Abstract
INTRODUCTION
Solitary or multiple lipomas, composed of mature fat, represents by far the most common benign mesenchymal neoplasm occurring throughout the whole body, but they rarely originate in the intestinal mesentery.
PRESENTATION OF CASE
A 60-year-old male presented with left sided abdominal distension and pain since 4 months, ultrasonography and computerized tomography abdomen was suggestive of multiple well-defined fat density lesions in the lower abdomen and pelvis. USG guided fine needle aspiration cytology was conclusive of a spindle cell lesion. Exploratory laparotomy was performed and multiple major fat tissue swellings were excised. Histopathology confirmed it to be spindle cell type of lipoma.
DISCUSSION
Because of the silent nature the exact prevalence of lipomas is unknown. It can arise in any location in which fat is normally present, reported intra abdominal lipomas have been very rare. Clinical manifestations depend on the size and location of the growth. In most patients, symptoms are few or absent. USG and CT scan abdomen are used for the diagnosis. Complete surgical excision being the only treatment.
CONCLUSION
Intra abdominal lipoma is a very rare entity, and many cases might be ignored due to their silent nature. They might or might not present with any symptoms. Complete surgical excision being the only treatment, with a very good prognosis.
Keywords: Intra abdominal, Lipoma, Complete surgical excision
1. Introduction
Lipoma is a benign soft tissue tumor, composed of mature fat, represents by far the most common mesenchymal neoplasm occurring throughout the whole body, but they rarely originate in the intestinal mesentery.6,8 A search of the English literature has revealed less than 30 documented cases. In the literature review, intra abdominal lipomas do not cause any intestinal symptoms in most cases, as it usually allow the passage of intestinal contents,1,5 and those causing abdominal pain make up only a small percentage.2,6 Because of its rarity we are presenting this case of multiple intra abdominal lipoma.
2. Presentation of case
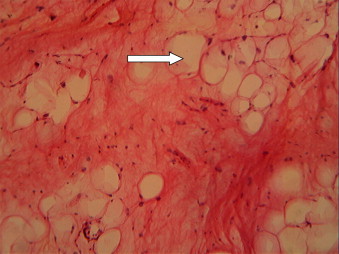
A 60-year-old male presented with left sided abdominal distension and pain since 4 months. Patient was vitally stable. On examination, left sided distension of abdomen was present, and a huge mass palpable in the left lumbar region, crossing the midline, extending up to umbilicus region. Blood investigations were within normal limits. USG and CT abdomen revealed a large well-defined fat density lesion in lower abdomen and pelvis, posteriorly encasing the adjacent aorta and inferior vena cava, displacing the small bowel loops to the right side with multiple fat density lesions with soft tissue component and septae within, in the left hypochondriac, supra-umblical and left lumbar regions. USG Guided FNAC was suggestive of a spindle cell lesion. In view of the CT findings (Fig. 1) exploratory laparotomy was performed. Multiple major fat tissue swellings (Fig. 2) were excised. Largest measuring 26 cm × 21 cm × 10 cm and weighing 3.5 kg and smallest measuring 7 cm × 6 cm × 4 cm and weighing 100 g. The masses totally weighed 9.8 kg. Cut section revealed greasy gray yellow–gray white surface with areas of cystic degeneration, along with a firm area at the center of tumor (Fig. 3). Histopathology (Figs. 4 and 5) was conclusive of spindle cell type of lipoma. Post-operative period was uneventful.
Fig. 1.
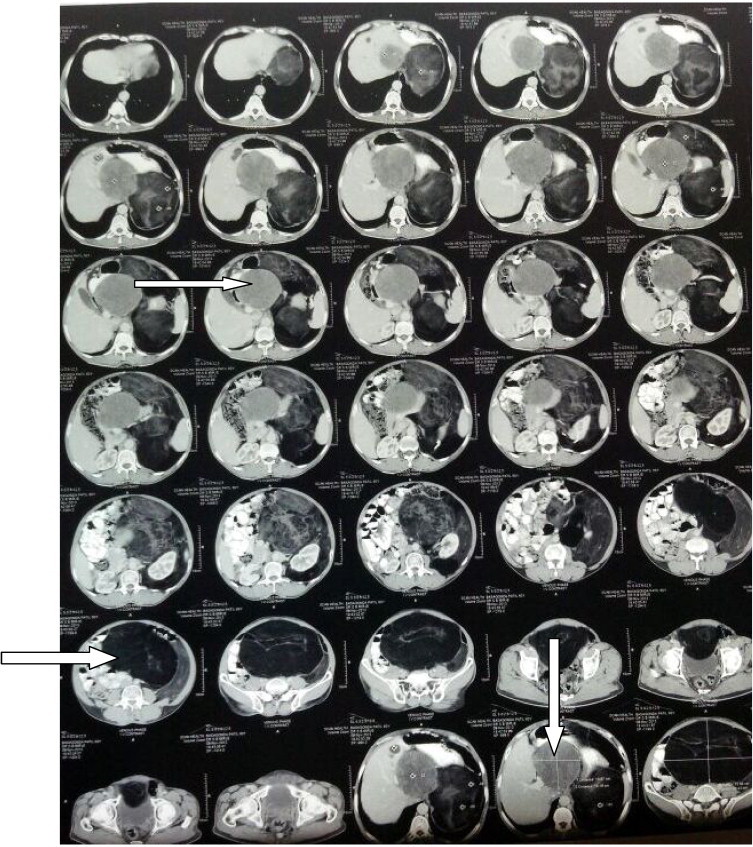
Photograph showing CT abdomen pelvis with findings of multiple well-defined fat density lesions with soft tissue component.
Fig. 2.
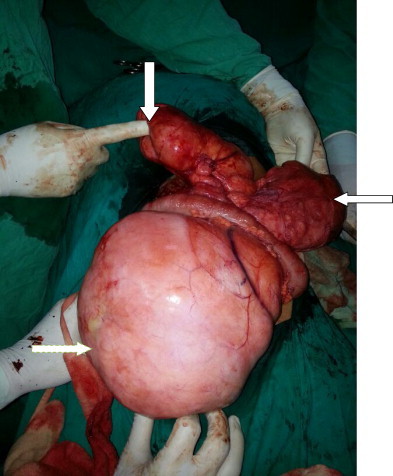
Intraoperative photograph of multiple intra abdominal lipomas.
Fig. 3.

Photograph showing cut section of intra abdominal lipoma.
Fig. 4.
Microphotograph (H&E staining) showing mature adipose tissue arranged in lobules.
Fig. 5.
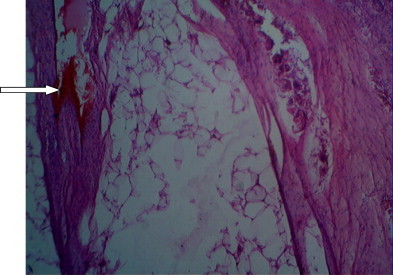
Microphotograph (H&E staining) showing lipoma with secondary changes of hemorrhage, giant cell reaction, spindle cell area also noted.
3. Discussion
The exact prevalence of lipomas is unknown, however, it is likely far higher than reported, because most cases with lipomas may be ignored due to their silent nature. It can arise in any location in which fat is normally present, reported intra abdominal lipomas have been very rare.1–9 A search of the English literature has revealed less than 30 documented cases.
Very little is known about the pathogenesis of lipomas. An increased incidence is associated with obesity, diabetes mellitus, elevation of serum cholesterol, radiation, familial tendency, chromosomal abnormalities.4,10,11 Malignant change of lipoma to liposarcoma is virtually unknown. These benign lesions may grow to large proportions and numbers but have no propensity to mutate.12,13
Deep lipomas are usually diagnosed only when the tumor grows very big or becomes symptomatic of its anatomical localization.4 Clinical manifestations depend on the size and location of the growth. In most patients, symptoms are few or absent. It may cause abdominal pain by complete intestinal obstruction as a result of torsion or volvulus3,7–9 or partial intestinal obstruction associated with compression of the intestine.
Ultrasonography will depict these intra abdominal lipomas as well-defined homogeneous, echogenic masses. Computed tomography will depict these as masses with low attenuation similar to adipose tissue.4
In most cases, complete surgical excision is easily performed because the capsule that surrounds the tumor presents a clear cleavage plane.4,14,15 When indicating excision, the possibility of liposarcoma always needs to be considered. If possible complete surgical excision of the lesion should be performed. Thus reducing the possibility of relapse, if the histopathological examination demonstrates the presence of liposarcoma.6,11,12 The recurrence rate of lipomas is less than 5% and is usually due to incomplete excision.14,15
Macroscopically, lipomas are soft, well capsulated, oval, and yellow. Lipomas generally form a slow growing non-lobulated soft and mobile mass which does not penetrate into the surrounding organs.1 Lipomas differ little in microscopic appearance from surrounding fat. Like fat they are composed of mature fat cells, but the cells vary slightly in size and shape and are somewhat larger, measuring up to 200 μm in diameter.11
The possibility of lesion being a lipoblastoma, lymphangioma, liposarcoma, or lymphangiolipoma should all be considered.12,13
4. Conclusion
Mesenteric lipoma is a very rare entity, and many cases might be ignored due to their silent nature. It has the tendency to grow to large proportions and numbers. USG and CT abdomen are the useful means for diagnosis. Complete surgical excision being the only treatment, with a very good prognosis.
Conflicts of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Ashok Y. Kshirsagar: Abstract; Nitin R. Nangare: Introduction; Dr. Vaibhav Gupta: Presentation of case and discussion; Mayank A. Vekariya: Conclusion; Ritvij Patankar: References; Abhishek Mahna: Figures; J.V. Wader: Figures.
Acknowledgment
We are thankful to Mrs. M.C. Deshingkar from Surgery Dept. Office for her secretarial help.
References
- 1.Prando A., Wallace S., Marins J.L., Pereira R.M., de Oliveira E.R., Alvarenga M. Sonographic features of benign intraperitoneal lipomatous tumor in children: report of 4 cases. Pediatr Radiol. 1990;20:571–574. doi: 10.1007/BF02129056. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Kaniklides C., Frykberg T., Lundkvist K. Pediatric mesenteric lipoma: an unusual cause of repeated abdominal pain. A case report. Acta Radiol. 1998;39:695–697. doi: 10.3109/02841859809175500. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Takagi Y., Yasuda K., Nakada T., Abe T., Saji S. Small bowel volvulus caused by a lipoma of the mesentery showing a distinct pattern on preoperative computed tomography. Dis Colon Rectum. 1998;41:122–123. doi: 10.1007/BF02236913. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Ilhan H., Tokar B., Işiksoy S., Koku N., Pasaoglu O. Giant mesenteric lipoma. J Pediatr Surg. 1999;34:639–640. doi: 10.1016/s0022-3468(99)90094-5. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Signer R.D., Bregman D., Klausner S. Giant lipoma of the mesentery: report of an unusual case and review of the literature. Am Surg. 1976;42:595–597. [PubMed] [PubMed] [Google Scholar]
- 6.Sato M., Ishida H., Konno K., Komatsuda T., Naganuma H., Segawa D. Mesenteric lipoma: report of a case with emphasis on US findings. Eur Radiol. 2002;12:793–795. doi: 10.1007/s003300101026. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Sheen A.J., Drake I., George P.P. A small bowel volvulus caused by a mesenteric lipoma: report of a case. Surg Today. 2003;33:617–619. doi: 10.1007/s00595-003-2533-3. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Ozel S.K., Apak S., Ozercan I.H., Kazez A. Giant mesenteric lipoma as a rare cause of ileus in a child: report of a case. Surg Today. 2004;34:470–472. doi: 10.1007/s00595-003-2724-y. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Wong H.I., Chen C.Y., Liu G.C. Primary mesenteric lipoma causing closed loop bowel obstruction: a case report. Kaohsiung J Med Sci. 2005;21:138–141. doi: 10.1016/S1607-551X(09)70291-8. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weiss S.W., Goldblum J.R. 5th ed. Mosby; St Louis, MO: 2007. Enzinger and Weiss's soft tissue tumors. [Google Scholar]
- 11.Enzinger F.M., Weiss S.W. 3rd ed. Mosby; St. Louis, MO: 1995. Soft tissue tumors; pp. 384–405. [Google Scholar]
- 12.Lucas D.R., Nascimento A.G., Sanjay B.K., Rock M.G. Well-differentiated liposarcoma. The Mayo Clinic experience with 58 cases. Am J Clin Pathol. 1994;102:677–683. doi: 10.1093/ajcp/102.5.677. [DOI] [PubMed] [Google Scholar]
- 13.Munk P.L., Lee M.J., Janzen D.L. Lipoma and liposarcoma: evaluation using CT and MR imaging. AJR Am J Roentgenol. 1997;169:589–594. doi: 10.2214/ajr.169.2.9242783. [DOI] [PubMed] [Google Scholar]
- 14.Livne P.M., Zer M., Shmuter Z., Dintsman M. Acute intestinal obstruction caused by necrotic mesenteric lipoma: a case report. Am J Proctol Gastroenterol Colon Rectal Surg. 1981;32:19–22. [PubMed] [Google Scholar]
- 15.Tani T., Abe H., Tsukada H., Kodama M. Lipomatosis of the ileum with volvulus: report of a case. Surg Today. 1998;28:640–642. doi: 10.1007/s005950050198. [DOI] [PubMed] [Google Scholar]


