Abstract
Objectives:
Oral submucous fibrosis (OSMF) is an insidious chronic disease that is associated with significant functional morbidity and an increased risk for malignancy. It initially affects the lamina propria of the oral mucosa, and, as the disease progresses, it involves the submucosa and deeper tissue, including muscles of the oral cavity, resulting in loss of fibroelasticity. OSMF is a pre-malignant condition mainly caused by areca nut chewing. The aim of this study was to find out the involvement of muscles of mastication and facial expression in patients with OSMF by assessing the cross-sectional thickness and activity of the masseter, anterior temporalis and orbicularis oris muscles by ultrasonography and electromyography and comparing with healthy controls and also to find out any correlation between the ultrasonographic cross-sectional thicknesses of the masseter, anterior temporalis and orbicularis oris muscles with electromyographic activity.
Methods:
40 patients with OSMF were included in the study group, and the patients were divided into four groups on the basis of interincisal mouth opening, i.e. Group I (mouth opening >35 mm), Group II (mouth opening between 30 and 35 mm), Group III (mouth opening between 20 and 30 mm) and Group IV (mouth opening <20 mm). Ultrasonographic cross-sectional thickness and electromyographic activity (amplitude and duration) of the masseter, anterior temporalis and orbicualris oris muscles were recorded in patients with OSMF and 20 controls. Intergroup comparison of ultrasonographic cross-sectional thickness and activity (amplitude and duration) was done, and Pearson's correlation coefficient was applied to find out any relation between ultrasonographic and electromyographic findings.
Results:
Thickness and activity of the masseter muscle was significantly reduced in Group IV (mouth opening <20 mm) when compared with the control group. The anterior temporalis and orbicularis oris muscles remained unaffected. A positive correlation was observed between the thicknesses of the masseter muscle and the amplitude in Groups I, II and III; the anterior temporalis muscle in Group II and the control group; and the orbicularis oris muscle in Groups II, III and IV.
Conclusions:
It was concluded that, among the muscles studied, there was an early involvement of the masseter muscle in patients with OSMF compared with that of other muscles.
Keywords: OSMF, ultrasonography, electromyography
Introduction
Oral submucous fibrosis (OSMF) is as an insidious chronic disease affecting any part of the oral cavity and sometimes the pharynx. Although occasionally preceded by and/or associated with vesicle formation, it is always associated with a juxta-epithelial inflammatory reaction followed by fibroelastic change of the lamina propria, with epithelial atrophy leading to stiffness of the oral mucosa and causing trismus and an inability to eat.1 The earliest report on muscle involvement in OSMF was by Binnie and Cawson;2 they reported a homogeneous collagenous subepithelial zone along with degeneration of muscle fibres. El-Labban and Caniff,3 on the basis of electron microscopic observations, reported muscle degeneration in OSMF, the extent of which significantly affects the already existing trismus in these patients. Based on histopathological observations, Khanna and Andrade4 reported thickened and dense collagen fibres interspersed with muscle fibres in moderately advanced cases of OSMF with interincisal distance of 15–25 mm, and they also observed extensive degeneration of muscle fibres in advanced cases with pre-malignant and malignant changes (interincisal distance < 15 mm). Based on the severity of trismus and the histopathological findings of secondary muscle degeneration and fibrosis in Groups III and IV, they defined OSMF as “a chronic, progressive premalignant condition, with juxtaepithelial deposition of fibrotic tissue followed by muscular degeneration and limitation in oral opening”.
Arecoline, an alkaloid component of the areca nut, stimulates fibroblastic proliferation and collagen synthesis.5–7 The flavanoid (+)-catechin and tannins are responsible for the stabilization of collagen fibrils, rendering them resistant to degradation by collagenase.5,8,9 The attendant trismus is the result of juxtaepithelial hyalinization and secondary muscle involvement (i.e. muscular degeneration and fibrosis).4 Gollnick et al10 stated that glycogen consumption is physiologically related to cellular activity. Overactivity of the muscle results in excessive glycogen consumption, leading to glycogen depletion. The increased muscle activity and diminished blood supply following connective tissue changes owing to extensive OSMF leads to muscle degeneration and fibrosis.4
The thickness and functions of the muscles of the head and neck can be assessed by various modalities. In recent studies, ultrasonography has been used for the evaluation of the cross-sectional dimensions of the muscles of the head and neck. Ultrasonography is uncomplicated and represents considerable improvement relative to conventional methods for assessing muscle thickness, particularly in terms of clinical availability and cost. Electromyographic activity of the masticatory muscles has been widely studied in clinical work and research.11 Electromyographic changes provide information regarding the electrical activity of muscles, thus supplementing the clinical biochemical investigations in the diagnosis of muscle diseases. Since electromyographic examination can sample a large number of muscles, it has a distinct advantage over histopathological studies, which represent the changes at one site only.12
In the present study, an attempt has been made to determine the involvement of muscles of mastication (the masseter and the anterior temporalis) and of facial expression (the orbicularis oris) in OSMF by assessing the cross-sectional thickness and activity of these muscles by non-invasive procedures, such as ultrasonography and electromyography, and comparing them with healthy controls. The objectives of this study were to evaluate and compare the cross-sectional thickness and activity (amplitude and duration) of the masseter, anterior temporalis and orbicularis oris muscles in patients with OSMF and healthy controls by ultrasonography and electromyography and to find out whether there is any correlation between the ultrasonographic cross-sectional thicknesses of the masseter, anterior temporalis and orbicularis oris muscles and the electromyographic activity.
Methods and Materials
This study was conducted in the Department of Oral Medicine and Radiology, Sharad Pawar Dental College and Hospital, Sawangi (Meghe), Wardha, India, after approval from the institutional ethics committee.
40 patients, aged 18–50 years, with signs and symptoms of OSMF were included in the study group. The patients were randomly assigned to the study groups. 20 age- and sex-matched healthy volunteers free from betel nut with or without tobacco chewing habit and interincisal mouth opening >35 mm were randomly assigned to the control group.
Patients with infections and inflammatory causes of trismus, intra-articular causes of trismus, myofascial pain dysfunction syndrome, dermatomyositis and myositis ossificans (facial muscles and muscles of mastication), temporomandibular joint arthritis and arthralgia and scleroderma were excluded from the study.
A detailed history of the patients was recorded, with special reference to the habit of chewing betel nut with or without tobacco. The patients were asked about the type of betel nut and tobacco consumed, duration of the habit and the amount of tobacco or betel nut consumed per day as per a structured pro forma. They were informed about the study procedure, and informed consent was obtained on an institutionally approved document.
A thorough clinical examination of all the patients was carried out, which included examining the oral cavity of the patients for findings such as blanching of the oral mucosa; ulceration of the oral mucosa; cheek flexibility; tongue movement in anterior, side-to-side and upward directions; and shrunken and atrophic uvula and palpatory findings such as the presence of fibrous bands in the buccal mucosa, upper and lower labial mucosa, hard and soft palate and floor of the mouth.
A total of 12 oral sites were clinically examined in all the patients, which included checking the patient for the presence of a shrunken uvula, restricted tongue movements, the presence of fibrous bands in the right and left buccal mucosa, retromolar region (right and left), upper and lower labial mucosa, hard and soft palate and floor of the mouth. The total number of clinically involved sites was recorded in all the patients.
The data obtained were entered in the structured pro forma for recording clinical findings, and a final diagnosis of OSMF was made. Histopathological confirmation of OSMF was not done, as the clinical manifestations, i.e. blanching and stiffening of the oral mucosa leading to the limitation of mouth opening and the presence of fibrous bands in the lips and cheeks, are a hallmark of the disease.
According to the criteria of Lai et al,13 the patients were divided into four groups on the basis of interincisal mouth opening, i.e. Group I (mouth opening >35 mm), Group II (mouth opening between 30 and 35 mm), Group III (mouth opening between 20 and 30 mm) and Group IV (mouth opening <20 mm).
After this, the patients were subjected to ultrasound imaging and electromyography for recording the cross-sectional thickness and activity (amplitude and duration) of the masseter, anterior temporalis and orbicualris oris muscles. The patients were instructed not to chew betel nut in any form for a period of 2 h before ultrasonographic and electromyographic examination.
Recording of muscle thickness
Real-time imaging of the cross-sectional thickness was done by ultrasound unit (EnVisor C version CO2; Philips, Zofingen, Switzerland) using a 15-MHz linear-phased array transducer (s42; Philips, Zofingen, Switzerland). Scanning was done in the supine position with the head turned sideways to provide good access for the probe. A transducer was placed in contact with the skin after applying an ultrasound gel.
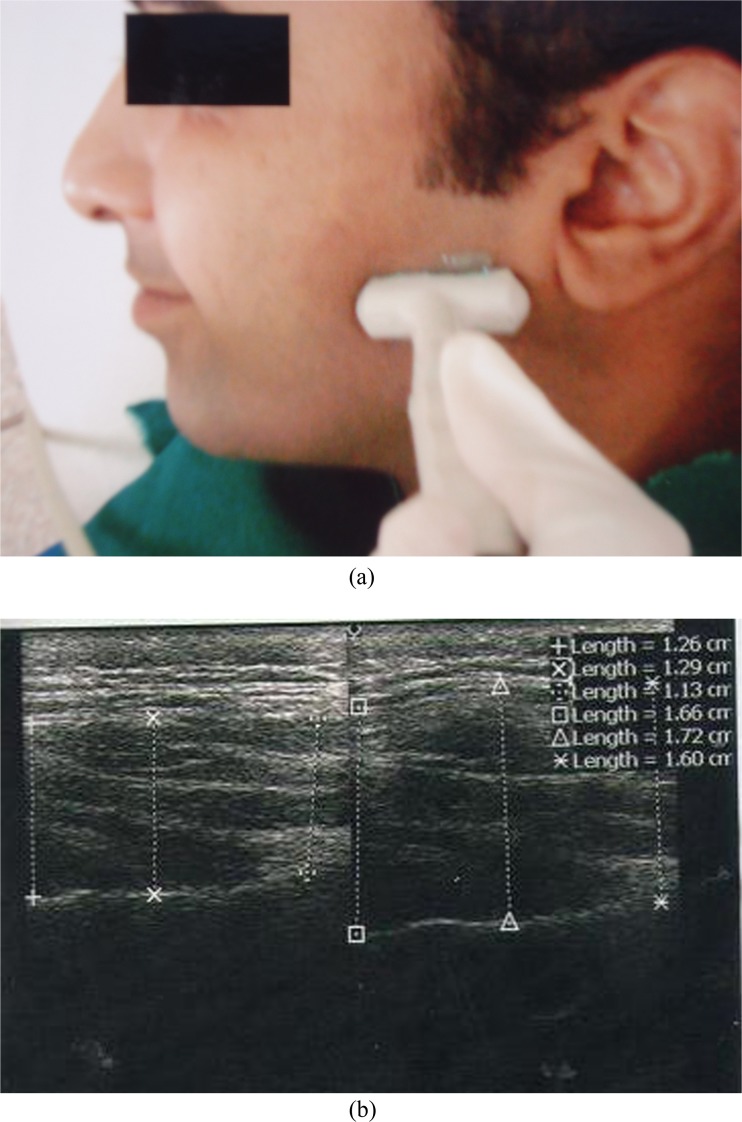
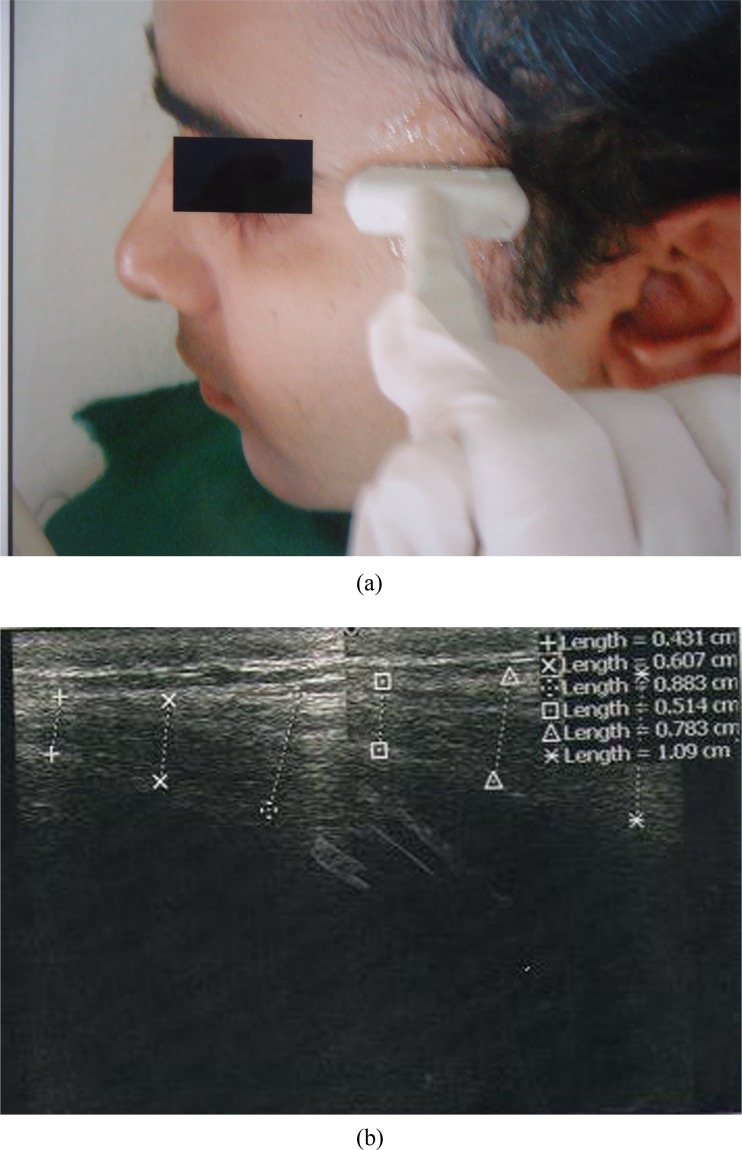
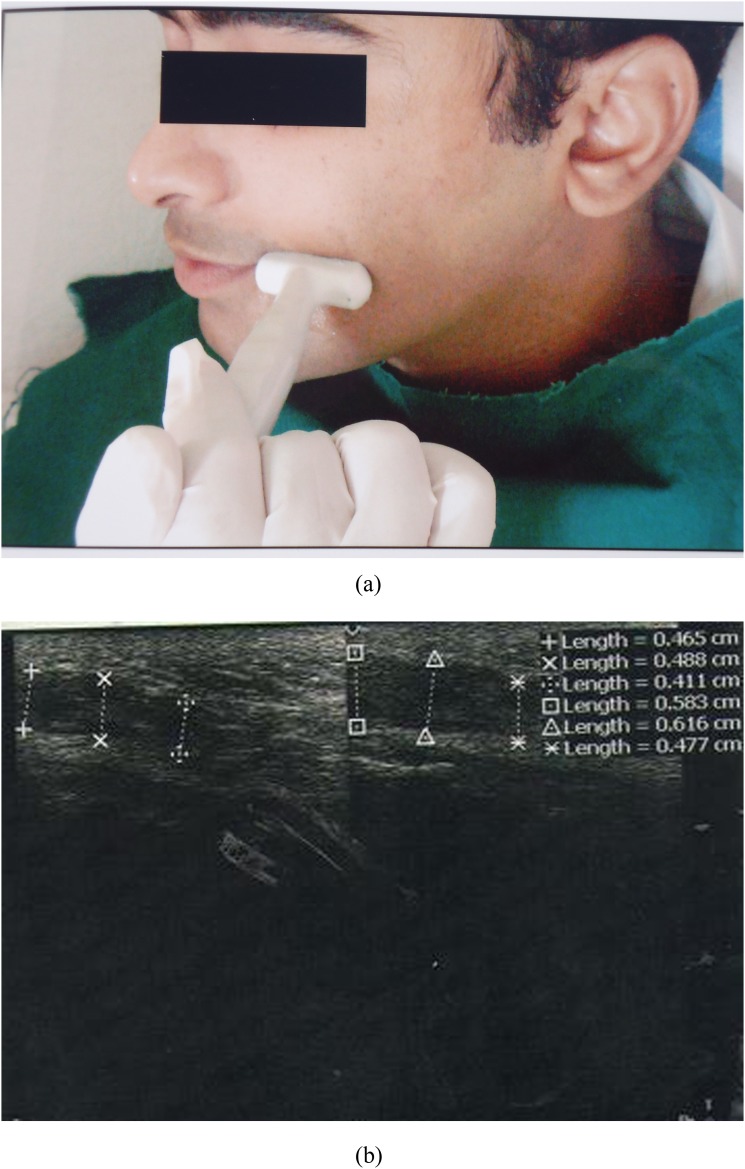
For the masseter muscle, the transducer was oriented perpendicular to the ramus corresponding to the bulkiest part of the superficial portion of the masseter muscle. The site of measurement was in the thickest part of the masseter muscle, close to the level of the occlusal plane, approximately in the middle of the mediolateral distance of the ramus (Figure 1a,b). For the anterior temporalis muscle, the transducer was oriented in front of the anterior border of the hairline (Figure 2a,b). For the orbicularis oris muscle, the transducer was placed near the angle of the mouth in each subject (Figure 3a,b). The real-time imaging of these three muscles was performed bilaterally in both the relaxed and contracted states.
Figure 1.
(a) Ultrasound transducer position for the masseter muscle. (b) Ultrasound image showing the cross-sectional thickness of the masseter muscle in the relaxed and contracted state.
Figure 2.
(a) Ultrasound transducer position for the anterior temporalis muscle. (b) Ultrasound image showing the cross-sectional thickness of the anterior temporalis muscle in the relaxed and contracted state.
Figure 3.
(a) Ultrasound transducer position for the orbicularis oris muscle. (b) Ultrasound image showing the cross-sectional thickness of the orbicularis oris muscle in the relaxed and contracted state.
For the masseter muscle, the relaxed state was achieved by asking the patient to occlude the teeth gently, and to achieve the contracted state, the patient was asked to clench his or her teeth in the maximum intercuspal position and hold for 3–4 s until the image was registered on the monitor.14
To achieve the relaxed state of the anterior temporalis muscle, the patient was instructed to maintain slight interocclusal contact, and to achieve the contracted state, the patient was asked to clench his or her teeth in the maximum intercuspal position and hold for 3–4 s until the image was registered on the monitor.14
To achieve the relaxed state of the orbicularis oris muscle, the patient was instructed to keep his or her lips in the normal position, and to achieve the contracted state, the patient was asked to smile and hold for 3–4 s until the image was registered on the monitor.
After the image was registered on the monitor, the image of the muscle was evaluated using an electronic caliper available within the software of the ultrasound unit. After the electronic caliper dots appeared in the scan, the thickness of the muscles was recorded in millimetres at the three sites in a standardized manner, and the thickness per side was calculated as the average of the three measurements.
Recording of muscle activity
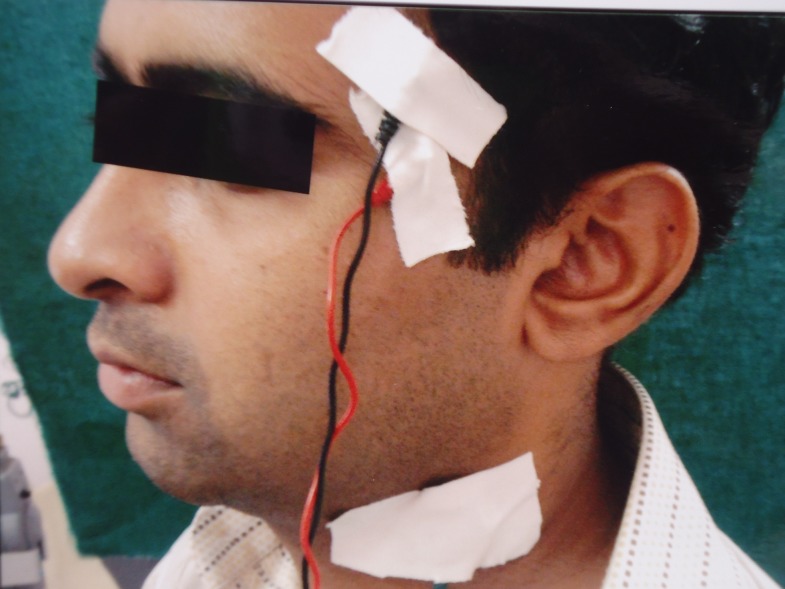
Electromyographic recording was done using an RMS (Recorders & Medicare Systems Pvt Ltd, Haryana, India) digitized polygraph, Polyrite D system (including both hardware and software). The subjects were asked to sit upright with their head in the natural position. Then, the skin was cleaned with cotton swabs soaked in 70% alcohol. Electrodes were placed by applying a small amount of electromyographic gel (RMS Kondukt gel) on the recording site. A set of two silver–silver chloride surface electrodes (black, active electrode; red, reference electrode) were held in position with collodion adhesive. The electrode pair was placed at 3–4 mm interelectrode distance. The paired electrodes act as exploring electrodes for electromyographic recording. One ground electrode (green) was attached on the lateral side of the neck.
For the masseter muscle, the site of measurement was in the thickest part of the muscle, close to the level of the occlusal plane, approximately in the middle of the mediolateral distance of the ramus (Figure 4). For the anterior temporalis muscle, the electrodes were placed in front of the anterior border of the hairline (Figure 5). For the orbicularis oris muscle, the electrodes were placed near the angle of the mouth (Figure 6). Muscle activity was recorded in the relaxed state and the maximum voluntary contracted state. The relaxed and contracted states of all three muscles were achieved as described previously. All the muscles were electrically silent in the relaxed state. The amplitude was recorded in microvolts and the duration was recorded in milliseconds.
Figure 4.
Electromyography surface electrode position for the masseter muscle.
Figure 5.
Electromyography surface electrode position for the anterior temporalis muscle.
Figure 6.
Electromyography surface electrode position for the orbicularis oris muscle.
Ultrasonographic cross-sectional thickness and the electromyographic activity of 240 muscles were recorded in the study groups (6 muscles from each patient) and 120 muscles in the control group (6 muscles from each subject). 2880 recordings for the ultrasonographic cross-sectional thickness (relaxed and contracted state) and 1440 recordings of the electromyographic activity (contracted state) were performed in patients with OSMF, and 1440 ultrasonographic recordings and 720 electromyographic recordings were performed in the control group of the present study.
Data analysis
Observations of the cross-sectional thickness of the masseter, anterior temporalis and orbicularis oris muscles in the relaxed and contracted states were recorded in millimetres, muscle activity in microvolts and duration in milliseconds and were statistically analysed to determine whether there were any significant differences between the four study groups and the control group. The calculation of mean, standard deviation and standard error was carried out for all the groups in this study. Intergroup comparison of muscle thickness and activity (amplitude and duration) was performed using Student's paired and unpaired t-tests.
Variations in the thickness (relaxed and contracted state) and activity (contracted state) of the masseter, anterior temporalis and orbicularis oris muscles between groups and within groups on the right and left sides were evaluated using ANOVA.
The Dunnett test is used to investigate the significance of the differences when several groups are compared with the control. In this study, this test was applied to find out significant differences in the thickness (relaxed and contracted state) and activity (contracted state) of the masseter, anterior temporalis and orbicularis oris muscles bilaterally on the right and left sides in all the four study groups compared with the control group.
Correlation between muscle thickness and activity was estimated using Pearson's correlation coefficient (r). A positive value of r was considered as significant.
Results and observations
A total of 40 patients with OSMF were included in the study group, and the control group included 20 subjects. In the present study, the male to female ratio was 39:1. This is because of the decreased prevalence of betel nut with or without pan chewing habit in females. The mean ± standard deviation (SD) of the age of the patients included in the study group ranged from 24.70 ± 2.21 to 27.80 ± 5.99 years (Table 1). As the severity of the disease increased, the mean mouth opening decreased from 38.90 ± 3.34 mm in Group I to 16.60 ± 3.77 mm in Group IV (Table 1). The most prevalent habit in all the 4 groups was kharra chewing (i.e. 19 patients); 4 patients had the habit of gutkha chewing; 7 patients had the combined habit of kharra and gutkha chewing; 1 patient had the habit of areca nut chewing; and 9 patients had mixed habits (Table 2). The number of clinically involved oral sites increased from Group I to Group IV (Table 3).
Table 1.
Mean ± standard deviation (SD) of the age and interincisal mouth opening in all the groups
| Group | Mean ± SD age (years) | Mean ± SD interincisal mouth opening (mm) |
|---|---|---|
| I | 27.80 ± 5.99 | 38.90 ± 3.34 |
| II | 25.20 ± 9.13 | 32.20 ± 1.31 |
| III | 24.70 ± 2.21 | 24.80 ± 2.78 |
| IV | 26.80 ± 7.94 | 16.60 ± 3.77 |
| Control | 22.25 ± 2.02 | 52.70 ± 5.28 |
Table 2.
Group-wise distribution of types of habit in Groups I–IV
| Habit | Group I | Group II | Group III | Group IV | Total |
|---|---|---|---|---|---|
| Kharaa (AN + T + L) | 6 | 6 | 2 | 5 | 19 |
| Gutkha (AN + T) | 1 | 1 | 2 | – | 4 |
| Kharaa (AN + T + L) + gutkha (AN + T) | 1 | 1 | 3 | 2 | 7 |
| Pan masala (AN + T) + tobacco + lime (T + L) | 1 | – | – | – | 1 |
| Kharaa (AN + T + L) + gutkha (AN + T) +tobacco + lime (T + L) + bidi | 1 | – | – | – | 1 |
| Kharaa (AN + T + L) + gutkha (AN + T) +tobacco + lime (T + L) | – | 1 | – | – | 1 |
| Kharaa (AN + T + L) + gutkha (AN + T) +tobacco + lime (T + L) + snuff | – | – | – | – | – |
| Kharaa (AN + T + L) + gutkha (AN + T) +snuff | – | 1 | 1 | 1 | 3 |
| Kharra (AN + T + L) + tobacco + lime + bidi | – | – | 1 | – | 1 |
| Kharaa (AN + T + L) + snuff | – | – | 1 | – | 1 |
| Kharaa (AN + T + L) + tobacco + lime (T + L) | – | – | – | 1 | 1 |
| AN | – | – | – | 1 | 1 |
AN, areca nut; L, lime; T, tobacco.
Table 3.
Group-wise distribution of clinically involved oral sites in Groups I–IV
| Sites | Group I | Group II | Group III | Group IV |
|---|---|---|---|---|
| 1–2 | 1 | 0 | 0 | 0 |
| 3–4 | 4 | 0 | 2 | 0 |
| 5–6 | 1 | 3 | 1 | 0 |
| 7–8 | 2 | 6 | 6 | 4 |
| 9–10 | 2 | 1 | 1 | 3 |
| >10 | 0 | 0 | 0 | 3 |
Masseter muscle thickness
On comparing the mean cross-sectional thickness of the masseter muscle in the relaxed and contracted states on the right and left sides (Table 4) in all the four study groups and the control group, there was a highly significant difference in the cross-sectional thickness of the masseter muscle in the relaxed vs the contracted states in Groups I, II (left side), III, IV and the control group on the right and left sides (p < 0.0001), whereas a significant difference was observed in Group II (right side, p < 0.05).
Table 4.
Comparison of the mean ± standard deviation (SD) of the cross-sectional thickness of the masseter, anterior temporalis and orbicularis oris muscles in the relaxed and contracted state (right and left side) in all four study groups and the control group (Student's unpaired t-test)
| Groups | Side | Masseter |
Anterior temporalis |
Orbicularis oris |
||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | p-value | Mean ± SD | p-value | Mean ± SD | p-value | |||
| Group Ia | Right | Relaxed | 10.19 ± 1.23 | 0.000, HS, p < 0.0001 | 5.63 ± 1.34 | 0.08, NS, p > 0.05 | 3.73 ± 0.75 | 0.003, S, p < 0.0500 |
| Contracted | 14.85 ± 2.84 | 6.89 ± 1.73 | 5.31 ± 1.25 | |||||
| Left | Relaxed | 10.50 ± 1.82 | 0.000, HS, p < 0.0001 | 6.15 ± 1.87 | 0.17, NS, p > 0.05 | 4.14 ± 0.54 | 0.000, HS, p < 0.0001 | |
| Contracted | 14.05 ± 2.69 | 7.52 ± 2.39 | 5.45 ± 0.67 | |||||
| Group IIa | Right | Relaxed | 10.48 ± 1.79 | 0.014, S, p < 0.0500 | 5.19 ± 1.35 | 0.09, NS, p > 0.05 | 5.19 ± 1.35 | 0.20, NS, p > 0.0500 |
| Contracted | 13.27 ± 2.14 | 6.73 ± 2.41 | 6.73 ± 2.41 | |||||
| Left | Relaxed | 9.23 ± 0.74 | 0.000, HS, p < 0.0001 | 5.34 ± 1.28 | 0.11, NS, p > 0.05 | 5.34 ± 1.28 | 0.05, NS, p > 0.0500 | |
| Contracted | 12.81 ± 1.54 | 6.26 ± 1.16 | 6.26 ± 1.16 | |||||
| Group IIIa | Right | Relaxed | 10.18 ± 1.48 | 0.000, HS, p < 0.0001 | 6.05 ± 1.16 | 0.05, NS, p > 0.05 | 6.05 ± 1.16 | 0.01, S, p < 0.0500 |
| Contracted | 14.18 ± 1.61 | 7.30 ± 1.52 | 7.30 ± 1.52 | |||||
| Left | Relaxed | 10.62 ± 0.86 | 0.000, HS, p < 0.0001 | 5.38 ± 1.10 | 0.05, NS, p > 0.05 | 5.38 ± 1.10 | 0.000, HS, p < 0.0001 | |
| Contracted | 13.87 ± 1.69 | 6.67 ± 1.62 | 6.67 ± 1.62 | |||||
| Group IVa | Right | Relaxed | 9.11 ± 1.14 | 0.000, HS, p < 0.0001 | 5.51 ± 1.04 | 0.01, S, p < 0.05 | 5.51 ± 1.04 | 0.01, S, p < 0.0500 |
| Contracted | 11.59 ± 1.96 | 6.69 ± 0.82 | 6.69 ± 0.82 | |||||
| Left | Relaxed | 9.14 ± 1.35 | 0.000, HS, p < 0.0001 | 5.38 ± 0.55 | 0.001, S, p < 0.05 | 5.38 ± 0.55 | 0.001, S, p < 0.0500 | |
| Contracted | 11.39 ± 1.86 | 6.34 ± 0.74 | 6.34 ± 0.74 | |||||
| Controlb | Right | Relaxed | 10.54 ± 2.11 | 0.000, HS, p < 0.0001 | 5.11 ± 0.85 | 0.06, NS, p > 0.05 | 5.11 ± 0.85 | 0.000, HS, p < 0.0001 |
| Contracted | 14.23 ± 2.67 | 5.78 ± 1.32 | 5.78 ± 1.32 | |||||
| Left | Relaxed | 10.33 ± 1.67 | 0.000, HS, p < 0.0001 | 6.89 ± 1.18 | 0.99, NS, p > 0.05 | 6.89 ± 1.18 | 0.001, S, p < 0.0500 | |
| Contracted | 14.65 ± 1.71 | 6.89 ± 1.20 | 6.60 ± 1.74 | |||||
HS, highly significant; NS, not significant; S, significant.
n = 10.
n = 20.
Comparisons were made between groups and within groups to find out variations in the cross-sectional thickness of the masseter muscle in the relaxed and contracted states on both right and left sides. In these comparisons, the p-value was calculated. From these values, it was concluded that there was a significant variation in the cross-sectional thickness of the masseter muscle in the relaxed state on the left side and in the contracted state on both the right and left sides in all study groups and the control group (p < 0.05, ANOVA), whereas others were insignificant (Table 5a).
Table 5.
(a) Comparison of the cross-sectional thickness of masseter, anterior temporalis and orbicularis oris muscles in the relaxed and contracted states (right and left side) of Groups I, II, III and IV with the control group (one-way ANOVA)
| |
Masseter |
Anterior temporalis |
Orbicularisoris |
||||
|---|---|---|---|---|---|---|---|
| Source of variation | Relaxed (p-value) | Contracted (p-value) | Relaxed (p-value) | Contracted (p-value) | Relaxed (p-value) | Contracted (p-value) | |
| Right side | Between groups | 0.02, S, p < 0.05 | 0.28, NS, p > 0.05 | 0.25, NS, p > 0.05 | 0.91, NS, p > 0.05 | 0.01, S, p < 0.05 | 0.37, NS, p > 0.05 |
| Within groups | |||||||
| Total | |||||||
| Left side | Between groups | 0.001, S, p < 0.05 | 0.04, S, p < 0.05 | 0.54, NS, p > 0.05 | 0.32, NS, p > 0.05 | 0.01, S, p < 0.05 | 0.06, NS, p > 0.05 |
| Within groups | |||||||
| Total | |||||||
NS, not significant; S, significant.
A comparison was made between the thickness of the masseter muscle in the relaxed and contracted states of Groups I, II, III and IV on the right and left sides and that of the control group of the present study. The mean difference and p-value were calculated. From these values, it was concluded that the mean difference between the cross-sectional thickness of the masseter muscle in the contracted state on the right and left sides in Group IV (mouth opening <20 mm) and that of the control group of the present study was significant (p < 0.05, Dunnett test) (Table 5b).
Table 5.
(b) Comparison of the cross-sectional thickness of masseter, anterior temporalis and orbicularis oris muscles in the relaxed and contracted states (right and left side) of Groups I, II, III and IV with the control group (multiple comparisons: Dunnett test)
| Side | Study group | Control group | Masseter |
Anterior temporalis |
Orbicularis oris |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Relaxed |
Contracted |
Relaxed |
Contracted |
Relaxed |
Contracted |
|||||||||
| Mean difference | p-value | Mean difference | p-value | Mean difference | p-value | Mean difference | p-value | Mean difference | p-value | Mean difference | p-value | |||
| Right side | I | Control | −0.34 | 0.967, NS, p > 0.05 | 0.62 | 0.92, NS, p > 0.05 | 0.51 | 0.61, NS, p > 0.05 | 0.004 | 1.000, NS, p > 0.05 | −0.74 | 0.28, NS, p > 0.05 | −0.75 | 0.478, NS, p > 0.05 |
| II | −0.05 | 1.000, NS, p > 0.05 | −0.95 | 0.72, NS, p > 0.05 | 0.07 | 1.00, NS, p > 0.05 | −0.151 | 0.99, NS, p > 0.05 | −0.36 | 0.84, NS, p > 0.05 | −0.95 | 0.26, NS, p > 0.05 | ||
| III | −0.35 | 0.963, NS, p > 0.05 | −0.05 | 1.00, NS, p > 0.05 | 0.93 | 0.12, NS, p > 0.05 | 0.415 | 0.918, NS, p > 0.05 | −0.14 | 0.994, NS, p > 0.05 | −0.26 | 0.975, NS, p > 0.05 | ||
| IV | −1.42 | 0.121, NS, p > 0.05 | −2.63 | 0.02, S, p < 0.05 | 0.39 | 0.81, NS, p > 0.05 | −0.195 | 0.995, NS, p > 0.05 | 1.02 | 0.074, NS, p > 0.05 | −0.68 | 0.576, NS, p > 0.05 | ||
| Left side | I | Control | 0.17 | 0.995, NS, p > 0.05 | −0.59 | 0.86, NS, p > 0.05 | 0.37 | 0.89, NS, p > 0.05 | 0.633 | 0.682, NS, p > 0.05 | −0.56 | 0.479, NS, p > 0.05 | −1.15 | 0.114, NS, p > 0.05 |
| II | −1.10 | 0.173, NS, p > 0.05 | −1.84 | 0.05, NS, p > 0.05 | −0.43 | 0.83, NS, p > 0.05 | −0.624 | 0.693, NS, p > 0.05 | −0.61 | 0.393, NS, p > 0.05 | −1.17 | 0.103, NS, p > 0.05 | ||
| III | 0.29 | 0.967, NS, p > 0.05 | −0.77 | 0.72, NS, p > 0.05 | −0.39 | 0.87, NS, p > 0.05 | −0.214 | 0.991, NS, p > 0.05 | −0.82 | 0.155, NS, p > 0.05 | −1.13 | 0.124, NS, p > 0.05 | ||
| IV | −1.19 | 0.123, NS, p > 0.05 | −3.25 | 0.00, S, p < 0.05 | −0.39 | 0.87, NS, p > 0.05 | −0.547 | 0.78, NS, p > 0.05 | 0.67 | 0.31, NS, p > 0.05 | −1.07 | 0.15, NS, p > 0.05 | ||
NS, not significant; S, significant.
Anterior temporalis muscle thickness
On comparing the mean cross-sectional thickness of the anterior temporalis muscle in the relaxed and the contracted states on the right and left sides (Table 4) in all the four study groups and the control group, there was a significant difference in Group IV on both the right and left sides (p < 0.05), whereas others were non-significant.
A comparison was made between groups and within groups to find out variations in the cross-sectional thickness of the anterior temporalis muscle in the relaxed and the contracted states on both the right and left sides. In these comparisons, the p-value was calculated. From these values, it was concluded that there was no significant variation in the cross-sectional thickness of the anterior temporalis muscle in the relaxed and the contracted states on both the right and left sides in all the study groups and the control group (p > 0.05, ANOVA) (Table 5a).
A comparison was made between the thickness of the anterior temporalis muscle in the relaxed and the contracted states of Groups I, II, III and IV on the right and left sides and that of the control group of the present study. The mean difference and the p-value were calculated. From these values, it was concluded that the cross-sectional thickness of the anterior temporalis muscle in the relaxed and the contracted states on both the right and left sides in all the four study groups when compared with that of the control group of the present study was non-significant (p > 0.05, Dunnett test) (Table 5b).
Orbicularis oris muscle thickness
On comparing the mean cross-sectional thickness of the orbicularis oris muscle in the relaxed and contracted states on the right and left sides in all the four studies and the control group, there was a highly significant difference in the cross-sectional thickness of the orbicularis oris muscle in the relaxed vs the contracted state in Group I (left side), Group III (left side) and the control group (right side) (p < 0.0001), and a significant difference was observed in Group I (right side), Group III (right side), Group IV (right and left side) and the control group (left side) (p < 0.05).
Comparisons were made between groups and within groups to find out variations in the cross-sectional thickness of the orbicularis oris muscle in the relaxed and contracted states on both the right and left sides. In these comparisons, the p-value was calculated. From these values, it was concluded that there was a significant variation in the cross-sectional thickness of the orbicularis oris muscle in the relaxed state on both the right and left sides in all the study groups and that of the control group (p < 0.05, ANOVA) (Table 5a). No significant variation was observed in the cross-sectional thickness of the orbicularis oris muscle in the contracted state on both the right and left sides in all the study groups and that of the control group (p > 0.05, ANOVA) (Table 5a).
A comparison was made between the thickness of the orbicularis oris muscle in the relaxed and contracted states of Groups I, II, III and IV on the right and left sides and that of the control group of the present study. The mean difference and the p-value were calculated. From these values, it was concluded that the cross-sectional thickness of the orbicularis oris muscle in the relaxed and contracted states on both the right and left sides in all the four study groups when compared with that of the control group of the present study was non-significant (p > 0.05, Dunnett test) (Table 5b).
Masseter muscle activity
On comparing the amplitude of the masseter muscle in the contracted state on the right and left sides in all the four study groups and the control group, there was a significant difference in the amplitude of the masseter muscle in the contracted state between the right and left sides in Group IV (p < 0.05), whereas the others were non-significant (Table 6a).
Table 6.
(a) A comparison of the electromyographic amplitude (μV) of the masseter, anterior temporalis and orbicularis oris muscles in the contracted state (right and left side) in all four study groups and the control group (Student's paired t-test)
| Group | Side | Masseter |
Anterior temporalis |
Orbicularis oris |
||||
|---|---|---|---|---|---|---|---|---|
| Mean | p-value | Mean | p-value | Mean | p-value | |||
| Amplitude | I | Right | 391.56 | 0.27, NS, p > 0.05 | 407.50 | 0.32, NS, p > 0.05 | 383.89 | 0.92, NS, p > 0.05 |
| Left | 364.26 | 377.43 | 379.40 | |||||
| II | Right | 437.73 | 0.39, NS, p > 0.05 | 389.13 | 0.33, NS, p > 0.05 | 362.83 | 0.99, NS, p > 0.05 | |
| Left | 414.29 | 364.03 | 362.46 | |||||
| III | Right | 382.63 | 0.19, NS, p > 0.05 | 367.53 | 0.55, NS, p > 0.05 | 328.03 | 0.76, NS, p > 0.05 | |
| Left | 411.80 | 389.46 | 333.73 | |||||
| IV | Right | 407.66 | 0.01, S, p < 0.05 | 407.53 | 1.00, NS, p > 0.05 | 407.53 | 1.00, NS, p > 0.05 | |
| Left | 358.69 | 407.53 | 407.53 | |||||
| Control | Right | 401.16 | 0.30, NS, p > 0.05 | 414.76 | 0.75, NS, p > 0.05 | 386.91 | 0.84, NS, p > 0.05 | |
| Left | 428.86 | 423.51 | 383.88 | |||||
NS, not significant; S, significant.
On comparing the duration of the masseter muscle in the contracted state on the right and left sides in all the four study groups and the control group, no significant difference was observed in all the groups (p > 0.05) (Table 6b).
Table 6.
(b) A comparison of the electromyographic duration (ms) of the masseter, anterior temporalis and orbicularis oris muscles in the contracted state (right and left side) in all four study groups and the control group
| Group | Side | Masseter |
Anterior temporalis |
Orbicularis oris |
||||
|---|---|---|---|---|---|---|---|---|
| Mean | p-value | Mean | p-value | Mean | p-value | |||
| Duration | I | Right | 5.90 | 0.92, NS, p > 0.05 | 6.40 | 0.63, NS, p > 0.05 | 6.65 | 0.92, NS, p > 0.05 |
| Left | 5.84 | 6.82 | 6.75 | |||||
| II | Right | 8.69 | 0.19, NS, p > 0.05 | 8.42 | 0.39, NS, p > 0.05 | 7.36 | 0.99, NS, p > 0.05 | |
| Left | 7.38 | 7.42 | 7.35 | |||||
| III | Right | 8.16 | 0.07, NS, p > 0.05 | 6.12 | 0.39, NS, p > 0.05 | 6.86 | 0.48, NS, p > 0.05 | |
| Left | 6.48 | 6.97 | 7.57 | |||||
| IV | Right | 5.84 | 0.91, NS, p > 0.05 | 7.80 | 0.35, NS, p > 0.05 | 7.80 | 0.35, NS, p > 0.05 | |
| Left | 6.50 | 6.94 | 6.94 | |||||
| Control | Right | 7.35 | 0.68, NS, p > 0.05 | 7.64 | 0.72, NS, p > 0.05 | 8.35 | 0.56, NS, p > 0.05 | |
| Left | 7.64 | 7.44 | 8.70 | |||||
NS, not significant; S, significant.
Comparisons were made between groups and within groups to find out variations in the amplitude and duration of muscles in the contracted state on both the right and left sides. In these comparisons, the p-value was calculated. From these values, it was concluded that there was no significant variation in the amplitude of the masseter muscle in the contracted state on both the right and left sides in all the study groups and the control group (p > 0.05, ANOVA) (Table 7a). There was a significant variation in the duration of the masseter muscle in the contracted state on the right side (p < 0.05, ANOVA), whereas others were non-significant (Table 7b).
Table 7.
(a) A comparison of the electromyographic amplitude of the masseter, anterior temporalis and orbicularis oris muscles in the contracted state (right and left side) of Groups I, II, III and IV with the control group (one-way ANOVA)
| Group | Source of variation | Masseter (p-value) | Anterior temporalis (p-value) | Orbicularis oris (p-value) | |
|---|---|---|---|---|---|
| Amplitude | Right side | Between groups | 0.24, NS, p > 0.05 | 0.68, NS, p > 0.05 | 0.24, NS, p > 0.05 |
| Within groups | |||||
| Total | |||||
| Left side | Between groups | 0.08, NS, p > 0.05 | 0.09, NS, p > 0.05 | 0.06, NS, p > 0.05 | |
| Within groups | |||||
| Total | |||||
NS, not significant; S, significant.
Table 7.
(b) A comparison of the electromyographic duration of the masseter, anterior temporalis and orbicularis oris muscles in the contracted state (right and left side) of Groups I, II, III and IV with the control group (one-way ANOVA)
| Group | Source of variation | Masseter (p-value) | Anterior temporalis (p-value) | Orbicularis oris (p-value) | |
|---|---|---|---|---|---|
| Duration | Right side | Between groups | 0.008, S, p < 0.05 | 0.070, NS, p > 0.05 | 0.35, NS, p > 0.05 |
| Within groups | |||||
| Total | |||||
| Left side | Between groups | 0.205, NS, p > 0.05 | 0.906, NS, p > 0.05 | 0.21, NS, p > 0.05 | |
| Within groups | |||||
| Total | |||||
NS, not significant; S, significant.
On comparing the amplitude and duration of the masseter muscle in the contracted state of Groups I, II, III and IV with those of the control group of the present study, no significant difference was observed (p > 0.05) (Table 7c,d).
Table 7.
(c) Comparison of electromyographic amplitude of masseter, anterior temporalis and orbiculais oris muscle in the contracted state (right and left side) of group I, II, III and IV with the control group (multiple comparisons: Dunnett test (2-sided)
| Side | Study group | Control group | Masseter |
Anterior temporalis |
Orbicularis oris |
|||
|---|---|---|---|---|---|---|---|---|
| Mean difference | p-value | Mean difference | p-value | Mean difference | p-value | |||
| Right side | I | Control | −9.59 | 0.983, NS, p > 0.05 | −7.26 | 0.999, NS, p > 0.05 | −3.01 | 1.000, NS, p > 0.05 |
| II | 36.56 | 0.310, NS, p > 0.05 | −25.63 | 0.885, NS, p > 0.05 | −24.08 | 0.823, NS, p > 0.05 | ||
| III | −18.53 | 0.841, NS p > 0.05 | −47.23 | 0.472, NS, p > 0.05 | −58.88 | 0.122, NS, p > 0.05 | ||
| IV | 6.50 | 0.996, NS, p > 0.05 | −7.23 | 0.999, NS, p > 0.05 | −1.68 | 1.000, NS, p > 0.05 | ||
| Left side | I | Control | −64.60 | 0.114, NS, p > 0.05 | −46.08 | 0.176, NS, p > 0.05 | −4.48 | 0.999, NS, p > 0.05 |
| II | −14.56 | 0.974, NS, p > 0.05 | −59.48 | 0.048, NS, p > 0.05 | −21.41 | 0.838, NS, p > 0.05 | ||
| III | −17.06 | 0.954, NS, p > 0.05 | −34.05 | 0.435, NS, p > 0.05 | −50.15 | 0.168, NS, p > 0.05 | ||
| IV | −70.16 | 0.074, NS, p > 0.05 | −15.98 | 0.918, NS, p > 0.05 | 35.58 | 0.462, NS, p > 0.05 | ||
NS, not significant; S, significant.
Table 7.
(d) A comparison of the electromyographic duration of the masseter, anterior temporalis and orbiculais oris muscles in the contracted state (right and left side) of Groups I, II, III and IV with the control group [multiple comparisons: Dunnett test (two-sided)]
| Side | Study group | Control group | Masseter |
Anterior temporalis |
Orbicularis oris |
|||
|---|---|---|---|---|---|---|---|---|
| Mean difference | p-value | Mean difference | p-value | Mean difference | p-value | |||
| Right side | I | Control | −1.44 | 0.252, NS, p > 0.05 | −1.24 | 0.381, NS, p > 0.05 | −1.70 | 0.27, NS, p > 0.05 |
| II | 1.34 | 0.316, NS, p > 0.05 | 0.77 | 0.772, NS, p > 0.05 | −0.99 | 0.74, NS, p > 0.05 | ||
| III | 0.80 | 0.750, NS, p > 0.05 | −1.52 | 0.205, NS, p > 0.05 | −1.48 | 0.39, NS, p > 0.05 | ||
| IV | −1.50 | 0.219, NS, p > 0.05 | 0.15 | 0.999, NS, p > 0.05 | −0.30 | 0.99, NS, p > 0.05 | ||
| Left side | I | Control | −1.79 | 0.116, NS, p > 0.05 | −0.62 | 0.875, NS, p > 0.05 | −1.94 | 0.12, NS, p > 0.05 |
| II | −0.26 | 0.995, NS, p > 0.05 | −0.02 | 1.000, NS, p > 0.05 | −1.35 | 0.42, NS, p > 0.05 | ||
| III | −1.15 | 0.476, NS, p > 0.05 | −0.47 | 0.950, NS, p > 0.05 | −1.12 | 0.59, NS, p > 0.05 | ||
| IV | −1.14 | 0.485, NS, p > 0.05 | −0.50 | 0.938, NS, p > 0.05 | −0.22 | 0.99, NS, p > 0.05 | ||
NS, not significant; S, significant.
Anterior temporalis muscle activity
On comparing the amplitude and duration of the anterior temporalis muscle in the contracted state on the right and left sides in all the four study groups and those of the control group, no significant difference was observed (p > 0.05) (Table 6a,b). Comparisons were made between groups and within groups to find out variations in the amplitude and duration of the anterior temporalis muscle in the contracted state on both the right and left sides. In these comparisons, p-value was calculated. From these values, it was concluded that there was no significant variation in the amplitude and duration of the anterior temporalis muscle in the contracted state on both the right and left sides in all the study groups and the control group (p > 0.05, ANOVA) (Table 7a,b).
On comparing the amplitude and duration of the anterior temporalis muscle in the contracted state of Groups I, II, III, IV with the control group of the present study, no significant difference was observed (Dunnett test p > 0.05) (Table 7c,d).
Orbicularis oris muscle activity
On comparing the amplitude and duration of the orbicularis oris muscle in the contracted state on the right and left sides in all the four study groups and the control group, no significant difference was observed (Table 6a,b).
Comparisons were made between groups and within groups to find out variations in the amplitude and duration of the orbicularis oris muscle in the contracted state on both the right and left sides. In these comparisons, p-value was calculated. From these values, it was concluded that there was no significant variation in the amplitude and duration of the orbicularis oris muscle in the contracted state on both the right and left sides in all the study groups and the control group (Table 7a,b).
On comparing the amplitude and duration of the orbicularis oris muscle in the contracted state of Groups I, II, III and IV with the control group of the present study, no significant differences were observed (p > 0.05) (Table 7c,d).
Relation between muscle thickness and muscle activity
Table 8 shows the correlation between the ultrasonographic cross-sectional thickness of the masseter, anterior temporalis and orbicularis oris muscles in the contracted state and the electromyographic amplitude. A positive correlation was found between the ultrasonographic cross-sectional thickness of the masseter muscle and the electromyographic amplitude in Group I (r = 0.05, p = 0.89), Group II (r = 0.36, p = 0.29) and Group III (r = 0.49, p = 0.15), whereas there was a negative correlation in Group IV (r = −0.75, p = 0.01) and the control group (r = −0.03, p = 0.89).
Table 8.
Correlation of the ultrasonographic cross-sectional thickness of the masseter, anterior temporalis and orbicularis oris muscles in the contracted state with amplitude of electromyography in Groups I–IV and the control group
| Group | Masseter muscle |
Anterior temporalis muscle |
Orbicularis oris muscle |
|||
|---|---|---|---|---|---|---|
| Correlation (r) | p-value | Correlation (r) | p-value | Correlation (r) | p-value | |
| Group I | 0.05 | 0.89, NS, p > 0.05 | −0.13 | 0.72, NS, p > 0.05 | −0.36 | 0.30, NS, p > 0.05 |
| Group II | 0.36 | 0.29, NS, p > 0.05 | 0.32 | 0.35, NS, p > 0.05 | 0.08 | 0.81, NS, p > 0.05 |
| Group III | 0.49 | 0.15, NS, p > 0.05 | −0.07 | 0.84, NS, p > 0.05 | 0.30 | 0.38, NS, p > 0.05 |
| Group IV | −0.75 | 0.01, S, p < 0.05 | −0.32 | 0.35, NS, p > 0.05 | 0.003 | 0.99, NS, p > 0.05 |
| Control group | −0.03 | 0.89, NS, p > 0.05 | 0.19 | 0.41, NS, p > 0.05 | −0.05 | 0.82, NS, p > 0.05 |
NS, not significant; S, significant.
A positive correlation was observed between the ultrasonographic cross-sectional thickness of the anterior temporalis and the electromyographic amplitude in Group II (r = 0.32, p = 0.35) and the control group (r = 0.32, p = 0.35), and there was a negative correlation in Group I (r = −0.13, p = 0.72), Group III (r = −0.07, p = 0.84) and Group IV (r = −0.32, p = 0.35).
There was a positive correlation between the cross-sectional thickness of the orbicularis oris muscle and the electromyographic amplitude in Group II (r = 0.08, p = 0.81), Group III (r = 0.30, p = 0.38) and Group IV (r = 0.003, p = 0.99), whereas there was a negative correlation in Group I (r = −0.36, p = 0.30) and the control group (r = −0.05, p = 0.82).
Discussion
Based on histopathological and electron microscopic observations, several authors have reported muscle degeneration in patients with OSMF.2,3 Khanna and Andrade4 reported dense collagen fibres interspersed with muscle fibres in patients with OSMF with interincisal mouth opening of 15–25 mm, and they also observed extensive muscle degeneration of muscle fibres in advanced cases with interincisal distance <15 mm. So, the present study was carried out to determine the involvement of muscles of mastication and muscles of facial expression in OSMF by assessing the cross-sectional thickness and activity of the masseter, anterior temporalis and orbicularis oris muscles by non-invasive procedures, such as ultrasonography and electromyography, and comparing the findings with age- and sex-matched controls.
CT and MRI are the common techniques used to measure the cross-sectional areas and volumes of human jaw muscles. CT shows cumulative biological effects, and the cost and availability limit the use of MRI.14,15
In recent years, the use of ultrasound has spread throughout different fields of medicine, as it is an accurate, easy and convenient method. Up to now, there has been no conclusive evidence of adverse biological effects on the use of ultrasound energy at diagnostic levels.16 Ultrasonography has been proven to be a reliable diagnostic technique for the evaluation of cross-sectional dimensions and areas of muscles of the head and neck.11
Electromyography has a long history of application in the study of functional jaw muscle anatomy. Normal healthy jaw muscles are able to both contract with adequate force in a coordinated manner and relax during mandibular rest. However, the assessment of these basic functions through palpation and visual observation is not always sufficient when rendering a diagnosis of muscular dysfunction. When a more comprehensive understanding is necessary, electromyography is the only reliable method available for the objective recording of a patient's muscular function. Electromyographic activity of the masticatory muscles has been widely studied in clinical work and research, with both indwelling electrodes and surface recordings. With regard to surface electromyography, the instruments currently available allow the investigation of several muscles involved in chewing and swallowing, and in the posture of the head (typically masseter, anterior temporalis and posterior, digastric anterior and sternocleidomastoid).17
The cross-sectional thickness of the muscles was recorded using a 15-MHz linear-phased array transducer. The cross-sectional thickness of the muscles was recorded in millimetres in the relaxed and contracted states and bilaterally on both the right and left sides.
The electromyographic activity was recorded using the RMS Polyrite D system. The amplitude and duration of the masseter, anterior temporalis and orbicularis oris muscles were recorded in the relaxed and contracted states on both the right and left sides. The amplitude was recorded in microvolts, and the duration was recorded in milliseconds. All the muscles were electrically silent in the relaxed state.
In this study, the thickness and activity of the masseter, anterior temporalis and orbicularis oris muscles were recorded in 40 patients with OSMF and 20 controls. The patients were divided into four groups on the basis of interincisal mouth opening, i.e. Group I (mouth opening >35 mm), Group II (mouth opening between 30 and 35 mm), Group III (mouth opening between 20 and 30 mm) and Group IV (mouth opening <20 mm).
In this study, the male to female ratio was 39:1. The mean ± SD of the age of the patients ranged from 24.70 ± 2.21 to 27.80 ± 5.99 years. The mean mouth opening decreased from 38.90 ± 3.34 mm in Group I to 16.60 ± 3.77 mm in Group IV. The prevalent habit in all the four groups was kharra chewing.
Ultrasonographic cross-sectional thickness and electromyographic activity of 240 muscles were recorded in the study groups (6 muscles from each patient) and 120 muscles in the control group (6 muscles from each subject). 2880 recordings for ultrasonographic cross-sectional thickness (relaxed and contracted state) and 1440 recordings of electromyographic activity (contracted state) were performed in patients with OSMF, and 1440 ultrasonographic recordings and 720 electromyographic recordings were performed in the control group of the present study.
Similar studies recording the cross-sectional thickness and the electromyographic activity of the muscles of mastication (the masseter and the anterior temporalis) and of facial expression (the orbicularis oris) in OSMF have not been reported previously in the literature.
In this study, there was an increase in ultrasonographic cross-sectional thickness of the masseter muscle in all the study groups and the control group from the relaxed to the contracted states. The cross-sectional thickness of the masseter muscle in Group I, Group II and Group III was not significantly altered when compared with that of the control group of the present study. The cross-sectional thickness of the masseter muscle in Group IV was reduced significantly when compared with Groups I, II, III and the control group.
Univariate analysis of variance (in all groups) for repeated measurements showed significant variation in the cross-sectional thickness of the masseter muscle in the relaxed state on the right and left sides and in the contracted state on the left side (p < 0.05, ANOVA).
The ultrasonographic cross-sectional thickness of the masseter muscle in Groups I, II, III and IV was compared with the control group by applying the Dunnett test, and no significant difference was observed (p > 0.05). This might be due to variations in the large number of ultrasonographic recordings.
The mean cross-sectional thickness of the masseter muscle in the control group of the present study in the relaxed state (10.43 ± 1.89 mm) and the contracted state (14.44 ± 2.19 mm) is comparable to the findings of Bertram et al;18 they reported a mean cross-sectional thickness of the relaxed masseter muscle in the range of 6.8–12.9 mm and of 9.0–16.1 mm in the contracted masseter muscle.
A significant difference was observed between the amplitude of the masseter muscle in Group IV (contracted state) between the right and left sides (p < 0.05).
To find out variations in the electromyographic amplitude and duration in all the study groups and the control group, one-way ANOVA was applied, and no significant variation was observed in the electromyographic amplitude of the masseter muscle in all study population of patients with OSMF and the control group (p > 0.05), whereas a significant variation was observed in the electromyographic duration of the masseter muscle on the right side (p < 0.05).
The electromyographic activity and duration of the masseter muscle in Groups I, II, III and IV were compared with the control group and no significant difference was observed (p > 0.05, Dunnett test).
Pearson's correlation coefficient showed a positive correlation between the ultrasonographic cross-sectional thickness of the masseter muscle and the electromyographic amplitude in Groups I, II and III and a negative correlation in Group IV and the control group.
The decreased cross-sectional thickness of the masseter muscle in Group IV (interincisal mouth opening <20 mm) compared with Groups I, II, III and the control group can be explained by the fact that, because of areca nut chewing, the muscles remain in a contracted state, which leads to glycogen depletion, leading to muscle degeneration, fibrosis and scarring. This might be responsible for the reduced thickness of the masseter muscle in Group IV, which correlates with the chronicity of the disease. The masseter and temporalis are strong elevator muscles of the mandible. The masseter muscle covers more surface area of the mandible and remains in close proximity to the muscles of facial expression; these two factors are responsible for the early involvement of the masseter.
In this study, there was an increase in the ultrasonographic cross-sectional thickness of the anterior temporalis muscle in all the study groups and the control group from the relaxed to the contracted state.
One-way ANOVA showed no significant variation in the cross-sectional thickness of the anterior temporalis muscle in all the study groups and the control group (p > 0.05).
On applying the Dunnett test, there was no significant difference in the ultrasonographic cross-sectional thickness of the anterior temporalis muscle in Groups I, II, III and IV in comparison with the control group (p > 0.05).
In the present study, there was no significant difference in the electromyographic activity between the right and left sides in all the study groups and the control group (p > 0.05). No significant variation was observed in the amplitude and duration of the anterior temporalis muscle in the study population of patients with OSMF and the control group (p > 0.05, ANOVA). No significant difference was observed in the activity (amplitude and duration) of the anterior temporalis muscle in Groups I, II, III and IV when compared with the control group of the study (p > 0.05, Dunnett test).
In this study, a positive correlation was observed between the ultrasonographic cross-sectional thickness of the anterior temporalis muscle and the electromyographic amplitude in Group II and the control group, and there was a negative correlation in Groups I, III and IV.
Owing to the anatomical position of the temporalis muscle (as only a sling of temporalis is inserted onto the coronoid process), the cross-sectional thickness and activity of the anterior temporalis remained unaffected.
There was an increase in ultrasonographic cross-sectional thickness of the orbicularis oris muscle in all the study groups and the control group from the relaxed to the contracted states.
There was a significant variation in the cross-sectional thickness of the orbicularis oris muscle (relaxed state) in all the study groups and the control group (p < 0.05, ANOVA). No significant difference was observed in the cross-sectional thickness of the orbicularis oris muscle in Groups I, II, III and IV when compared with the control group (p > 0.05, Dunnett test).
No significant difference was observed in the electromyographic activity between the right and left sides in all the study population of OSMF and the control group.
ANOVA showed no significant variation in the amplitude and duration of the orbicularis oris muscle in all the study groups and the control group (p > 0.05). The activity of the orbicularis oris muscle in Groups I, II, III and IV remained unaltered in comparison with the control group (p > 0.05, Dunnett test).
A positive correlation was observed between the ultrasonographic cross-sectional thickness of the orbicularis oris muscle with the electromyographic amplitude in Groups II, III and IV, and there was a negative correlation in Group I and the control group.
The cross-sectional thickness and activity of the orbicularis oris remained unaffected, as the leaching out compounds from the areca nut product affect the labial mucosa last and the other muscles intermingled with the orbicularis oris might protect the labial musculature of the rima oris unless a linear fibrosis occurs.
The present study was able to establish the normal values of ultrasonographically and electromyographically measured thickness and activity of the masseter, anterior temporalis and orbicularis oris muscles for a small subset of the Indian population.
For the first time, an attempt has been made to find out the involvement of the muscles of mastication (the masseter and the anterior temporalis) and the muscles of facial expression (the orbicularis oris) in patients with OSMF by non-invasive procedures such as ultrasonography and electromyography.
The drawback of our study is that the deeper muscles of mastication and other muscles of facial expression were not studied because of the limitation of ultrasonography in recording the cross-sectional thickness of deeper muscles. In our study, surface electrodes were used, and the accuracy of these in recording the action potential of the muscle to be studied may be altered in cases of mixing of action potentials of the neighbouring muscle fibres, whereas needle electrodes, which are inserted directly into the belly of the muscle in question, are more accurate in recording the action potential of the desired muscle.
Summary and conclusion
This study was performed to measure the cross-sectional thickness and activity of the masseter, anterior temporalis and orbicularis oris muscles in patients with OSMF and in healthy controls and to compare the cross-sectional thickness and activity of the masseter, anterior temporalis and orbicularis oris muscles in patients with OSMF with those of healthy controls and to find out any correlation between the ultrasonographic cross-sectional thicknesses of the masseter, anterior temporalis and orbicularis oris muscles and the electromyographic activity. The observations of the study were subjected to statistical analysis, results were tabulated and the following conclusions were drawn:
The cross-sectional thickness of the masseter muscle decreased in Group IV (interincisal mouth opening <20 mm), the muscle activity remained unaltered as compared with Groups I, II, III and IV, and a positive correlation was observed between the ultrasonographic cross-sectional thicknesses of the masseter muscle and the electromyographic amplitude in Groups I, II and III.
The cross-sectional thickness and activity of the anterior temporalis remained unaffected in all the study population of OSMF compared with the control group, and a positive correlation was observed between the ultrasonographic cross-sectional thickness of the anterior temporalis muscle and the amplitude of electromyography in Group II and the control group.
The cross-sectional thickness and activity of the orbicularis oris muscle remained unaffected in all the study groups compared with the control group, and a positive correlation was observed between the ultrasonographic cross-sectional thickness of the orbicularis oris muscle and the electromyographic amplitude in Groups II, III and IV.
So it would be fair to conclude from the present study that, amongst the muscles evaluated, the masseter muscle is more likely to be involved early in patients with OSMF. The use of real-time ultrasonography with high-frequency transducers and electromyography can serve as a useful aid in detecting the early involvement of the muscles of mastication and muscles of facial expression in patients with OSMF.
To validate these findings, future comparative studies with a larger sample size using ultrasonography, electromyography (using needle and surface electrodes) and muscle biopsy are required.
References
- 1.Pindborg JJ, Sirsat SM. Oral submucous fibrosis. Oral Surg Oral Med Oral Pathol 1966; 22: 764–79. [DOI] [PubMed] [Google Scholar]
- 2.Binnie WH, Cawson RA. A new ultrastructural finding in oral submucous fibrosis. Br J Dermatol 1972; 86: 286–9. [DOI] [PubMed] [Google Scholar]
- 3.El-Labban NG, Caniff JP. Ultrastructural findings of muscle degeneration in oral submucous fibrosis. J Oral Pathol 1985; 14: 709–17. [DOI] [PubMed] [Google Scholar]
- 4.Khanna JN, Andrade NN. Oral submucous fibrosis: a concept in surgical management. Int J Oral Maxillofac Surg 1995; 24: 433–9. [DOI] [PubMed] [Google Scholar]
- 5.Caniff JP, Harvey W. The aetiology of oral submucous fibrosis. The stimulation of collagen synthesis by extract of areca nut. Int J Oral Surg 1981; 10(Suppl. 1): 163–7. [PubMed] [Google Scholar]
- 6.Harvey W, Scutt A, Meghji S, Canniff JP. Stimulation of human buccal mucosa fibroblasts in vitro by betel-nut alkaloids. Arch Oral Biol 1986; 1: 45–9. [DOI] [PubMed] [Google Scholar]
- 7.Murti PR, Gupta PC, Bhonsle RB, Daftary DK, Mehta FS, Pindborg JJ. Effect on the incidence of oral submucous fibrosis of intervention in the areca nut chewing habit. J Oral Pathol Med 1990; 19: 99–100. [DOI] [PubMed] [Google Scholar]
- 8.Jayanthi V, Mayberry JF. Oral submucosal fibrosis: a preventable disease. Gut 1992; 33: 4–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuttan R, Donnelly PV, Di Ferrante N. Collagen treated with (+)- catechin becomes resistant to the action of mammalian collagenase. Experientia 1981; 37: 211–23. [DOI] [PubMed] [Google Scholar]
- 10.Gollnick PA, Karlsson J, Piehl K, Saltin B. Selective glycogen depletion in skeletal muscle fibres of man following sustained contractions. J Physiol 1974; 241: 59–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emshoff R, Bertram S, Brandlmaier I. Ultrasonographic assessment of local cross-sectional dimensions of masseter muscle sites: a reproducible technique. J Oral Rehabil 2002; 29: 1059–62. [DOI] [PubMed] [Google Scholar]
- 12.Misra UK, Kalita J. Clinical neurophysiology. Nerve conduction, electromyography, evoked potentials. New Delhi, India: B.I. Churchill Livingstone; 2001. pp. 114–26. [Google Scholar]
- 13.Lai DR, Chen HR, Lin LM, Huang YL, Tsai CC. Clinical evaluation of different treatment methods for oral submucous fibrosis. A 10-year experience with 150 cases. J Oral Pathol Med 1995; 24: 402–40. [DOI] [PubMed] [Google Scholar]
- 14.Hannam AG, Wood WW. Relationships between the size and spatial morphology of human masseter and medial pterygoid muscles, the craniofacial skeleton, and jaw mechanics. Am J Phys Anthropol 1989; 80: 429–45. doi: 10.1002/ajpa.1330800404 [DOI] [PubMed] [Google Scholar]
- 15.Newton JP, Abel RW, Robertson EM, Yemm R. Changes in human masseter and medial pterygoid muscles with age: a study by computed tomography. Gerodontics 1987; 3: 151–4. [PubMed] [Google Scholar]
- 16.Bakke M, Tuxen A, Vilmann P, Jensen BR, Vilmann A, Toft M. Ultrasound image of human masseter muscle related to bite force,elcteromyography, facial morphology, and occlusal factors. Scand J Dent Res 1992; 100: 164–71. [DOI] [PubMed] [Google Scholar]
- 17.Widmalm SE, Lee YS, McKay DC. Clinical use of electromyography in the evaluation of jaw muscle function: a practitioner’s guide. Cranio 2007; 25: 63–73. [DOI] [PubMed] [Google Scholar]
- 18.Bertram S, Brandlmaier I, Rudisch A, Bodner G, Emshoff R. Cross-sectional characteristics of the masseter muscle: an ultrasonographic study. Int J Oral Maxillofac Surg 2003; 32: 64–8. doi: 10.1054/ijom.2002.0259 [DOI] [PubMed] [Google Scholar]