Summary
Operative removal of impacted mandibular third molars is a common and not riskless surgical procedure. We present an emblematic case of an osteoma closely associated with an impacted third left mandibular molar treated by Mectron Piezosurgery medical ultrasonic device.
Keywords: tooth retention, osteoma, piezoelectric bone surgery
Introduction
Removal of third molars is one of the most frequently carried out procedures in oral surgery (1, 2). Common complications following third molar surgery include: sensory nerve damage, alveolitis, infection, hemorrhage during or after surgery (3–5). Less common complications are: severe trismus, iatrogenic damage to the adjacent second molar and iatrogenic mandibular fracture (3, 5). The incidence of inferior alveolar nerve injury varies from 0.41% to 8.1% for temporary lack of sensation and 0.014 % to 3.6% for prolonged signs and symptoms. When the radiologic markers of proximity of the inferior alveolar nerve canal to the root of the third molars are present, the incidence of damage can be as high as 35% (6–8). Risk factors also include advanced age and difficult operation (9, 10). Renton and McGurk reported that the incidence of temporary and permanent lingual nerve injury is 1 and 0.3%, respectively (11). The surgical skill (i.e. lingual plate perforation utilizing bone removal with burs or chisels), the surgical technique (i.e. elevation of a lingual mucoperiosteal flap) and the difficulty of the extraction are considered to be the strongest risk factors of lingual nerve injury. Surgical difficulty is associated with deeply impacted teeth particularly if distal bone removal is required.
Osteomas are benign osteogenic tumors relatively rare in the jaws, characterized by the proliferation of compact and/or cancellous bone tissue. The osteomas can be divided into the peripheral-type (periosteal-type) or central-type (endosteal-type). Peripheral osteomas are masses adhering the cortical surface, while central lesions arise from endosteal bone surface. Radiographically osteomas appears as well-circumscribed sclerotic radiopaque masses (12).
Histologically they consist of either dense compact bone with sparse marrow spaces or lamellar trabeculae of cancellous bone with fibrofatty marrow spaces. Osteoblastic activity is often predominant (12). In the mandible, common affected regions include the lingual side of the premolars, the inferior border of the chin, and the interior and lateral regions of the mandibular angle (13, 14).
The preoperative diagnosis is radiological, with the panoramic radiograph as first level examination followed by CT (computed tomography)/CBCT (cone beam computed tomography) scan.
The therapeutic approach is surgical with careful removal of the lesion and curettage of the adjacent tissue. The prognosis is extremely favorable since the recurrence is not expected (15).
Piezoelectric surgery has during the last decade been used in oral and maxillo-facial surgery, ENT surgery, orthopedic surgery, hand surgery and neurosurgery to perform odontectomies, osteotomies and osteoplasties (16). The main feature of piezoelectric surgery is the selective cut which consists into cutting only hard tissue sparing soft tissue structures included nerve tissue. The instruments used for ultrasonic cutting create microvibrations caused by the piezoelectric effect: certain ceramics and crystal deform when an electric current is passed across them, resulting in oscillations of ultrasonic frequency. The used frequency is in the 20–32 kHz range and creates micromovements ranging between 60 to 210 μm that cut only mineralized tissue while soft tissue is cut at frequencies higher than 50 kHz. The amplitude of these microvibrations permits a clean, precise cut. In addition the operative site is blood-free due to the action of the saline solution and cavitation. The cavitation assists in closing the smallest blood vessels and rinses away any blood from the larger vessels.
We present an emblematic case of a deeply located osteoma all-surrounding an impacted left mandibular third molar treated by Mectron Piezosurgery medical ultrasonic device.
Case report
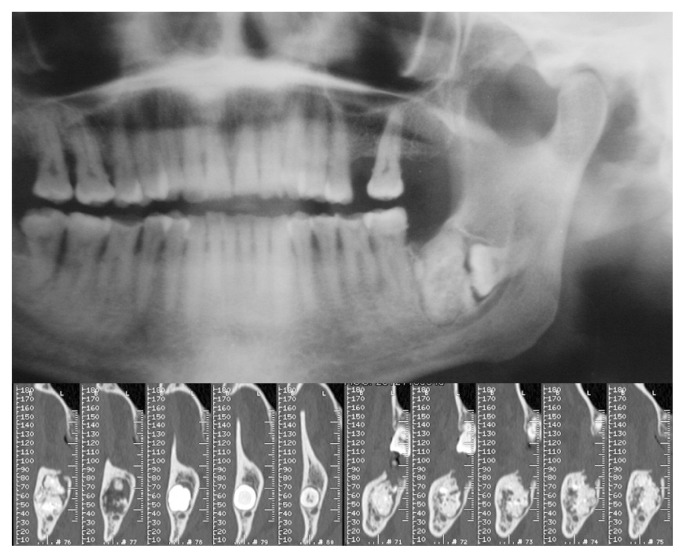
A 39-year-old woman was referred to the Department of Oral and Maxillofacial Surgery, Second University of Naples for the accidental finding of a radiopaque mass in the mandibular left third molar region. Clinical examination showed a non-pathological condition in the posterior mandibular left side except for decayed first molar, the third molar was totally impacted whereas other mandibular permanent teeth were perfectly formed and well arranged; there were no deformations or swelling of the region. The panoramic radiograph (Figure 1) showed an oval-shaped radiopaque mass with well defined margins closely associated with the crown of the unerupted mandibular molar; the provisional diagnosis was osteoma-like lesion. CBCT scan was obtained in order to precisely define extension of the lesion and regional anatomical topography and showed an intimate relationship between the inferior alveolar nerve and the osteoma-tooth unit with the nerve canal directly apical to the lesion and lingual to the third molar; on the bucco-lingual aspect, the lesion appeared to be casted into the lingual bone plate which was thinner in the area (Figure 1).
Figure 1.
Appearance of the lesion at panoramic radiograph and CBCT examination.
Surgical removal of the lesion together with the extraction of the impacted third molar and curettage of the area was planned. After local anaesthesia a mucosal incision along the anterior part of the mandibular ramus was intrasulculary extended to the mesial region of the first molar and buccal bone plate in the third molar region was exposed. Osteotomy was performed at the interface between bone and lesion on the mesial, buccal, distal, and lingual aspect using the MT1-10 insert of the Mectron Piezosurgery medical ultrasonic device in a continuous gentle upward-downward or forward-backward movements of the vibrating tip, extreme attention was paid in order to preserve the bony peak distal to the second molar; the lesion was successively fragmented and removed using a curved luxating elevator (Figure 2), extraction of the third molar was easily performed by using the same device. Wound surgical toilette and closure with plain 3.0 Vicryl® were performed. No intraoperative complications occurred. On macroscopic examination the mass appeared to be an osteoma-like lesion, the extraction socket was normal and the alveolar nerve canal was detectable at the bottom of the alveolus. The mass was processed for histopathological examination, which confirmed the diagnosis of osteoma. Immediate postoperative wound healing was satisfactory, radiological check up was obtained ten days postoperatively (Figure 3) and at one year follow-up the patient was totally asymptomatic and the area of interest appeared to be healed in a satisfactory way both at clinical and radiological examination. No symptoms or signs of neurosensory impairment to the innervated area neither of the inferior alveolar nerve or the lingual nerve could be detected.
Figure 2.
Intraoperative appearance of the surgical field after removal of the lesion.
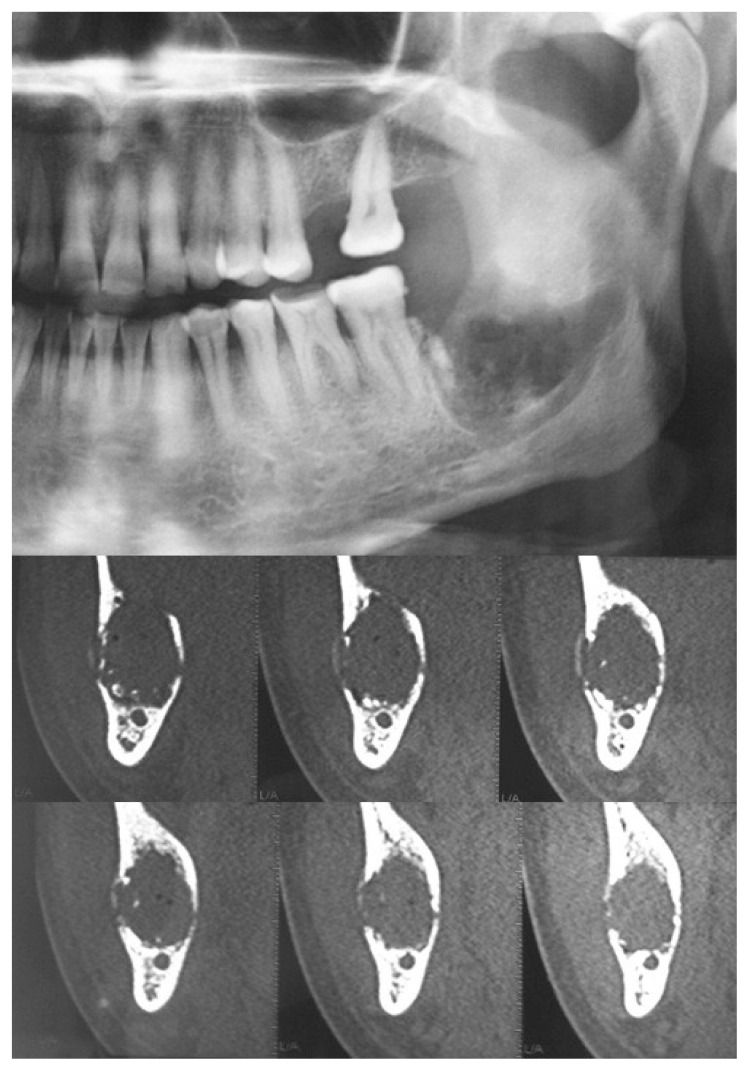
Figure 3.
Panoramic radiograph and CBCT examination taken ten days after surgery.
Discussion
The present case showed a relatively large osteoma that occurred in the mandibular third molar region of a 39 year-old woman associated with an impacted third molar. The lesion was in intimate relationship with inferior alveolar nerve canal and lingual cortical bone plate. When it comes to the occurrence of complications related to third molar extraction, surgical technique seems to play a major role (17). Thus, a careful operating technique and adequate instruments may limit complications occurrence. In the present case removal of the lesion-tooth unit was carried out by using piezoelectric surgery device with the main intent to reduce risk for lingual and inferior alveolar nerve damage and peri-postoperative hemorrhage. Piezoelectric bone surgery is a tissue-selective technique that allows a micrometric, exact and smooth cut into mineralized tissue, while adjacent soft tissue such as nerves, vessels, periosteum or schneiderian membrane, when the ultrasonic device is correctly used, remain unharmed because surgical action ceases when the device tips come in contact with non-mineralized tissue (18, 19). An in vitro study concerning inferior alveolar nerve transposition by piezoelectric surgery showed that after surgery the epineurium became roughened without any damage to the deeper structures (20). Comparing with traditional surgery carried out by using conventional burs or chisels, ultrasonic cutting precision and selectivity have undoubtedly to be considered important advantages particularly in such cases where the surgery target is in close relationship with noble soft tissue structures. As a result, even less experienced, though properly trained, surgeons can perform such a kind of surgery, being the learning curve with ultrasonic surgery technique dramatically reduced comparing to traditional surgery with rotating instruments (19). Nevertheless, a careful surgical approach remains critical considering that soft tissue can be damaged by excessive mechanical force while using the device.
An additional consideration regarding ultrasonic surgery is its favorable role in surgical wound healing because the less invasive cutting action produce minor tissue damage and consequently better healing. Besides, when compared with traditional surgery, bone healing following piezoelectric surgery seems to be either similar (21) or even improved due to the fact that piezoelectric bone surgery seems to induce an earlier increase in neo-osteogenesis resulting in a more favourable osseous response (22, 23). The latter may depend on the cavitation effect induced by ultrasonic cutting that allows an effective cooling avoiding significant hyperthermia and coagulation damages to the surrounding area (24). The same effect is responsible for a higher visibility during surgery compared to conventional instruments due to the evacuation of detritus with the aerosol formation (18). In the present case the assessment of wound healing and neurosensory function of the inferior alveolar nerve and of the lingual nerve in the immediate postoperative period and at one year follow up was totally satisfactory. Besides, when compared to surgery performed by using traditional rotation instruments, it is reasonable to speculate that the surgical trauma was markedly reduced in this case due to the intrinsic features of the Piezoelectric device, as described above, in conjunction to the specific morphology of the device inserts. We therefore promote the use of Piezoelectric device in surgical cases where risk for noble soft tissue damage is high. In particular, the issue of inferior alveolar nerve injury during the removal of lower third molars is a well known clinical and medico-legal problem so any technique that can reduce the possibility of this damage is worthy of exploration.
References
- 1.Woldenberg Y, Gatot I, Bodner L. Iatrogenic mandibular fracture associated with third molar removal. Can it be prevented? Med Oral Patol Oral Cir Bucal. 2007;12:E70–2. [PubMed] [Google Scholar]
- 2.Visintini E, Angerame D, Costantinides F, Maglione M. Peripheral neurological damage following lower third molar removal. A preliminary clinical study. Minerva Stomatol. 2007;56:319–26. [PubMed] [Google Scholar]
- 3.Sisk AL, Hammer WB, Shelton DW, Joy ED., Jr Complications following removal of impacted third molars: the role of the experience of the surgeon. J Oral Maxillofac Surg. 1986 Nov;44(11):855–9. doi: 10.1016/0278-2391(86)90221-1. [DOI] [PubMed] [Google Scholar]
- 4.Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003 Dec;61(12):1379–89. doi: 10.1016/j.joms.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Lopes V, Mumenya R, Feinmann C, Harris M. Third molar surgery: an audit of the indications for surgery, post-operative complaints and patient satisfaction. Br J Oral Maxillofac Surg. 1995 Feb;33(1):33–5. doi: 10.1016/0266-4356(95)90083-7. [DOI] [PubMed] [Google Scholar]
- 6.O’Riordan BC. Coronectomy (intentional partial odontectomy of lower third molars) Oral Surg Oral Med Oral Pathol. 2004 Sep;98(3):274–80. doi: 10.1016/S1079210404000496. [DOI] [PubMed] [Google Scholar]
- 7.Ziccardi VB, Zuniga JR. Nerve injuries after third molar removal. Oral Maxillofac Surg Clin North Am. 2007;19:105–15. doi: 10.1016/j.coms.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Tay AB, Go WS. Effect of exposed inferior alveolar neurovascular bundle during surgical removal of impacted lower third molars. J Oral Maxillofac Surg. 2004;62:592–600. doi: 10.1016/j.joms.2003.08.033. [DOI] [PubMed] [Google Scholar]
- 9.Howe GL, Poyton HG. Prevention of damage to the inferior dental nerve during the extraction of mandibular third molars. Br Dent J. 1960;109:355–63. [Google Scholar]
- 10.Rud J. Third molar surgery: relationship of root to mandibular canal and injuries to inferior dental nerve. Tandlaegebladet. 1983;87:619–31. [PubMed] [Google Scholar]
- 11.Renton T, McGurk M. Evaluation of factors predictive of lingual nerve injury in third molar surgery. Br J Oral Maxillofac Surg. 2001 Dec;39(6):423–5. doi: 10.1054/bjom.2001.0682. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan I, Calderon S, Buchner A. Peripheral osteoma of the mandible: a study of 10 new cases and analysis of the literature. J Oral Maxillofac Surg. 1994;52:467–70. doi: 10.1016/0278-2391(94)90342-5. [DOI] [PubMed] [Google Scholar]
- 13.Takeuchi Y, Kobayasi A, Shibuya T, Tachibana T, Takagi M, Amagasa T. A case of relatively large peripheral osteoma at the inferior border of the mandible. J Jpn Stomatol Soc. 2004;53:37–40. [Google Scholar]
- 14.Sugiyama T, Jinbu Y, Ikeda K, Itoh H, Kusama M, Tsukinoki K. A case of peripheral osteoma of the inferior border of the mandible. Jpn J Oral Maxillofac Surg. 2009;55:194. [Google Scholar]
- 15.Johann A, de Freitas J, Aguiar M, de Arujo N, Mesquita R. Peripheral osteoma of the mandible. Case report and review of the literature. J Cranio Maxillofacial Surg. 2005;33:276–281. doi: 10.1016/j.jcms.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 16.Labanca M, Azzola F, Vinci R, Rodella LF. Piezoelectric surgery: Twenty years of use. Br J Oral Maxillofac Surg. 2008;46:265–269. doi: 10.1016/j.bjoms.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 17.Brann CR, Brickley MR, Shepherd JP. Factors influencing nerve damage during lower third molar surgery. Br Dent J. 1999 May 22;186(10):514–6. doi: 10.1038/sj.bdj.4800155. [DOI] [PubMed] [Google Scholar]
- 18.Barone A, Santini S, Marconcini S, Giacomelli L, Gherlone E, Covani U. Osteotomy and membrane elevation during the maxillary sinus augmentation procedure. A comparative study: piezoelectric device vs. conventional rotative instruments. Clin Oral Impl Res. 2008;19:511–5. doi: 10.1111/j.1600-0501.2007.01498.x. [DOI] [PubMed] [Google Scholar]
- 19.Schlee M, Steigmann M, Bratu E, Garg AK. Piezosurgery: Basics and Possibilities. Impl Dent. 2006;15(4):334–40. doi: 10.1097/01.id.0000247859.86693.ef. [DOI] [PubMed] [Google Scholar]
- 20.Sakkas N, Otten JE, Gutwald R, Schmelzeisen R. Transposition of the mental nerve by piezosurgery followed by postoperative neurosensory control: A case report. Br J Oral Maxillofac Surg. 2008;46:270–1. doi: 10.1016/j.bjoms.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 21.Chiriac G, Herten M, Schwarz F, Rothamel D, Becker J. Autogenous bone chips:influence of a new piezoelectric device (Piezosurgery) on chip morphology, cell viability and differentiation. J Clin Periodontol. 2005;32:994–9. doi: 10.1111/j.1600-051X.2005.00809.x. [DOI] [PubMed] [Google Scholar]
- 22.Preti G, Martinasso G, Peirone B, et al. Cytokines and growth factors involved in the osseointegration of oral titanium implants positioned using piezoelectric bone surgery versus a drill technique: a pilot study in minipigs. J Periodontol. 2007;78:716–22. doi: 10.1902/jop.2007.060285. [DOI] [PubMed] [Google Scholar]
- 23.Vercellotti T, Kim DM, Wada K, Fiorellini JP. Osseous response following resective therapy with piezosurgery. Int J Periodontics Restorative Dent. 2005;25:543–9. [PubMed] [Google Scholar]
- 24.Emam TA, Cuschieri A. How safe is high-power ultrasonic dissection? Ann Surg. 2003;237:186–191. doi: 10.1097/01.SLA.0000048454.11276.62. [DOI] [PMC free article] [PubMed] [Google Scholar]