Abstract
Gastritis cystica profunda (GCP) is a rare pseudotumor of the stomach characterized by benign growths of deep gastric glands through the muscularis mucosae into the submucosa. We review a case of GCP in a 61-year-old patient with GCP, with emphasis on endoscopic ultrasound findings and present review of the current literature.
Keywords: Gastric polyp, gastritis cystica polyposa, gastritis cystica profunda
INTRODUCTION
Gastritis cystica profunda (GCP) is a rare hyperplastic lesion with unclear pathogenesis. Clinical symptoms related to GCP are variable and ranges from nonspecific abdominal pain to symptoms related to gastric outlet obstruction. In this report, we present a case of 61-year-old female with GCP who underwent endoscopic ultrasonography (EUS). EUS features of this rare condition are not widely reported in the literature.
CASE REPORT
The case we present here is about a 61-year-old African American woman presented with 1 year history of dull epigastric pain. Her past medical history was remarkable for chronic hepatitis C and tobacco consumption. She did not have any previous surgeries. Physical examination was only significant for mild epigastric tenderness and laboratory tests were unremarkable. An esophagogastroduodenoscopy showed a large submucosal mass in the antrum along the lesser curvature, with overlying nipple like cystic projection [Figure 1]. Routine endoscopic biopsies showed mild chronic inactive gastritis without evidence of Helicobacter pylori. An upper EUS showed a 3 cm submucosal antral mass with heterogeneous echogenicity, irregular shape, and cystic spaces [Figure 2]. The mass appeared to be involving the muscularis propria layer [Figure 3]. EUS guided fine-needle aspiration using 22 gauge needle (FNA) was insufficient. Patient preferred to undergo surgical resection as opposed to repeat EUS-FNA to confirm the diagnosis. Partial gastrectomy was performed and macroscopic examination of the specimen revealed a pink-tan soft 4.5 cm × 3 cm × 2 cm lesion with a 0.6 cm polypoid lesion on its mucosal aspect. The tissue was sectioned through the polypoid lesion revealing a tan homogenous cut surface with a cystically dilated area in the subepithelial region. Microscopically, there was pseudo-invasion of benign gastric glands into the muscularis propria, with cystically dilated appearing glands and no dysplastic changes [Figure 4]. These features were consistent with GCP. She was followed-up for 36 months, with no recurrence of disease or development of malignancy.
Figure 1.
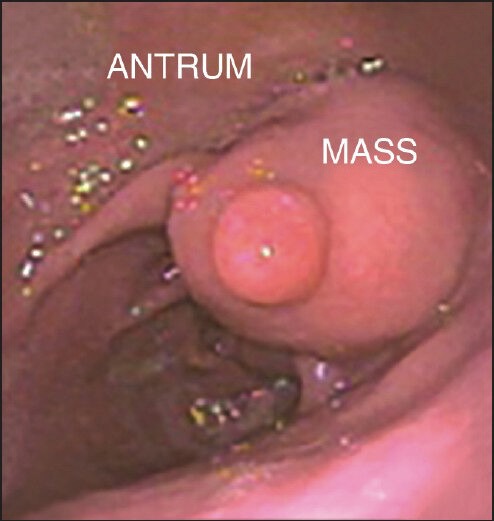
Submucosal mass in the antrum with overlying nipple like cystic projection
Figure 2.
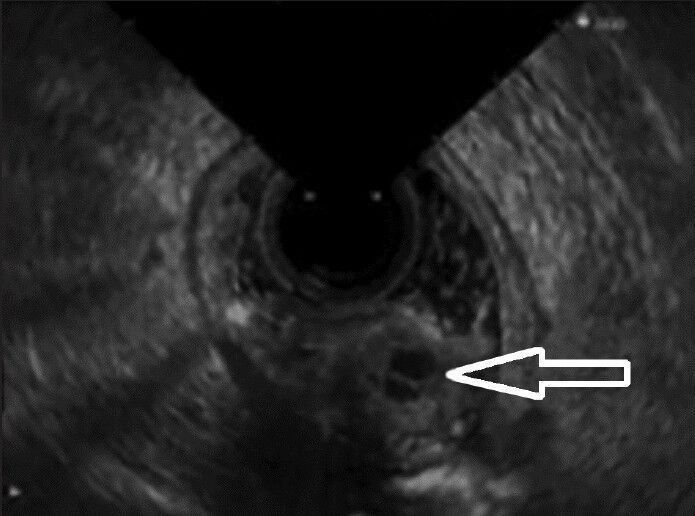
Heterogenous submucosal mass with internal cystic space (Black arrow)
Figure 3.
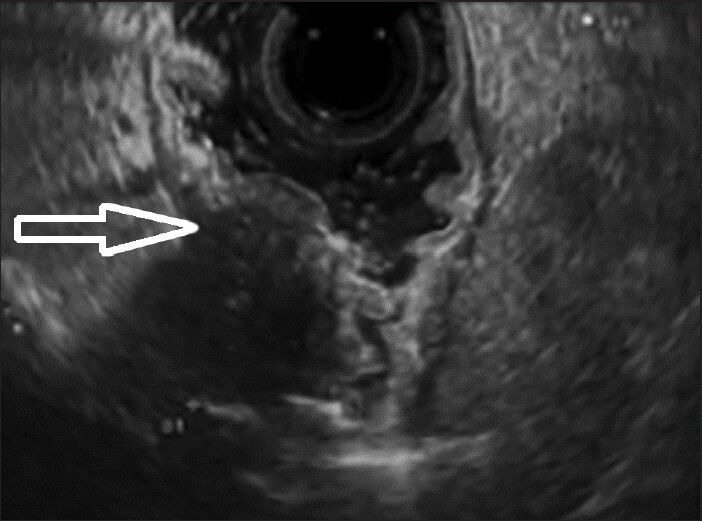
Involvement of muscularis propria layer by the heterogenous mass (White arrow)
Figure 4.
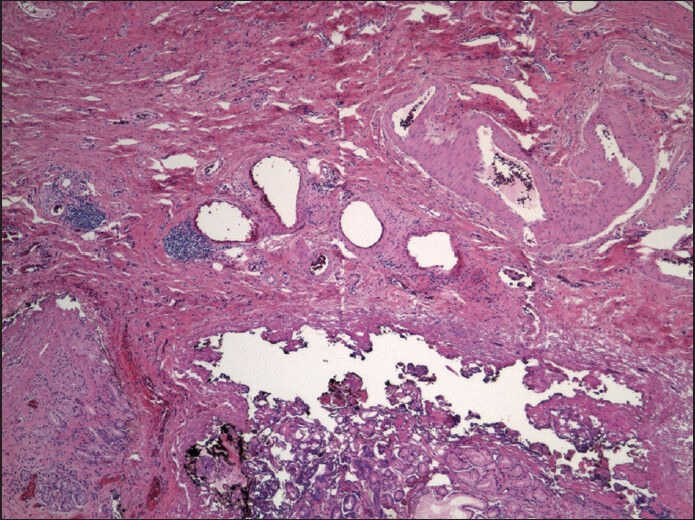
Cystically dilated gastric glands without dysplastic changes into submucosal and muscularis propria
DISCUSSION
Chronic inflammation and ischemia are the most important factors involved in the pathogenesis of GCP.[1] It is been reported in patients who have undergone gastroenterostomy[2] and is rarely found in unoperated stomachs.[2,3,4] The migration of epithelial cells into the submucosa with subsequent cystic dilation is thought to be the pathogenesis, especially in cases of prior gastric surgery. However, the pathogenesis in patients with an otherwise normal stomach remains unknown.[2]
Clinical manifestations of GCP are variable and include abdominal pain, gastrointestinal bleeding, anemia, abdominal mass and occasionally gastric outlet obstruction. Diagnosis by endoscopy is difficult because standard biopsy specimen is usually limited to the mucosa and seldom offers information about submucosa.[1] Computed tomography scan and EUS have a complementary role in delineating additional characteristics of the lesions such as size, surface contour, depth of invasion, and cystic changes.[4,5]
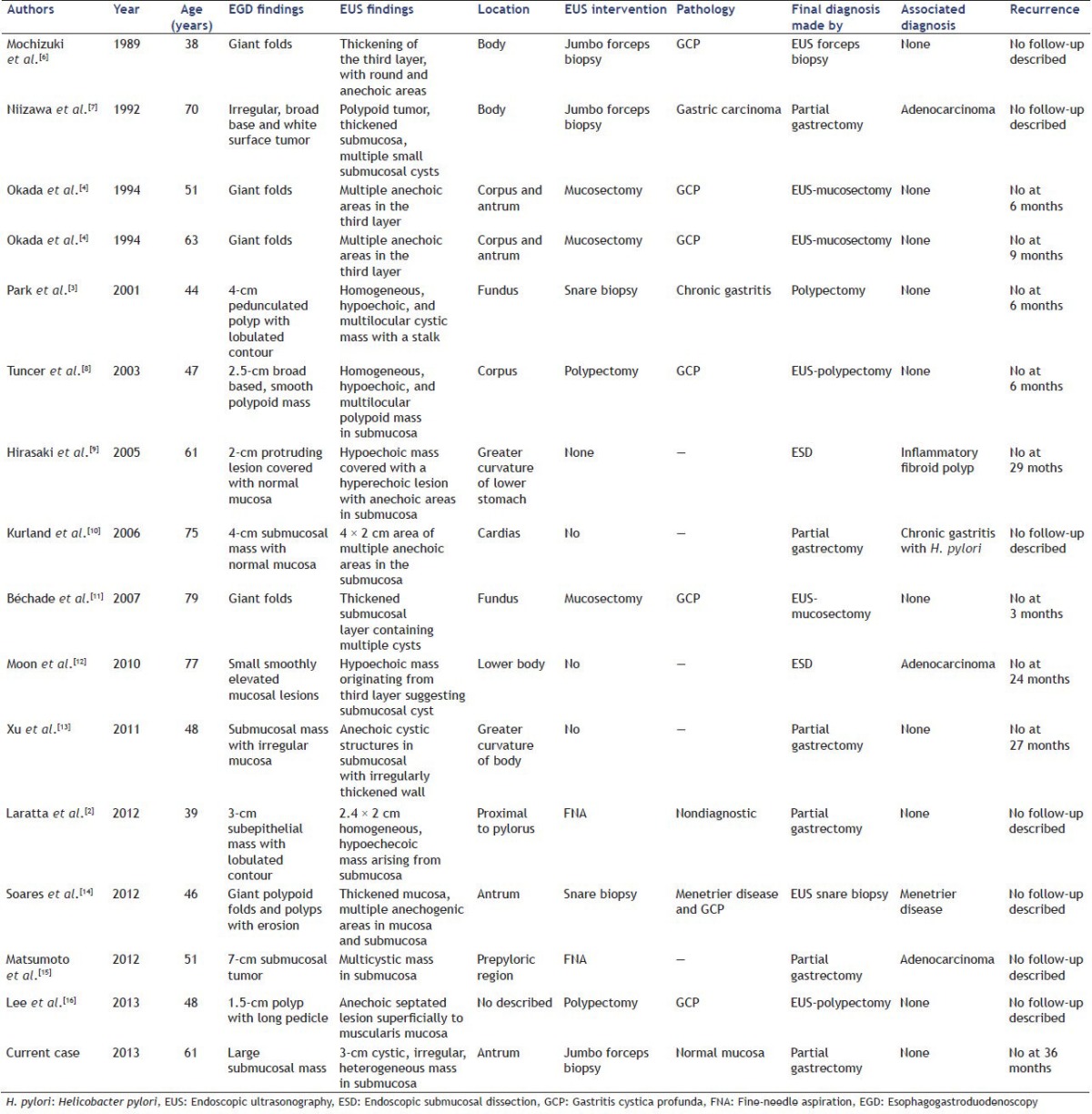
We found additional 15 cases of GCP in published literature that underwent EUS examination.[2,3,4,6,7,8,9,10,11,12,13,14,15,16] Table 1 summarizes details regarding demographics, endoscopic and EUS findings and subsequent clinical course of all these cases, including our case. The most frequent EUS feature of GCP was multiple anechoic cystic spaces/cysts in the submucosal in these cases. Heterogeneously enhancing polypoid lesions with cystic components should raise the suspicion for GCP.[5] In many cases, preoperative diagnosis of GCP remains challenging despite the current advanced in endoscopic technique and patients might have to undergo gastric resection surgery for final diagnosis and treatment.[2] A current debate exists about its biological behavior and malignant potential.[2,17] Recent advances in the endoscopic techniques like development of EUS guided FNA biopsy with 19 gauge biopsy needle and endoscopic submucosal dissection might prove useful in arriving at correct preoperative diagnosis and avoiding unnecessary surgery.
Table 1.
Endoscopic and endosonographic features of published cases with GCP
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Franzin G, Novelli P. Gastritis cystica profunda. Histopathology. 1981;5:535–47. doi: 10.1111/j.1365-2559.1981.tb01817.x. [DOI] [PubMed] [Google Scholar]
- 2.Laratta JL, Buhtoiarova TN, Sparber LS, et al. Gastritis cystica profunda: A rare gastric tumor masquesading as a malignancy. Surg Sci. 2012;3:158–64. [Google Scholar]
- 3.Park JS, Myung SJ, Jung HY, et al. Endoscopic treatment of gastritis cystica polyposa found in an unoperated stomach. Gastrointest Endosc. 2001;54:101–3. doi: 10.1067/mge.2001.114412. [DOI] [PubMed] [Google Scholar]
- 4.Okada M, Iizuka Y, Oh K, et al. Gastritis cystica profunda presenting as giant gastric mucosal folds: The role of endoscopic ultrasonography and mucosectomy in the diagnostic work-up. Gastrointest Endosc. 1994;40:640–4. doi: 10.1016/s0016-5107(94)70272-1. [DOI] [PubMed] [Google Scholar]
- 5.Wu MT, Pan HB, Lai PH, et al. CT of gastritis cystica polyposa. Abdom Imaging. 1994;19:8–10. doi: 10.1007/BF02165852. [DOI] [PubMed] [Google Scholar]
- 6.Mochizuki Y, Yao T. Diffuse heterotopic cystic malformation of the stomach report of a case. Stomach Intestine (Tokyo) 1989;24:1057–61. [Google Scholar]
- 7.Niizawa M, Ishida H, Morikawa P, et al. Diffuse heterotopic submucosal cystic malformation of the stomach: Ultrasonographic diagnosis. Gastrointest Radiol. 1992;17:9–12. doi: 10.1007/BF01888497. [DOI] [PubMed] [Google Scholar]
- 8.Tuncer K, Alkanat M, Musoðlu A, Aydin A. Gastritis cystica polyposa found in an unoperated stomach: An unusual case treated by endoscopic polypectomy. Endoscopy. 2003;35:882. doi: 10.1055/s-2003-42612. [DOI] [PubMed] [Google Scholar]
- 9.Hirasaki S, Tanimizu M, Tsubouchi E, et al. Gastritis cystica polyposa concomitant with gastric inflammatory fibroid polyp occurring in an unoperated stomach. Intern Med. 2005;44:46–9. doi: 10.2169/internalmedicine.44.46. [DOI] [PubMed] [Google Scholar]
- 10.Kurland J, DuBois S, Behling C, et al. Severe upper-GI bleed caused by gastritis cystica profunda. Gastrointest Endosc. 2006;63:716–7. doi: 10.1016/j.gie.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 11.Béchade D, Desramé J, Algayres JP. Gastritis cystica profunda in a patient with no history of gastric surgery. Endoscopy. 2007;39(Suppl 1):E80–1. doi: 10.1055/s-2006-945070. [DOI] [PubMed] [Google Scholar]
- 12.Moon SY, Kim KO, Park SH, et al. Gastritis cystica profunda accompanied by multiple early gastric cancers. Korean J Gastroenterol. 2010;55:325–30. doi: 10.4166/kjg.2010.55.5.325. [DOI] [PubMed] [Google Scholar]
- 13.Xu G, Qian J, Ren G, et al. A case of gastritis cystica profunda. Ir J Med Sci. 2011;180:929–30. doi: 10.1007/s11845-010-0618-8. [DOI] [PubMed] [Google Scholar]
- 14.Soares JB, Bastos P, Gonçalves R. Ménétrier disease with antrum polyposis and gastritis cystica profunda. Endoscopy. 2012;44(Suppl 2 UCTN):E56–7. doi: 10.1055/s-0031-1291561. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto T, Wada M, Imai Y, et al. A rare cause of gastric outlet obstruction: Gastritis cystica profunda accompanied by adenocarcinoma. Endoscopy. 2012;44(Suppl 2 UCTN):E138–9. doi: 10.1055/s-0030-1256842. [DOI] [PubMed] [Google Scholar]
- 16.Lee TH, Lee JS, Jin SY. Gastritis cystica profunda with a long stalk. Gastrointest Endosc. 2013;77:821–2. doi: 10.1016/j.gie.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 17.Mitomi H, Iwabuchi K, Amemiya A, et al. Immunohistochemical analysis of a case of gastritis cystica profunda associated with carcinoma development. Scand J Gastroenterol. 1998;33:1226–9. doi: 10.1080/00365529850172610. [DOI] [PubMed] [Google Scholar]


