Summary
The role of the orthopaedic surgeon in the treatment of patients with fragility fractures is twofold: the conservative or surgical treatment of the fracture, and the prevention of further fractures, establishing diagnostic and therapeutic procedures for osteoporosis.
We evaluated 72 patients treated surgically for fragility vertebral fracture and 801 patients treated surgically for fragility hip fracture, operated from 2009 to 2010 at O.U. Orthopaedics and Traumatology of S.M. Annunziata Hospital of Florence, that have followed a treatment for refractures prevention according to the TARGET (Appropriate Treatment for Refractures GEriatric in Tuscany) Project of Tuscany Region.
The average follow-up was 34 months.
Patients with vertebral fracture treated for refractures prevention were 58 (80.6%), while patients with hip fracture treated for refractures prevention were 307 (38.3).
Results
the number of patients with vertebral fracture who had a refracture in the first two years after surgery was 12 (16.6%), of which 9 patients were not treated for osteoporosis.
The percentage of refracture at 1 year after surgery in patients with hip fractures was 3.19% in 2009 and 2.17% in 2010, compared to 5.16% of refracture of 2006 when the TARGET Project was not yet started.
Mortality at 1 year after surgery in patients with hip fracture treated for osteoporosis was 19% compared to 25–31% in the patients not treated for osteoporosis.
Keywords: osteoporosis, fragility fractures, hip fractures, vertebral fractures, refractures
Introduction
Osteoporosis is a chronic disease and increases the risk of fragility fractures which are a very important problem for incidence and social cost (1–3).
The progressive age increasing of the population leads inevitably to an increase of all the age associated pathologies, making the osteoporosis a health and social care priority in our Country (17–21).
Osteoporosis is considered by the World Health Organization (WHO) to be second only to cardiovascular disease as a critical health problem (4–15, 16).
It is estimated that each year 9 million new fragility fractures occurs in the world, of whom approximately 1.6 million are fractures of the proximal femur.
The prevention is therefore of strategic importance.
It is important to remind that a fragility fracture represents the most important predictive factor for further fragility fractures and therefore how important it is to implement any form of prevention to reduce the risk of subsequent fractures (5).
The disability in femoral fracture is permanent in 20% of cases with a high rate of institutionalization (20–25%) and only 30–40% of patients recuperate an autonomy compatible with previous activities of daily living (Osteoporosis International Foundation, 2002).
The risk of a contralateral hip fracture after a hip fracture is 13.8%, with an increase also of fractures in other sites (9–11).
Mortality at 1 year after surgery in patients with hip fracture is greater than 20%.
The total estimated cost to Tuscany Region was 101 million euro in the 2007 (2).
Vertebral fractures are associated to a higher risk of subsequent fragility fractures and increased risk of mortality (6–8).
The total estimated cost to Italy of all the 190,000 new fractures vertebral (including hospitalizations and interventions) is 300 million euro year (5).
All these data indicate that the amount of osteoporotic fractures in Italy is extremely high and the prevention strategies aimed at reducing the incidence of these invoices should be a goal of public health.
Some experiences have already started at the regional level, such as the TARGET project in the Tuscany region, in order to reduce the incidence of hip refractures in elderly of the whole regional population (12).
The role of the orthopaedic surgeon in the treatment of patients with fragility fractures is twofold: the conservative or surgical treatment of the fracture, and the prevention of further fractures, establishing diagnostic and therapeutic procedures for osteoporosis, to avoid any refractures.
Materials and methods
We report the results on the incidence of vertebral and hip refractures in patients treated for osteoporosis in the postoperative after surgical treatment for hip or vertebral fracture at the Orthopaedics and Traumatology Hospital S.M. Annunziata of Florence in 2009–2010.
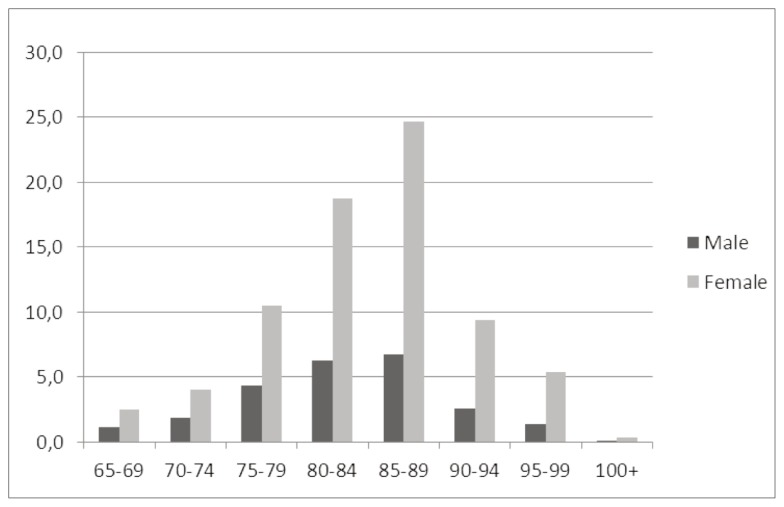
Patients treated for vertebral fragility fracture were 72 (50 females and 22 males) (Figure 1).
Figure 1.
Vertebral fractures patients distribution for sex and age.
Patients with hip fracture were 801. The males were 24.6% (197 patients) and females 75.4% (604 patients) (Figure 2).
Figure 2.
Hip fractures patients distribution for sex and age.
The average age at surgery of patients with vertebral fracture was 76.6 years (min. 63.7, max 90.3).
The minimum age at surgery of patients with hip fractures was 65 years and the maximum age was 105 years, with 71.2% aged 75 to 89 years and 18.7% aged 90 to 99 years.
The surgical treatment of patients with vertebral fractures was Vertebroplasty (13, 14) in 40 patients (55.5%) and Kyphoplasty in 32 patients (44.5%).
The surgical treatment of patients with hip fractures was Osteosynthesis or prosthetic replacement, according to the anatomic site of the fracture.
The average follow-up was 34 months with a minimum of 24 and a maximum of 44 months.
In the postoperative we evaluated serum levels of calcium, phosphorus, creatinine, albumin, alkaline phosphatase.
All the patients received adequate supplementation with Vitamin D and Calcium.
The choice of the type of antifracture drug therapy was performed specifically for each patient, taking into account also the expected “compliance” of the patient in relation to his state of general health, its cognitive status and presence of “care-givers”.
Therefore, a general assessment of the patient was carried out by means of specific tests, in order to investigate the level of autonomy (Barthel Index), cognitive status (MMSE), co-morbidity preceding the fall, the cause of fall and fracture.
Our patients with vertebral fracture were mainly aged less than or equal to 75 years with functional level prior to fracture of mild grade, with a clinical complexity before admission around 40%.
Our patients with hip fractures in the 86% of cases were elder than 75 years.
The clinical complexity at admission of patients with hip fracture was 70%. The comorbidity was present in 76% of patients. The percentage of cognitive disorder at admission was of 35%.
If a patient was in good psychophysical condition, even aged greater than or equal to 70 years, an oral therapy was prescribed, unless, for clinical needs, either an infusion or an injection therapy was necessary. Instead, in patient very old or in poor physical conditions, for which it was possible to foresee a compliance not adequate to ensure the effectiveness of the treatment, it was considered the possibility of an infusion therapy at excellence centers.
Clinical and radiographic evaluation was performed to every patient at 1, 6 and 12 month after surgical treatment.
Results
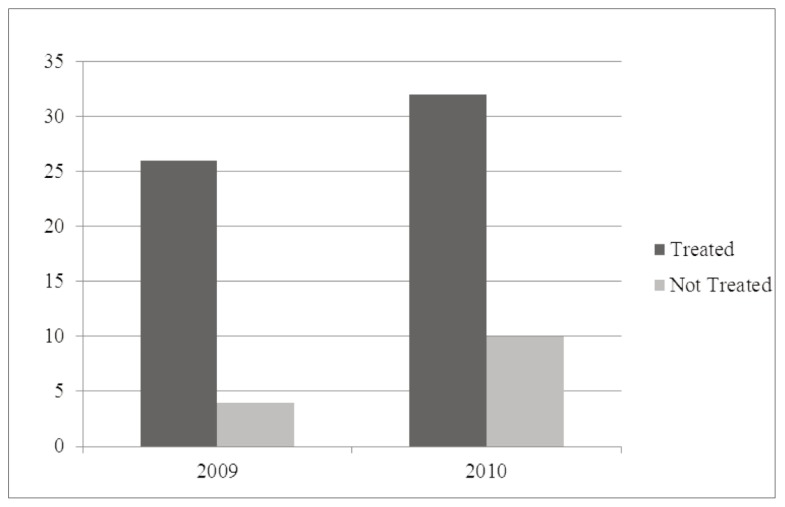
The patients with vertebral fracture treated for refractures prevention in postoperative were 58 (80.6%) (Figure 3).
Figure 3.
Patients with vertebral fracture treated for osteoporosis in postoperative for year.
The patients with hip fracture treated for refractures prevention were 307 (38.3%), 117 (28.8%) in 2009 and 190 (47%) in 2010 (Figure 4).
Figure 4.
Patients with hip fracture treated for osteoporosis in postoperative for year.
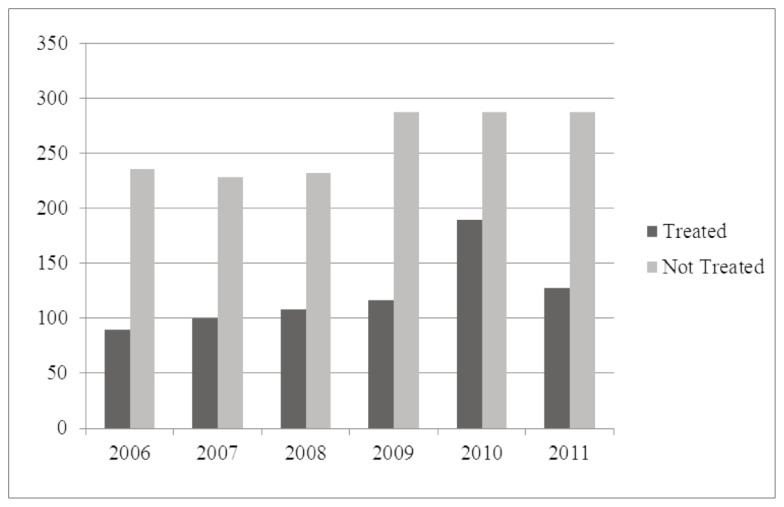
According to official data of the Region of Tuscany, between 2005 and 2007 the number of elderly people who followed therapy for osteoporosis decreased from 13.1% to 12.0% (average regional) and in 2010 a regional average was 24% about (equal to 1605 patients treated), thanks to the start of a Regional project for refracture prevention (TARGET project)
The percentage of refracture in the first two years after surgery in patients surgically treated for vertebral fracture was about 16.6% (12 patients), of which 9 patients not treated for osteoporosis (Table 1).
Table 1.
Percentage of refracture in two years after surgery in patients surgically treated for vertebral fracture.
| TREATED | NOT TREATED | |
|---|---|---|
| Refracture | 3 | 9 |
| Total Patients | 58 | 14 |
| % | 5.2% | 64.3% |
A percentage of refracture of about 70% was observed in patients with vertebral fracture that don’t treated for osteoporosis (14 patients).
The percentage of refracture at 1 year after surgery in patients surgically treated for hip fracture was 3.19% for patients operated in 2009, and 2.17% for patients operated in 2010, compared with 5.23% for patients operated in 2006, year before the beginning of the refracture prevention project (Table 2).
Table 2.
Percentage of refracture at one year after surgery in patients surgically treated for hip fracture.
| Hip Fractures | % refracture at one year | |
|---|---|---|
| 2006 | 325 | 5.23% |
| 2009 | 376 | 3.19% |
| 2010 | 326 | 2.17% |
The mortality in patients with hip fracture, in 2010 was 8% within 1 month after surgery, while the mortality within 1 year was of 19%. This percentage is 25–31% in the elderly with hip fracture who do not treated for osteoporosis.
Conclusion
The present study demonstrates that an adequate treatment for osteoporosis of the patients with bone fragility is very important in reducing the refractures.
This represents an enormous challenge for all those who in future will be engaged to deal with an increasing number of patients with osteoporotic fractures.
It is essential that the orthopedic surgeon establish a diagnostic and therapeutic process for osteoporosis, which goal is the prevention of further fractures.
It is desirable, therefore, that the role of the orthopedic surgeon shall be active both in conservative or surgical treatment of the fracture, and in the management of patients with bone fragility; this in order to reduce the risk of subsequent fractures and improve functional long-term outcome arresting the downward spiral of health and quality of life of the patient, and at the same time bring economic benefits to the community.
References
- 1.Piscitelli P, Iolascon G, et al. Incidence and costs of hip fractures vs. acute myocardial infarction in the Italian population: a 4 years survey. Osteoporos Int. 2007;18:211–219. doi: 10.1007/s00198-006-0224-9. [DOI] [PubMed] [Google Scholar]
- 2.Piscitelli P, Tarantino U, et al. Updated incidence rates of fragility fractures in Italy. Clinical Cases in Mineral Bone Metabolism. 2011;8(3):54–61. [PMC free article] [PubMed] [Google Scholar]
- 3.Riggs BL, Melton LJ., 3rd The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone. 1995;17(5 supp):505S–511S. doi: 10.1016/8756-3282(95)00258-4. [DOI] [PubMed] [Google Scholar]
- 4.Kanis JA, Burlet N, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2008;19(4):399–428. doi: 10.1007/s00198-008-0560-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piscitelli P, Brandi ML, et al. The incidence of hip, forearm, humeral, ankle, and vertebral fragility fractures in Italy: results from a 3-year multi-center study. Arthritis Res. & Therapy. 2010;12:R226. doi: 10.1186/ar3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lindsay R, Silverman SL, et al. Risk of new vertebral fractures in the year following a fracture. JAMA. 2001;285:320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 7.Husserius R, Karlsson MK, et al. Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a ten-year population-based study in 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int. 2003;14:61–68. doi: 10.1007/s00198-002-1316-9. [DOI] [PubMed] [Google Scholar]
- 8.Ismail AA, O’Neill TV, et al. Mortality associated with vertebral deformity in men and women: results from the European Prospective Osteoporosis Study (EPOS) Osteoporos Int. 1998;8:291–297. doi: 10.1007/s001980050067. [DOI] [PubMed] [Google Scholar]
- 9.Vuochteloo AJ, Borger van der Burg BL, et al. Controlateral hip fractures and other osteoporosis related fractures in hip fracture patients: incidence and risk factors. An observational cohort study of 1,299 patients. Arch Orthop Trauma Surg. 2012;132:1191–1197. doi: 10.1007/s00402-012-1520-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lindsay R, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285:320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 11.Tarantino U, et al. The diagnosis and treatment of osteoporosis and the predictors receiving pharmacological therapy: our experience in the Italian population. ASBMR. 2009 [Google Scholar]
- 12.Piscitelli P, Parri S, Brandi ML. Antifracture drug consumption in Tuscany Region before the Target Proiect: a valuable model for the analysis of administrative database. Clinical Cases in Mineral and Bone Metabolism. 2012;9(2):76–79. [PMC free article] [PubMed] [Google Scholar]
- 13.Garfin SR, Buckley RA, Ledlie J. Balloon kyphoplasty for symptomatic vertebral body compression fractures results in rapid, significant, and sustained improvements in back pain, function, and quality of life for elderly patients. Spine. 2006;31(19):2213–20. doi: 10.1097/01.brs.0000232803.71640.ba. [DOI] [PubMed] [Google Scholar]
- 14.Ettinger B, Black DM, Mitlak BH, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene. Result from a 3 year randomized clinical trial. JAMA. 1999;282:637–645. doi: 10.1001/jama.282.7.637. [DOI] [PubMed] [Google Scholar]
- 15.Piscitelli P, Brandi ML, Nuti R, Rizzuti C, et al. The Target project in Tuscany: the first disease management model of regional project for the prevention of hip refractures in the elderly. Clinical Cases in Mineral Bone Metabolism. 2010;7(3):251–254. [PMC free article] [PubMed] [Google Scholar]
- 16.Piscitelli P, Tarantino U, et al. Updated incidence rates of fragility fractures in Italy. Clinical Cases in Mineral Bone Metabolism. 2011;8(3):54–61. [PMC free article] [PubMed] [Google Scholar]
- 17.Brandi ML. Evaluation of fracture risk and fracture prevention: an Italian picture. Clinical Cases in Mineral Bone Metabolism. 2012;9(2):73–75. [PMC free article] [PubMed] [Google Scholar]
- 18.Piscitelli P, Brandi ML, et al. Epidemiology of fragility fractures in Italy. Clinical Cases in Mineral Bone Metabolism. 2011;8:29–34. [PMC free article] [PubMed] [Google Scholar]
- 19.Piscitelli P, Gimigliano F, et al. Hip fractures in Italy: 2000–2005 extension study. Osteoporos Int. 2010;21:1223–1230. doi: 10.1007/s00198-009-1084-x. [DOI] [PubMed] [Google Scholar]
- 20.Piscitelli P, Marcucci G, Parri S, et al. Compliance to antifracture treatments in Tuscany: a regional survey based on institutional pharmaceutical dataset. Clinical Cases in Mineral Bone Metabolism. 2011;8:62–65. [PMC free article] [PubMed] [Google Scholar]
- 21.Ciaschini PM, Straus SE, et al. Community based intervention to optimize osteoporosis management: randomized controlled trial. BMC Geriatrics. 2010;10:60–66. doi: 10.1186/1471-2318-10-60. [DOI] [PMC free article] [PubMed] [Google Scholar]