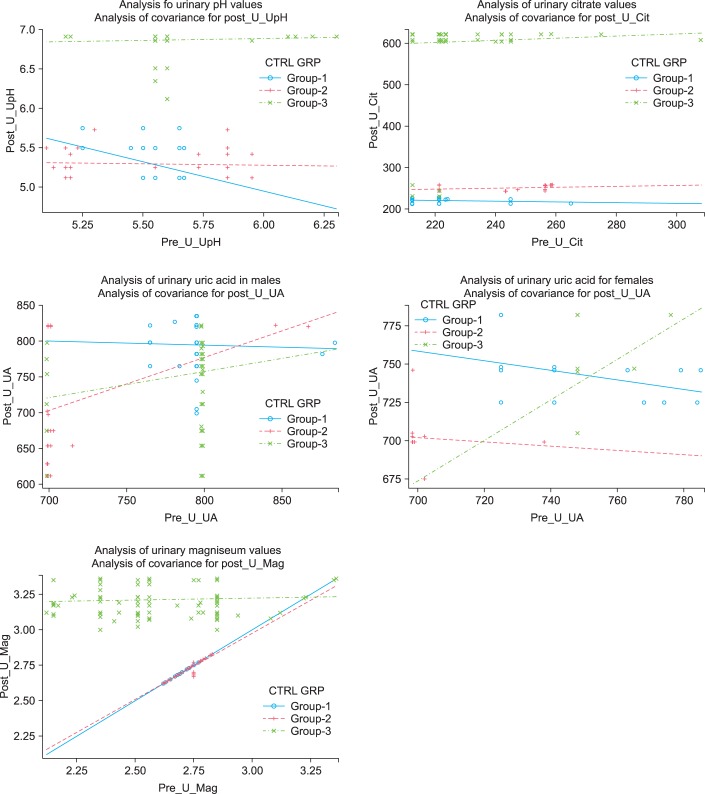
There was a sustained rise of pH from 5.62±0.2 to 6.87±0.01, which was at the high normal range and was a statistically significant change (p<0.0001) (Fig. 1). The urine citrate level increased from 221.79±13.39 to 604.04±5.00 mg, which was also a statistically significant change (p<0.0001) (Fig. 1). The urinary uric acid level decreased from 793.27±22.65 to 748.91±7.05 mg for males and from 750.14±6.99 to 721.77±8.74 mg for females, both of which were statistically significant (p<0.0001) (Fig. 1). Urinary magnesium increased from 2.60±0.29 to 3.21±0.01 mg, which was statistically significant (p<0.0001) (Fig. 1). There was a significant difference in the incidence of stone formation from 3.23±1.04 per patient per year in control group 1 to 0.35±0.48 per patient per year in group 3, which was statistically significant (p<0.0001) (Table 3).
FIG. 1.
Comparitive analysis of pre- and posttreatment urinary values.
TABLE 3.
Stone formation rate
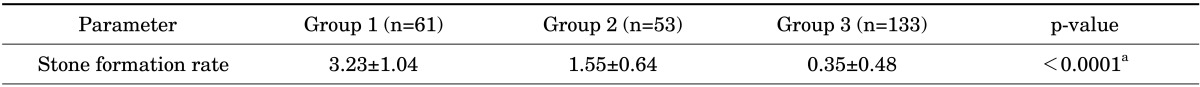
Values are presented as mean±standard deviation.
a:Significant.
Comparative analysis between the groups was done, and group 3 and control group 1 varied significantly in 24-hour urinary values like pH, citrate, uric acid in males, and magnesium; these results are shown in Table 2. Other urinary parameters were not altered and hence were not statistically significant. In the conservatively treated group (control group 1) of 61 patients (24.7%), there was no significant rise in pH or the citrate level and the stone formation rate remained the same as before (Table 3). In control group 2, 53 patients (21.5%) who were first-time stone formers and were not put on potassium magnesium citrate and vitamin B-6 prophylaxis therapy had a stone formation rate of 1.55±0.64 per patient per year with a mean follow-up of 3.16±0.08 years (Table 3).
DISCUSSION
Our findings suggest that hypocitraturia with or without hyperuricosuria was pathogenetically important in the formation of calcium nephrolithiasis in these patients. Hypocitraturia is most often idiopathic but can be secondary to acid-base disorders [13]. Systemic acidosis, distal renal tubular acidosis, hypocalciuria, and hypomagnesemia are common acid-base disturbances that can cause calcium oxalate urolithiasis. Furthermore, electrolyte disorders [14], drugs [15,16], changes in diet [17], and other disorders can be associated with low urine citrate [18,19]. Genetic polymorphisms of VDR and NaDc-1 genes have also been linked with hypocitraturia [13]. High urinary pH leads to increased saturation of phosphate predisposing to urolithiasis [20]. However, a low urinary pH predisposes to uric acid urolithiasis [21]. Pak [22] showed that adequate citrate excretion inhibits calcium oxalate stone formation, because it retards the crystallization of stone-forming calcium salts. Lee and Moon [23] demonstrated that correction of complicated hypocitraturia (coexistence with other metabolic abnormalities) with potassium citrate had no clinical significance against prevention of recurrent nephrolithiasis. Kok et al. [24] claimed that induced hypercitraturia with potassium magnesium citrate and vitamin B-6 prophylaxis enhances the inhibitor activity against calcium oxalate crystallization by providing an alkali load and reduces tubular reabsorption of citrate and increases citrate excretion [14]. There is clinical and biochemical evidence to prove the utility of potassium magnesium citrate and vitamin B-6 prophylaxis therapy in these patients. The therapy restores normal urinary citrate excretion and increases urinary pH to the range optimal for the control of calcium stone formation. Tiselius [25] claimed that urinary pH was kept below 7 to obviate hydroxyl apatite stone formation but greater than 6 to maximize inhibitor activity and the formation of anionic calcium complexes.
The close association between clinical and biochemical or physicochemical responses suggests that inhibition of stone formation was the result of potassium magnesium citrate therapy and vitamin B-6 prophylaxis therapy rather than conservative care (stone clinic effect) [26]. The rate of recurrence in first-time stone formers (control group 2) was almost equivalent to that in the patients selected for potassium magnesium citrate and vitamin B-6 prophylaxis therapy; hence, our policy of not prescribing to first-time stone formers is justified. Pak and Peterson [27] showed that potassium magnesium citrate and vitamin B-6 prophylaxis may be an alternative to allopurinol in the management of hypeuricosuric calcium oxalate nephrolithiasis. Ettinger et al. [28] in their study showed that potassium magnesium citrate and vitamin B-6 prophylaxis is superior to potassium citrate in raising urinary pH and that undissociated uric acid decreases; consequently, urinary saturation of calcium oxalate decreases, which was marginal with potassium citrate alone [29].
The major causes of discontinuation of therapy in the 61 patients (24.7%) in our series were nonpalatability, nausea, and vomiting. The minor side effects reported in the literature are diarrhea, nausea, and vomiting. Major side effects are due to overdose and include severe abdominal pain due to peptic ulceration; confusion; breathing difficulty; irregular heartbeat; nervousness; numbness or tingling in the hands, feet, or lips; weakness or heaviness of the legs due to hyperkalemia; and serious allergic reaction such as rash or itching or swelling of the face, tongue, and throat. In our study, potassium magnesium citrate and vitamin B-6 (Urikind-KM6) prophylaxis was relatively free of side effects except for occasional minor gastrointestinal complaints, which were addressed by adding sweet flavoring and by increasing the dilution of the compound in drinking water for each dose. These problems can be minimized by use of slow-release tablet or capsule preparations.
CONCLUSIONS
The favorable results of potassium magnesium citrate and vitamin B-6 prophylaxis therapy as reflected in the treated patient series reinforce our conclusion that this additional prophylactic measure rather than the stone clinic effect alone was largely responsible for the clinical efficacy observed. Clinical efficacy after spontaneous passage or compelled procedural clearance of symptomatic stones was better in the treated patients than in the controls who underwent similar procedures for their stones but in whom potassium magnesium citrate and vitamin B-6 prophylaxis was either discontinued or deliberately avoided.
Footnotes
The authors have nothing to disclose.
References
- 1.Ramello A, Vitale C, Marangella M. Epidemiology of nephrolithiasis. J Nephrol. 2000;13(Suppl 3):S45–S50. [PubMed] [Google Scholar]
- 2.Turney BW, Reynard JM, Noble JG, Keoghane SR. Trends in urological stone disease. BJU Int. 2012;109:1082–1087. doi: 10.1111/j.1464-410X.2011.10495.x. [DOI] [PubMed] [Google Scholar]
- 3.Ljunghall S, Danielson BG. A prospective study of renal stone recurrences. Br J Urol. 1984;56:122–124. doi: 10.1111/j.1464-410x.1984.tb05346.x. [DOI] [PubMed] [Google Scholar]
- 4.Shetty PS. Nutrition transition in India. Public Health Nutr. 2002;5(1A):175–182. doi: 10.1079/PHN2001291. [DOI] [PubMed] [Google Scholar]
- 5.Taylor EN, Curhan GC. Fructose consumption and the risk of kidney stones. Kidney Int. 2008;73:207–212. doi: 10.1038/sj.ki.5002588. [DOI] [PubMed] [Google Scholar]
- 6.Meschi T, Maggiore U, Fiaccadori E, Schianchi T, Bosi S, Adorni G, et al. The effect of fruits and vegetables on urinary stone risk factors. Kidney Int. 2004;66:2402–2410. doi: 10.1111/j.1523-1755.2004.66029.x. [DOI] [PubMed] [Google Scholar]
- 7.Taylor EN, Curhan GC. Oxalate intake and the risk for nephrolithiasis. J Am Soc Nephrol. 2007;18:2198–2204. doi: 10.1681/ASN.2007020219. [DOI] [PubMed] [Google Scholar]
- 8.Koyuncu HH, Yencilek F, Eryildirim B, Sarica K. Family history in stone disease: how important is it for the onset of the disease and the incidence of recurrence? Urol Res. 2010;38:105–109. doi: 10.1007/s00240-009-0249-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Curhan GC, Willett WC, Rimm EB, Stampfer MJ. Family history and risk of kidney stones. J Am Soc Nephrol. 1997;8:1568–1573. doi: 10.1681/ASN.V8101568. [DOI] [PubMed] [Google Scholar]
- 10.D'Angelo A, Calo L, Cantaro S, Giannini S. Calciotropic hormones and nephrolithiasis. Miner Electrolyte Metab. 1997;23:269–272. [PubMed] [Google Scholar]
- 11.Paliouras C, Trampikaki E, Alirasis P, Aperis G. Pathophysiology of nephrolithiasis. Nephrol Rev. 2012;4:e14. [Google Scholar]
- 12.Johri N, Cooper B, Robertson W, Choong S, Rickards D, Unwin R. An update and practical guide to renal stone management. Nephron Clin Pract. 2010;116:c159–c171. doi: 10.1159/000317196. [DOI] [PubMed] [Google Scholar]
- 13.Hamm LL, Hering-Smith KS. Pathophysiology of hypocitraturic nephrolithiasis. Endocrinol Metab Clin North Am. 2002;31:885–893. doi: 10.1016/s0889-8529(02)00031-2. [DOI] [PubMed] [Google Scholar]
- 14.Domrongkitchaiporn S, Stitchantrakul W, Kochakarn W. Causes of hypocitraturia in recurrent calcium stone formers: focusing on urinary potassium excretion. Am J Kidney Dis. 2006;48:546–554. doi: 10.1053/j.ajkd.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 15.Welch BJ, Graybeal D, Moe OW, Maalouf NM, Sakhaee K. Biochemical and stone-risk profiles with topiramate treatment. Am J Kidney Dis. 2006;48:555–563. doi: 10.1053/j.ajkd.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 16.Melnick JZ, Preisig PA, Haynes S, Pak CY, Sakhaee K, Alpern RJ. Converting enzyme inhibition causes hypocitraturia independent of acidosis or hypokalemia. Kidney Int. 1998;54:1670–1674. doi: 10.1046/j.1523-1755.1998.00150.x. [DOI] [PubMed] [Google Scholar]
- 17.Amanzadeh J, Gitomer WL, Zerwekh JE, Preisig PA, Moe OW, Pak CY, et al. Effect of high protein diet on stone-forming propensity and bone loss in rats. Kidney Int. 2003;64:2142–2149. doi: 10.1046/j.1523-1755.2003.00309.x. [DOI] [PubMed] [Google Scholar]
- 18.Marangella M, Vitale C, Manganaro M, Cosseddu D, Martini C, Petrarulo M, et al. Renal handling of citrate in chronic renal insufficiency. Nephron. 1991;57:439–443. doi: 10.1159/000186347. [DOI] [PubMed] [Google Scholar]
- 19.Weinstein DA, Somers MJ, Wolfsdorf JI. Decreased urinary citrate excretion in type 1a glycogen storage disease. J Pediatr. 2001;138:378–382. doi: 10.1067/mpd.2001.111322. [DOI] [PubMed] [Google Scholar]
- 20.Pak CY. Physicochemical basis for formation of renal stones of calcium phosphate origin: calculation of the degree of saturation of urine with respect to brushite. J Clin Invest. 1969;48:1914–1922. doi: 10.1172/JCI106158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pak CY, Sakhaee K, Peterson RD, Poindexter JR, Frawley WH. Biochemical profile of idiopathic uric acid nephrolithiasis. Kidney Int. 2001;60:757–761. doi: 10.1046/j.1523-1755.2001.060002757.x. [DOI] [PubMed] [Google Scholar]
- 22.Pak CY. Citrate and renal calculi: an update. Miner Electrolyte Metab. 1994;20:371–377. [PubMed] [Google Scholar]
- 23.Lee SY, Moon YT. Clinical significance of hypocitraturia in patients with nephrolithiasis. Korean J Urol. 2006;47:631–634. [Google Scholar]
- 24.Kok DJ, Papapoulos SE, Bijvoet OL. Excessive crystal agglomeration with low citrate excretion in recurrent stone-formers. Lancet. 1986;1:1056–1058. doi: 10.1016/s0140-6736(86)91329-2. [DOI] [PubMed] [Google Scholar]
- 25.Tiselius HG. The effect of pH on the urinary inhibition of calcium oxalate crystal growth. Br J Urol. 1981;53:470–474. doi: 10.1111/j.1464-410x.1981.tb03233.x. [DOI] [PubMed] [Google Scholar]
- 26.Hosking DH, Erickson SB, Van den Berg CJ, Wilson DM, Smith LH. The stone clinic effect in patients with idiopathic calcium urolithiasis. J Urol. 1983;130:1115–1118. doi: 10.1016/s0022-5347(17)51711-5. [DOI] [PubMed] [Google Scholar]
- 27.Pak CY, Peterson R. Successful treatment of hyperuricosuric calcium oxalate nephrolithiasis with potassium citrate. Arch Intern Med. 1986;146:863–867. [PubMed] [Google Scholar]
- 28.Ettinger B, Pak CY, Citron JT, Thomas C, Adams-Huet B, Vangessel A. Potassium-magnesium citrate is an effective prophylaxis against recurrent calcium oxalate nephrolithiasis. J Urol. 1997;158:2069–2073. doi: 10.1016/s0022-5347(01)68155-2. [DOI] [PubMed] [Google Scholar]
- 29.Jaipakdee S, Prasongwatana V, Premgamone A, Reungjui S, Tosukhowong P, Tungsanga K, et al. The effects of potassium and magnesium supplementations on urinary risk factors of renal stone patients. J Med Assoc Thai. 2004;87:255–263. [PubMed] [Google Scholar]