Abstract
Osteosarcoma of the temporomandibular joint (TMJ) is rare. We report a case of osteosarcoma in the TMJ of a 62-year-old female, pre-operatively diagnosed to have a benign tumour, and discuss the usefulness and limits of MRI using a TMJ coil as a diagnosis.
Keywords: osteosarcoma, TMJ, MR imaging
Introduction
Osteosarcoma accounts for approximately 20% of primary bone tumours.1 The most common sites are the long bones, particularly in adolescent patients, with the majority occurring in the distal femoral metaphysis, proximal tibia and humeral metaphysis.1 Lesions of the jaw are uncommon, and most are regarded as being variants of osteosarcoma, representing about 6% of the total.1 Tumours occur in the mandible as frequently as in the maxilla. The body and the angle are the most commonly affected sites in the mandible.2
Osteosarcoma of the jaws generally occurs in the third decade of life, in contrast to osteosarcoma of the long bones, which is more common in the second decade of life.2
MR is superior to CT in detecting soft-tissue extension and bone-marrow extension of the malignant bone tumours.3 There are a few reports on temporomandibular joint (TMJ) osteosarcoma,4 but they do not describe the TMJ disc or disc–condyle relationship.
We report a case of TMJ osteosarcoma in a senior patient and discuss the findings obtained by MRI using a TMJ coil, with special emphasis on the disc and disc–condyle relationship.
Case report
In April 2011, a 62-year-old female noticed swelling of the left cheek. The swelling seemed to have disappeared after application of anti-inflammatory analgesic plaster. In July 2011, the swelling reappeared, and she visited a local hospital. She complained of disorders of the left masseter muscle and the left digastric muscle, although the TMJ did not have trismus or emit any abnormal sounds. She was diagnosed with a masticatory muscle disorder and was administered an analgesic drug. The pain disappeared, but the swelling increased. MRI with a head coil revealed a mass at the left TMJ. She was then referred to our hospital for further examination in August 2011. There were no signs of pain, sound, swelling at the TMJ or trismus. The maximum mouth opening length was 42 mm.
MRI (1.5 T; GE Healthcare, Milwaukee, WI) was performed with a TMJ coil. MR images were acquired in the parasagittal of the condyle to detect the disc and disc–condyle relationship. MR images showed a relatively well-defined lesion situated around the condyle and in the eminence of the left TMJ (Figures 1–3). The lesion showed inhomogeneous intermediate signal intensity on the T1 weighted image (Figure 1a) and inhomogeneous intermediate signal intensity on the T2 weighted image (Figure 1b). The lesion was slightly enhanced on the contrast-enhanced T1 weighted image (Figure 1c). The disc position was normal on the T1 weighted image (Figure 2a). The condylar head and the disc moved under the eminence in the mouth-opened position on the T1 weighted image (Figure 2b). The T1 weighted image revealed a relatively well-defined lesion around the condylar head (Figure 2b). The upper and the lower joint spaces did not have any areas with a low signal intensity (Figure 2). On the contrast-enhanced T1 weighted image, the lesion in the anterior of the condylar head did not show continuity with the lesion in the eminence (Figure 3a). There was an area in the posterior of the condylar head showing low signal intensity on the contrast-enhanced T1 weighted image (Figure 3b). The cortex and the bone marrow of the condylar head showed a normal signal intensity (Figures 1–3). T1 and T2 weighted images did not reveal any areas with low signal intensity in the joint spaces. Synovial chondromatosis was not suspected since there were no signs of calcification. Under the pre-operative diagnosis of a benign tumour, in November 2011, we started to perform surgery to remove the lesion. However, the intraoperative rapid diagnosis indicated that the tumour was malignant, and we had to discontinue the procedure. Histopathological analysis indicated osteosarcoma of the TMJ (Figure 4).
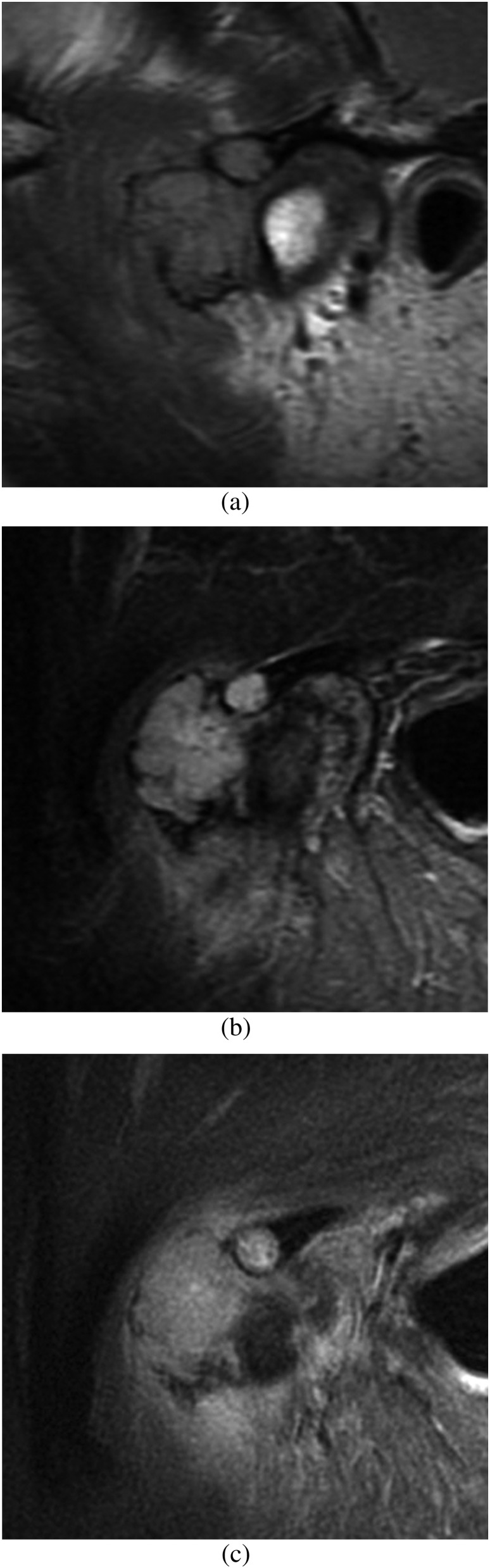
Figure 1.
MR images show a relatively well-defined lesion around the condylar head and in the eminence of the lateral part of the temporomandibular joint on the left side. (a) The lesion shows inhomogeneous intermediate signal intensity on T1 weighted image. (b) The lesion shows inhomogeneous intermediate signal intensity on T2 weighted image. (c) The lesion shows slight enhancement on the contrast-enhanced T1 weighted image.
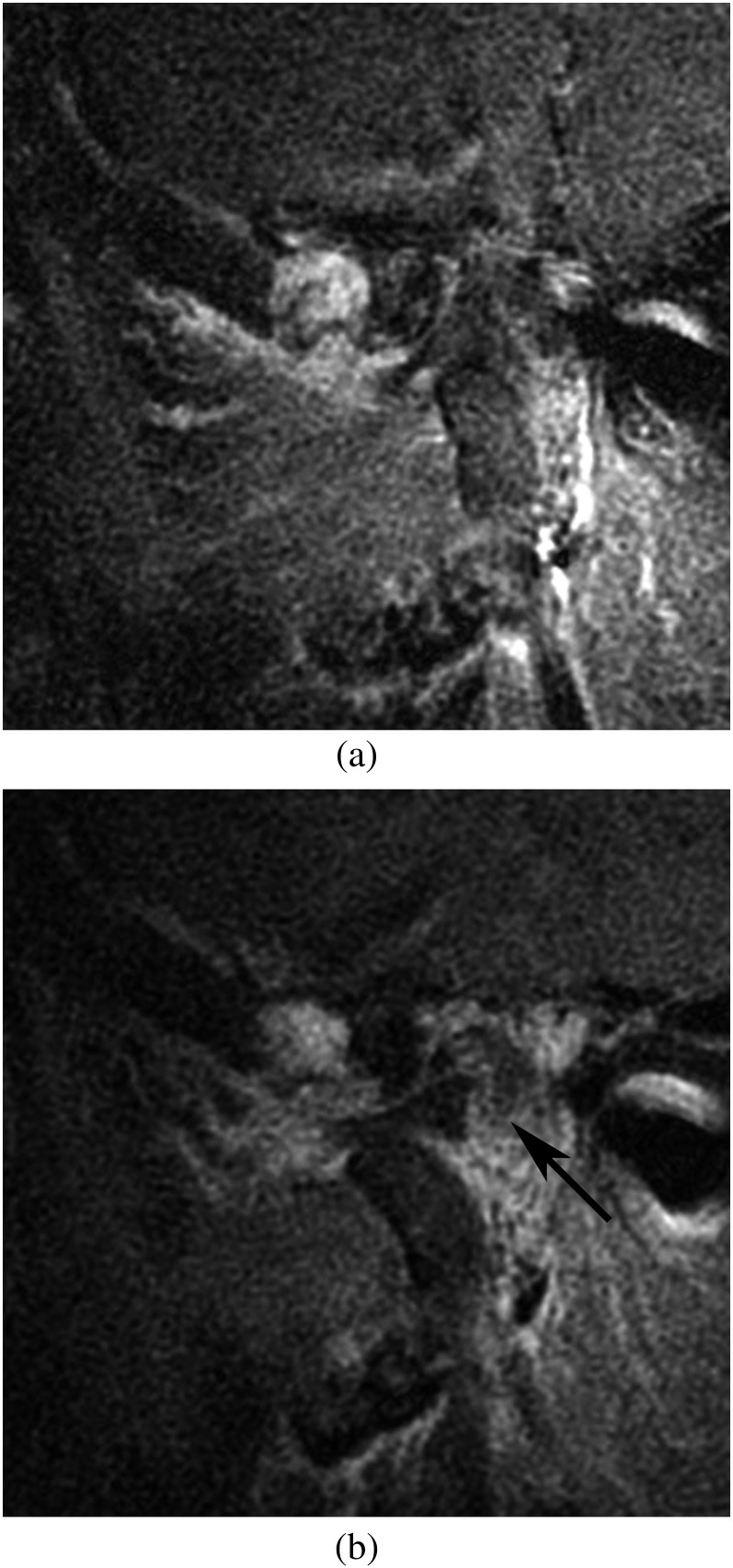
Figure 3.
MR images of the medial part of the temporomandibular joint. (a) The contrast-enhanced T1 weighted image shows no continuity between the lesion in the anterior of the condylar head and the eminence in the closed position. (b) Area in the posterior of the condylar head showing a low signal intensity on contrast-enhanced T1 weighted image (arrow).
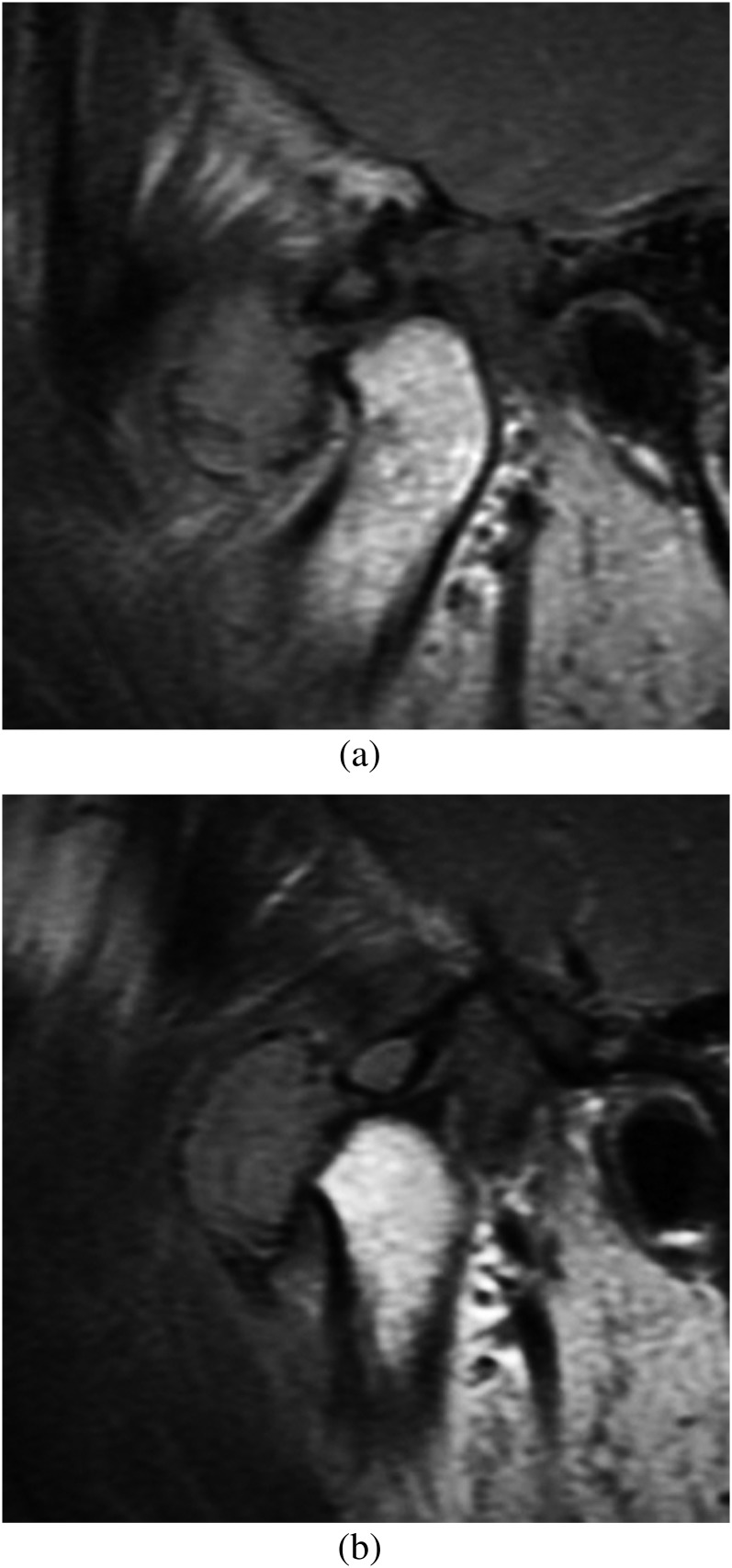
Figure 2.
The central part of the temporomandibular joint. (a) The disc position is normal on the T1 weighted image. The cortex and bone marrow of the condylar head appear normal on T1 weighted image. (b) The condylar head and the disc move under the eminence in the opened position.
Figure 4.
Chondroid matrix is predominant in the tumour. The tumour cells show variation in size and shape [haematoxylin and eosin; bar, 100 μm].
In January 2012, we performed boron neutron capture therapy (BNCT) because the lesion appeared to have invaded into the cranial base, and surgery was not considered an option. The patient is being followed up in the outpatient clinic without any signs of recurrence as of March 2013.
Discussion
Tumour and tumourous masses rarely arise as primary lesions in the TMJ. A mistaken diagnosis is often made since the patients with TMJ tumours present with unilateral facial swelling, external auditory canal obstruction or chronic TMJ dysfunction, which are also symptoms of more common disorders. The delay in diagnosis has been reported to range from 3 months to 8 years.5
Osteosarcoma is rare in the TMJ. A patient complaining of pain in the TMJ region will be diagnosed with a TMJ disorder. Our patient was initially diagnosed with a masticatory muscle disorder. The pain disappeared after administration of an analgesic drug, but the swelling increased. MRI using a TMJ coil demonstrated a relatively well-defined mass situated around the condylar head and in the eminence of the left TMJ. MRI using a TMJ coil showed that the disc position was normal, and the cortex and the bone marrow of the condylar head were normal. There were no areas with a low signal intensity on T1 and T2 weighted images in the joint spaces. There were no findings suspicious of calcifications. MRI is superior to CT in distinguishing the margins of the tumour. Periosteal new bone growth appears as a low intensity area on various MRI sequences.4 Thus, we did not suspect synovial chondromatosis or a lesion with osteoblastic reaction. Osteosarcoma resembling osteoblastoma or parosteal osteosarcoma might mimic benign bone growth, aggressive osteoblastoma or osteochondroma, but the presence of a soft-tissue component and bone marrow extension will be a clue.6
However, in our case, there was no bone marrow extension on the MR images and the lesion was relatively well defined. On the MR images, the lesion in the anterior of the condylar head did not show continuity with the lesion appearing in the eminence of the left TMJ (Figure 3). The presence of continuity would have been suggestive of intraosseous infiltration into the eminence, and the lesion might have been diagnosed as a malignant tumour.
dos Santos and Cavalcanti4 reported MR images of TMJ osteosarcoma obtained using a head coil but did not describe the disc or relationship between the disc and the condyle. Since we performed MRI using the TMJ coil with contrast enhancement, the MR images were acquired from the parasagittal of the condyle. The disc position was normal (Figure 2a), and the condylar head and the disc moved under the eminence in the mouth-opened position (Figure 2b). The upper and the lower joint spaces did not have any areas showing a low signal intensity (Figure 2). MRI using the TMJ coil was useful to demonstrate the disc, the relationship between the disc and the condyle, the movement of the disc and the joint spaces. MRI using a TMJ coil might be helpful in detecting lesions in the TMJ.
BNCT is a form of high linear energy transfer radiation therapy. With this type of treatment, high radiation doses can be selectively delivered to tumour cells without causing serious damage to the normal surrounding tissue, utilizing the high boron 10 (10B) accumulation that occurs in the tumour.7 For patients with the cancer infiltrating nerve or bone, it is difficult to be cured to get enough surgical margin, but BNCT makes it possible to be cured because of tumour selectivity.8 26 patients with head and neck malignancy, including sarcoma, were treated with BNCT. BNCT was effective in 22 of 26 patients.8 The lesion in this patient appeared to have invaded into the cranial base, and surgery was not considered an option. Thus, BNCT was selected to cure this patient. There were no signs of recurrence during the follow-up.
With BNCT, it was possible to preserve important structures and function. BNCT might be useful in treating tumour infiltrating important structures, and it might be considered to be good prognosis.
References
- 1.Bennett JH, Thomas G, Evans AW, Speight PM. Osteosarcoma of the jaws: a 30-year retrospective review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90: 323–33. [DOI] [PubMed] [Google Scholar]
- 2.Zorzan G, Tullio A, Bertolini F, Sesenna E. Osteosarcoma of the mandibular condyle: case report. J Oral Maxillofac Surg 2001; 59: 574–7. doi: 10.1053/joms.2001.22694 [DOI] [PubMed] [Google Scholar]
- 3.Bloem J, Bluemm RG, Taminiau AH, van Oosterom AH, Stolk J, Doornbos J. Magnetic resonance imaging of primary malignant bone tumors. Radiographics 1987; 7: 425–45. doi: 10.1148/radiographics.7.3.3482329 [DOI] [PubMed] [Google Scholar]
- 4.dos Santos DT, Cavalcanti MG. Osteosarcoma of the temporomandibular joint: report of 2 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 94: 641–7. [DOI] [PubMed] [Google Scholar]
- 5.Mostafapour SP, Futran ND. Tumors and tumorous masses presenting as temporomandibular joint syndrome. Otolaryngol Head Neck Surg 2000; 123: 459–64. doi: 10.1067/mhn.2000.109662 [DOI] [PubMed] [Google Scholar]
- 6.Lee YY, Van Tassel P, Nauert C, Raymond AK, Edeiken J. Craniofacial osteosarcomas: plain film, CT, and MR findings in 46 cases. AJR Am J Roentgenol 1988; 150: 1397–402. doi: 10.2214/ajr.150.6.1397 [DOI] [PubMed] [Google Scholar]
- 7.Aihara T, Morita N, Kamitani N, Kumada H, Ono K, Hiratsuka J, et al.. Boron neutron capture therapy for advanced salivary gland carcinoma in head and neck. Int J Clin Oncol June 2013. Epub ahead of print. doi: 10.1007/s10147-013-0580-3 [DOI] [PubMed] [Google Scholar]
- 8.Kato I, Fujita Y, Maruhashi A, Kumada H, Ohmae M, Kirihata M, et al.. Effectiveness of boron neutron capture therapy for recurrent head and neck malignancies. Appl Radiat Isot 2009; 67: S37–42. doi: 10.1016/j.apradiso.2009.03.103 [DOI] [PubMed] [Google Scholar]