Abstract
INTRODUCTION
Gastric diverticulum is a rare and frequently asymptomatic condition. Symptoms include vague pain, fullness, dyspepsia, vomiting, hemorrhage and perforation. Occasionally, the patient can present with belching and oral fetor.
PRESENTATION OF CASE
We report a 58-year-old woman with a gastric diverticulum who was suffering from a socially disabling oral fetor. After a thorough evaluation, a laparoscopic resection of the diverticulum was offered and completed successfully. At follow-up, the oral fetor had disappeared. The patient had no complaints and regarded herself as cured.
DISCUSSION
Although indications for the treatment of asymptomatic patients remain to be defined, pharmacological therapies including protein pump inhibitors and histamine receptor blockers have been employed, with limited effects in patients with miscellaneous symptoms. Surgery is required when serious complications such as hemorrhage or perforation of the diverticulum occur.
CONCLUSION
Surgery is required when serious complications such as hemorrhage or perforation of the diverticulum occur. Therapy resistent social disabling oral fetor may add to the indications for surgery.
Keywords: Gastric diverticulum, Halitosis, Oral fetor, Surgery, Laparoscopy, Treatment
1. Introduction
Gastric diverticula are rare and usually incidental findings.1,2 Its symptoms, including pain, reflux, bloating, a sensation of fullness and nausea, can be vague and unspecific.3 In rare cases, a gastric diverticulum has simulated a left adrenal tumor4,5 and has been diagnosed based on signs of gastrointestinal bleeding6 or even hemorrhagic shock.7 Recently, troublesome belching with fetor has been linked to the condition.8 In most patients, it remains challenging to associate a diverticulum diagnosed by radiology or endoscopy with relatively unspecific symptoms and complaints.
2. Case report
An otherwise healthy 58-year-old woman was referred due to a long history of belching and halitosis that severely impacted her social life. Various conservative treatments, including appropriate dental and oral maintenance and treatment with a proton pump inhibitor (PPI), had been used without success.
During gastroscopy, a gastric diverticulum situated in the corpus-fundic region was encountered (Fig. 1). No specific content or findings were observed through the 20 mm circular opening of the diverticulum. Endoscopy revealed a normal diverticular mucosa, and there were no signs of malignancy. The remaining findings were normal, with no evidence of hiatal hernia, gastritis or gastroesophageal reflux disease.
Fig. 1.

Endoscopic view of a 2 cm opening at the base of the diverticulum.
Imaging by computer tomography (CT) (Fig. 2) revealed a significant diverticulum on the posterior wall of the gastric corpus.
Fig. 2.
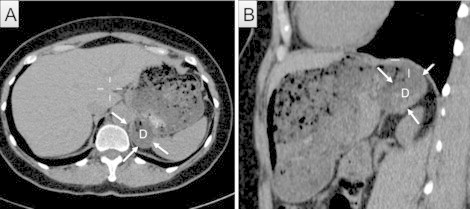
Imaging (computer tomography, CT) of the diverticulum situated at the upper dorsal region of the stomach. (A) Transverse view with the diverticulum (D) indicated by arrows. (B) Sagital view of the same.
An association between the patient's gastric diverticulum and the oral fetor was suspected, and a laparoscopic resection of the gastric diverticulum was offered. The patient regarded her social situation as “hopeless” and was happy to accept a laparoscopic surgical approach after being informed about the risks of the procedure and that the procedure could not guarantee a successful result.
Our laparoscopic set-up in this case was similar to the standard laparoscopic Nissen fundoplication set-up. The omental bursa was approached by dividing the gastrocolic ligament with a Harmonic scalpel (Ethicon UltraCision Harmonic Scalpel ™, Ethicon Norway, a Johnson & Johnson Company, USA). The diverticulum was identified on the posterior gastric wall by a cephalic elevation of the stomach. After carefully dissection to free the diverticulum from surrounded tissues, a linear stapler (Endo-GIA™ Universal Stapling System, Covidien company, USA), was placed across the base of the diverticulum, which was resected by executing the linear stapler (Fig. 3). The stapler row was over sewn by a running suture with resorbable coated polyclacin 3–0 suture (Vicryl ™, Ethicon Norway) and reinforced by a tegmentation with an omental flap. Finally, by installation of 100 ml methylene blue sterile water into the stomach, no leakage was suspected, and the procedure was successfully completed without any technically difficulties. The postoperative period was uneventful. The patient resumed an oral diet over the next few days, and was discharged from the hospital on the fourth postoperative day.
Fig. 3.
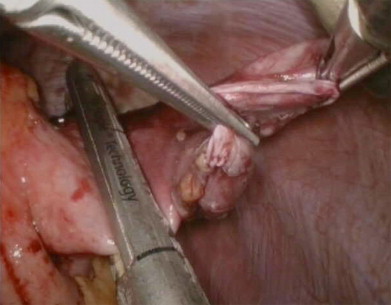
Laparoscopic resection by stapling the basis of the diverticulum.
A morphological analysis of the specimen revealed a gastric diverticulum measuring 3.2 cm × 3.2 cm with a completely normal mucosa. A routine bacterial swab of the diverticulum did not show growth of any microbes or fungi.
At a follow-up 2 months after the operation, both the belching and the oral fetor had disappeared. Moreover, 14 months after surgery, she remains asymptomatic, and regards herself as cured.
3. Discussion
Gastric diverticula are rare and mostly asymptomatic. Their reported incidence ranges from 0.01 to 2.6%, depending on the method of detection.9 No specific treatment for an asymptomatic gastric diverticulum is recommended, and even in symptomatic patients, the appropriate treatment is not well defined. Vague upper abdominal pain, explained by the distension of the diverticulum, is the most common complaint, encountered in 18–30% of symptomatic patients. Other complaints include vomiting, dysphagia and belching. Food retention and bacterial overgrowth within the diverticulum have been suggested to explain the belching and oral fetor.8,10 The same authors also reported successful surgical resection. However, the true mechanisms of bacterial overgrowth in the gastrointestinal tract are complex,11 and we could not confirm the growth of any gram-negative bacilli or other microbes from swabs of the diverticulum.
Treatment with PPIs has been suggested to resolve the symptoms of gastric diverticula, but this therapy does not resolve the underlying pathology.12 A suggested relationship between Helicobacter pylori infection and objective halitosis could not be confirmed in a recent study, and the authors conclude that halitosis nearly always originates within the oral cavity, and seldom or never within the stomach.13 In contrast, a recent study on children and young adults by Kinberg et al.,14 reports that gastrointestinal pathology was common in patients with halitosis, regardless of dental or otolaryngeal findings, and most patients improved with treatment.
Surgical resection is recommended if the diverticulum causes symptoms despite pharmacological treatment or is complicated by large size (a diameter exceeding 4 cm), bleeding, perforation or malignancy.2 Laparoscopic resection is considered a safe and suitable procedure when surgery is planned.9,10 Excellent outcomes after laparoscopic resection have been reported.2
Of note, many patients with a gastric diverticulum have comorbid gastrointestinal diseases that may cause their symptoms, and appropriate investigations and evaluation of these diseases are important before specific treatment is employed. A careful history is of great importance, and the patient's complaints should be appropriately appreciated and acknowledged. As shown in our patient, surgery may some times make a clinical difference, even though the true mechanisms to explain this clinical observation are not fully understood.
Conflict of interest
Nothing to declare.
Funding
No funding.
Ethical approval
According to the general guidelines of the Regional Ethics Committee (“REK-Vest”) the surgical treatment employed on this patient is not considered a matter of ethical concern.
Author Contributions
Marius Osland Muis: patient management, study concept, data & literature analysis and interpretation, writing the paper.
Kristian Leitao: patient management, literature interpretation, writing the paper, final revision and approval of the submitted manuscript.
Jorunn Havnen: patient management, literature analysis and interpretation, final revision and approval of the submitted manuscript.
Tom B. Glomsaker: patient management, literature analysis and interpretation, final revision and approval of the submitted manuscript.
Jon Arne Søreide: patient management, study concept, data & literature analysis and interpretation, writing the paper, final revision and approval of the submitted manuscript.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
References
- 1.Brown C.H., Bissonnette R.P., Albee R.D. Diverticula of the stomach; a report of 30 cases and a review of the literature. Gastroenterology. 1949;12:10–23. [PubMed] [Google Scholar]
- 2.Rashid F., Aber A., Iftikhar S.Y. A review on gastric diverticulum. World J Emerg Surg. 2012;7:1. doi: 10.1186/1749-7922-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eitzen K., Eslick G.D., Daneshjoo R. Dyspepsia and gastroesophageal reflux symptoms predominate in gastric diverticulum. J Dig Dis. 2012;13:335–336. doi: 10.1111/j.1751-2980.2012.00595.x. [DOI] [PubMed] [Google Scholar]
- 4.Araki A., Shinohara M., Yamakawa J. Gastric diverticulum preoperatively diagnosed as one of two left adrenal adenomas. Int J Urol. 2006;13:64–66. doi: 10.1111/j.1442-2042.2006.01236.x. [DOI] [PubMed] [Google Scholar]
- 5.Chasse E., Buggenhout A., Zalcman M. Gastric diverticulum simulating a left adrenal tumor. Surgery. 2003;133:447–448. doi: 10.1067/msy.2003.47. [DOI] [PubMed] [Google Scholar]
- 6.Zakary N.Y., van Langenberg D.R., Alshumrany M. Gastrointestinal: acute haemorrhage from a Dieulafoy lesion within a gastric diverticulum managed endoscopically. J Gastroenterol Hepatol. 2009;24:1891. doi: 10.1111/j.1440-1746.2009.06094.x. [DOI] [PubMed] [Google Scholar]
- 7.Perbet S., Constantin J.M., Poincloux L. Gastric diverticulum: a rare cause of hemorrhagic shock. Intensive Care Med. 2008;34:1353–1354. doi: 10.1007/s00134-008-1070-3. [DOI] [PubMed] [Google Scholar]
- 8.Rashid F., Singh R., Cole A. Troublesome belching with fetor odour. Gut. 2010;59(310):324. doi: 10.1136/gut.2009.177337. [DOI] [PubMed] [Google Scholar]
- 9.Schiller A.H., Roggendorf B., Delker-Wegener S. [Laparoscopic resection of gastric diverticula: two case reports] Zentralbl Chir. 2007;132:251–255. doi: 10.1055/s-2007-960753. [DOI] [PubMed] [Google Scholar]
- 10.Donkervoort S.C., Baak L.C., Blaauwgeers J.L. Laparoscopic resection of a symptomatic gastric diverticulum: a minimally invasive solution. JSLS. 2006;10:525–527. [PMC free article] [PubMed] [Google Scholar]
- 11.Husebye E. The pathogenesis of gastrointestinal bacterial overgrowth. Chemotherapy. 2005;51(Suppl. 1):1–22. doi: 10.1159/000081988. [DOI] [PubMed] [Google Scholar]
- 12.Mohan P., Ananthavadivelu M., Venkataraman J. Gastric diverticulum. CMAJ. 2010;182:E226. doi: 10.1503/cmaj.090832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tangerman A., Winkel E.G., de Laat L. Halitosis and Helicobacter pylori infection. J Breath Res. 2012;6:017102. doi: 10.1088/1752-7155/6/1/017102. [DOI] [PubMed] [Google Scholar]
- 14.Kinberg S., Stein M., Zion N. The gastrointestinal aspects of halitosis. Can J Gastroenterol. 2010;24:552–556. doi: 10.1155/2010/639704. [DOI] [PMC free article] [PubMed] [Google Scholar]


