Abstract
Clean intermittent catheterization has been demonstrated to be a safe and effective method of bladder drainage in patients with neurogenic bladder dysfunction. However, breakdowns in technique may allow the introduction of foreign matter into the bladder and thereby result in bladder calculi. The three cases reported herein demonstrate this potential problem in persons with spinal cord injury (SCI) with hair nidus as the source of bladder calculi causing neurogenic bladder. In each situation, the problem was identified, calculi were removed cystoscopically and the patient and/or the ancillary aid were reinstructed. We recommend annual renal function tests, ultrasound and cytoscopic screening in high suspicion cases to allow early detection of bladder calculi in persons with SCI and prevent further urinary tract infections. This report also emphasizes the need for patient education and a careful follow-up preventing bladder calculi and thus, minimizing the morbidity in persons with SCI.
Keywords: Spinal injury, Urinary bladder calculi, Autonomic dysreflexia, Neurogenic bladder
Introduction
Clean intermittent catheterization has been demonstrated to be a safe and effective method of bladder drainage in patients with neurogenic bladder dysfunction.1–3
This technique was advocated by Lapides et al.1 in 1972 and has been demonstrated to be an effective regimen for patients with neurogenic bladder dysfunction. This regimen utilizes a clean catheter to drain the bladder completely every 4 hours so that the bladder does not distend beyond approximately 300 ml during any period of the day. The catheter, after being used, is washed with mild soap and water, then rinsed and left to dry. Patients, who follow this regimen in the majority of instances, are completely asymptomatic.
Theoretically, the occurrence of bladder calculi in patients using this technique should be virtually non-existent because urinary stasis is eliminated. However, breakdowns in technique may allow the introduction of foreign matter into the bladder and thereby result in bladder calculi. The three cases reported herein demonstrate this potential problem. In each situation, the problem was identified and the patient and/or the ancillary aid were reinstructed.
Case 1
The first patient was a 24-year-old male who suffered traumatic tetraplegia since 2007 (C5 level, American Spinal Injury Association (ASIA) Impairment Scale (AIS) AIS-A) secondary to a road traffic accident; using assisted intermittent catheterization for bladder management, he presented with complaints of frequent intermittent leaks and symptoms of autonomic dysreflexia. Investigations revealed low Hb (10.2 g/dl) and elevated TLC (13.6 × 10/μl). Renal function tests were abnormal with urea (127 mg/dl) and serum creatinine (1.9 mg/dl). Urinalysis revealed proteins and nitrites, red blood cells (RBCs), and white blood cells (WBCs). Routine urine culture demonstrated significant bacterial counts (>100 colonies in Mac Conkey agar). Ultrasound (USG) of abdomen revealed echogenic foci in the bladder with increased bladder wall thickness. The patient was given 1 week of broad spectrum antibiotic therapy and a repeated urine culture after one week demonstrated sterile urine. Cystoscopy was then done and serpentine stones (Fig. 1) were removed; on breaking the calculus a pubic hair was visualized grossly as nidus. His symptoms improved after cystoscopic lithotripsy.
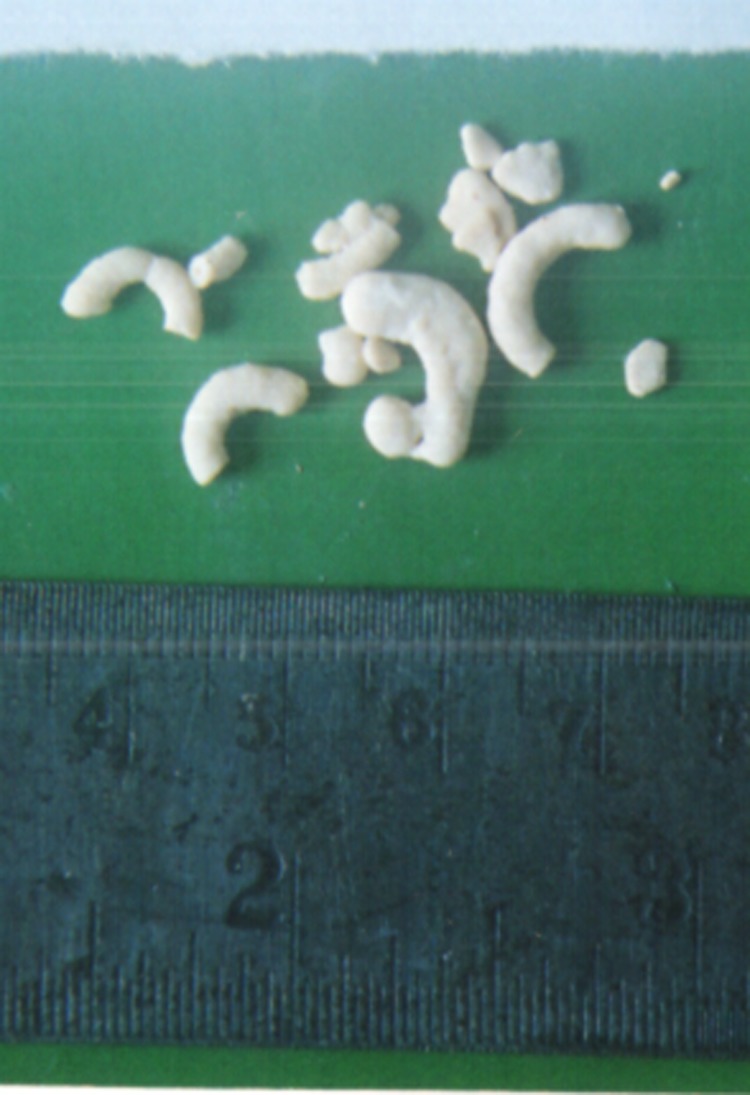
Figure 1.
Several serpentine stones of various sizes extracted cystoscopically.
Case 2
The second patient was a 27-year-old male with tetraplegia since 2007 (T 10 level, AIS-A) secondary to fall from a height; on self-intermittent catheterization, he had come for an annual review. Initial investigations revealed leukocytosis (15.4 × 10/μl), elevated creatinine levels (1.3 mg/dl) and positive urinalysis for RBCs, protein, and nitrites. Blood and urine cultures were negative. USG revealed a large bladder calculus, which was removed cystoscopically. The patient was administered two days of post-cystoscopy broad spectrum antibiotic coverage, because a significant percentage of patients develop symptomatic bacteremia after cystoscopy as reported in the literature. The serpiginous calculus was woven around hair nidus visualized on examination.
Case 3
The third patient was a 32-year-old male with tetraplegia since 2005 (C7 level, AIS-A), who was admitted with symptoms of frequent leaks and symptoms of autonomic dysreflexia (sweating, headache, and high blood pressure) occurring one to two times per day for the previous 6 months, precipitated after insertion of catheter during assisted intermittent catheterization. Urinalysis revealed numerous bacteria and WBCs. Plain radiography showed a linear, sausage calcification in the lower abdomen, and intra venous urogram (IVU) demonstrated a round filling defect with linear radio opacity in the bladder, suggesting calculus. USG revealed detrusor hypertrophy and echogenic shadow in the bladder obstructing the bladder neck. Patient was given broad spectrum antibiotic coverage as suggested by urine culture and sensitivity and serial urine cultures were obtained. Cystoscopy was performed after 10 days when urine culture became sterile, and using forceps, several stone fragments were removed, leading to subsequent relief in his symptoms. The gross appearance of the stone after extraction demonstrated a hair nidus from the stone fragments.
Discussion
Persons with spinal cord injury (SCI) are prone to develop a variety of urologic complications.4 Bladder stone disease is one of the common complications. Multitude of foreign bodies involved in the creation of bladder calculi include Foley balloon fragments,5 silk sutures,6 fragments of clothing,7 intrauterine devices,8 and rarely hair nidus.9–11
Calculi formation caused by hair introduced in the bladder is a preventable complication, which, if unrecognized, may jeopardize the entire urinary tract.12 Pubic hair can be introduced into the bladder either by adhering directly to the lubricated catheter or by overlying the urethral meatus and being pushed into the bladder. Impaired tactile discrimination in patients with SCI can also make the sensation of a small hair less noticeable as compared to persons with normal sensation. Assisted clean intermittent catheterization (CIC) increased the risk even further.
Being a foreign material, hair in the bladder is an ideal locus for crystalline precipitation, which may then be perpetuated by the reaction of the urothelium to the extraneous material.13 Similar cases associated with intermittent catheterization have been described previously10,11,14–18 and comparable cases of calculi forming on hair in pedicle island patch urethroplasty have been reported.
It is also possible that persons using intermittent catheterization limit fluid intake to reduce the frequency of catheterization, leading to a concentrated urine and subsequent preponderance to stone formation. An inappropriate technique like improper position in bed or wheelchair during intermittent catheterization leading to poor visibility of the urethral meatus and glans penis region may increase the likelihood of foreign body introduction (i.e. pubic hair) into the bladder. This could act as locus to initiate stone formation around the foreign body nidus.
Accounting for the apparent ease of introduction of pubic hairs in the bladder during intermittent catheterization, the physician's level of suspicion about hair nidus as a source of bladder calculi must be kept high in persons with SCI with recent onset of urinary complaints.
One of our cases diagnosed with bladder stones on annual review had no urinary complaints, which confirms the view of Vermeulen and associates that bladder calculi can develop even in the absence of infection but not nearly as rapidly.19 Annual urologic surveillance allows for timely intervention and prevents any long-term complications. Cystoscopic screening examination and subsequent calculi removal done for all three cases establish its utility as an excellent modality for both diagnostic and therapeutic intervention of bladder calculi. Likewise, we recommend annual renal function tests, USG, and cytoscopic screening in high suspicion cases to allow early detection of bladder calculi with the advantage to perform stone removal at the same time in persons with SCI and prevent further urinary tract infections. This report also emphasizes the need for patient education and a careful follow-up, preventing bladder calculi and minimizing the morbidity in persons with SCI.
References
- 1.Lapides J, Djokno AC, Silber SJ, Lowe BS. Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol 1972;107(3):458–61 [DOI] [PubMed] [Google Scholar]
- 2.Lapides J, Diokno AC, Gould FR, Lowe BS. Further observations on self-catheterization. J Urol 1976;116(2):169–71 [DOI] [PubMed] [Google Scholar]
- 3.McGuire EJ, Diddel G, Wagner F, Jr.. Balanced bladder function in spinal cord injury patients. J Urol 1977;118(4):626–28 [DOI] [PubMed] [Google Scholar]
- 4.Stover SL, Lloyd LK, Waites KB, Jackson A. Urinary tract infection in spinal cord injury. Arch Phys Med Rehabil 1989;70(1):47–54 [PubMed] [Google Scholar]
- 5.Matsuoka K, Nakawaga K, Eto K. A case history of foreign body stone in the urinary bladder. Kurume Med J 1988;35(3):123–5 [DOI] [PubMed] [Google Scholar]
- 6.Su CM, Lin HY, Li CC, Chou YH, Huang CH. Bladder stone in a woman after cesarean section: a case report. Kaohsiung J Med Sci 2003;19(1):42–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanno N, Iwasa A, Senoh H, Takemoto M. An unusual foreign body in the urinary bladder. Br J Urol 1994;73(5):587–8 [DOI] [PubMed] [Google Scholar]
- 8.Güvel S, Tekin MI, Kilinc F, Peskircioglu L, Ozkardeş H. Bladder stones around a migrated and missed intrauterine contraceptive device. Int J Urol 2001;8(2):78–9 [DOI] [PubMed] [Google Scholar]
- 9.Dalton DL, Hughes J, Glenn JF. Foreign bodies and urinary stones. Urology 1975;6(1):1–5 [DOI] [PubMed] [Google Scholar]
- 10.Zeitlin AB, Cottrell TL, Lloyd FA. Hair as a lower urinary tract foreign body. J Urol 1957;77(6):840–42 [DOI] [PubMed] [Google Scholar]
- 11.Derry P, Nuseibeh I. Vesical calculi formed over a hair nidus. Br J Urol. 1997;80(6):965. [DOI] [PubMed] [Google Scholar]
- 12.Soloman MH, Koff SA, Diokno AC. Bladder calculi complicating intermittent catheterization. J Urol 1980;124(1):140–41 [DOI] [PubMed] [Google Scholar]
- 13.Edwards CN, Garvey FK, Boyce WH. Studies on urothelium. III. Experimental vesical stone formation in the dog. J Urol 1963;89:207–13 [Google Scholar]
- 14.Amendola MA, Sonda LP, Diokno AC, Vidyasagar M. Bladder calculi complicating intermittent clean catheterization. AJR Am J Roentgenol. 1983;141(4):751–53 [DOI] [PubMed] [Google Scholar]
- 15.Kutscher AH, Vinson KR. Bladder calculi formation during clean intermittent catheterization. Urology 1979;14(4):357–8 [DOI] [PubMed] [Google Scholar]
- 16.Vaidyanathan S, Singh G, Seth P, Soni BM. Bladder stones of unusual shape in a male with paraplegia due to spinal cord injury who performed self catheterization. Spinal Cord 1999;37(5):375–6 [DOI] [PubMed] [Google Scholar]
- 17.Lee HJ, Kim HJ. Characterstic plain radiographic and intravenous urographic findings of bladder calculi formed over a hair nidus: a case report. Korean J Radiol 2001;2(1):61–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vaidyanathan S, Bingley J, Soni BM, Krishnan KR. Hair as the nidus of a bladder stone in a traumatic paraplegia patient. Spinal Cord 1997;35(8):558. [DOI] [PubMed] [Google Scholar]
- 19.Vermeulen CW, Grove WJ, Goetz R, Ragins HD, Correll NO. Experimental urolithiasis. I. Development of calculi upon foreign bodies surgically introduced into bladder of rats. J Urol 1950;64:541–48 [DOI] [PubMed] [Google Scholar]