Abstract
Objective
To determine (a) how child age relates to parent concerns about child behavior and (b) how child age and parent concerns correlate with provider referrals and family attendance at mental health consultant (MHC) appointments.
Methods
Data were obtained from Rhode Island’s Project LAUNCH (Linking Actions for Unmet Needs in Children’s Health) in which universal developmental and behavioral screening and MHCs were embedded within primary care sites serving low-income, diverse families. Children 9 months to 8 years were eligible for the study if they had a scheduled screening well child visit in 2010 (N = 1,451). Families completing screening and/or those referred for a MHC appointment were included in analyses (n = 700). Outcome measures included parent reported concerns about child behavior, referral status following screening, and family attendance at the MHC appointment.
Results
For every 1-month increase in child age, there was a 1.02 times increase in the likelihood of parent behavioral concern and a 1.04 times increase in the likelihood of mental health referral, even when controlling for child behavior. MHC-referred children over 5 years were 2.61 times more likely to attend than children less than 5. When examining parent behavioral concerns and child age jointly, only concerns remained significant.
Conclusion
Infants and toddlers, who have the highest rates of unmet mental health needs, may be least likely to benefit from universal screening and on-site MHC support. Efforts to incorporate behaviorally-based screening tools and increase parent concerns where appropriate appear warranted, particularly for families with very young children.
Keywords: Mental health consultation, screening, integrated care, primary care, early childhood
Introduction
Research suggests that infants and toddlers exhibit mental health problems1 (e.g., behavior problems, inattention, difficulties interacting with peers, anxiety), that these problems can be accurately assessed, and that problems often persist.1,2 Yet, unmet mental health needs, (i.e., presence of elevated symptoms that are not being addressed in treatment), are high among this population.3 This may be due in part to lower levels of parent concern about mental health problems at this age,4,5 as parents of younger2 children may believe that problems are normative or transient.6 Moreover, these parents have fewer contexts, such as school, in which to evaluate impairment and receive input about their child’s functioning.2,7 With fewer points of referral and lower levels of parent concerns, the burden of identifying and addressing early childhood mental health problems falls heavily on primary care providers,8 who are expected to provide regular surveillance and screening of developmental and behavioral health problems, and provide referrals when needed.9,10 However, there are difficulties in identifying and addressing mental health problems in primary care, including screening implementation challenges (e.g., staff and time limitations),11,12 lack of confidence and time to interpret screens and handle mental health concerns,13–15 and limited referral options.16 Such challenges threaten the feasibility of implementing universal mental health screening and raise ethical issues about screening without the adequate ability to cope with identified concerns.17 Indeed, despite American Academy of Pediatrics (AAP) recommendations,10 many providers do not administer a standardized screening tool or provide a referral when concerns arise about possible delays.12
Models in which mental health consultants (MHCs) are embedded in pediatric practices provide an opportunity to surmount barriers and support screening by enabling provider-to-provider consultation, in-person introductions or “warm hand-offs,” and consultation with families to help triage concerns that are raised via screening. Randomized control trial research with adults has found that integrated care models have been associated with greater rates of treatment engagement when compared to enhanced community-based referrals (e.g., providing assistance with transportation).18 Within pediatric settings, such models have shown promise in increasing the identification and referral of children with mental health problems19–21 but research is limited and there is variability in findings. For example, in one study, adolescents who had been referred for mental health counseling were more likely to follow up with the referral if the mental health professional was located at the pediatric practice (66% received counseling) than if the professional was offsite (2.6% received counseling)20. However, in another study of children 4 years 11 months-to 19 years of age, much lower levels of follow-up with an on-site social worker were documented (17%).21 Thus, despite the potential of integrated care models and increased emphasis on the promotion of such models,8 research has been limited on the effectiveness of screening and embedding MHCs, particularly in serving the needs of very young children who are at increased risk of having unmet mental health needs. The goal of this study was to examine factors that influence young child mental health service access and receipt within a pediatric practice in which universal screening and integrated consultation were being implemented.
To address this broad aim, the extent to which child age was associated with three areas—parent concerns about child behavior, provider referrals, and parent usage of on-site mental health services—were addressed. Two elements of parent reports were examined: 1) Parent endorsement of behaviorally-based items on screening tools (e.g., extent to which child tantrums), referred to as child behavior scores; 2) Parent endorsement of worry or concern about their child’s behavior, referred to as parent concerns about child behavior. A focus on both areas is important because there are often discrepancies between parent concerns and parent reports of child behavior (e.g., parent endorses high frequency of symptoms on a behaviorally-based measure but does not report concerns about the behavior)4, as well as discrepancies in the predictive validity of concerns and reports of behavior1. Additionally, parent concerns are an important predictor of help-seeking (e.g., discussion with health professional, service receipt).5,21,22 It was hypothesized that child age would positively correlate with parent concerns about child behavior and with family attendance at the MHC appointment. It was also hypothesized that parent concern about child behavior would be associated with increased likelihood of referral to the MHC and with attendance at the MHC appointment.
Methods
Study Sites and Context
Data were obtained through Rhode Island’s Project LAUNCH (Linking Actions for Unmet Needs in Children’s Health), an initiative in which universal developmental and behavioral screening and MHCs were embedded within pediatric primary care sites in Providence, RI (2009–2013). Data for this study comes from one of the sites employing 3–4 providers affiliated with a community hospital serving high-risk, low-income, racially and ethnically diverse families. Screening was facilitated by partnerships between the RI Department of Health and AmeriCorps. Clinical psychologists, social workers, and master’s- or PhD-level trainees served as MHCs 1–2 days per week during which time they provided consultation to practice providers and administrators about screening implementation and other programmatic issues impacting child mental health. They also provided “on the fly” consultation (e.g., unscheduled clinical discussions with providers and/or families about mental health issues, warm hand-offs) and completed “triage assessments,” which served as a family’s first structured appointment with the MHC following referral from their primary care provider. The triage assessment (TA) is a brief (~60 minutes) standardized, yet flexible assessment in which MHCs gather more information about “red flags” identified via screening in order to contextualize concerns and offer more refined recommendations and referrals.23 Within this LAUNCH site, MHCs primarily served in the role of completing triage assessments.
Participants
Children were eligible for the study if they had a scheduled screening well child visit (WCV) in 2010, which occurred at 9 months, 18 months, 30 months, and annually from 3 to 8 years. Children whose parents completed screening during a screen-eligible visit and/or those referred for a TA were included in the overall study sample.
Procedures
Parents completed screening with help from the screening assistant, who approached the family to introduce screening, answered questions or completed screening with families when needed, and scored measures. The screening assistant attempted to provide the completed and scored packet to the pediatrician before or soon after s/he entered the room to see the patient, but there were often cases in which this was not possible because parents were still completing the forms or the screening assistant was busy assisting another family. Pediatricians could refer any family with children 8 years of age or younger for a TA with the MHC or to other services (e.g., Early Intervention), whether referred following a screen-eligible well child visit or whether referred when screening was not completed (e.g., referral done following a sick visit in which parent raised behavioral concerns). Children with elevated screening scores were not automatically referred for a TA, but rather pediatricians used available screening information, their knowledge of and discussion with the family, and their clinical judgment to determine the referral disposition, which they discussed with families during the visit when possible (though there were some cases when this was not possible due to time limitations or the fact that screening forms were not completed prior to the visit). MHCs reviewed screening summary sheets and referrals on a regular basis, occasionally clarifying pediatrician recommendations to ensure the appropriateness of referrals. Typically, clinic staff contacted referred families to schedule a TA appointment, which occurred within 1 month (rather than getting to meet the MHC at the time of initial referral as is typical in a warm hand-off model). Two hospital institutional review boards (IRB) and one university IRB approved the study. Informed consent was not obtained because data were gathered for program evaluation.
Measures
Data gathered during screening included sociodemographic information (child sex, race, and ethnicity; respondent; and respondent language), provider seen, and the screening measures.
Screening measures
Parents of children 5 years of age and younger completed the Ages and Stages Questionnaire, Third Edition (ASQ-3)24 and the Ages and Stages Questionnaire: Social-Emotional (ASQ: SE),25 validated, norm-referenced screening measures to assess development and social-emotional functioning respectively, with questionnaires that vary by child age. Parents of children 18 months to 5 years also completed the Early Childhood Screening Assessment (ECSA)26 to further assess social-emotional/behavioral functioning. The ECSA includes the 2 validated US Preventative Health Task Force parent depression questions and 2 questions about parent stress. Parents of children 5 to 8 years of age completed the Pediatric Evaluation of Developmental Status (PEDS),27 a brief questionnaire designed to elicit parental concerns about child learning, development, and behavior, and the Pediatric Symptom Checklist (PSC),28 a 35-item questionnaire designed to identify psychosocial problems that has established validity with the CBCL.28 Despite the fact that the study protocol indicated age cutoffs for completing the “young child screening packet” [ASQ(SE)/ECSA] and the “older child screening packet” (PEDS/PSC), there was variability in which set of forms parents of children 5 to 6 years (n = 69) actually completed. Most (65.2%) completed the young child screening packet, while 34.8% completed the older child screening packet. Variability in questionnaires completed in this age range was likely due to screening assistant error, which was exacerbated by the fact that both sets of screening packets are developmentally appropriate and valid for use in this age range. Given that screening information would be valid for children in this age range and given randomization of the error, (supported by a lack of significant differences in those who completed the younger versus older child measures), we retained all data regardless of which set of questionnaires families completed to increase the available sample size.
Main outcome measures
Child behavior score was dichotomized to indicate whether any of the behavioral screening tools (ASQ:SE, ECSA, PEDS, PSC) were above the clinical cutoff (versus scores deemed in the “normal” or “at risk” range), which varied based on child age and screening measure used. Child development score was dichotomized to indicate whether the ASQ-3 score fell above the clinical cutoff. Parent concerns were dichotomized to indicate whether the parent reported concerns on any of the close- or open-ended questions on the ASQ-3, ASQ:SE, and ECSA (e.g., “Do you have concerns about your child’s behavior?”), and were categorized as behavioral (e.g., internalizing, externalizing, or regulatory), developmental (e.g., language, motor), or “other” (e.g., medical). Due to time and budget constraints as well as this study’s focus on early childhood, parent concerns were only examined among children whose parents completed the young child screening packet. A master’s level clinician (LG) completed all coding with oversight from two PhD level supervisors (ASC and RS).
Referral disposition, gathered from screening forms, were categorized as “mental health” (e.g., referral to MHC for a TA or referral to an outside provider), “developmental” (e.g., early intervention), “other” (e.g., audiology), and “no referral”. It was also noted if the child was already receiving services and thus required no follow-up.
TA appointment schedules were used to determine families who had been referred following a non-screening visit (i.e., those who would not be tracked by referral disposition at the WCV) and to determine family attendance at the triage assessment (TA).
Data analysis
Univariate and bivariate analyses, including one-way Analysis of Variance (ANOVAs) for continuous variables and chi-square tests for categorical variables, were used to identify factors associated with the main outcome variables. Factors with significant associations were retained in multivariate logistic regression analyses. Statistical Package for the Social Sciences 18.0 was used for quantitative analyses.
Sample sizes for analyses varied depending on available data. Specifically, analyses that included parental concerns were only conducted with families who completed the young child screening packet (n = 371) for whom data on parent concerns about child behavior were coded. However, children of all ages (i.e., 9 months-8 years) were included in analyses that did not include parent concerns, including those examining the association between child age or sociodemographic factors on referral dispositions (n = 664) and family attendance at the TA (n = 136). This inclusive data analytic approach was taken to examine a broader age range where possible and to provide a comparison group for very young children. Descriptions of subsamples included in analyses are presented below.
Results
Sample description
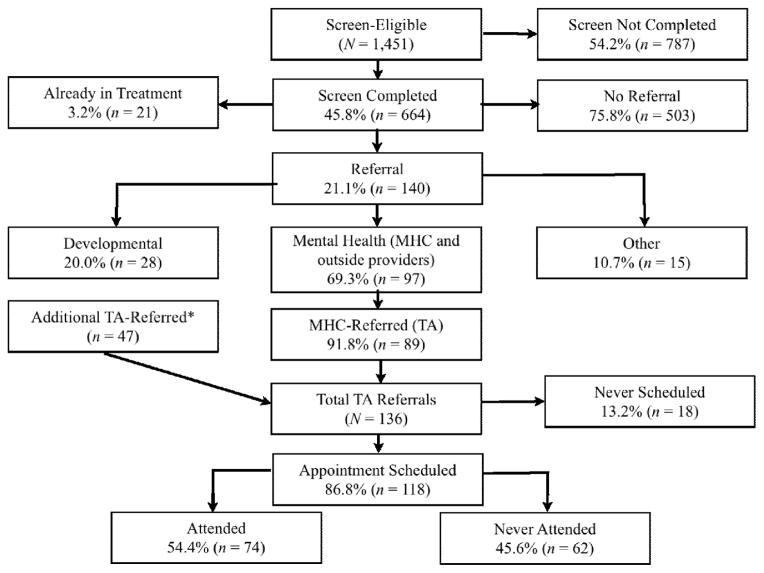
Table 1 provides a description of the sample. Figure 1 outlines the flow of families from initial eligibility (n = 1,451 children with a scheduled screening WCV in 2010) to attendance at the TA appointment (n = 74). Of the eligible sample, 25.2% (n = 366) never attended their WCV and 30.1% (n = 437) did not complete screening due to factors such as staffing problems (i.e., screening assistant not present to facilitate screening) and lack of time. Overall, 664 parents completed screening during a screen-eligible visit (63% of those who attended), of whom 371 (55.9%) completed the young child screening packet. Families completing screening had children who were significantly older (M = 58.68, SD = 29.69) than families who did not complete screening (M = 54.91, SD = 29.02; t [1449] = −2.07, p = .039), though a Chi-square test revealed no significant difference in screening completion rates across children completing the young child packet (58.5%) and those completing the older child packet (61.4%; p > .05).
Table 1.
Sample Descriptives
| Total Screen Eligible Sample (N = 1451) | Screening Complete (n = 664) | Referred for Triage Assessment (N = 136)
|
||
|---|---|---|---|---|
| Attended Appointment (n = 74) | Did Not Attend Appointment (n = 62) | |||
| Child age (years) | M = 4.81 (SD = 2.47) | M = 4.88 (SD = 2.47) | M = 5.05 (SD = 2.02) | M = 4.22 (SD = 1.99) |
| Male | 49.3% (716) | 50.0% (332) | 58.1% (43) | 54.8% (34) |
| Race and ethnicity | ||||
| Non-Hispanic | 28.4% (259) | 34.1% (184) | 22.6% (14) | 37.5% (15) |
| White | 3.2% (29) | 3.9% (21) | 4.8% (3) | 4.8% (2) |
| Black | 12.0% (109) | 13.5% (73) | 5.1% (5) | 16.7% (7) |
| Asian/Pacific Islander | 6.1% (56) | 8.2% (44) | 4.8% (3) | 7.1% (3) |
| Other | 4.1 (37) | 5.2% (28) | 0.0% | 4.8% (2) |
| Multiracial | 3.1% (28) | 3.3% (18) | 4.8% (3) | 2.4% (1) |
| Hispanic | 71.3% (650) | 65.9% (355) | 77.4% (48) | 62.5% (25) |
| No other race info | 39.5% (360) | 28.9% (156) | 3.2% (2) | 28.6% (12) |
| White | 8.4% (77) | 10.4% (56) | 3.2% (2) | 7.1% (3) |
| Black | 0.8% (7) | 0.7% (4) | 1.6% (1) | 2.4% (1) |
| Asian/Pacific Islander | 0.8% (7) | 1.1% (6) | 0% | 2.4% (1) |
| Other | 18.4% (168) | 21.4% (115) | 38.7% (24) | 14.3% (6) |
| Multiracial | 3.4% (31) | 3.3% (18) | 6.5% (4) | 2.4% (1) |
| Respondent was mother | 85.2% (334) | 85.6% (297) | ||
| Language | ||||
| English | 67.2% (981) | 65.4% (434) | 67.6% (50) | 79.0% (49) |
| Spanish | 30.5% (442) | 33.7% (224) | 32.4% (24) | 21.0% (13) |
| Other | 1.9% (28) | 0.9% (6) | 0.0% (0) | 0.0% (0) |
Figure 1.
Flow of families from eligibility to attendance at first mental health consultant (MHC) appointment (Triage Assessment; TA).
How does child age influence parent concerns about child behavior?
Table 2 provides screening profile information for the families who completed screening (n = 664), though as noted above, analyses of parent concerns about child behavior were only conducted among parents completing the young child screening (n = 371). Of these 371 parents, most (71.7%) reported no concerns, while 28.3% reported some type of concern, including non-behavioral (e.g., language, health) concerns only (7.2%), behavioral concerns only (13.7%), and both behavioral and non-behavioral concerns (7.3%). Parents of children with elevated behavior scores were more likely to report behavioral concerns (51.5% reported concerns) than parents of children without elevated behavior scores (15.7% reported concerns), χ2 (1, n = 371) = 75.05, p < .001, phi = .46. There was no association between parent behavioral concerns and child race and ethnicity, respondent, parent language, and child sex (p’s > .05). Parents with behavioral concerns had children who were older (M = 3.54 years, SD = 1.39 years) than parents without behavioral concerns (M = 2.88 years, SD = 1.58 years), t (135) = −3.60, p < .001. Moreover, the relationship between clinically elevated screening status and parent-reported concerns was weaker among younger children than among older children. While 59.7% of parents of children 3–6 years who reported elevated behavior problems also reported concerns, only 35.3% of parents of children under 3 years with elevated behavioral problems also reported behavioral concerns. Child age was not associated with concern in non-behavioral domains (p > .05). A binary logistic regression revealed that, child age and behavior scores significantly and independently predicted parent behavioral concerns, χ2 (2, n = 371) = 79.25, p < .001. For every 1-month increase in age, there was a 1.02 increase in the likelihood of parent behavioral concern (p = .004), even when controlling for child behavior scores.
Table 2.
Screening profile information for children with complete screening (n = 664)
| Score | Clinically Elevated? | |
|---|---|---|
| M (SD) | % (n) | |
| Children with completed young child screening packet (n = 371)1 | ||
| Development (ASQ-3) | ||
| Communication | 50.5 (11.7) | 3.8% (14) |
| Gross Motor | 53.9 (9.6) | 3.8% (14) |
| Fine Motor | 45.6 (13.7) | 8.6% (32) |
| Problem Solving | 47.7 (13.2) | 10.8% (40) |
| Personal-Social | 51.4 (10.0) | 4.9% (18) |
| Any Developmental Domain | --- | 19.7% (73) |
| Social-Emotional | ||
| ASQ: SE | 39.6 (28.5) | 20.5% (76) |
| ECSA: Child Score | 12.8 (9.6) | 16.2% (60) |
| Any Social-Emotional Domain | --- | 27.2% (101) |
| Parent Distress (ECSA Parent Score) | 0.5 (1.1) | 13.5% (50) |
| Developmental or Social-Emotional | --- | 37.7% (140) |
| Children with completed older child screening packet (n = 293)2 | ||
| PEDS | 0.78 (1.2) | 20.5% (60) |
| PSC | 10.26 (9.1) | 5.5% (16) |
| PEDS or PSC | --- | 21.5% (63) |
ASQ-3 and ASQ:SE mean scores vary by child age. Each ASQ-3 domain score is scored on a scale of 0 to 60. Possible ASQ: SE score ranges are from 0 to over 300 depending on the questionnaire form since number of questions varies across forms. On the ASQ-3, lower scores indicate increased clinical risk, while on the ASQ: SE, higher scores indicate increased clinical risk. Scores on the ECSA child portion can range from 0 to 72 with scores of 18 or higher indicating clinical significance. Scores on the ECSA parent portion can range from 0 to 8 with scores of 1 or higher indicating clinical risk.
Parents can indicate concerns in 10 areas on the PEDS with higher scores indicating increased clinical risk. Scoring guidelines vary by child age, but > 2 predictive concerns indicates clinically elevated concerns. Scores on the PSC can range from 0 to 70 with higher scores indicating increased clinical risk. Scores of 28 and above indicate clinical significance.
How does child age and parent concern about child behavior influence provider referral decisions following screening?
Of children with completed screening (n = 664), 140 (21%) received some type of referral or were noted by providers to require some type of follow-up. Child age was significantly associated with referral disposition (Table 3); χ2 (1, n = 664) = 29.86, p < .001, phi = .21. Specifically, child age was positively associated with already being connected with services and with mental health referral. Age was negatively associated with developmental referral and with “other” referrals. Further analysis of children whose parents completed the young child screening packet (n = 371) revealed that child age remained significantly predictive of mental health referral, even when controlling for clinically-elevated child behavioral problems, behavioral concerns, and clinically-elevated parent distress scores, χ2 (4, n = 371) = 139.43, p < .001. For every 1-month increase in child age, there was a 1.04 times increase in the likelihood of mental health referral (95% CI = 1.01–1.06, p < .001).
Table 3.
Referral disposition for children across different age ranges with complete screening (n = 664).
| Children < 3 (n = 158) % (n) |
Children 3–5 (n = 237) % (n) |
Children 6–8 (n = 269) % (n) |
χ2 (phi) | |
|---|---|---|---|---|
| Any clinically elevated screening | 34.8% (55/158) | 38.8% (92/237) | 20.8% (56/269) | 20.99*** |
| Already connected with services | 0.6% (1/158)a | 1.7% (4/237)a | 5.9% (16/269)b | 11.80 (.13)** |
| No referral | 79.1% (125/158)a | 68.4% (162/237)b | 80.3% (216/269)a | 11.06 (.13)** |
| Referral/recommendation | 20.3% (32/158)a | 30.0% (71/237)b | 13.8% (37/269)a | 19.97 (.17)*** |
| Mental health (TA and outside) | 8.2% (13/158)a | 19.8% (47/237)b | 13.8% (37/269)ab | 10.42 (.13)** |
| Developmental | 9.5% (15/158)a | 5.5% (13/237)a | 0% (0/269)b | 23.68 (.19)*** |
| Other | 2.5% (4/158)a | 4.6% (11/237)a | 0% (0/269)b | 12.36 (.14)** |
p < .05,
p < .01,
p < .001,
Different letters are used to denote differences significant at the p < .05
How does child age and parent concern about child behavior influence parent usage of on-site mental health services?
One hundred and thirty-six eligible children were referred for a TA appointment either following screening (n = 89) or at another point during the study (n = 47). Overall, 54.4% of referred children attended the TA appointment. There was no association between appointment attendance and child race and ethnicity, parent language, and child sex (p’s > .05). Child age was the only sociodemographic variable that predicted appointment attendance. Children attending the appointment (M = 5.05 years, SD = 23.9 months) were significantly older than children who never attended (M = 4.22 years, SD = 24.3 months), t [134] = −2.38, p = .019. Referred children over 5 years (of whom 67.2% attended) were 2.61 times more likely to ever be seen for a TA than children less than 5 years (of whom 44.0% attended) (χ2 (1, n = 136) = 7.40; 95% CI: 1.29 –5.27; p = .007).
For children whose parents had completed screening prior to TA referral (n = 89), there were no significant differences in clinical cutpoint status on any of the screening measures across children who attended the appointment and those who did not (p’s > .05). For MHC-referred children whose parents completed the young child screening packet (n = 63), parents who expressed behavioral concerns were more likely to attend the TA (58.3% attended) than parents without any behavioral concerns (25.9% attended); χ2 (1, n = 63) = 5.32, p = .021. Results of a binary logistic regression with child age and parent behavioral concerns was significant: χ2 (2, n = 63) = 6.93, p = .031, although only parent behavioral concerns remained significant after controlling for child age: β = 3.70, CI: 1.19 – 11.57, p = .024.
Discussion
Universal developmental and behavioral health screening in pediatric primary care linked with on-site MHC support has potential in identifying and addressing the unmet needs of young children. These efforts are consistent with the AAP’s Bright Futures initiative,29 which encourages the use of structured developmental assessment and improvements in linkages from primary care to community resources to address children’s special health care needs. In the present study, an integrated care model that provided professional support to assist with universal screening and referrals was explored. Success of the overall model was examined, with an emphasis on the role of child age given the importance of early intervention and given that younger children are more likely to have unmet mental health needs.3 Findings suggest that, despite the promise of the integrated care model in increasing the identification of early childhood mental health problems, younger children were the least likely to benefit.
Importantly, only 63% of screen-eligible families who attended their well child visit appointment completed screening during that visit. While this number is comparable to rates of screening completion found in other pediatric primary care studies or universal screening,12,21,30–32 it is notable given the fact that a screening assistant and on-site MHC were available to facilitate screening. It should also be noted that the screening packet completed in this study, which contained 2–3 different questionnaires, was lengthier than that completed in other studies. This finding warrants attention in future research, which should examine the economic costs and benefits of screening and focus on ways to increase screening completion rates (e.g., streamlining processes, shortening initial screening tools used).
Among parents who completed screening, those reporting elevated behavioral scores also reported more concerns about their child’s behavior. One mother described how the severity of the child’s behavior impacted her concerns about the behavior noting, “He’s hitting my daughter…. he’s hitting my friend’s daughter and I was just really concerned because I thought he was going to hurt somebody.” However, parents of younger children were less likely to be concerned about behavior even when screening suggested that concerns were warranted. Nearly two-thirds (64.7%) of parents of children under 3 years with elevated behavioral problems based on screening cutpoints did not report behavioral concerns, whereas 40.3% of parents of children 3–5 years with behavior problems did not report concerns. This finding could relate to the parent’s beliefs and expectations and/or to the screening instruments (if they were not sufficiently sensitive or specific in identifying symptoms in children under 3). Parents of younger children may be less concerned about their children’s behaviors because they do not realize that young children can experience significant mental health problems (e.g., “They’re too small for that!”) and/or because they think that the problems are transient and normative and therefore not of significant concern (e.g., “She’s just young. She’ll grow out of it. It’s normal”).
These findings, which are consistent with previous research,1,4 highlight the limitations of relying on parent concerns as a proxy for child behavior problems, particularly for young children. Findings also underscore the importance of using behaviorally-based measures that have a lower inference level required to make ratings as such measures can yield more reliable results, are less influenced by parent biases, and can help to predict later behavior.1 Indeed, studies have demonstrated that, while parent concern about child behavior can be a useful predictor of clinically significant social-emotional problems (as it was in the present study), it is not adequately sensitive to detect such problems nor to detect children in the at-risk range.4,33 Moreover, whereas behaviorally-based mental health screening scores at 12–36 months have been found to predict parent- and teacher-rated problems and diagnostic status in early elementary school, early parent concern about child behavior was only predictive of later parent-reported behavior problems.1 Despite the limitations of sole reliance on parental concerns, asking about concerns can be done relatively quickly (though following up on their response may take longer) and may be useful clinically as it provides information about parent perceptions of child behavior and motivation to seek help. Additionally, some parents in the present study said that questions about their concerns reminded them of issues they wanted to discuss and helped them “verbalize” their concerns.
In addition to the increase in the likelihood of parent behavioral concern over time (OR = 1.02 for every 1-month increase in age), there was also an increase in the likelihood of mental health referral over time (OR = 1.04 for every 1-month increase in age). Thus, although parents of younger children report less concerns about child behavior, providers may also view younger children’s behavior problems as less concerning and therefore feel less compelled to provide referrals. Additionally, the increased frequency of well child visits in early childhood may mean that providers feel more comfortable taking a “wait-and-see” approach. As one provider noted, “A lot of times (parents) will say, ‘well my other kid was like this—he’ll grow out of it,’ and if it’s a young child you know you’ll be seeing them before too long.” While in some cases, this approach is warranted, in other cases it may postpone the child’s receipt of needed services. Other factors impacting provider’s referral decisions may include lack of comfort, knowledge, and training identifying and addressing mental health concerns13 as well as limited referral sources. However, given that one of the main objectives of LAUNCH was to increase provider knowledge and comfort by making MHCs available for case consultation and to reduce supply issues by embedding early childhood mental health specialists within the clinic (which decreased wait times and provided free services to families), such issues would have presented less of a barrier in this study. These issues, though problematic for children of all ages, may be particularly pronounced for younger children, thereby contributing to provider’s reluctance to address elevated screening scores in this age group. Efforts to enhance early childhood mental health provider training and to expand early childhood service delivery systems could help to increase provider’s ability to identify and address early childhood mental health problems.
Overall, 54.4% of families referred to the MHC attended their TA appointment, which is similar to findings from other studies of child attendance at initial outpatient mental health appointments.34–37 The finding falls within the wide range of attendance rates for mental health providers co-located within health centers20, which range from 17%21 to 95%20,38. The initial appointment attendance rate may not have been significantly higher than outpatient mental health attendance rates because the MHC did not typically get the chance to meet the family during the well child visit as is ideally the case in integrated care models (the “warm hand-off”). Additionally, the clinic in the present investigation serves a high rate of low-income families who can face significant barriers to visit attendance. Parents who were less concerned and whose children were younger were less likely to attend the TA appointment to which they were referred. When examining both child age and parent behavioral concerns simultaneously, only parent behavioral concerns remained significant, although the low sample size for this analysis warrants caution in interpreting the findings.
Findings regarding the increase in parent concerns, provider referrals, and parent attendance over time suggest that as children get older they are increasingly likely to be identified as having mental health problems, which is consistent with prior research.3 Findings also indicate that child age may serve as a useful proxy for parent concerns, but that ultimately parent concerns may drive parent attendance at mental health referrals. Findings and prior research point towards several possible methods for increasing parent attendance at MHC visits. Providers can explore parent beliefs about child behavior, including their level of concern about the behavior and their beliefs about their child’s susceptibility to mental health problems. For example, it would be beneficial to help parents understand when elevated behavior scores may be of concern given that concerns predicted attendance. Consistent with motivational interviewing principles, providers could present developmental norms, highlight the impact of the child’s behaviors on development and family functioning, and they could encourage parents to consider how their child’s behavior problems will unfold over time. Providers could also discuss the nature and benefits of intervention. Though these efforts may increase attendance for families with children of varying ages, such efforts may be most fruitful for families with younger children who tend to be less concerned about their child’s behavior. Prior research suggests that broader engagement efforts should focus on helping families understand the reason for the referral12 and providing appointment reminders.39 Lastly, prior research suggests that parent fears of being blamed for child problems and fears that one’s children would be taken away may hamper successful referrals.40 Thus, it may be beneficial to engage in open, non-judgmental conversation about the MHC’s role and parent fears about the referral. Such discussion may help to ensure that providers can address parent concerns or determine an alternative course of action (e.g., scheduling a follow-up pediatric visit), rather than having parents accept the referral and then not attend the MHC appointment.
Limitations
Findings should be interpreted in light of the study’s limitations. Examining a wider range of variables that could have impacted outcomes, such as parents’ health literacy, the length and quality of the parent-provider relationship, parent expectancies for treatment, and other family psychosocial stressors, would be beneficial. It would also have been informative to code and examine parent concerns among older children, and to gather more information about TA referrals that stemmed from non-CWS eligible visits, which was outside of the scope of the present investigation. Additionally, observational measures of the visit and the child’s behavior should be gathered in future studies, as this would enable improved accuracy of data, reduce method bias stemming from having a sole reporter, and facilitate better understanding of parent-provider discussion and the referral process. While there has been some promising randomized control trial research on integrated care models with adults,18 such research is lacking among pediatric populations, particularly that incorporates the use of universal screening. Lastly, in an age in which health care costs are being closely scrutinized, longitudinal research that includes cost analyses would be useful.
Conclusion
In the present investigation, a comprehensive approach was undertaken to examine universal developmental and behavioral health screening and integrated mental health consultation, an increasingly common and recommended model within pediatric primary care. Findings suggest that, while this model may improve identification of children in need of services, young children are at increased risk of falling through service delivery gaps. Thus, efforts to implement screening and integrated care models should be mindful of young children who are most at risk of having unmet mental health needs.
Acknowledgments
This study was funded by a SAMSHA grant awarded to Drs. Dickstein and Seifer (1H79SM058854-01). Work on this study was completed as part of Dr. Godoy’s dissertation at the University of Massachusetts Boston with support from a National Institute of Child Health and Human Development grant (F31 HD063344-03).
Footnotes
The term “mental health” is used throughout the article to encompass social-emotional and behavioral domains and may be used interchangeably with these terms.
“Young” children are considered, for the purpose of this paper, to include preschool-aged children (i.e., those less than 6 years old), although within this age group our focus is largely on infants and toddlers less than 3 years of age.
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Contributor Information
Leandra Godoy, Children’s National Medical Center, Washington, DC.
Alice S. Carter, University of Massachusetts Boston, Boston, MA.
Rebecca B. Silver, Warren Alpert Medical School of Brown University, Providence, RI.
Susan Dickstein, Warren Alpert Medical School of Brown University, Providence, RI.
Ronald Seifer, Warren Alpert Medical School of Brown University, Providence, RI.
References
- 1.Briggs-Gowan MJ, Carter AS. Social-emotional screening status in early childhood predicts elementary school outcomes. Pediatrics. 2008 May;121(5):957–962. doi: 10.1542/peds.2007-1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carter AS, Godoy L, Marakovitz SE, Briggs-Gowan MJ. Parent reports and infant-toddler mental health assessment. In: Zeanah CH, editor. Handbook of infant mental health. 3. New York, NY: Guilford Press; 2009. pp. 233–251. [Google Scholar]
- 3.Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: variation by ethnicity and insurance status. Am J Psychiatry. 2002 Sep;159(9):1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- 4.Glascoe FP. Parents’ evaluation of developmental status: how well do parents’ concerns identify children with behavioral and emotional problems? Clin Pediatr (Phila) 2003 Mar;42(2):133–138. doi: 10.1177/000992280304200206. [DOI] [PubMed] [Google Scholar]
- 5.Ellingson KD, Briggs-Gowan MJ, Carter AS, Horwitz SM. Parent identification of early emerging child behavior problems: predictors of sharing parental concern with health providers. Arch Pediatr Adolesc Med. 2004 Aug;158(8):766–772. doi: 10.1001/archpedi.158.8.766. [DOI] [PubMed] [Google Scholar]
- 6.Pavuluri MN, Luk SL, McGee R. Help-seeking for behavior problems by parents of preschool children: a community study. J Am Acad Child Adolesc Psychiatry. 1996 Feb;35(2):215–222. doi: 10.1097/00004583-199602000-00015. [DOI] [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Bureau. The National Survey of Children With Special Health Care Needs Chartbook 2005–2006. Rockville, MD: US Department of Health and Human Services; 2007. [Google Scholar]
- 8.Foy JM. Enhancing pediatric mental health care: report from the American Academy of Pediatrics Task Force on Mental Health. Introduction. Pediatrics. 2010 Jun;125( Suppl 3):S69–74. doi: 10.1542/peds.2010-0788C. [DOI] [PubMed] [Google Scholar]
- 9.American Academy of Pediatrics Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health. Policy statement--The future of pediatrics: mental health competencies for pediatric primary care. Pediatrics. 2009 Jul;124(1):410–421. doi: 10.1542/peds.2009-1061. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Pediatrics Council on Children With Disabilities, Section on Developmental Behavioral Pediatrics, Bright Futures Steering Committee, Medical Home Initiatives for Children With Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006 Jul;118(1):405–420. doi: 10.1542/peds.2006-1231. [DOI] [PubMed] [Google Scholar]
- 11.Sand N, Silverstein M, Glascoe FP, Gupta VB, Tonniges TP, O’Connor KG. Pediatricians’ reported practices regarding developmental screening: do guidelines work? Do they help? Pediatrics. 2005 Jul;116(1):174–179. doi: 10.1542/peds.2004-1809. [DOI] [PubMed] [Google Scholar]
- 12.King TM, Tandon SD, Macias MM, et al. Implementing developmental screening and referrals: lessons learned from a national project. Pediatrics. 2010 Feb;125(2):350–360. doi: 10.1542/peds.2009-0388. [DOI] [PubMed] [Google Scholar]
- 13.Horwitz SM, Kelleher KJ, Stein RE, et al. Barriers to the identification and management of psychosocial issues in children and maternal depression. Pediatrics. 2007 Jan;119(1):e208–218. doi: 10.1542/peds.2005-1997. [DOI] [PubMed] [Google Scholar]
- 14.Wissow LS, Larson S, Anderson J, Hadjiisky E. Pediatric residents’ responses that discourage discussion of psychosocial problems in primary care. Pediatrics. 2005 Jun;115(6):1569–1578. doi: 10.1542/peds.2004-1535. [DOI] [PubMed] [Google Scholar]
- 15.Williams J, Klinepeter K, Palmes G, Pulley A, Foy JM. Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics. 2004 Sep;114(3):601–606. doi: 10.1542/peds.2004-0090. [DOI] [PubMed] [Google Scholar]
- 16.Meyers JC, Perry DF, Kaufmann RK, Knitzer J, editors. Social & emotional health in early childhood: Building bridges between services & systems. Baltimore, MD: Brookes Publishing; 2007. Developing the work force for an infant and early childhood mental health system of care. [Google Scholar]
- 17.Perrin E, Stancin T. A continuing dilemma: whether and how to screen for concerns about children’s behavior. Pediatr Rev. 2002 Aug;23(8):264–276. doi: 10.1542/pir.23-8-264. [DOI] [PubMed] [Google Scholar]
- 18.Bartels SJ, Coakley EH, Zubritsky C, et al. Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. Am J Psychiatry. 2004 Aug;161(8):1455–1462. doi: 10.1176/appi.ajp.161.8.1455. [DOI] [PubMed] [Google Scholar]
- 19.Briggs RD, Racine AD, Chinitz S. Preventive pediatric mental health care: A co-location model. Infant Ment Health J. 2007;28(5):481–494. doi: 10.1002/imhj.20149. [DOI] [PubMed] [Google Scholar]
- 20.Lieberman A, Adalist-Estrin A, Erinle O, Sloan N. On-site mental health care: a route to improving access to mental health services in an inner-city, adolescent medicine clinic. Child Care Health Dev. 2006 Jul;32(4):407–413. doi: 10.1111/j.1365-2214.2006.00620.x. [DOI] [PubMed] [Google Scholar]
- 21.Hacker KA, Myagmarjav E, Harris V, Suglia SF, Weidner D, Link D. Mental health screening in pediatric practice: factors related to positive screens and the contribution of parental/personal concern. Pediatrics. 2006 Nov;118(5):1896–1906. doi: 10.1542/peds.2006-0026. [DOI] [PubMed] [Google Scholar]
- 22.Godoy L, Mian ND, Eisenhower AS, Carter AS. Pathways to service receipt: Modeling parent help-seeking for childhood mental health problems. Administration and Policy in Mental Health and Mental Health Services Research. doi: 10.1007/s10488-013-0484-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silver RB, Beers MM, Godoy L, Dickstein SD. Addressing Barriers and Limitations of Developmental Screening in Community Contexts: Moving Beyond the Red Flag. In: Carter AS, DelCarmen-Wiggins R, editors. Handbook of Infant, Toddler, and Preschool Mental Health Assessment. 2. New York, NY: Oxford University Press; in press. [Google Scholar]
- 24.Squires J, Bricker D. Ages and Stages Questionnaires: A parent completed monitoring system. 3. Baltimore, MD: Paul H. Brookes Publishing Co; 2009. [Google Scholar]
- 25.Squires J, Bricker D, Twombly E. Ages and Stages Questionnaire: Social-Emotional: A parent-completed, child-monitoring system for social-emotional behaviors. Baltimore, MD: Paul H. Brookes Publishing Co; 2002. [Google Scholar]
- 26.Gleason MM, Zeanah CH, Dickstein S. Recognizing young children in need of mental health assessment: Development and preliminary validity of the early childhood screening assessment. Infant Ment Health J. 2010;31(3):335–357. doi: 10.1002/imhj.20259. [DOI] [PubMed] [Google Scholar]
- 27.Glascoe FP. Parents’ Evaluation of Developmental Status. Nashville, TN: Ellsworth & Vandermeer Press, Ltd; 1997. [Google Scholar]
- 28.Jellinek MS, Murphy JM, Little M, Pagano ME, Comer DM, Kelleher KJ. Use of the Pediatric Symptom Checklist to screen for psychosocial problems in pediatric primary care: a national feasibility study. Arch Pediatr Adolesc Med. 1999 Mar;153(3):254–260. doi: 10.1001/archpedi.153.3.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hagan JF, Shaw JS, Duncan PM, editors. Bright futures: Guidelines for health supervision of infants, children, and adolescents. 3. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 30.Hacker KA, Arsenault LN, Williams S, Digirolamo AM. Mental and behavioral health screening at preventive visits: opportunities for follow-up of patients who are nonadherent with the next preventive visit. J Pediatr. 2011 Apr;158(4):666–671. e662. doi: 10.1016/j.jpeds.2010.09.059. [DOI] [PubMed] [Google Scholar]
- 31.McMenamy J, Sheldrick RC, Perrin EC. Early intervention in pediatrics offices for emerging disruptive behavior in toddlers. J Pediatr Health Care. 2011 Mar-Apr;25(2):77–86. doi: 10.1016/j.pedhc.2009.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schonwald A, Huntington N, Chan E, Risko W, Bridgemohan C. Routine developmental screening implemented in urban primary care settings: more evidence of feasibility and effectiveness. Pediatrics. 2009 Feb;123(2):660–668. doi: 10.1542/peds.2007-2798. [DOI] [PubMed] [Google Scholar]
- 33.Weitzman CC, Edmonds D, Davagnino J, Briggs-Gowan M. The association between parent worry and young children’s social-emotional functioning. J Dev Behav Pediatr. 2011 Nov;32(9):660–667. doi: 10.1097/DBP.0b013e31822bc76b. [DOI] [PubMed] [Google Scholar]
- 34.McKay MM, Bannon WM., Jr Engaging families in child mental health services. Child Adolesc Psychiatr Clin N Am. 2004 Oct;13(4):905–921. vii. doi: 10.1016/j.chc.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Harrison ME, McKay MM, Bannon WM., Jr Inner-city child mental health service use: the real question is why youth and families do not use services. Community Ment Health J. 2004 Apr;40(2):119–131. doi: 10.1023/b:comh.0000022732.80714.8b. [DOI] [PubMed] [Google Scholar]
- 36.McKay MM, McCadam K, Gonzales JJ. Addressing the barriers to mental health services for inner city children and their caretakers. Community Ment Health J. 1996 Aug;32(4):353–361. doi: 10.1007/BF02249453. [DOI] [PubMed] [Google Scholar]
- 37.McKay MM, Lynn CJ, Bannon WM. Understanding inner city child mental health need and trauma exposure: implications for preparing urban service providers. Am J Orthopsychiatry. 2005 Apr;75(2):201–210. doi: 10.1037/0002-9432.75.2.201. [DOI] [PubMed] [Google Scholar]
- 38.Valleley RJ, Kosse S, Schemm A, Foster N, Polaha J, Evans JH. Integrated primary care for children in rural communities: An examination of patient attendance at collaborative behavioral health services. Families, Systems, & Health. 2007;25(3):323–332. [Google Scholar]
- 39.Macharia WM, Leon G, Rowe BH, Stephenson BJ, Haynes RB. An overview of interventions to improve compliance with appointment keeping for medical services. JAMA. 1992 Apr 1;267(13):1813–1817. [PubMed] [Google Scholar]
- 40.Sices L, Egbert L, Mercer MB. Sugar-coaters and straight talkers: communicating about developmental delays in primary care. Pediatrics. 2009 Oct;124(4):e705–713. doi: 10.1542/peds.2009-0286. [DOI] [PMC free article] [PubMed] [Google Scholar]