Abstract
Objective. To describe the planning, implementation, and outcomes of an interprofessional education clinical laboratory facilitated through human patient simulation.
Design. An interprofessional education clinical laboratory was developed with a patient-care scenario of acute exacerbation of heart failure that incorporated the use of a high-fidelity patient simulator. Pharmacy and nursing students assumed clinical roles in this realistic scenario and collaborated to diagnose and treat the patient.
Assessment. Student attitudes toward and readiness to participate in interprofessional education improved following participation in the laboratory. Students reported that the greatest benefit of the experience was in their communication skills.
Conclusion. Students’ ability to participate in interprofessional education experiences and their attitudes toward them improved following participation in this curricular initiative. Further evaluation of the impact of interprofessional education on student learning outcomes and changes in practice is warranted.
Keywords: interprofessional education, pharmacy students, nursing students, simulation
INTRODUCTION
Interprofessional education (IPE) has been a growing part of the curricula in colleges of medicine and nursing for the last decade. However, literature describing IPE between pharmacy students and those enrolled in other health professional training programs is limited. One of the first reports of an IPE experience involving pharmacy students with those from other disciplines involved collaborative care in the management of patients with asthma.1 Two others have described the use of standardized patients in the development of collaboration and communication skills among students from multiple disciplines.2,3 Another used IPE to teach team-building skills early in the pharmacy curriculum.4 Other reports described IPE experiences that developed pharmacy students’ patient-care skills and other abilities, including having difficult conversations with patients,5 promoting asthma health,6 teaching pediatric prescribing,7 and improving self-confidence on an interprofessional healthcare team.8
Despite limited research on the effects of IPE on student knowledge and skill development, several organizations have taken positions advocating for its incorporation into the curriculum of health professions education. The American Association of Colleges of Pharmacy has advocated for the incorporation of IPE in colleges and schools of pharmacy,9 and the Accreditation Counsel for Pharmacy Education has incorporated IPE into its Accreditation Standards and Guidelines for the Doctor of Pharmacy Degree.10 The updated Educational Outcomes 2013 from the Center for the Advancement of Pharmacy Education do not use the term IPE, but subdomain 3.4, “Interprofessional Collaboration,” embodies the spirit of IPE and encourages programs to incorporate IPE learning objectives in line with their curricular outcomes.11 Outside of organizations focused on academia, the American College of Clinical Pharmacy has published a Position Statement and White Paper advocating for the incorporation of IPE in the education of pharmacy and other healthcare professionals.12,13
As with colleges and schools of pharmacy, incorporation of IPE in prelicensure curricula is also advocated in nursing education. The National League for Nursing and the American Association of Colleges of Nursing include IPE criteria in their accreditation guidelines.14,15 Organizations such as the International Nursing Association for Clinical Simulation and Learning (INACSL) and the Society for Simulation in Healthcare also have focused on IPE strategies at their annual meetings and conferences and in their academic publications.16,17
Much like the growth of IPE in the education of health professions students, there has been similar expansion in the use of human patient simulation. Simulation has been used in medical education for nearly 2 decades but has only recently been used in the education of other health professions students.18 Less than 10 years ago, human patient simulation was introduced into nursing curricula and has been viewed as an effective way to provide realistic and safe opportunities for students to develop clinical nursing judgment.19 The introduction of human patient simulation into the curricula of pharmacy colleges and schools has occurred more recently, and several reports have described its benefits to student learning.20-26
Only a few reports have examined the use of human patient simulation in an IPE experience among pharmacy students and those from other health disciplines. One report described the use of human patient simulation to teach patient safety, collaboration, and communication among an interprofessional group of students.27 Another described 1 pharmacy school’s efforts to increase their IPE curriculum using human patient simulation with teams representing 5 disciplines.28 With the introduction of human patient simulation in the nursing and pharmacy curricula at Wilkes University, faculty members were seeking to create opportunities to use this technology in an IPE experience among students in the 2 schools. Therefore, we created the first IPE clinical laboratory within the curricula of both programs.
Approximately 1 year prior to the implementation of this curricular innovation, faculty members in the schools of pharmacy and nursing began discussing the possibility of developing an IPE experience for doctor of pharmacy (PharmD) and nursing students. It was decided early in the development of this curricular initiative that human patient simulation would be used to facilitate the IPE experience. Although the schools had been combined under the same college for nearly a decade, there were no IPE offerings among students in the programs, and there was very little IPE within the curricula of either program. Additionally, in contrast to students in the school of nursing, those in the school of pharmacy had minimal experience with human patient simulation, and none of it was with high-fidelity simulators. Therefore, there were 2 goals for this curricular innovation: to increase the IPE offerings within and between the 2 programs and to provide additional advanced human patient simulation exposure to pharmacy students. Because this was 1 of the first IPE experiences in the curricula of both schools, student attitudes toward IPE were assessed before and after the laboratory with the hypothesis that attitudes would improve after the experience.
DESIGN
The desired outcome of this curricular innovation for both groups of students was for them to gain experience and appreciation for working with another health care discipline to achieve common goals. The knowledge-specific objective was for students to identify the circumstances under which interprofessional care would lead to an improvement in patient outcomes. The skill-based objective was to develop effective collaboration among student health professionals from similar and divergent fields to optimize patient care. An objective related to student attitudes was for students to recognize that effective interprofessional care optimizes individual patient therapy and improves outcomes. Another objective was for students to further develop, achieve, and demonstrate the verbal and nonverbal communication skills necessary for effective interprofessional interaction.
A clinical laboratory using human patient simulation was developed in order to facilitate IPE. All junior nursing students and all third-year pharmacy students participated in the laboratory in the 2012 spring semester as part of 1 of their required clinical laboratory courses. An acute-care scenario was developed wherein a patient who had been stable after recovering from an acute exacerbation of heart failure developed weakness and new onset shortness of breath just before the nursing change-of-shift in the morning. The cause of the patient’s symptoms was new-onset atrial fibrillation leading to another acute exacerbation of heart failure; however, the cause was unknown to the students. Students working in groups composed of 2 nursing students and 2 to 3 pharmacy students were provided with basic information about the patient similar to what a nurse or pharmacist might know about a patient at the beginning of the work day. This basic information was made available to students 1 week prior to the laboratory and again during the laboratory as they prepared. The roles assigned to the pharmacy students were those of the telemetry floor pharmacist and cardiac intensive care unit/cardiology pharmacist(s). The nursing students’ roles were those of the primary and secondary nurses for the shift. The students needed to work together to acquire the additional pieces of subjective and objective information necessary to appropriately diagnose the patient and initiate therapy.
For homework prior to the laboratory, pharmacy students were instructed to review several readings on various cardiovascular disorders from their required therapeutics text, Pharmacotherapy: Principles and Practice. Nursing students were assigned readings from their required medical-surgical textbook, Brunner & Suddarth’s Textbook of Medical-Surgical Nursing: North American Edition, to reinforce the concepts pertinent to care of the cardiovascular patient. Nursing students were also provided access to the patient’s chart so they could begin their nursing care plan or concept map.
Additional preparation for the pharmacy students included a clinical laboratory in the same course during the preceding week that exposed them to the same high-fidelity patient simulator they would be working with the following week. This exposure allowed students to gain familiarity with this technology, which was new to them. All students were made aware at least a week prior to the laboratory that its purpose was interprofessional patient care. Students were also provided with the same objectives noted previously but were not informed of what they each needed to do or how and on what they were being assessed during the simulation portion of the laboratory.
The laboratory took place in the Clinical Nursing Simulation Center on the University’s main campus. One high-fidelity simulator, the S3600 HAL Mobile Team Trainer, (Gaumard, Miami, FL) served as the patient for the IPE laboratory. The simulation portion of the laboratory was conducted in a room that resembled a typical patient room, complete with a medical bed, mock wall ports, equipment (eg, oxygen tubing with face mask), supplies (including both necessary and unnecessary mock medications and syringes), and a vital signs monitor synchronized with the wireless simulator controls. Students also were provided with the results of the patient’s STAT 12-lead electrocardiogram when they entered the patient room. Faculty facilitators were able to observe student interaction during patient assessment and treatment through a 1-way mirror, and an audio system allowed facilitators to hear what was occurring in the room. The patient simulator was preprogrammed with branching scenarios for appropriate vital sign changes based on the treatments students might administer (eg, decreased blood pressure and heart rate following administration of diltiazem). Additionally, preprogrammed and impromptu verbal responses initiated by the facilitators allowed the patient to respond appropriately to student questions and therapeutic interventions. Facilitators were provided with a storyboard for the patient scenario that served as a guide so that vital sign changes and patient responses based on therapeutic interventions remained consistent between the student groups.
One of the main obstacles to overcome in developing this curricular innovation was finding a common time in the curricula of the 2 programs for the IPE clinical laboratory. Although this issue was easily resolved because the scheduled times of both 3-hour clinical laboratory courses overlapped by 2 hours, student groups had to be scheduled over a longer 4-hour period to allow all students in any of the 3 once-weekly sections of the courses to complete the laboratory. If scheduled to be in the laboratory outside normal class time, students were contacted several weeks in advance to ensure they would be available.
Several logistical issues had to be addressed as well to allow all students enrolled in a particular course section to participate using only 1 patient simulator. To work around these issues, student groups and facilitators were scheduled for 1-hour blocks of time during which they moved through 3 stations (approximately 1 every 20 minutes), with a new group beginning the first station each time the previous group moved to their next station. One pharmacy and 1 nursing faculty member each were assigned as facilitators for each student group. There was also an additional facilitator present from the Clinical Nursing Simulation Center to control the simulator during the human patient simulation portion of the laboratory. Therefore, 7 facilitators were needed for each section of the courses, with each facilitator pair facilitating a new student group every hour. Students were instructed to arrive at least 5 minutes prior to their scheduled time. At their scheduled time, 1 of the facilitators provided group members with a brief overview of the laboratory logistics and informed them of the supplies and equipment that would be available in the patient room. Groups were then given 5 minutes to become acquainted with one another and prepare. Facilitators provided no instruction to the groups as to how they were to interact during the simulation or what they were to do individually. Groups were then directed into the patient room and allowed up to 20 minutes to complete the simulation. Immediately following the simulation, groups were taken into an adjacent room for an interprofessional debriefing conducted by both the pharmacy and nursing facilitators using scripted questions focused on IPE. Following this activity, the groups split into their individual disciplines and moved to 2 other separate rooms where discipline-specific debriefings were conducted by the appropriate faculty facilitator during the remaining time (approximately 15 to 20 minutes). During this time, facilitators used scripted questions that focused on both discipline-specific issues related to the patient case and interprofessional issues.
EVALUATION AND ASSESSMENT
Achievement of the primary outcome was assessed by means of a prelaboratory and postlaboratory survey instrument, which was created using a modification of the Readiness for Interprofessional Learning Scale (RIPLS). The RIPLS is a validated 19-item instrument that uses a 5-point Likert scale to assess student readiness for interprofessional learning.29 This instrument was the best available tool for assessing how students’ attitudes were influenced by the curricular initiative, given their general lack of prior IPE experiences in the curricula of both programs. The instrument was modified to exclude 1 survey item that did not apply to pharmacists (ie, “The function of nurses and therapists is mainly to provide support for doctors”). Additional 5-point Likert-scale items were added to the survey instrument to assess student opinions of how IPE affects certain discipline-specific abilities, such as communication, along with attitudes toward IPE and the influence of human patient simulation on the IPE laboratory session. The research aspect of this curricular innovation was granted exempt status by the study university’s institutional review board.
Students were sent an invitation by e-mail 2 weeks prior to the IPE clinical laboratory asking them to participate in this voluntary anonymous survey, which was distributed using an online service (SurveyMonkey, Portland, Oregon). Two reminders were sent to students who had not participated or only partially responded before the survey closed on the day the first groups of students participated in the laboratory. Immediately after all 3 course sections had completed the IPE clinical laboratory, students who had provided consent and completed the prelaboratory survey instrument were e-mailed an invitation to complete a survey instrument that included the same items as in the prelaboratory survey instrument, along with additional items that evaluated aspects of the laboratory unrelated to the course objectives. Students who did not initially participate or partially responded were once again sent 2 reminders seeking their participation. The postlaboratory instrument also used retrospective pretest/posttest methodology for the questions assessing the influence of human patient simulation on IPE and how IPE affects discipline-specific abilities. This portion of the instrument was included to account for any response-shift bias, which occurs when the intervention changes evaluation standards in these self-reported measures.30
Only responses of students who completed both the prelaboratory and postlaboratory survey instruments were included in the data analysis. Each student’s responses on the prelaboratory survey instrument were paired to those on their postlaboratory survey instrument for data analysis using a unique personal identification number that students created and included on both survey instruments. Given that data were not normally distributed for any of the results, the Wilcoxon signed-rank test was used to test for significance between responses on the prelaboratory and postlaboratory survey instruments. All data analyses were conducted using SPSS, version 19.0 (IBM SPSS Statistics, IBM Corporation, Armonk, New York). All p values were two-sided and considered significant if less than 0.05 for all results.
One hundred twenty students who were enrolled in 2 separate courses were surveyed (69 pharmacy and 51 nursing). Among these 75 consented to participate (61 pharmacy, 13 nursing, and 1 participant did not identify their major) and 72 completed the prelaboratory survey instrument. Of those who completed the prelaboratory survey, 64 also completed the postlaboratory survey instrument, including 56 pharmacy students and 9 nursing students. Among the 64 students who completed the postlaboratory survey instrument, 55 students’ responses on the prelaboratory and postlaboratory survey instruments were capable of being paired, including those of 48 pharmacy students and 7 nursing students. Thus, although the overall response rate for consenting students who completed both survey instruments was 53%, analysis was performed on 86% of the data.
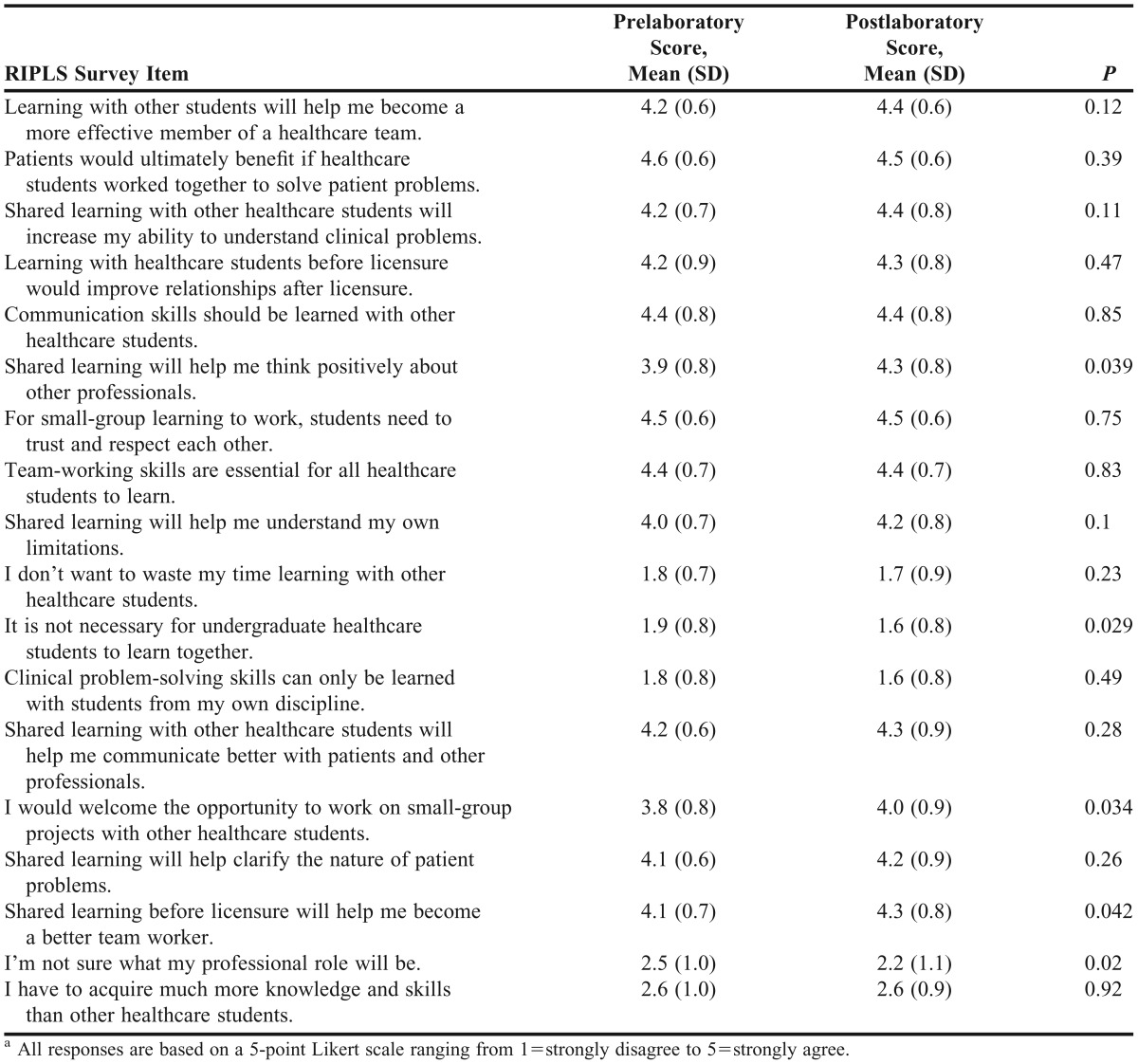
Aggregate student responses to the RIPLS instrument are provided in Table 1. Scores improved from the prelaboratory survey instrument, indicating that students were more prepared for IPE after the IPE laboratory. However, the scores improved significantly from baseline for only 5 survey items. Specifically, students’ scores indicated that the experience helped them think more positively about other professionals, made them want to work on projects with other healthcare students, and helped them become better team members. They also felt that working with other healthcare students was necessary and that they better understood their professional role as a result of the experience.
Table 1.
Student Responses to the Readiness for Interprofessional Learning Scale (RIPLS)a
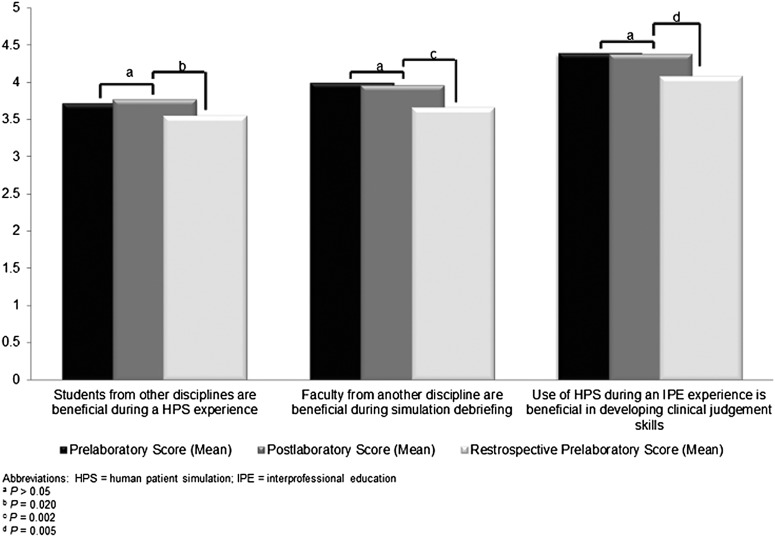
The effects of the curricular intervention on students’ knowledge and skills within their specific disciplines were not significant when comparing prelaboratory and postlaboratory test scores (Table 2). However, the difference in scores became significant for all 6 criteria using the retrospective pretest/posttest methodology. Student attitudes about IPE and the use of human patient simulation to facilitate IPE did not improve significantly when comparing responses on the prelaboratory and postlaboratory survey instruments but once again did using the retrospective pretest/posttest methodology (Figure 1).
Table 2.
Effect of Interprofessional Education on Student Knowledge, Skills and Attitude
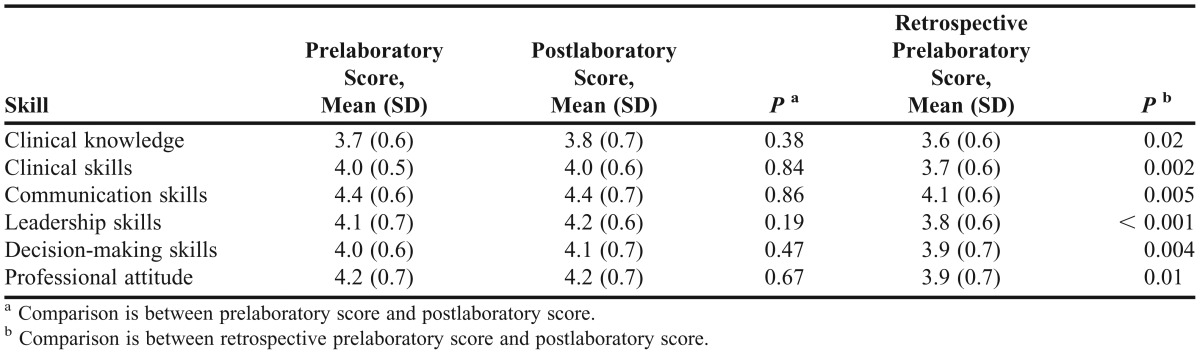
Figure 1.
Student Attitudes Toward Interprofessional Education and Human Patient Simulation
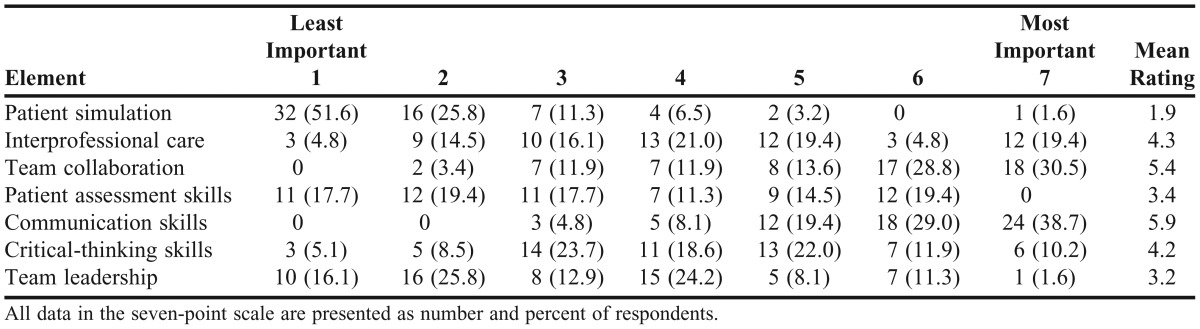
An additional item on the postlaboratory survey instrument asked students to rank 7 elements used during the IPE laboratory based on their perceived order of importance for enhancing student learning during the IPE experience (Table 3). Students ranked communication skills and team collaboration very high and gave team leadership and patient simulation the lowest rankings overall.
Table 3.
Student Ranking of Elements Used During the Interprofessional Education Laboratory
DISCUSSION
We designed our curricular innovation with 2 goals in mind: to increase the IPE offerings within the schools of pharmacy and nursing and to expose pharmacy students to high-fidelity human patient simulation. Our hypothesis was that students who worked together to solve a common problem would develop better attitudes toward IPE as a result of their experience. Although the data we collected did not show significant improvement for all survey items related to student attitudes and readiness to participate in IPE, overall scores improved.
While IPE is becoming more prevalent and integrated in the curricula of various health disciplines, 1 study showed that few programs have their students participate in true IPE experiences.31 The schools of pharmacy and nursing at Wilkes University had coexisted on the main campus of the university for nearly 16 years prior to this curricular innovation. While students from both schools had been participating in an annual IPE collaborative care summit involving multiple disciplines, they had not participated in an IPE experience wherein they were expected to assume a clinical role during a realistic patient-care scenario. Some of the perceived barriers to this experience included the coordination of student schedules, availability of adequate facilities to accommodate an IPE experience, and participation of all students in a graduating class from both schools.
Using human patient simulation to facilitate IPE has been reported by others and may be a potential starting point for programs to overcome some of these perceived barriers. Three reports have described the successful use of human patient simulation-facilitated IPE among nursing and medical students.32-34 However, we were able to find only 3 prior reports of human patient simulation-facilitated IPE involving pharmacy students and those from other disciplines. One of these showed that human patient simulation can be used in an IPE experience to teach healthcare teams how to have difficult conversations with patients.5 This study was limited because the cohort consisted of an interprofessional group of only 12 students, and no direct assessment of the intervention’s impact on IPE was conducted. Another report showed that after the integration of human patient simulation into a 4-week IPE curriculum, pharmacy students’ interprofessional collaboration and communication skills were enhanced.27 A subsequent report described the use of human patient simulation during an IPE scenario involving 5 different disciplines and its impact on communication, but only 8 students were involved in this feasibility study.28
The introduction of high-fidelity human patient simulation in the school of nursing was perceived as an opportunity to develop IPE experiences between the 2 schools and to increase pharmacy students’ exposure to human patient simulation. To overcome the barriers of coordination of student class schedules and participation among all students of a graduating class, faculty members from both programs collaborated to determine the appropriate courses within the 2 curricula to include an IPE curricular initiative facilitated by human patient simulation. The clinical laboratory courses of both curricula seemed to be the ideal fit. Because the class schedules of these courses overlapped, we were able to avoid the need to conduct this IPE experience entirely outside the normal class time for either group of students. We also had the advantage of flexibility in both the nursing and pharmacy class schedules before and after the overlapping time. Otherwise, the scheduling of this curricular initiative would have had to occur outside normal class time for at least 1 of the disciplines.
With these barriers resolved, we still had to address how to use the 1 high-fidelity adult patient simulator in our Clinical Nursing Simulation Center with all of the students during each laboratory section. Having several groups of facilitators allowed us to move the student groups through each of the 3 stations of the IPE laboratory. Therefore, there was always a group of students performing the simulation portion of the laboratory, and we were able to complete each laboratory section for all the assigned student groups using only 1 patient simulator. An added benefit to this schedule was that the faculty facilitators were able to stay with the same student group throughout the 3 stations, allowing them to address issues during the debriefings that were specific to each student group. With additional patient simulators, we could have had more realistic group sizes that consisted of 1-2 nursing students and 1 pharmacy student, and could have conducted each laboratory section in a shorter amount of time. However, doing so would have required additional faculty facilitators, which may have provided an additional challenge.
The data we collected showed that students met the objectives of the curricular innovation. Scores from the RIPLS instrument and additional survey instrument items showed that students gained an appreciation for IPE, that the experience prepared them for additional IPE, and that they considered improvement in interprofessional communication as the most important benefit of the curricular innovation.
Despite the successful integration of this IPE experience into the curricula of both schools, there were limitations to our initiative. The largest is that we did not directly assess the impact of this IPE experience on student learning, which would be a key factor in determining further incorporation of IPE into our curricula. One potential method to assess the effect of this and other IPE initiatives on student learning would be with an IPE-focused objective structured clinical examination (OSCE). Given that the impact of an IPE experience on student learning was not the goal of this curricular initiative, we did not develop and OSCE for assessment. Instead, we chose to focus on student attitudes and perceptions of IPE, as this was the first IPE experience between the 2 schools. Another limitation of our initiative was that we did not provide the students with any preparation regarding the IPE aspects of this curricular innovation. Given the hypothesis and objectives we were assessing, we did not want to introduce bias. We do not know if this curricular initiative resulted in application of the knowledge and skills gained to experiential and eventual practice settings, but assessing such an effect would be confounded by several factors inherent in clinical practice. Conducting such assessment may be more practical if knowledge, skills, and attitudes gained during prior IPE experiences were assessed for their application in subsequent IPE curricula. This type of assessment also could be accomplished through a structured assessment such as an OSCE focused on IPE. A final limitation is that extrapolation of our findings to nursing students is limited because of the low participation rate by nursing students in the survey.
Despite these limitations, this IPE experience remained in the curricula of both schools at the time of this writing, and several improvements were made for the following year. These included all students being required to review online IPE informational resources developed by the faculty instructors during the week prior to the laboratory, such as researching the roles of the other discipline in the acute care setting and watching videos of health professional student IPE experiences that use human patient simulation. The pharmacy students also were required to review a video on the functionality of the high-fidelity patient simulator used in the laboratory. The revisions facilitated additional preparation on what students in each discipline might be expected to do during the simulation, possibly allowing for improved assessment of student learning from the experience.
Along with these recent improvements, plans were being made to implement more IPE experiences. Faculty members from the schools of pharmacy and nursing were working together to develop an additional IPE experience in which students from both schools would collaborate to assess a standardized patient during a home health visit. An additional IPE experience using human patient simulation is being developed wherein students will assess and treat a pediatric patient who presents to the emergency department with an acute asthma exacerbation. Both schools also plan to collaborate with a local medical college and neighboring universities with additional allied health programs to incorporate students from additional disciplines into future IPE curricula. This collaboration was expected to be facilitated through the Northeastern/Central Pennsylvania Interprofessional Education Collation.
SUMMARY
The IPE offerings at the schools of pharmacy and nursing were increased and pharmacy students were exposed to human patient simulation with a human patient simulation-facilitated IPE clinical laboratory focused on a cardiovascular patient-care scenario. There was an improvement in student attitudes toward IPE following participation in the laboratory. Students also reported feeling more prepared for future IPE experiences and indicated that the laboratory especially helped develop their interprofessional communication skills. However, assessing the effects of IPE on student learning will be critical as health professional disciplines continue to move out of their silos and into an environment of collaborative interprofessional care.
REFERENCES
- 1.Rodehorst TK, Wilhelm SL, Jensen L. Use of interdisciplinary simulation to understand perceptions of team members' roles. J Prof Nurs. 2005;21(3):159–166. doi: 10.1016/j.profnurs.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 2.Wamsley M, Staves J, Kroon L, et al. The impact of an interprofessional standardized patient exercise on attitudes toward working in interprofessional teams. J Interprof Care. 2012;26(1):28–35. doi: 10.3109/13561820.2011.628425. [DOI] [PubMed] [Google Scholar]
- 3.Westberg SM, Adams J, Thiede K, Stratton TP, Bumgardner MA. An interprofessional activity using standardized patients. Am J Pharm Educ. 2006;70(2) doi: 10.5688/aj700234. Article 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fernandez R, Parker D, Kalus JS, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710351. Article 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marken PA, Zimmerman C, Kennedy C, Schremmer R, Smith KV. Human simulators and standardized patients to teach difficult conversations to interprofessional health care teams. Am J Pharm Educ. 2010;74(7) doi: 10.5688/aj7407120. Article 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saini B, Shah S, Kearey P, Bosnic-Anticevich S, Grootjans J, Armour C. An interprofessional learning module on asthma health promotion. Am J Pharm Educ. 2011;75(2) doi: 10.5688/ajpe75230. Article 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor D, Yuen S, Hunt L, Emond A. An interprofessional pediatric prescribing workshop. Am J Pharm Educ. 2012;76(6) doi: 10.5688/ajpe766111. Article 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacDonnell CP, Rege SV, Misto K, Dollase R, George P. An introductory interprofessional exercise for healthcare students. Am J Pharm Educ. 2012;76(8) doi: 10.5688/ajpe768154. Article 154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kroboth P, Crismon LM, Daniels C, et al. Getting to solutions in interprofessional education: report of the 2006-2007 Professional Affairs Committee. Am J Pharm Educ. 2007;71(6) Article S19. [Google Scholar]
- 10.Accreditation Council for Pharmacy Education. Chicago, Illinois: Accreditation Council for Pharmacy Education; 2006. Accrediation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed September 15, 2013. [Google Scholar]
- 11.Medina MS, Plaza CM, Stowe CD, et al. Center for the Advancement of Pharmacy Education (CAPE) educational outcomes 2013. American Association of Colleges of Pharmacy, 2013. http://www.aacp.org/resources/education/cape/Pages/default.aspx. Accessed September 15, 2013.
- 12.American College of Clinical Pharmacy. Interprofessional education and practice. Pharmacotherapy. 2009;29(7):880–881. doi: 10.1592/phco.29.7.880. [DOI] [PubMed] [Google Scholar]
- 13.Page RL, Hume AL, Trujillo JM, et al. Interprofessional education: principles and application a framework for clinical pharmacy. Pharmacotherapy. 2009;29(7):879. [Google Scholar]
- 14.American Association of Colleges of Nursing. The essentials of baccalaureate education for professional nursing practice. Ocotber 20, 2008. http://www.aacn.nche.edu/publications/order-form/baccalaureate-essentials. Accessed September 27, 2013.
- 15.National League of Nursing Accreditation Commission. NLNAC accreditation manual. 2011. http://www.nlnac.org/Manual%20&%20IG/2003_manual_TOC.htm. Accessed September 27, 2013.
- 16.Society for Simulation in Healthcare. SSH Accreditation Process 9.10: Informational guide for the accreditation process from the SSH Council for Accreditation of Healthcare Simulation Programs. Society for Simulation in Healthcare; 2011.
- 17.The INASCL Board of Directors. Standards of best practice: simulation. Clin Simul Nurs. 2011;7(4S):S3–S19. [Google Scholar]
- 18.Gordon JA, Wilkerson WM, Shaffer DW, Armstrong EG. “Practicing” medicine without risk: students' and educators' responses to high-fidelity patient simulation. Acad Med. 2001;76(5):469–472. doi: 10.1097/00001888-200105000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Jeffries PR. A framework for designing, implementing, and evaluating simulations used as teaching strategies in nursing. Nurs Educ Perspect. 2005;26(2):96–103. [PubMed] [Google Scholar]
- 20.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720237. Article 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mieure KD, Vincent WR, III, Cox MR, Jones MD. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ. 2010;74(2) doi: 10.5688/aj740222. Article 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gilliland I, Frei BL, McNeill J, Stovall J. Use of high-fidelity simulation to teach end-of-life care to pharmacy students in an interdisciplinary course. Am J Pharm Educ. 2012;76(4) doi: 10.5688/ajpe76466. Article 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seybert AL, Smithburger PL, Kobulinsky LR, Kane-Gill SL. Simulation-based learning versus problem-based learning in an acute care pharmacotherapy course. Simul Healthc. 2012;7(3):162–165. doi: 10.1097/SIH.0b013e31825159e3. [DOI] [PubMed] [Google Scholar]
- 26.Branch C. Pharmacy students' learning and satisfaction with high-fidelity simulation to teach drug-induced dyspepsia. Am J Pharm Educ. 2013;77(2) doi: 10.5688/ajpe77230. Article 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vyas D, McCulloh R, Dyer C, Gregory G, Higbee D. An interprofessional course using human patient simulation to teach patient safety and teamwork skills. Am J Pharm Educ. 2012;76(4) doi: 10.5688/ajpe76471. Article 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smithburger PL, Kane-Gill SL, Kloet MA, Lohr B, Seybert AL. Advancing interprofessional education through the use of high fidelity human patient simulators. Pharm Pract (Granada) 2013;11(2):61–65. doi: 10.4321/s1886-36552013000200001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parsell G, Bligh J. The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS) Med Educ. 1999;33(2):95–100. doi: 10.1046/j.1365-2923.1999.00298.x. [DOI] [PubMed] [Google Scholar]
- 30.Howard GS. Response-shift bias: a problem in evaluation interventions with pre/post self-reports. Eval Rev. 1980;4(1):93–106. [Google Scholar]
- 31.Lapkin S, Levett-Jones T, Gilligan C. A cross-sectional survey examining the extent to which interprofessional education is used to teach nursing, pharmacy and medical students in Australian and New Zealand Universities. J Interprof Care. 2012;26(5):390–396. doi: 10.3109/13561820.2012.690009. [DOI] [PubMed] [Google Scholar]
- 32.Dillon PM, Noble KA, Kaplan L. Simulation as a means to foster collaborative interdisciplinary education. Nurs Educ Perspect. 2009;30(2):87–90. [PubMed] [Google Scholar]
- 33.Reese CE, Jeffries PR, Engum SA. Learning together: using simulations to develop nursing and medical student collaboration. Nurs Educ Perspect. 2010;31(1):33–37. [PubMed] [Google Scholar]
- 34.Reising DL, Carr DE, Shea RA, King JM. Comparison of communication outcomes in traditional versus simulation strategies in nursing and medical students. Nurs Educ Perspect. 2011;32(5):323–327. [PubMed] [Google Scholar]