Abstract
INTRODUCTION
We aimed to present the management of a patient with fistula of ileal conduit in open abdomen by intra-condoid negative pressure in conjunction with VAC Therapy and dynamic wound closure system (ABRA).
PRESENTATION OF CASE
65-Year old man with bladder cancer underwent radical cystectomy and ileal conduit operation. Fistula from uretero-ileostomy anastomosis and ileus occurred. The APACHE II score was 23, Mannheim peritoneal index score was 38 and Björck score was 3. The patient was referred to our clinic with ileus, open abdomen and fistula of ileal conduit. Patient was treated with intra-conduid negative pressure, abdominal VAC therapy and ABRA.
DISCUSSION
Management of urine fistula like EAF in the OA may be extremely challenging. Especially three different treatment modalities of EAF are established in recent literature. They are isolation of the enteric effluent from OA, sealing of EAF with fibrin glue or skin flep and resection of intestine including EAF and re-anastomosis. None of these systems were convenient to our case, since urinary fistula was deeply situated in this patient with generalized peritonitis and ileus.
CONCLUSION
Application of intra-conduid negative pressure in conjunction with VAC therapy and ABRA is life saving strategies to manage open abdomen with fistula of ileal conduit.
Keywords: Negative pressure, Dynamic closure, Open abdomen, Entero atmospheric fistula, Ileal conduit
1. Introduction
The treatment of open abdomen (OA) in trauma, abdominal compartment syndrome, severe secondary peritonitis and major abdominal wall defects is extremely important and difficult condition.1,2 Numerous methods have been presented for management of OA.6,7 However, data confirming their role in the management of OA complicated with fistula are limited.3
The fistula may be present at the beginning or develop during treatment. The fistula formation in OA is the most critical complication. If an enteric fistula occurred in OA, it is called entero-atmospheric fistula (EAF). It is not a true fistula since it has no a fistula tract and it is not covered with tissue. For these reasons, spontaneous closure of EAF is almost impossible.3 EAF occurs in 25% of patients with OA with a reported mortality rate of 42% up to 75%.4
In recent years, although great deal on management of open abdomen, difficulties of treatment of open abdomen with fistula remain as a constant problem. Correcting the nutritional depletion, severe fluid and electrolyte imbalance, controlling local infection, systemic sepsis, fistula drainage and definitive abdominal closure may be extremely challenging.1 Management of OA with urinary fistula of ileal conduit by VAC therapy was very rare in literature. VAC therapy was applied successfully in one patient with urinary tract leakage after surgical treatment of bladder cancer and in 2 patients with recurrent urinary fistula following kidney transplantation into an ileal conduit.5,6
Our aim is to present application of intra-conduit negative pressure in conjunction with abdominal VAC therapy and ABRA to manage open abdomen with fistula of ileal conduit. According to our knowledge this is the first case in the literature.
2. Case report
65-Year old man with bladder cancer had undergone radical cystectomy and urinary diversion with ileal conduit. General condition of the patient deteriorated at 8th postoperative day, he couldn’t defecate and abdominal distention increased. The patient underwent operation emergently. There was severe intestinal ileus, urine peritonitis, fistula from uretero-ileostomy. It was seen that intestinal obstruction developed due to compression of ileal conduit to ileoileal anastomosis. Intestinal passage was maintained by dissecting ileal conduit and ileoileal anastomosis side. Abdominal content was irrigated with Normal Saline (NS) and leakage point was repaired primarily. When general condition of the patient deteriorated and intraabdominal pressure of patient increased up to 25 mmHg, the patient underwent 3rd operation at postoperative 14th day. Leakage point was repaired again. Since abdomen of the patient could not be closed, VAC therapy was started to manage the open abdomen. (Table 1) Patient was consulted to us 17 days after first operation. On admission, patient was in septic shock status and intubated. Arterial blood pressure:70/30 mmHg, Heart rate: 120/min, Body temperature: 38.0 °C, Hemoglobine: 9 g/L, WBC: 21.000, Plt: 55000, Urea: 70, creatinine: 2.1, K: 2.9, Na: 134, Albumin: 2.5, Alanine transaminase: 210, Aspartate transaminase: 260, Aalkaline phosphatase: 190.
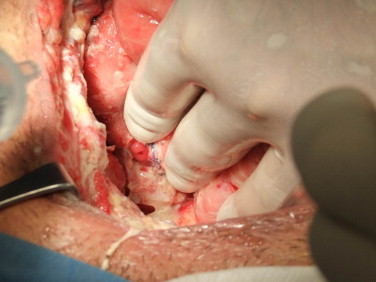
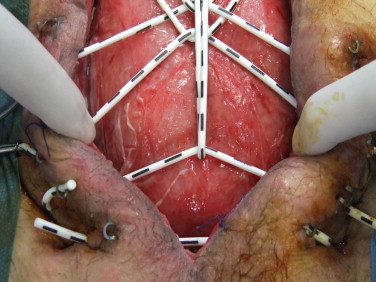
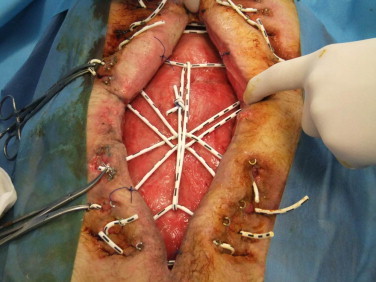
Apache II score, Björck score,7 and MPI score8 was 23, 3, 38 respectively. Abdomen was fully open (wide 29 cm length 25 cm). There was severe urine peritonitis with edematous abdominal content and ileus at 4th operation. (Fig. 1) Fascia of abdomen was severely damaged because of relaparotomies. Abdominal content was irrigated with warm NS and fistula of uretero-ileostomy was seen. (Fig. 2), Ileostomy was opened to patient's left side to resolve ileus. Fistula was repaired primarily and nephrostomy catheters were inserted to the kidneys bilaterally to drain urine outside. Abdomen negative pressure system was applied by standard method to the abdomen (ABthera, KCI) A perforated polyethylene sheet was placed over the abdominal content under the fascia in order to prevent other intestinal fistula formation and adhesion to the abdominal wall. (Fig. 3) Sponge was placed over the silicone sheet between fascias and covered with drapes. Approximately 5–6 cm opening was made in the center of the drape to apply suction tubing system. Creatinine level of abdominal fluid increased on 4th day of our first opration. After debridement and irrigation of abdomen with warm NS, leakage point was repaired primarily again (Fig. 4). The second negative pressure system was applied on uretero-ileostomy in conjunction with standard abdominal VAC therapy of 21st day of first operation. First of all, two Foley catheters were inserted in ileum pouch up to fistula point. Catheters were cut at skin level. Approximately 8 cm × 8 cm circle crafted sponge was put on the catheters and covered with drapes. An opening was made in center of second system to apply tubing system. One more drape was added all over them. These two systems were synchronized by Y connector system (Fig. 4). Continuous −75 mm Hg negative pressure was used for first 3 days. After this, the negative pressure of VAC dressing was adjusted between (−75 to 125 mmHg) intermittantly, 4 or 10 min of high negative pressure was followed by 1 or 2 min of low negative pressure respectively. The dressing was changed every 2–4 days. The second system was controlled and changed more often to prevent clogging. After urinary fistula was taken under control, patient's general condition has improved. After resolution of ileus nasoduodenal tube feeding was started from 2nd day and early enteral feeding of patient was given on 4th day and parenteral nutritional support was decreased. After both negative pressure systems has been used together for 6 days, the second system was stopped. ABRA system was added to management on regression of sepsis at 30. day of 1st operation (Fig. 5). The elastomers of ABRA were inserted through the full thickness of the abdominal wall at a distance of approximately 5 cm from the medial fascia margin. The elastomers were aligned about 3 cm part across the defect of OA. We had to modify the application of ABRA, since he has urostomy on right side and ileostomy on left side. The upper two elastomers were used crossing over lower two elastomers to occupy center of abdomen (Fig. 6). The optimal tension was obtained by stretching the elastomers 1.5–2 their tension free length. ABRA was adjusted when VAC dressing was changed9 (Fig. 6). After 3 weeks, abdominal fascia of patient came across and fascia was closed by PDS suture without mesh. Skin closure was performed and the patient was discharged 2 days after fascial closure (Fig. 7). Anchors of ABRA were removed and treatment was terminated 5 days after skin closure.
Fig. 1.

Severe urine peritonitis with edematous abdominal content and ileus. Dilated small intestine loops and large abdominal defect (29 cm × 25 cm) of open abdomen are shown.
Fig. 2.
Fistula from uretero-ileostomy anastomosis (arrow sign).
Fig. 3.

Standard abdomen negative pressure system was applied to the abdomen (ABthera, KCI) Silicone cover of VAC Therapy is seen.
Fig. 4.

Both applied standard abdominal VAC therapy system and intra-conduit negative pressure system are seen. Two negative pressure systems connected by Y connector are seen.
Fig. 5.
Well granulation tissue and ABRA system.
Fig. 6.
Modified application of ABRA.
Fig. 7.

Totally closed fascia and skin.
We used the VAC system at 17th day of the first laparotomy and treatment duration was 33 days. We added second negative pressure system to VAC therapy at 21st day and used together for 6 days. On 30th day after first operation, ABRA system was added to treatment. VAC therapy and ABRA systems were used together for 20 days. ABRA system was used 27 days.
3. Discussion
Management of urine fistula like EAF in the OA may be extremely challenging. Success rate of septic OA management was influenced by hemodynamic status, degree of peritonitis, adhesion and fixity of abdominal organ.7,8,10 Primary suturing of the fistula is rarely successful as in this patient. Three different treatment modalities of EAF are established especially in recent literature.They are isolation of the enteric effluent from OA, sealing of EAF with fibrin glue or skin flep and resection of intestine including EAF and re-anastomosis. For isolation of enteric effluent from OA, floating stoma, fistula VAC, nipple VAC, ring and silo VAC, fistula intubation systems are used.3 For all of these systems to be applied successfully, fistula should be superficially located and taken under control to some extent. None of these systems were convenient to our case, since urinary fistula was deeply situated in this patient with generalized peritonitis and ileus. Resection of intestinal loop including fistula and re-anastomosis of the intestine was also impossible in this case because of the fact that anatomy of ileal conduit could not be visualized due to intraabdominal adhesions.
In 1995 Morykwas and Argenta introduced vacuum assisted closure (VAC) into the management of complex wound healing disorders.11 Intra-abdominal exudates and edema was evacuated with abdominal VAC therapy. Synchronized negative pressure system placed inside the ileal conduit on uretero-ileostomy was used to neutralize negative pressure effects of abdominal VAC therapy on the ileum pouch at fistula side, otherwise abdominal VAC therapy could increase leakage by expanding the fistula orifice (Fig. 8). By using intra-conduit negative pressure system diversion of urine output was provided and isolated from OA. After all the effluent was isolated from abdominal wound, healing was accelerated. We also took fistula under control by using intrarectal(intraluminal) NPS in a similar open abdomen patient with colorectal fistula.12 After regression of abdominal sepsis dynamic wound closure system was added to treatment. It prevented further lateral retraction of the abdominal muscles and fascia by offering a dynamic and continuously adjustable traction. In the meantime, it allowed both expansion and retraction in accordance with oscillation of breathing and patient movement.13 As far as we are concerned, application of ABRA is best employed in combination with VAC dressing in septic OA.9,14
Fig. 8.
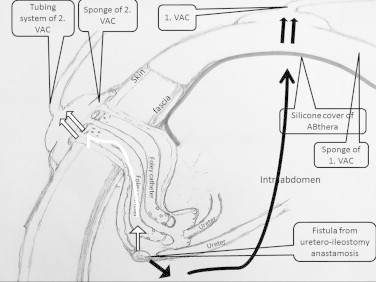
Schematic illustration of abdominal VAC therapy in conjunction with intra-conduit negative pressure systems.
Denzinger et al. presented that VAC therapy was performed successfully in urinary tract leakage after surgical treatment of bladder cancer.5 Heap et al. used VAC therapy in the treatment of two patients with urinary fistula of ileal conduit after kidney transplantation.6 Hovewer, these three patients healed by granulation with giant hernia, creating a need for one more operation. Whereas, there was no any hernia in our patient and no need any operation during follow up. This may be caused by use of intra-conduit negative pressure in conjunction with abdominal VAC therapy and ABRA system to close the fascia and skin without mesh.
4. Conclusion
We present the first report in application of intra-conduit negative pressure in conjunction with VAC therapy and ABRA. It is a life saving strategy to manage open abdomen with fistula of ileal conduit.
Conflict of interest
None declared.
Funding
None declared.
Ethical approval
We had obtained written and signed consent to publish the case report from the patient.
Author contributions
Fahri YETİŞİR: Study design and study analysis, Writing, Data collection, patient treatment and follow-up; A.Ebru SALMAN: Writing, patient treatment and follow-up; Muhittin AYGAR: Writing, Data collection; Faik YAYLAK Writing; M.AKSOY. Data collection; A. YALCIN. Data collection.
References
- 1.D’Hondt M., Devriendt D., Van Rooy F. Treatment of small-bowel fistulae in the open abdomen with topical negative-pressure therapy. Am J Surg. 2011;202:20–24. doi: 10.1016/j.amjsurg.2010.06.025. [DOI] [PubMed] [Google Scholar]
- 2.Verdam F.J., Dolmans D.E.J.G., Loos M.J., Raber M.H., De Vit R.J., Charbon J.A. Delayed primary closure of the septic open abdomen with a dynamic wound closure system. World J Surg. 2011;35:2348–2355. doi: 10.1007/s00268-011-1210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marinis A., Gkiokas G., Argyra E., Fragulidis G., Polymeneas G., Voros D. Enteroatmospheric fistulae-gastrointestinal openings in the open abdomen: a review and recent proposal of a surgical technique. Scand J Surg. 2013;102(2):61–68. doi: 10.1177/1457496913482252. [DOI] [PubMed] [Google Scholar]
- 4.Makhdoom Z., Komar M.J., Still C.D. Nutrition and enterocutaneous fistulas. J Clin Gastroenterol. 2000;31:195–204. doi: 10.1097/00004836-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Denzinger S., Luebke L., Burger M., Kessler S., Wieland W.F., Otto W. Vacuum-assisted closure therapy in ureteroileal anastomotic leakage after surgical therapy of bladder cancer. World J Surg Oncol. 2007;5:41. doi: 10.1186/1477-7819-5-41. [PMID: 17430598] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heap S., Mehra S., Tavakoli A., Augustine T., Riad H., Pararajasingam R. Negative pressure wound therapy used to heal complex urinary fistula wounds following renal transplantation into an ileal conduit. Am J Transplant. 2010;10(October (10)):2370–2373. doi: 10.1111/j.1600-6143.2010.03237.x. [DOI] [PubMed] [Google Scholar]
- 7.Björck M., Bruhin A., Cheatham M. Classification – important step to mprove management of patients with an open abdomen. World J Surg. 2009;33:1154–1157. doi: 10.1007/s00268-009-9996-3. [DOI] [PubMed] [Google Scholar]
- 8.Bosscha K., Reijnders K., Hulstaert P.F. Prognostic scoring systems to predict outcome in peritonitis and intraabdominal sepsis. Br J Surg. 1997;84:1532–1534. [PubMed] [Google Scholar]
- 9.Salman A.E., Yetişir F., Aksoy M., Tokaç M., Yıldırım M.B., Kılıç M. Use of dynamic wound closure system in conjunction with vacuum-assited closure therapy in delayed closure of open abdomen. Hernia. 2012 doi: 10.1007/s10029-012-1008-0. [DOI] [PubMed] [Google Scholar]
- 10.Tsuei B.J., Skinner J.C., Bernard A.C. The open peritoneal cavity: etiology correlates with the likelihood of fascial closure. Am Surg. 2004;70:652–656. [PubMed] [Google Scholar]
- 11.Argenta L.C., Morykwas M.J. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997;38:563–576. [PubMed] [Google Scholar]
- 12.Yetişir F., Salman A.E., Mamedov R., Aksoy M., Yalcin A., Kayaalp C. Intrarectal negative pressure system in the management of open abdomen with colorectal fistula: a case report. Int J Surg Case Rep. 2014 doi: 10.1016/j.ijscr.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boele van Hensbroek P., Wind J., Dijkgraaf M.G., Busch O.R., Goslings J.C. Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg. 2009;33:199–207. doi: 10.1007/s00268-008-9867-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yetişir F., Salman A.E., Özdemir F. Modified application of dynamic wound closure system in the management of septic open abdomen. World J Trauma Critical Care Med. 2013;1:1–8. [Google Scholar]


