Abstract
INTRODUCTION
Hydatid cyst of bone constitutes only 0.5-2% of all hydatidoses. The thoracic spine is the most common site of spinal hydatidoses. Primary hydatid cyst of the sacral spinal canal is rare.
PRESENTATION OF CASE
A 19-year-old man had cauda equina syndrome with pelvic pain 15 days ago, the pelvic radiography shows a lytic image depend on the left sacral wing. MRI showed an intra-pelvic cystic image invading the sacrum T1 hypointense and T2W hyperintense. The Hydatid serology was positive.Surgical treatment consisted of a wide drainage of hydatid cavity dug in the left sacral wing, and by which it communicated intra pelvic, with removal of the entire cyst by gentle aspiration, abundant rinsing with hypertonic saline, release and sacred roots encompassed in a puddle of fibrosis hydatid.The evolution was good with recovery of perineal sensation and anal tone. The sacroiliac joint was considered stable and did not require synthesis or reconstruction.
DISCUSSION
Hydatid cysts predominantly occur in liver and lungs. Involvement of other organs is uncommon. Neither surgery nor medical therapy is generally effective for bone, especially spinal hydatidosis. The initial treatment of choice is surgical excision for neural decompression and establishing diagnosis. Albendazole is the drug of choice against this disease, when suspected, presurgical use of Albendazole in Echinococcus infestations reduces risk of recurrence and/or facilitates surgery by reducing intracystic pressure.
CONCLUSION
A missed diagnosis of hydatid cyst could be devastating. Hence, hydatid cyst should be kept as a differential diagnosis, when encountered with a cystic lesion of sacrum. In addition, longterm follow-up is mandatory as recurrence is high despite use scolicidal agents.
Keywords: Hydatid cyst, Sacral, Surgery
1. Introduction
Hydatic cysts are caused by Echinococcus granulosus, his commonest site is liver and lungs. Skeletal hydatidoses occurs in 0.5–2% cases, half of which infest the spine.1–3 The commonest site is thoracic and sacral involvement is rare.2 We report a case of sacral hydatic cyst revealed by a cauda equina syndrome.
2. Case report
A man aged 19 years presented with cauda equine syndrome with pelvic pain 15 days ago, the pelvic radiography shows a lytic image depend on the left sacral wing (Fig. 1). We complete by an MRI which showed intra-pelvic cystic picture invading the sacrum, hypointense on T1 sequence and hyperintense on T2 sequence (Fig. 2). Hydatic cyst of bone was suspected and we completed by an hydatid serology that confirmed the diagnosis. Surgical treatment consisted on a wide drainage of hydatid cavity dug in the left sacral wing by a posterior surgical approach, with removal of the entire cyst by gentle aspiration associated to an abundant rinsing of soft tissue and cysts with hypertonic saline, after verifying that there was no opening of the dura. The sacred roots were encompassed in a puddle of fibrosis hydatid and their release was too difficult. The sacroiliac joint was considered stable and did not require synthesis or reconstruction. Subcutaneous drainage was maintained for 6 days due to persistent discharge. Two weeks after surgery, the evolution was good with recovery of perineal sensation and anal tone. The patient was put on long-term Albendazole treatment, with a regular physical reeducation program. After 8 months of follow-up, our patient has a steady neurological state with a new MRI showing no recurrence of hydatid cyst (Figs. 3 and 4).
Fig. 1.

Lytic image depend on the left sacral wing.
Fig. 2.
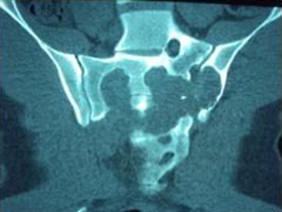
CT lytic image on the left sacral wing.
Fig. 3.

MRI: intra-pelvic cystic image invading the sacrum.
Fig. 4.

A wide drainage of hydatid cavity dug in the left sacral wing with release sacred roots encompassed in a puddle of fibrosis hydatid.
3. Discussion
Hydatid cysts predominantly occur in liver and lungs. Involvement of other organs is uncommon. Skeletal involvement occurs in 0.5–2% of all cases, half of which are in the spine.1–4 A neurosurgeon encounters hydatid cyst in brain and spine. Hydatid cyst of brain is more common than spine. In a series of 29 cases of intracranial and spinal hydatid cyst, no sacral lesion was seen.5 In a series of 25 cases of vertebral hydatidosis the cyst was located in the cervical vertebrae in three, the thoracic vertebrae in 11, the lumbar in five, and the sacrum in six cases.6 In another series of 13 cases of vertebral hydatidosis, sacrum was involved in only one case.7 Approximately 90% of spinal hydatidosis cases are located extradurally, most commonly in the vertebral body. Intradural location is very rare and appears like an arachnoid cyst.8
As there is no host reaction the cyst can grow to enormous size and remain asymptomatic. The initial symptom is back pain when cyst invades spinal canal after erosion of bony cortex. As whole vertebral body is destroyed, gibbous deformity does not result. The neurological symptoms are those of extradural tumor or disc disease.1
Hydatid disease of sacrum is not easily detected. In two cases report, sacral hydatid cyst was not suspected and the symptoms were considered due to lumbar disc disease. In the first case, the diagnosis was delayed up to 12 years as pelvis was not imagined, which could have shown a cystic lesion in presacral space.9 In the second case, a small cystic lesion was presumed as tarlov's cyst.
The other differential diagnosis of cystic lesion of sacrum includes developmental cysts (epidermoid, dermoid, teratoma, neurenteric and retrorectal cystic hamartoma) anterior sacral meningocele, necrotic sacral chordoma, schwannoma, arachnoid cyst, and anevrysmal bone cyst.
Neither surgery nor medical therapy is generally effective for bone, especially spinal hydatidosis. The initial treatment of choice is surgical excision for neural decompression and establishing diagnosis. After excision local scolicidal agents like hypertonic saline or certimide should be used for irrigation instead for formalin. Inadvertent opening of dura can lead to intradural recurrence and spillage local scolicidal agent; in one case, death occurred due to toxic myelitis and respiratory arrest from intradural spillage of formalin.7 Patient may require stabilization after extensive resection. Subcutaneous drainage for prolonged period after surgery is advised due to persistent discharge.
Albendazole is the drug of choice against this disease, when suspected, presurgical use of Albendazole in Echinococcus infestations reduces risk of recurrence and/or facilitates surgery by reducing intracystic pressure.10 Though it is a benign disease, due to frequent recurrences and dissemination, the behavior is of malignancy. The overall recurrence rate is 30–40%. When recurrence occurs, repeat excision should be attempted if feasible.
4. Conclusion
A missed diagnosis of hydatid cyst could be devastating. Hence, hydatid cyst should be kept as a differential diagnosis, when encountered with a cystic lesion of sacrum. In addition, long-term follow-up is mandatory as recurrence is high despite use scolicidal agents.
Conflict of interest
Nil.
Funding
None.
Ethical approval
Approval has been given by the patient.
Author contributions
Kherfani Abdelhakim and Mestiri Mondher contributed in writing the paper. Bouhali Haroune and Amri Khalil contributed in the data collection. Marzouk Oubaid contributed in study concept.
References
- 1.Abbassioun K., Amirjamshidi A. Diagnosis and management of hydatid cyst of the central nervous system: Part 2: Hydatid cysts of the skull, orbit, and spine. Neuro Quart. 2001;11:10–16. [Google Scholar]
- 2.Fiennes A.G., Thomas D.G. Combined medical and surgical treatment of spinal hydatid disease: a case report. J Neurol Neurosurg Psychiatry. 1982;45:927–931. doi: 10.1136/jnnp.45.10.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray R.O., Hddad F. Hydatid disease of the spine. J Bone Joint Surg Br. 1959;4:499–506. doi: 10.1302/0301-620X.41B3.499. [DOI] [PubMed] [Google Scholar]
- 4.Sapkas G.S., Machinis T.G., Chloros G.D., Fountas K.N., Themistocleous G.S., Vrettakos G. Spinal hydatid disease, a rare but existent pathological entity: case report and review of the literature. South Med J. 2006;99:178–183. doi: 10.1097/01.smj.0000199747.81684.54. [DOI] [PubMed] [Google Scholar]
- 5.Rumana M., Mahadevan A., Nayil Khurshid M., Kovoor J.M., Yasha T.C., Santosh V. Cestode parasitic infestation: intracranial and spinal hydatid disease: a clinicopathological study of 29 cases from South India. Clin Neuropathol. 2006;25:98–104. [PubMed] [Google Scholar]
- 6.Song X., Liu D., Wen H. Diagnostic pitfalls of spinal echinococcosis. J Spinal Disord Tech. 2007;20:180–185. doi: 10.1097/01.bsd.0000211288.37013.42. [DOI] [PubMed] [Google Scholar]
- 7.Işlekel S., Erşahin Y., Zileli M., Oktar N., Oner K., Ovül I. Spinal hydatid disease. Spinal Cord. 1998;36:166–170. doi: 10.1038/sj.sc.3100512. [DOI] [PubMed] [Google Scholar]
- 8.Pushparaj K., Sundararajan M., Madeswaran K., Ambalavanan S. Primary spinal intradural hydatid cyst: a short report. Neurol India. 2001;40:203–204. [PubMed] [Google Scholar]
- 9.Joshi N., Hernandez-Martinez A., Seijas-Vazquez R. Primary sacral hydatid cyst: a case report. Acta Orthop Belg. 2007;73:674–677. [PubMed] [Google Scholar]
- 10.Sharma N.K., Chitkara N., Bakshi N., Gupta P. Primary spinal extradural hydatid cyst. Neurol India. 2003;61:89–90. [PubMed] [Google Scholar]


