Abstract
Objectives:
The aim of this prospective study was to compare dynamic and static sequences in the evaluation of temporomandibular joint disorders using a 3.0 -T imaging unit.
Methods:
194 patients were evaluated by static (double echo proton density weighted/turbo spin echo T2 weighted sequences) and dynamic (half-Fourier single-shot turbo spin echo sequences)imaging. Two radiologists evaluated in consensus the quality of images, the disc position and morphological alterations. The Kendall rank correlation coefficient (τ-b) was used to compare the qualitative rating between static and dynamic sequences. Cohen's kappa coefficient (k) was used to assess the agreement of disc position and morphological alterations between both sequences. The intraclass correlation coefficient was used to calculate the intraobserver variability. The significance was set at p ≤ 0.05.
Results:
The correlation between both sequences in the qualitative evaluation was τ-b = 0.632. The agreement between both techniques in the evaluation of disc position was k = 0.856. The agreement between both techniques in assessing the morphological alterations was k = 0.487. In the static sequences, the intraclass correlation coefficient was 0.915 in the qualitative evaluation, 0.873 in the evaluation of disc position and 0.934 in the assessment of morphological alterations. In the dynamic sequences, the intraclass correlation coefficient was 0.785 in the qualitative evaluation, 0.935 in the evaluation of disc position and 0.826 in the assessment of morphological alterations.
Conclusions:
Static imaging remains the gold standard in the evaluation of the temporomandibular joint. Dynamic imaging is a valuable tool that can provide additional information about topographic changes in the disc–condyle relationship.
Keywords: temporomandibular joint; temporomandibular joint disorders; magnetic resonance imaging; image interpretation, computer-assisted
Introduction
The use of different technologies in temporomandibular joint (TMJ) imaging is useful to define the morphology of anatomical structures and to detect several organic pathologies and dysfunctional phenomena.1,2 MRI allows acquisition of images in conditions such as complete occlusion, partial occlusion and disorders of opening of the mouth. To reproduce joint movements, several authors performed MRI examinations with static examinations of the joint in different positions during the various phases of the movement, rebuilding then the movement of opening and closing the mouth through dedicated cinematographic software.3–8 In these previous studies, cine MRI that relied on pseudodynamic images employing a bite block to control the mouth opening position for sequential step-by-step acquisitions was mostly used. The retrospective combination of images depicting static positions is physiologically not equivalent to the situation encountered during active jaw movement.
The long measuring times and cumbersome examinations, and the supine position, which is not physiological and could result in slight posterior displacement of the mandible, may also modify the examination results.9 Only recently have optimized sequences for the acquisition of dynamic images been used: echo planar imaging,9 true-fast imaging with steady-state precession10–12 and half-Fourier acquisition single-shot turbo spin echo (HASTE) sequences.13 These sequences assess the TMJ movement almost in real time, providing more reliable imaging than pseudodynamic sequences do.
High-field MRI with field strengths of 3.0 T has been increasingly used for clinical purposes and an increased signal-to-noise ratio (SNR) at 3.0 T was shown to improve the evaluation of anatomical structures.2
The aim of this study was to compare the dynamic single-shot turbo spin echo (TSE) MRI technique and proton density/TSE T2 weighted static imaging with a 3.0-T unit in the evaluation of TMJ disorders and morphological alterations.
Methods and materials
Patient population
To compare the dynamic single-shot TSE MRI technique and proton density/TSE T2 weighted static imaging, a prospective study was carried out between January 2008 and December 2012. The inclusion criteria were the presence of at least one of the following temporomandibular disorder symptoms: joint pain, sounds associated with jaw movement or limited mouth opening. Patients who underwent TMJ conservative or surgical therapy were excluded from the study. A total of 194 patients (388 TMJs) were included (46 males and 148 females; mean age, 33 years; range, 13–65 years).
MRI examinations were performed using a superconducting magnet of 3.0 T (Verio Magnetom®; Siemens Medical Solutions, Erlangen, Germany) with a double loop array coil.
All the patients were informed of the study protocol and signed an informed consent form. The study was approved by the local ethics committee and conducted in accordance with the Helsinki Declaration of 1975 as revised in 2000.
MRI acquisition protocol
The static imaging protocol consisted of separate sagittal oblique double echo proton density weighted/TSE T2 weighted sequences obtained in maximum open- and closed-mouthed positions. Open-mouthed imaging was performed using an intraoral device whose thickness was customized to the opening ability of patients. Images were angled perpendicular to the long axis of the condylar head, as determined from axial scout imaging, and were obtained with the following parameters: repetition time, 3500 ms; echo time, 15/102 ms; field of view (FOV), 154 × 160 mm; 15 sections of 2-mm thickness; flip angle, 150°; matrix, 256 × 256; and acquisition time 3:10 min.
For dynamic imaging, all patients were trained before the examination to perform a cycle of opening and closing of the mouth in a time of about 6 s. MR examination was performed with a sagittal HASTE sequence with the following parameters: repetition time, 1100 ms; echo time, 118 ms; FOV, 150 × 1550 mm; thickness, 6 mm; flip angle, 150°; matrix, 256 × 154; temporal resolution, 1.17 s per image. Images were acquired along the direct sagittal plane. The dynamic imaging scan consisted of continuous scanning for 16.5 s during slow opening and closing of the jaw (approximately 6 s per cycle of jaw opening and closing).
MRI interpretation
Two oral radiologists (both with 20 years' experience) evaluated static and dynamic MR images during four reading sessions independently and blinded to clinical symptoms. Any disagreement was solved by consensus. When it was not possible to find complete agreement between the two experts, a third oral radiologist was consulted.
First reading session
Each expert evaluated the quality of dynamic and static images, assigning a score to the conspicuity of the contours of the articular disc, mandibular condyle, articular eminence and lateral pterygoid muscle and to the presence of motion artefacts as described below:
• unclear contours: 1
• probable recognition of the contours: 2
• definite recognition of the contours: 3.
The presence of motion artefacts was rated as follows:
• severe artefacts: 1
• mild artefacts: 2
• none: 3.
The sum of the scores of each component determines, according to the following conversion table, the degree of image quality:
• score from 15 to 13: excellent
• score from 12 to 10: good
• score from 9 to 7: fair
• score <7: poor.
Second reading session
The disc position was evaluated in both sequences. The position of the disc was considered to be “normal” when the posterior band of the disc was located at the superior or 12 o'clock position relative to the condyle; “anterior disc displacement with reduction” (DDwR) when the disc was displaced anteriorly during the translation movement and returned to a normal position relative to the condyle during jaw opening and closing; or “anterior disc displacement without reduction” (DDw/oR) when the disc was displaced anteriorly and remained in a faulty position during all jaw movements.
Third reading session
The presence of joint effusion, retrodiscal tissue fibrosis and osteoarthrosis was assessed in both sequences. In an MRI T2 weighted image, an absence of high signal or the presence of a linear signal along the articular surface was defined as negative for joint effusion, whereas joint effusion was considered to be present when there was more than one line of high signal (spot intensity) inside the upper or lower joint compartment.14 Retrodiscal tissue fibrosis was determined by identifying an area of hypointense signalling in the joint space rear to the posterior band of the articular disc. Osteoarthrosis was defined by the presence of condylar deformities associated with flattening, subchondral sclerosis, surface irregularity, erosion and osteophyte presence.15
Fourth reading session
In the last reading session performed after 1 month, the specialists reassessed in consensus the quality of the images, disc position and morphological alterations in both techniques to calculate the intraobserver variability.
Statistical analysis
Data were evaluated using statistical analysis software (SPSS®; Statistical Package for Social Science, IBM Corporation, Armonk, NY).
The image quality (excellent, good, fair and poor), the disc displacement (normal, DDwR and DDw/oR) and the morphological alterations (joint effusion, retrodiscal fibrosis and osteoarthritis) were described with the frequency distribution.
The Kendall rank correlation coefficient (τ-b) was used to compare the score of the quality of static images with the score of the quality of dynamic images.
The Cohen's kappa coefficient (k) was used to assess the agreement between static and dynamic images in the evaluation of disc position and morphological alterations.
The Wilcoxon rank sum test was used to determine the level of significance between the outcomes of static and dynamic images in the evaluation of the quality of the images, disc displacement and morphological alterations.
The intraclass correlation coefficient (ICC) was used to calculate the intraobserver variability in the evaluation of the quality of the images, disc displacement and morphological alterations. A p ≤ 0.05 was considered significant.
Results
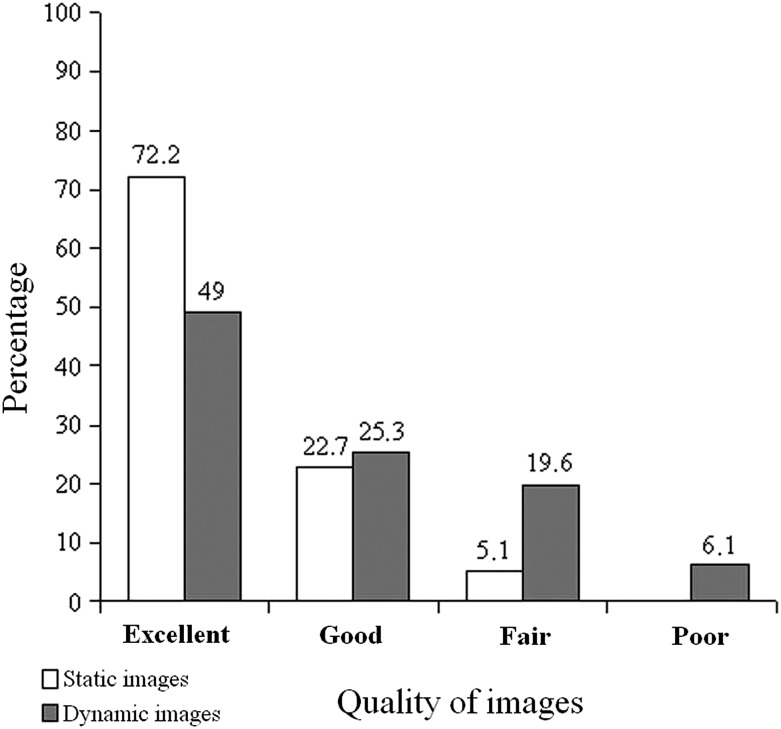
In the qualitative assessment, 280 (72.2%) excellent, 88 (22.7%) good, 20 (5.1%) fair and 0 poor images were rated in static sequences; 190 (49.0%) excellent, 98 (25.3%) good, 76 (19.6%) fair and 24 (6.1%) poor images were rated in dynamic sequences (Figure 1). The correlation between static and dynamic images in the qualitative evaluation was τ-b = 0.632 (p ≤ 0.001) and the level of significance found by the Wilcoxon rank sum test was p ≤ 0.001. The intraobserver variability was ICC = 0.915 in static and ICC = 0.785 in dynamic sequences.
Figure 1.
Frequency distribution of the qualitative rating in static and dynamic images.
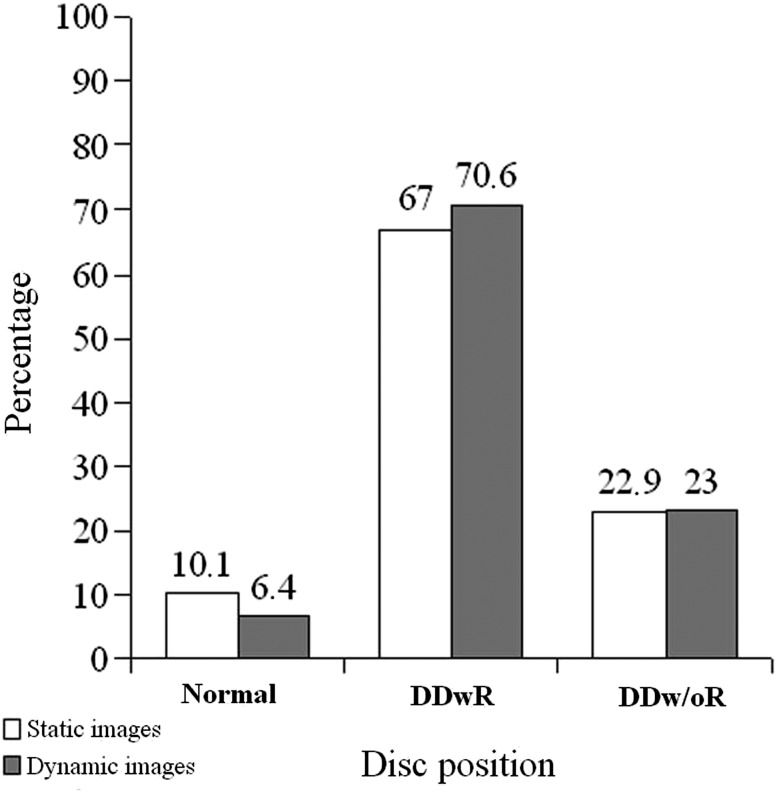
In the evaluation of disc position, 39 (10.1%) normal disc positions, 260 (67.0%) DDwR and 89 (22.9%) DDw/oR were found on static imaging; 25 (6.4%) normal disc positions, 274 (70.6%) DDwR and 89 (23.0%) DDw/oR were found on dynamic imaging (Figure 2). The agreement between static and dynamic images in the evaluation of disc position was k = 0.856 (95% confidence interval: 0.826–0.895, p ≤ 0.001) and the level of significance found by Wilcoxon rank sum test was p ≤ 0.44. The intraobserver variability was ICC = 0.873 in static and ICC = 0.935 in dynamic sequences.
Figure 2.
Frequency distribution of disc position in static and dynamic images. DDwR, anterior disc displacement with reduction; DDw/oR, anterior disc displacement without reduction.
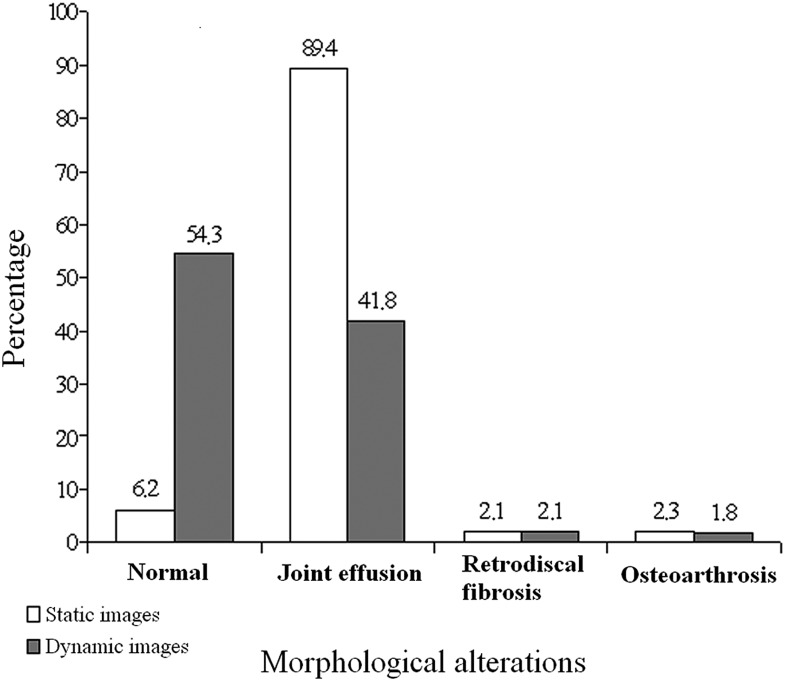
In the assessment of morphological alterations, 24 (6.2%) normal TMJs, 347 (89.4%) TMJs with joint effusion, 8 (2.1%) TMJs with retrodiscal fibrosis and 9 (2.3%) TMJs with osteoarthritis were detected on static imaging; 211 (54.3%) normal discs, 162 (41.8%) TMJs with joint effusion, 8 (2.1%) TMJs with retrodiscal fibrosis and 7 (1.8%) TMJs with osteoarthritis were identified on dynamic images (Figure 3). The correlation between static and dynamic images in the assessment of morphological alterations was k = 0.487 (95% confidence interval 0.446–0.528, p ≤ 0.001), and the level of significance found by Wilcoxon rank sum test was p ≤ 0.002. The intraobserver variability was ICC = 0.934 in static and ICC = 0.826 in dynamic sequences.
Figure 3.
Frequency distribution of morphological alterations in static and dynamic images.
Discussion
The dynamic evaluation of TMJ using MRI has been the object of several studies: the first movement simulations have been performed in 1987.3
Different imaging strategies have been utilized with seriated acquisitions of static images of TMJ during different stages of mouth opening, through the use of dedicated tools; the single snapshots were merged on a magnetic tape to project them (cine loop). Sequences such as gradient echo, gradient recalled acquisition in steady state, fast low angle shot MRI 20° have been utilized.3–8 These sequences were characterized by low SNR and low spatial resolution.
Recently, echo planar imaging, true-fast imaging with steady state precession and HASTE sequences have been used for dynamic real time TMJ MRI.
An improvement of the quality of the MRI of the TMJ can be achieved with the use of 3.0 T field strengths as a result of their higher SNR which increases the spatial resolution.16 The benefits of high field strengths have already been shown for examinations of different joints. In comparative studies of smaller joints, field strengths of 3.0 T were provided for superior quality vs a field strength of 1.5 T.17 Stehling et al18 showed a better visualization of the smaller TMJ structures at 3.0 T than 1.5 T. Schmid-Schwap et al19 found that with comparable examination sequences and identical resolution, the 3.0 T MRI of the TMJ provides a better perceptibility of the disc shape and disc position than the 1.5 T MRI
This prospective study was designed to compare dynamic and static sequences in the evaluation of TMJ at 3.0 T.
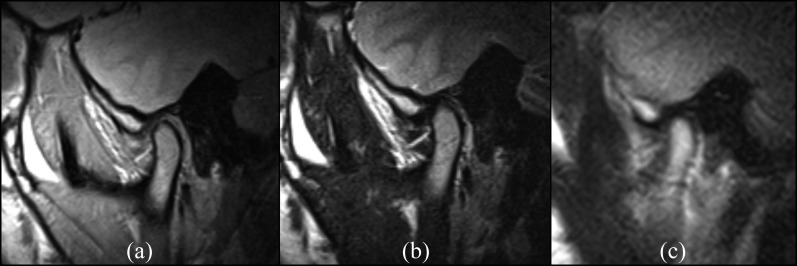
The HASTE sequence, owing to its smaller motion artefacts and a good spatial resolution achieved in a shorter acquisition time compared with true-fast imaging with steady-state precession MR images (16 s vs 34 s), was chosen for the MRI acquisition protocol. Despite the more reliable results obtained with HASTE dynamic sequences, the spatial resolution of the static sequences is nevertheless qualitatively superior (Figure 4). In the qualitative rating, the correlation between static and dynamic images was low (τ-b = 0.632) and with highly significant differences in the outcomes (Wilcoxon rank sum test p ≤ 0.001). A greater intraobserver variability was found in the evaluation of dynamic images than in the evaluation of static images (ICC = 0.785 vs ICC = 0.915). These results may be the result of lower spatial resolution and of a greater number of motion artefacts on the dynamic sequences, which increase the difficulty in the identification of different anatomical structures and in the overall evaluation of the images.
Figure 4.
Static proton density weighted (a), static turbo spin echo T2 weighted (b) and dynamic half-Fourier acquisition single-shot turbo spin echo (c) MR images of a 24-year-old female patient with disc displacement with reduction, obtained at closed-mouthed position, showing the higher quality of static sequences compared with dynamic ones in terms of spatial resolution. The contours of the articular disc, mandibular condyle, articular eminence, lateral pterygoid muscle and the cortical bone are better displayed in the static images than in the dynamic ones.
The lower spatial resolution of dynamic sequences may be caused by technical factors and by some issues related to the imaging acquisition mode. The technical factors include a greater slice thickness, a lower matrix size and a higher SNR. The issues related to imaging acquisition mode may be owing to the rotation movements of a patient's head while opening and closing the mouth during the acquisition time and the rotation and lateral movement of the disc during the opening of the mouth that may bring the disc out of the acquisition layer.
Anterior disc dislocation with reduction is the more frequent clinical manifestation of the temporomandibular disorders. This phase is characterized by the anteromedial dislocation of the articular disc and subsequent alteration of the relationship between the disc and condyle. During mouth closure, the condyle loses its contact with the articular disc and compresses the retrodiscal region. The loss of adhesion between the intermediate portion of the disc and the cartilaginous surface of the eminence determines the presence of synovial fluid in the joint space of a displaced disc. The joint effusion on T2 weighted MRI showed as an area of hyperintense signal.14
The assessment of the time of the articular disc recapture is important to set the relevant treatment plan. The prognosis of the joint disorder is less favourable if the disc is repositioned late in opening and early in closing movements. The use of dynamic sequences is needed to evaluate the time of articular disc recapture in DDwR.13 The static sequences instead are not able to analyse the movement of the TMJ because they can evaluate the disc location only in maximum open- and closed-mouthed positions (Figure 5).
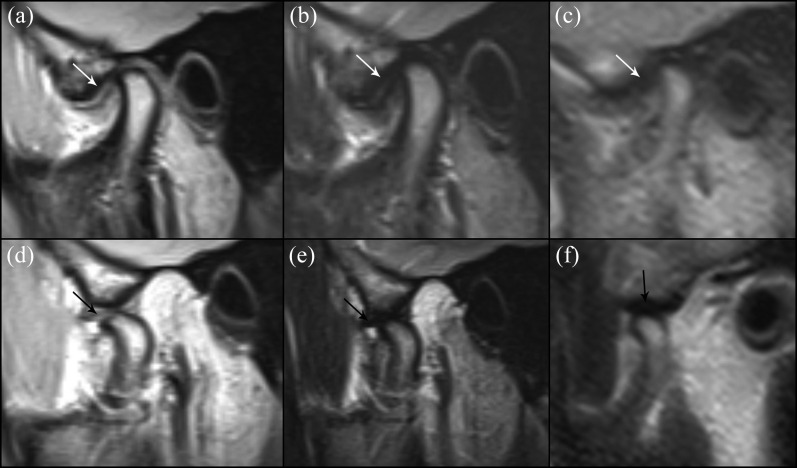
Figure 5.
MR images of a 36-year-old female patient complaining of joint pain and sounds associated with jaw movement. Static proton density weighted (a), static turbo spin echo T2 weighted (b) and dynamic half-Fourier acquisition single-shot turbo spin echo (HASTE) (c) MR images obtained at closed-mouthed position showing the disc displaced anteriorly to the condyle (white arrows). Static proton density weighted (d) and turbo spin echo T2 weighted (e) images obtained at open-mouthed position are doubtful because the disc seems to be not completely returned to its normal position relative to the condyle (black arrows). The assessment of dynamic HASTE sequences (f) resolves doubt, showing, at open-mouthed position, the correct relationship between the condyle and the disc with the condyle located below the eminence and the disc (black arrow) in its physiological position.
The role of dynamic sequences in the evaluation of displacement without reduction (closed lock) is less important than in rating the displacement with reduction because they do not add any important information. In the evaluation of disc position, a good agreement was found between static and dynamic imaging (k = 0.856), and a slightly higher intraobserver variability was observed in the dynamic images compared with static ones (ICC = 0.935 vs ICC = 0.873). This difference may be owing to the greater difficulty in the assessment of minimal anterior disc dislocations in static imaging without the possibility of evaluating the movement of the articular disc and to the greater accuracy in the evaluation of articular disc displacement in dynamic imaging.
In the evaluation of morphological alterations, a statistically significant low agreement (k = 0.487; Wilcoxon rank sum test p ≤ 0.002) between static and dynamic images was found. In the assessment of the frequency distribution, a comparable percentage of TMJs with retrodiscal fibrosis and osteoarthritis was reported. These results highlight how the TMJ degenerative diseases can be identified by sequences without a high spatial resolution (Figure 6). Conversely, in the evaluation of joint effusion (Figure 7), a higher incidence of TMJs with joint effusion in static images compared with dynamic images was found (89.4% vs 41.8%). This finding may be due to a lower contrast resolution of dynamic images.
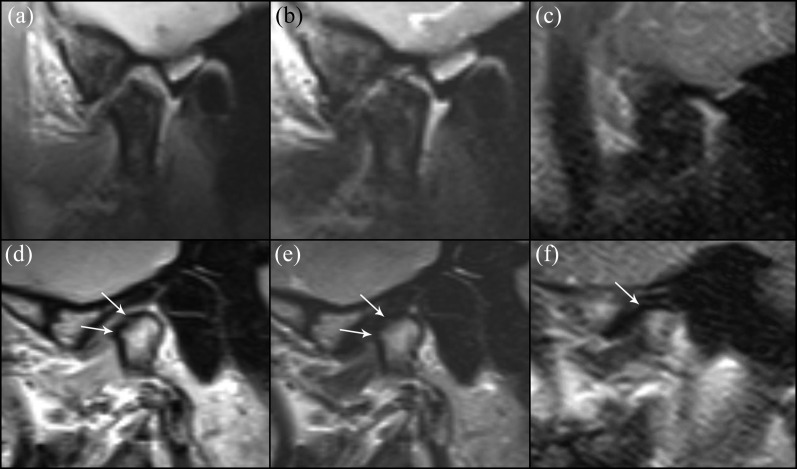
Figure 6.
(a–c) MR images obtained at open-mouthed position of a 49-year-old female patient with disc displacement with reduction, complaining of joint pain, sounds associated with jaw movement and limited mouth opening. Static proton density weighted (a) and turbo spin echo T2 weighted (b) images show a morphostructural alteration of the ramus of the mandible, of the condyle and of the tubercle eminence, which appear enlarged with a widespread low signal intensity; these findings are less depicted in the dynamic half-Fourier acquisition single-shot turbo spin echo (HASTE) image (c). (d–f) MR images obtained at closed-mouthed position of a 53-year-old female patient with disc displacement with reduction, complaining of joint pain and limited mouth opening. Static proton density weighted (d) and turbo spin echo T2 weighted (e) images show an irregular surface of the condylar head with tiny osteophytes at the upper and anterior edge (white arrows). Dynamic HASTE (f) image shows a lesser definition of the contours of the condylar head and the tiny osteophytes are not well identified (white arrow).
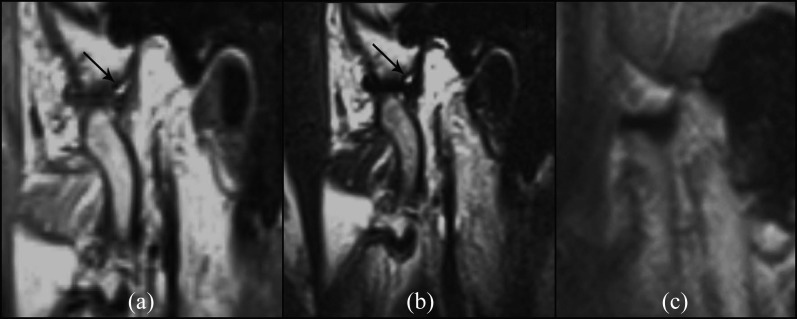
Figure 7.
Static proton density weighted (a), static turbo spin echo T2 weighted (b) and dynamic half-Fourier acquisition single-shot turbo spin echo (c) MR sequences of a 33-year-old female patient with disc displacement with reduction, obtained at open-mouthed position. Static images show a joint effusion in the posterior recesses of the temporomandibular joint, depicted as areas of hyperintense signal (black arrows); no areas of hyperintense signal within the temporomandibular joint are seen in the dynamic image.
Conclusion
Static MRI remains the gold standard in TMJ assessment and in the evaluation of TMJ structural alterations (joint effusion, retrodiscal tissue fibrosis and osteoarthrosis) and functional diseases (disc displacement with or without reduction), because of its high quality of images in terms of spatial resolution. Dynamic MRI, however, provides additional information about topographic changes in the disc–condyle relationship during the mouth opening movement.
The information given by dynamic images, acquired with only a few additional minutes of scanning, is a valuable tool to supplement static MRI in the decision-making of a treatment plan and in rating the prognosis of TMJ diseases.
References
- 1.Mazza D, Marini M, Impara L, Cassetta M, Scarpato P, Barchetti F, et al. Anatomic examination of the upper head of the lateral pterygoid muscle using magnetic resonance imaging and clinical data. J Craniofac Surg 2009; 20: 1508–11. doi: 10.1097/SCS.0b013e3181b09c32 [DOI] [PubMed] [Google Scholar]
- 2.Cassetta M, Di Carlo S, Pranno N, Stagnitti A, Pompa V, Pompa G. The use of high resolution magnetic resonance on 3.0-T system in the diagnosis and surgical planning of intraosseous lesions of the jaws: preliminary results of a retrospective study. Eur Rev Med Pharmacol Sci 2012; 16: 2021–8. [PubMed] [Google Scholar]
- 3.Burnett KR, Davis CL, Read J. Dynamic display of the temporomandibular joint meniscus by using “fast-scan” MR imaging. AJR Am J Roentgenol 1987; 149: 959–62. doi: 10.2214/ajr.149.5.959 [DOI] [PubMed] [Google Scholar]
- 4.Yoshida H, Hirohata H, Onizawa K, Niitsu M, Itai Y. Flexure deformation of the temporomandibular joint disk in pseudodynamic mangnetic resonance images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89: 104–11. [DOI] [PubMed] [Google Scholar]
- 5.Conway WF, Hayes CW, Campbell RL. Dynamic magnetic resonance imaging of the temporomandibular joint using FLASH sequences. J Oral Maxillofac Surg 1988; 46: 930–8. [DOI] [PubMed] [Google Scholar]
- 6.Behr M, Held P, Leibrock A, Fellner C, Handel G. Diagnostic potential of pseudo-dynamic MRI (CINE mode) for evaluation of internal derangement of the TMJ. Eur J Radiol 1996; 23: 212–15. [DOI] [PubMed] [Google Scholar]
- 7.Manière-Ezvan A, Havet T, Franconi JM, Quémar JC, de Certaines JD. Cinematic study of temporomandibular joint motion using ultrafast magnetic resonance imaging. Cranio 1999; 17: 262–7. [DOI] [PubMed] [Google Scholar]
- 8.Eberhard D, Bantleon PH, Steger W. Functional magnetic resonance imaging of temporomandibular joint disorders. Eur J Orthod 2000; 22: 489–97. [DOI] [PubMed] [Google Scholar]
- 9.Chen YJ, Gallo LM, Meier D, Palla S. Dynamic magnetic resonance imaging technique for the study of the temporomandibular joint. J Orofac Pain 2000; 14: 65–73. [PubMed] [Google Scholar]
- 10.Abolmaali ND, Schmitt J, Schwarz W, Toll DE, Hinterwimmer S, Vogl TJ. Visualization of the articular disk of the temporomandibular joint in near-real-time MRI: feasibility study. Eur Radiol 2004; 14: 1889–94. doi: 10.1007/s00330-004-2418-x [DOI] [PubMed] [Google Scholar]
- 11.Shimazaki Y, Saito K, Matsukawa S, Onizawa R, Kotake F, Nishio R. Image quality using dynamic MR imaging of the temporomandibular joint with true-FISP sequence. Magn Reson Med Sci 2007; 6: 15–20. [DOI] [PubMed] [Google Scholar]
- 12.Yen P, Katzberg RW, Buonocore MH, Sonico J. Dynamic MR imaging of the temporomandibular joint using a balanced steady-state free precession sequence at 3T. AJNR Am J Neuroradiol 2013; 34: E24–6. doi: 10.3174/ajnr.A2734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang EY, Mulholland TP, Pramanik BK, Nusbaum AO, Babb J, Pavone AG. Dynamic sagittal half-Fourier acquired single-shot turbo spin-echo MR imaging of the temporomandibular joint: initial experience and comparison with sagittal oblique proton-attenuation images. AJNR Am J Neuroradiol 2007; 28: 1126–32. doi: 10.3174/ajnr.A0487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Westesson PL, Brooks S. Temporomandibular joint: relationship between MR evidence of effusion and the presence of pain and disk displacement. AJR Am J Roentgenol 1992; 159: 559–63. doi: 10.2214/ajr.159.3.1503025 [DOI] [PubMed] [Google Scholar]
- 15.Tasaki MM, Westesson PL. Temporomandibular joint: diagnostic accuracy with sagittal and coronal MR imaging. Radiology 1993; 186: 723–9. doi: 10.1148/radiology.186.3.8430181 [DOI] [PubMed] [Google Scholar]
- 16.Trattnig S, Pinker K, Ba-Ssalamah A, Nöbauer-Huhmann IM. The optimal use of contrast agents at high field MRI. Eur Radiol 2006; 16: 1280–7. doi: 10.1007/s00330-006-0154-0 [DOI] [PubMed] [Google Scholar]
- 17.Wieners G, Detert J, Streitparth F, Pech M, Fischbach F, Burmester G, et al. High resolution MRI of the wrist and finger joints in patients with rheumatoid arthritis: comparison of 1.5 Tesla and 3.0 Tesla. Eur Radiol 2007; 17: 2176–82. doi: 10.1007/s00330-006-0539-0 [DOI] [PubMed] [Google Scholar]
- 18.Stehling C, Vieth V, Bachmann R, Nassenstein I, Kugel H, Kooijman H, et al. High resolution magnetic resonance imaging of the temporomandibular joint: image quality at 1.5 and 3.0 Tesla in volunteers. Invest Radiol 2007; 42: 428–34. doi: 10.1097/01.rli.0000262081.23997.6b [DOI] [PubMed] [Google Scholar]
- 19.Schmid-Schwap M, Drahanowsky W, Bristela M, Kundi M, Piehslinger E, Robinson S. Diagnosis of temporomandibular dysfunction syndrome–image quality at 1.5 and 3.0 Tesla magnetic resonance imaging. Eur Radiol 2009; 19: 1239–45. doi: 10.1007/s00330-008-1264-7 [DOI] [PubMed] [Google Scholar]