Abstract
Objective. To describe the education, training, and academic experiences of newly hired faculty members at US colleges and schools of pharmacy during the 2012-2013 academic year.
Methods. A survey regarding education, training, and academic experiences was conducted of all first-time faculty members at US colleges and schools of pharmacy hired during the 2012-2013 academic year.
Results. Pharmacy practice faculty members accounted for the majority (68.2%) of new hires. Ambulatory care was the most common pharmacy specialty position (29.8%). Most new faculty members had a doctor of pharmacy (PharmD) as their terminal degree (74.8%), and 88.3% of pharmacy practice faculty members completed a residency. Of new faculty members who responded to the survey, 102 (67.5%) had at least 3 prior academic teaching, precepting, or research experiences.
Conclusion. New faculty members were hired most frequently for clinical faculty positions at the assistant professor level and most frequently in the specialty of ambulatory care. Prior academic experience included precepting pharmacy students, facilitating small discussions, and guest lecturing.
Keywords: faculty member, pharmacy education, training, hiring, survey
INTRODUCTION
An increase in the number of universities with pharmacy programs along with the expansion of existing pharmacy programs have increased the demand for high-caliber faculty members for these colleges and schools. However, new faculty member characteristics, such as education, training, and academic experiences have not been reported in over 10 years. An analysis of changes in pharmacy practice faculty member demographics was conducted between the years of 1995 and 2001.1 Using the American Association of Colleges of Pharmacy (AACP) institutional research system, the study found that the pharmacy practice department had 3.8 times more faculty members than did other academic departments. The study also reported a 58% increase in nontenure-track assistant professors and only a 4% increase in tenure-track assistant professors. The article concluded that colleges and schools of pharmacy were relying heavily on nontenure-track clinical faculty members to meet the clinical education demands of the pharmacy curriculum. However, it did not analyze the education, training, and academic experience of the junior faculty members being hired.
There is no standardized hiring practice for faculty members at colleges of pharmacy. The Accreditation Council for Pharmacy Education (ACPE) released its most recent Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree in February 2011.2 Standard number 25, relating to qualitative factors of faculty and staff members, states, “The college or school must have qualified faculty and staff who, individually and collectively, are committed to its mission and goals and respect their colleagues and students. Faculty must possess the required professional and academic expertise, have contemporary knowledge and abilities in current educational philosophy.” Standard 25 also states that faculty members should have a doctoral degree appropriate to their responsibilities (either doctor of philosophy [PhD] or doctor of pharmacy [PharmD]), postdoctoral research training or residency, fellowship, or equivalent experience, and appropriate licensure. The ACPE standards provide a blueprint for faculty and staff education and training requirements but do not mandate a specific set of hiring guidelines, such as postgraduate year 2 (PGY2) residency training or equivalent experience, fellowship training, board certification, prior teaching experience, or other specific qualifications. In 2006, the American College of Clinical Pharmacy published a position statement recommending at least a PGY2 residency, or equivalent experience for any pharmacist looking to obtain a pharmacy practice faculty position.3 One study reported that 50% of faculty members surveyed agreed with the American College of Clinical Pharmacy recommendations that a 2-year residency was appropriate for a full-time assistant professor position, whereas 35% disagreed with this recommendation.4 There is clearly a difference in hiring practices and opinions relating to the hiring of pharmacy faculty members in the United States.
The primary objective of this study was to assess the education, training, and experience of new faculty members hired in US colleges and schools of pharmacy during the 2012-2013 academic year. The authors set out to answer 3 distinct questions. (1) With the changing landscape of pharmacy education, what type of positions are being hired? (2) What education, training and academic experience did these new faculty members have prior to starting their faculty roles? and (3)What were the most important factors that led these new faculty members to pursue an academic career? We believe this research will benefit both US colleges and schools of pharmacy as well as potential faculty candidates. These data will provide a benchmark for pharmacy colleges and schools to compare the type of faculty members they currently hire with national statistics. For potential future faculty candidates, these data will provide a perspective on how their education, training, and experience compared to that of recently hired faculty peers.
METHODS
According to the AACP database, 307 new, first-time, pharmacy faculty members were hired in the United States during the 2012-2013 academic year. These first-time faculty members were either prior residents, fellows, graduate students, clinicians, or researchers who had never held a faculty position at a college or school of pharmacy prior to this new appointment. A survey instrument was developed that included questions designed to capture data regarding the education, training, and prior academic experiences (teaching, service, and research) of the new faculty members. The survey instrument was beta-tested on faculty members recently hired by the study institution (n=5) and was edited and revised by members of the research team, as deemed necessary. The survey instrument included 24 questions and was estimated to take between 5-10 minutes to complete.
Permission was obtained from AACP to send the survey instrument using Qualtrics software (Qualtrics, LLC, Provo, Utah) to the 307 new, first-time faculty members listed in their database. The potential respondents received an e-mail containing an electronic letter of consent to participate in the research and a Web link to complete the survey instrument if they wished to participate. Participants were allowed 30 days to complete the survey instrument and were sent 2 additional follow-up reminders encouraging participation. Participation in the survey was completely anonymous, and participants were told that only aggregate data would be reported. Random drawings for 8 Amazon gift cards ($25 each) were used as an incentive to participate. The survey instrument was approved by the University of Houston Institutional Research Board prior to obtaining approval from AACP to distribute to new faculty members. Survey responses were tabulated by means of the Qualtrics database and exported to Microsoft Excel for data analysis. Participants were included in the data analysis if they answered at least 50% of the questions. Descriptive statistics were tabulated using Excel.
RESULTS
One hundred fifty-seven survey responses were collected over a 4-week period from April to May 2013. Six of the survey participants were excluded because they answered less than 50% of the questions, resulting in 151 completed survey instruments (49.2% of the 307 instruments distributed) eligible for inclusion in the final analysis. Seventy-one unique colleges and schools of pharmacy from 31 different states were represented in the survey. Illinois had the greatest number of new faculty respondents (12), followed by Ohio (11), Pennsylvania (11) and Texas (10). Sixteen of the 151 respondents did not indicate their pharmacy college or school.
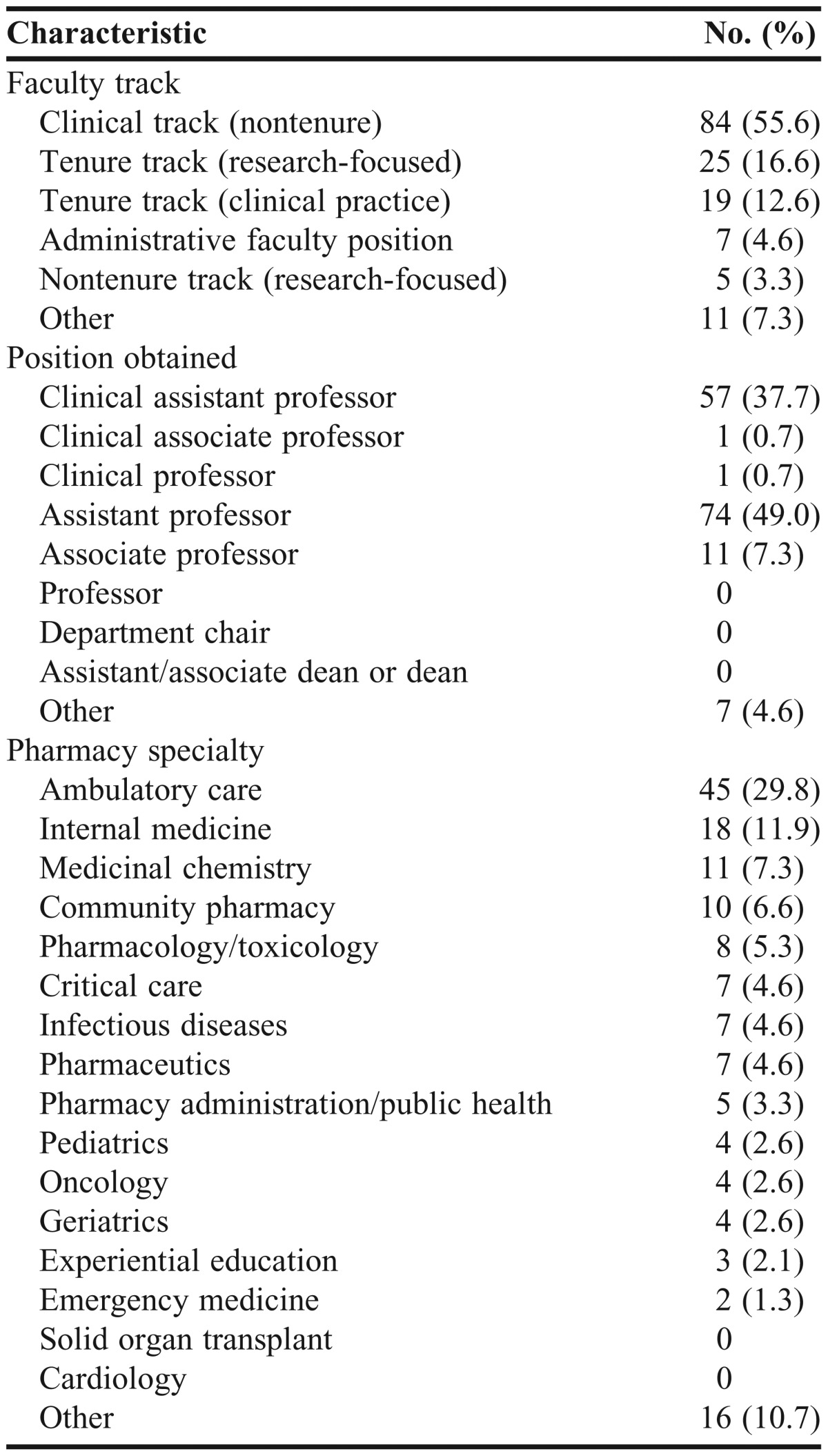
The most frequent faculty track hired was the clinical-track, nontenured position, followed by tenure-track, research-focused, and tenure-track, clinical-focused (Table 1). Administrative faculty positions comprised less than 5% of the new faculty members hired, and of the remainder fit into the “other” category. Positions in this category included visiting professors, instructors, and pharmacy residents with full-time faculty appointments. The vast majority of new faculty members were hired at the assistant-professor level. The remaining percentage of new faculty members were comprised of associate professor positions or categorized as “other.” None of the survey respondents were hired as full professors or to dean-level positions. Ambulatory care was the most frequently reported pharmacy specialty of new faculty positions, followed by internal medicine, “other” or positions that did not fall into one of the 18 categories, medicinal chemistry, and community pharmacy.
Table 1.
Characteristics of New, First-Time Pharmacy Faculty Members Hired by US Pharmacy Colleges and Schools, 2012-2013 Academic Year (n=151)
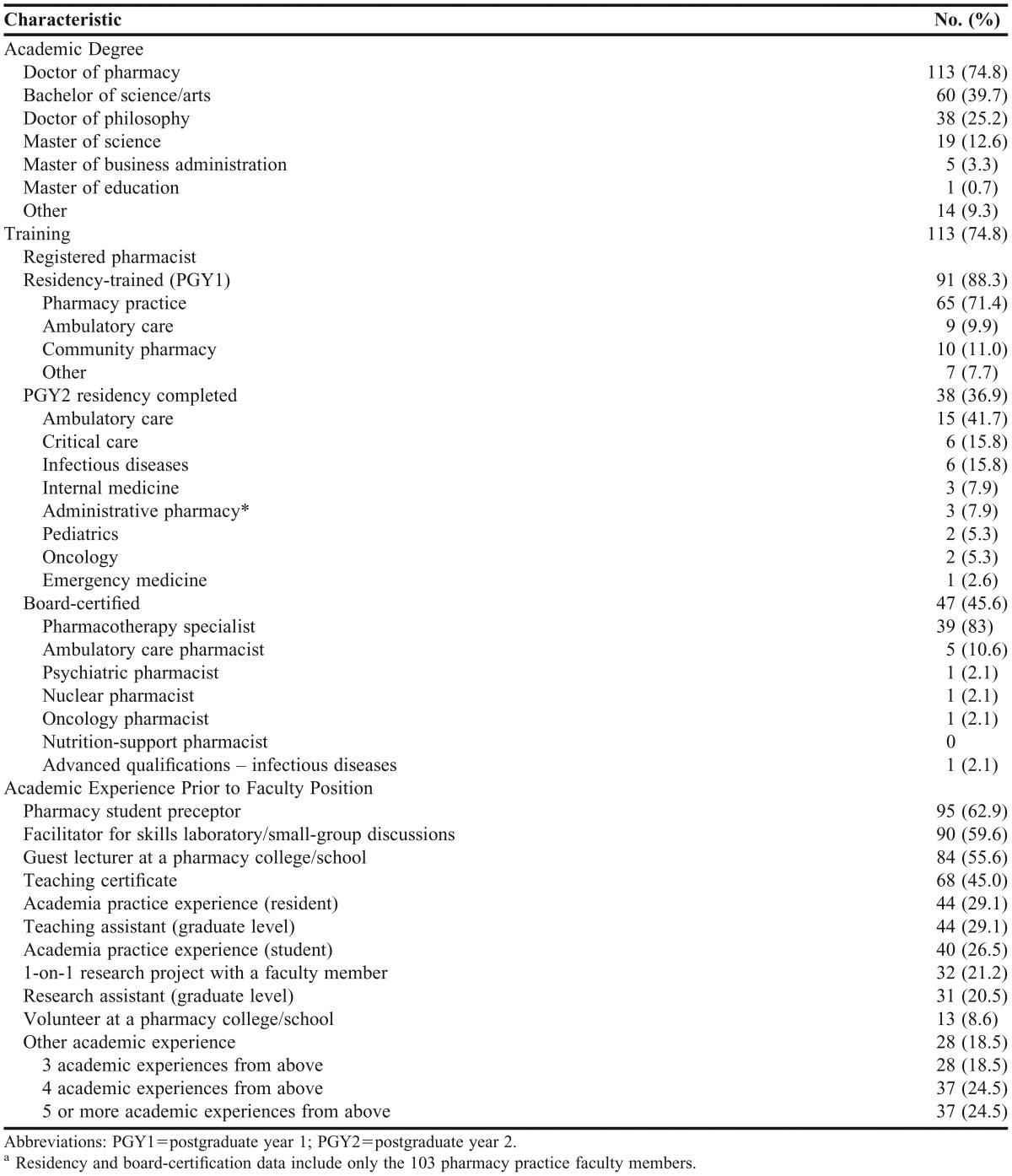
The education, training, and academic experience of new faculty members varied widely among respondents (Table 2). The most common degree among new faculty members was the PharmD degree. Sixty new faculty members had a bachelor of science or arts, and 38 had doctor of philosophy degrees. Three-fourths of the new faculty members were registered pharmacists; however, not every respondent with a PharmD was a registered pharmacist. Of the 103 pharmacy practice faculty members, a great majority was residency trained, with pharmacy practice being the most commonly obtained postgraduate year 1 residency among new faculty members. Thirty-eight pharmacy practice faculty members also completed a PGY2 residency. The most common PGY2 residencies obtained by new faculty members were ambulatory care, followed by critical care and infectious diseases. Nearly half of the new faculty members were board-certified in a pharmacy specialty, with the majority being board-certified pharmacotherapy specialists (BCPS) (83% of all board-certified faculty members). The most common teaching experiences among new faculty members included precepting pharmacy students, acting as a facilitator for skills laboratories or small-group discussions, giving a guest lecture at a college or school of pharmacy, and completing a pharmacy-teaching training program, such as a teaching certificate program.
Table 2.
Frequency Distribution of Education, Training, and Academic Experience Among Newly Hired, First-Time Pharmacy Faculty Members During the 2012-2013 Academic Year (n=151)a
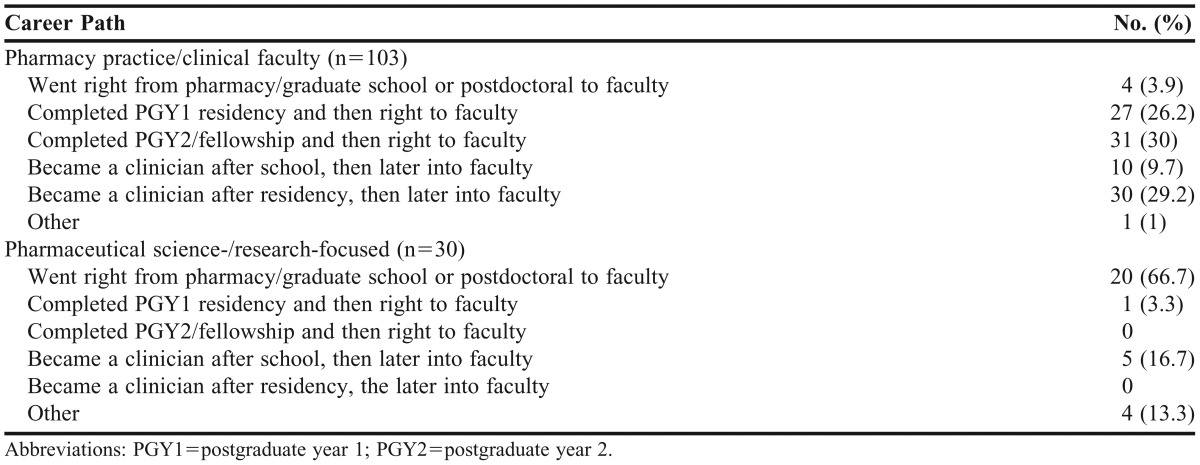
New pharmacy practice or clinical faculty members most commonly completed a PGY2 residency and then went directly into a faculty position (30%), followed by pursuing a clinical job after residency and subsequently taking a faculty position (29.2%), and going directly from postgraduate year 1 (PGY1) residency into a faculty position (26.2%) (Table 3). The 40 clinical faculty members who went into the workforce prior to their faculty positions had an average of 5.1 (±7.1) years of work experience (median, 3 years; range, 1 to 42 years). The majority of faculty members focused on pharmaceutical science or research went directly from pharmacy or graduate school or postdoctoral programs into faculty positions (66.7%). The overall mean number of years of pharmacy practice or experience prior to starting as a faculty member was 5.1±7.9 years, with a median of 3 years (range, 0 to 42 years).
Table 3.
Career Paths of Newly Hired, First-Time Pharmacy Faculty Members During the 2012-2013 Academic Year
Forty-two (40.1%) of the first-time clinical faculty members had a peer-reviewed publication. Among clinical faculty members who had published at least once, the average number of publications (either in press or already published) was 2.9±3.4 (median, 3; range, 1 to 18). For faculty members focused on pharmaceutical science/research 28 (93.3%) had at least 1 publication, with an average of 20.6±24.6 (median, 15; range, 1-108).
Eighty-one of the new clinical faculty members (78.6%) attended the 2012 ASHP Midyear Clinical Meeting in Las Vegas, NV. Thirty-seven (45.7%) of the new clinical faculty members who attended the meeting interviewed for faculty positions at the meeting. Of the 37 new clinical faculty members who had interviewed for faculty positions at the meeting, 34 (91.9%) were residents (either PGY1 or PGY2) at the time and went directly from residency into their faculty position. When looking at total number of positions applied for (not just at the ASHP Midyear Meeting), the average number of positions applied for was 3.1± 5.3 (median, 1.5). Survey respondents indicated that they received an average of 2 onsite interviews.
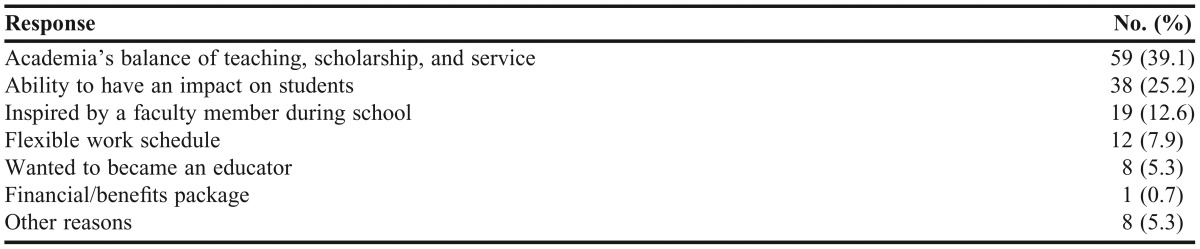
The majority of new faculty members (39.1%) indicated they chose to pursue a career in academia because of the balance of teaching, research, and service the position entailed (Table 4). The second most common reason for pursuing a career in academia was the ability to have an impact on students (25.2%), followed by being inspired by a faculty member during their pharmacy education (12.6%).
Table 4.
Responses of Newly Hired, First-Time Pharmacy Faculty Members During 2012-2013 Academic Year to Question, “What was the Single Most Important Factor That Led You Into a Career in Academia?”
DISCUSSION
This research aimed to assess the education, training, and teaching experience of newly hired faculty members. The information obtained from survey respondents was intended to help US colleges and of pharmacy by providing an overview of the skills and experiences among new faculty pharmacy programs throughout the United States. These data could also provide guidance to potential new faculty members regarding the types of education, training, and experience they should pursue to best align themselves for a future faculty position.
The questionnaire was designed to address how the changing landscape of pharmacy education can impact the types of positions being offered at US colleges and schools of pharmacy. New faculty members hired at the assistant-professor or clinical assistant-professor level accounted for almost 90% of all new faculty hires. Of these new junior faculty members, three-fourths were pharmacy practice faculty members. Raehl and colleagues concluded that 65% of all junior faculty members in 2001 were in pharmacy practice.1 Our results show an increase in the number of junior pharmacy practice faculty members being hired compared with the data from 2001. In the earlier study, the authors concluded that colleges and schools of pharmacy relied heavily on hiring nontenure-track, junior clinical faculty members to meet teaching needs and that the demand for these faculty members was high. In our study, only 8% of new faculty members were hired at the associate-professor level, and only a single new faculty member was hired at the clinical-professor level. Our data are similar to findings of the earlier study in showing that junior pharmacy practice faculty members represented the majority of new hires by colleges and schools of pharmacy in 2012-2013. The majority of new faculty members being hired at the assistant-professor level may be related to the large number being hired directly from residency or graduate school into faculty positions. Ambulatory care was the most common pharmacy specialty of new faculty members in our study, but we do not have data from 2001 to compare the changes in ambulatory care positions over time. As healthcare delivery continues to change and the focus shifts to more preventive care, pharmacists will continue to play a role in primary or ambulatory care, and we will likely see a continuing increase in ambulatory-care faculty positions throughout the country.
Another aim of our study was to describe the education, training, and academic experience of new faculty members. More than half of new pharmacy practice faculty members went directly from residency to their faculty positions, but only a third of new clinical pharmacy faculty members completed a specialized PGY2 residency. This difference may be attributable to the decreased availability of PGY2 vs PGY1 residency positions.5 ASHP match statistics reported only 590 PGY2 residency positions available in 2012, compared with 2,408 PGY1 positions available by means of the ASHP match. However, PGY2 positions have increased by 34% since 2009. Of first-time pharmacy practice faculty members responding to the current survey, less than half had achieved board-certification in 1 of the pharmacy specialties, most commonly BCPS. Given the percentage of pharmacy practice faculty members who were not board-certified at the time of hire, prospective new faculty members might consider achieving this certification to help them be more competitive for available positions.
Academic experience obtained prior to applying for a faculty position may be just as important as education and training for a new faculty member. In our survey, new faculty members participated in many different academic experiences prior to obtaining their faculty positions. The majority had served as a preceptor for pharmacy students, whereas only a third had taken advantage of the opportunity to complete an academic practice experiences during APPEs or residency. Academic practice experiences may be an excellent opportunity for potential faculty members to obtain a more in-depth academic experience and also make a good impression on current faculty members. Less than half of new pharmacy practice faculty member had at least 1 peer-reviewed publication, demonstrating that previous scholarship experience was not required among new pharmacy practice faculty members. Although having published does not appear to be a prerequisite for many new pharmacy practice faculty positions, previous scholarship may represent an area where potential new applicants can distinguish themselves from other candidates. In contrast, the scholarly work of faculty members focused on science or research was quite impressive, with over 90% having at least 1 publication, with a mean of 20 publications. The difference between scholarly activity among pharmacy practice faculty members compared with pharmaceutical science faculty members appears to correlate with expectations of faculty members in each of these academic tracks.
This study has several limitations. Although 151 new faculty members responded to the survey (49.2%), the data describe only half of the new faculty members hired for the 2012-2013 academic year. However, over 70 different colleges and schools of pharmacy – more than 50% of all those in the United States – were represented in this survey. The survey data also do not report respondent demographics, such as the age or gender of new faculty members. Demographic questions were excluded from the survey instrument to ensure anonymity of respondents. Additionally, some questions from the survey instrument, such as those relating to residency training or achievement of board certification, also would not be relevant to new faculty members who were not registered pharmacists.
CONCLUSION
The findings of this survey provide information for colleges and schools of pharmacy and potential future new faculty members regarding the education, training, and academic experience of recently hired pharmacy faculty members. Many of the new positions are in the practice area of ambulatory care, which may indicate a shift in pharmacy practice; however, these data will need to be tracked with future hiring statistics of ambulatory care faculty members. Training pharmacy students for roles in medication-therapy management requires faculty members with training and experience in ambulatory care. Residency programs continue to attract new faculty members interested in academia. Future studies should address the success of newly hired pharmacy faculty members, based on their prior education and experience. Understanding the factors associated with successful new faculty members is expected to assist colleges and schools of pharmacy in hiring the best candidates based on their specific skill sets.
REFERENCES
- 1.Raehl CL. Changes in pharmacy practice faculty 1995-2001: implications for junior faculty development. Pharmacotherapy. 2002;22(4):445–462. doi: 10.1592/phco.22.7.445.33678. [DOI] [PubMed] [Google Scholar]
- 2.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy learning to the doctor of pharmacy degree. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Adopted January 23, 2011. Accessed: July 20th, 2013.
- 3.Murphy JE, Nappi JM, Bosso JA, et al. American College of Clinical Pharmacy’s vision of the future: postgraduate pharmacy residency training as a prerequisite for direct patient care practice. Pharmacotherapy. 2006;26(5):722–733. doi: 10.1592/phco.26.5.722. [DOI] [PubMed] [Google Scholar]
- 4.Leiker LL, Mehta BH, Rodis JL, Pruchnicki MC, Pedersen CA. Assessment of pharmacy faculty members opinions regarding required postgraduate pharmacy residencies. Am J Health Syst Pharm. 2009;66(4):378–388. doi: 10.2146/ajhp070586. [DOI] [PubMed] [Google Scholar]
- 5.American Society of Health-System Pharmacists. ASHP Resident Matching Program. Summary of programs and positions offered and filled for the 2013 match. https://www.natmatch.com/ashprmp/stats/2013summpos.html. Accessed August 7, 2013.


