Abstract
Following a smoking cessation attempt, smokers with posttraumatic stress disorder (PTSD) experience smoking relapse at a higher and faster rate. Black ethnicity and female gender are also associated with lower success rates following smoking cessation. No study to date has prospectively examined how ethnicity and gender may moderate the effect of PTSD on smoking relapse. It was hypothesized that female gender and Black ethnicity would significantly predict early lapse after quitting; further, it was predicted that ethnicity and gender would moderate the effect of PTSD on relapse rate. Smokers with PTSD (n = 48) and without PTSD (n = 56) completed ecological momentary assessment (EMA) the week after a quit date, and self-initiated EMA entries after smoking lapse. Smoking abstinence was biologically verified. The sample included Black (62%) and White (38%) participants, and was 50% female. Study hypotheses were tested with Cox proportional hazards regression modeling time to first smoking lapse. Study results confirmed the main hypothesis, with a significant PTSD X Ethnicity interaction emerging. The effect of PTSD on smoking relapse was significant for White participants but not for Black participants. No significant gender moderation was found. Taken together, study results support previous research, and suggest that the relationship between smoking and PTSD is stronger for White smokers than for minorities. This study has significant implications for research in smoking and mental disease, as well as for smoking cessation treatments for Black smokers.
Keywords: Tobacco control, smoking cessation, ethnic minorities, African Americans, posttraumatic stress disorder = PTSD, health disparities
1. Introduction
Posttraumatic stress disorder (PTSD) presents a significant barrier to smoking cessation in the general population (Hapke et al., 2005). Around 45% of individuals with PTSD are current smokers, and PTSD is associated with an increased likelihood of being a smoker (Feldner, Babson & Zvolensky, 2007). Evidence suggests smoking increases the risk of developing PTSD (Breslau, Novak & Kessler, 2004; Koenen et al., 2005). Moreover, PTSD smokers are less able to quit smoking and have a shorter time to first smoking lapse within the first week of a quit attempt (Zvolensky et al., 2008). It is theorized that core features of PTSD, including trauma symptoms and increased negative affect, represent key risk factors for smoking lapse and relapse (Beckham, Calhoun, Dennis, Wilson, & Dedert, 2013; Beckham et al., 2007; Cook, McFall, Calhoun, & Beckham, 2007). Additionally, individuals with PTSD experience more intense withdrawal symptoms during smoking cessation, which could also increase risk for smoking relapse (Dedert et al., 2012). Since smoking is related to PTSD symptoms and PTSD symptoms can in turn increase the risk for smoking relapse, it is essential to further investigate early lapse in PTSD smokers.
Rates of smoking relapse within the general population are also affected by gender and ethnicity (Japuntich et al., 2011). In a large-scale clinical trial testing the efficacy and effectiveness of different types of smoking cessation treatment, both females (compared to males) and Black smokers (compared to White smokers) were more likely to relapse following a quit attempt, largely regardless of treatment used (Piper et al., 2010). It is theorized that ethnic and gender differences in nicotine metabolism (Hukkanen, Jacob, & Benowitz, 2005) – possibly related in part to genetic polymorphism of CYP2A6 gene (Derby et al., 2008) – significantly contribute to increased susceptibility of smoking relapse. Specifically, females may be more highly addicted to nicotine due to their faster nicotine metabolism, which likely increases their level of dependence (Benowitz, Lessov-Schlaggar, Swan, & Jacob, 2006). In contrast, smokers of African and Asian descent generally metabolize nicotine more slowly than smokers of European descent (Nakajima et al., 2006); yet Black smokers take in significantly more nicotine per cigarette and are more highly addicted compared to White smokers (Benowitz, 2008; Perez-Stable, Herrera, Jacob, & Benowitz, 1998). These data, taken together, suggest that women and Black smokers have increased risk for smoking lapse following a quit attempt.
1.1. Ethnicity X psychiatric illness interaction predicts smoking cessation
In addition to main effects of ethnicity and PTSD on smoking cessation, ethnicity may moderate the effect of PTSD on smoking cessation. Differences in smoking rates between ethnicities are likely influenced by several societal and cultural factors, as well as individual differences. A nationally representative study found that for minorities (defined as Black and Hispanic respondents) there was no significant relationship between past-30-day psychological distress and current smoking status or cigarettes smoked per day. However, there was a significant association of psychological distress with smoking status in White respondents (Kiviniemi, Orom, & Giovino, 2011). While an association between general distress and smoking status has clinical relevance, it is important to determine whether the same relationship may or may not be present when considering an interaction between ethnicity and specific psychiatric diagnoses. Another nationally representative study of Black Americans found that the presence of a lifetime or current psychiatric disorder was significantly associated with current smoking status. In addition, past year and past month psychiatric disorder were significantly associated with lower odds of being at least one year abstinent (Hickman, Delucchi, & Prochaska, 2010). Existing knowledge regarding the interaction between ethnicity and psychiatric disorders is limited because previous research has relied on retrospective report and has not examined specific psychiatric disorders, such as PTSD. There is a need for research that utilizes prospective methodology to monitor post-quit lapse events as they occur.
1.2. Significance
The effects of major sociodemographic factors such as ethnicity and gender on smoking cessation in PTSD is particularly important because women and Black Americans are more likely to have PTSD, and are more likely to have difficulty quitting smoking (Benowitz, 2008; Brewin, Andrews, & Valentine, 2000). As these groups are overrepresented among PTSD smokers, it is important to investigate how ethnicity and gender influence cessation behaviors in smokers with PTSD. The aim of the current study is to provide the first prospective investigation of the moderating effect of ethnicity on PTSD with regards to smoking lapse following a quit attempt. The study hypotheses were: 1) ethnicity will significantly predict lapse after quitting, with Black smokers exhibiting a faster lapse rate compared to Whites; 2) female gender will be associated with faster lapse rate; 3) ethnicity will moderate the effect of PTSD on lapse rate, such that Black smokers will exhibit a smaller effect of PTSD on lapse rate; and 4) gender will also moderate the effect of PTSD on lapse rate, such that women will have a larger effect of PTSD on lapse rate.
2. Material and methods
2.1. Participants
Data for the current study were taken from a larger study investigating early smoking lapse in smokers with and without PTSD (Beckham et al., 2013). Participants were Black and White smokers with PTSD (n = 48) and a comparison group with no current Axis I psychiatric disorders (n = 56). Eligibility criteria included smoking at least 10 cigarettes daily for the past year, willingness to make a smoking cessation attempt, and age 18-65. One hundred ninety-nine individuals were recruited and screened for study inclusion. During screening, participants meeting criteria for current alcohol or other substance abuse or dependence, psychotic disorder, or bipolar disorder with active manic symptoms were excluded from both groups (n = 41). Additionally, potential participants were excluded from either group if they used non-cigarette forms of nicotine, had major unstable medical problems or major respiratory disorders, or used bupropion or benzodiazepines (n = 13) Participants were eliminated from the comparison group if they met criteria for lifetime PTSD, major depressive disorder, panic disorder, specific phobia, generalized anxiety disorder, obsessive compulsive disorder, bipolar disorder, dysthymia, or an eating disorder (n = 36). Participant data for ethnicities other than Black or White (n = 5) were excluded from analysis.
2.2. Procedures
A more detailed description of study procedures is available in a previously published study (Beckham et al., 2013). Participants were recruited via flyers posted in medical centers and in the community, and via word of mouth. Participants completed a screening session, two smoking cessation counseling sessions based on the NCI Freshstart program (Rosenbaum & O’Shea, 1992), and one week of electronic diary (ED) monitoring following a quit date set by the participant. On the quit date and every two days following the quit date, participants returned to the laboratory for bioverification of smoking abstinence by providing expired carbon monoxide (CO) and saliva to be tested for cotinine level. Electronic diary monitoring and bioverification continued for seven days post-quit. Participants were paid $750 for their complete participation.
2.3. Measures
At screening, each participant provided sociodemographic information, smoking history, and completed measures of nicotine dependence (Fagerström Test of Nicotine Dependence [Heatherton, Kozlowski, Frecker, & Fagerström, 1991]), smoking cessation self-efficacy (Relapse Situation Efficacy Questionnaire [Gwaltney, 2001], and PTSD symptom severity (Davidson Trauma Scale [Davidson et al., 1997]). Socioeconomic status (SES) was calculated with the Hollingshead two-factor index of social position (Hollingshead & Redlich, 1958). Psychiatric disorders were assessed using the Structured Clinical Interview for DSM–IV Axis I disorders (SCID-I; First, Spitzer, Gibbon, & Williams, 1994) and the Clinician Administered PTSD Scale (CAPS; Blake et al., 1995), with excellent inter-rater reliability (κ = .95).
Each participant self-reported their ethnicity. Participants were asked to choose one ethnic group with the following response options: American Indian/Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, Black or African American, White, or More Than One Race. Participants also indicated whether they identified as Hispanic or Latino/a. Participants were categorized as Black if they indicated “Black or African American.” Participants were categorized as White if they only indicated “White” and did not indicate any other ethnic group.
2.3.2. Ecological Momentary Assessment Procedures
EMA data were collected with an ED system on a PalmOne Treo 600 handheld computer (PalmOne, Inc.). Procedures for EMA data collection have been previously described (Beckham et al., 2013). EMA data were utilized to compute time to first smoking lapse, defined as the first self-reported cigarette the participant entered into the daily diary.
2.3.3. Biological Measures
Smoking abstinence was verified by biological measures: expired carbon monoxide and salivary cotinine. Procedures for biological measurement can be found in Beckham, et al. (2013).
2.4. Statistical Analysis
All statistical analyses were performed using SAS 9.2, and plots were generated using SPSS 17.0. The outcome variables included in Cox proportional hazard regression were the dichotomous lapse variable (smoked or did not smoke during the quit week) and time to first smoking lapse after the quit date. The main outcome will henceforth be referred to as the lapse rate (the rate at which participant groups lapsed). Prior to analysis, the proportional hazards assumption was using the PROC LIFETEST command to inspect natural logarithm plots stratified by categorical variables. Additionally, the SAS TEST statement was used to examine linear hypotheses about the regression coefficients in the multivariate models. Since there were ties in the dataset (i.e., a few participants coincidently had the same minutes to first lapse), the Breslow approximation of partial log-likelihood was used (Breslow, 1974). Unadjusted hazard ratios were calculated for all variables of interest. Variables were retained for adjusted hazard ratio analysis if they were either significant at a .10 alpha level or important for theoretical reasons (i.e., empirical and theoretical evidence suggests a relationship with smoking lapse). Interaction terms were added to the model at the last step. The likelihood ratio was calculated to measure the improvement in model fit over the null model (for interaction model, it is the improvement over the model without interaction terms). The ratio was tested following a chi-square distribution with degrees of freedom equaling the number of added parameters.
3. Results
Descriptive characteristics are presented in Table 1. At baseline, individuals with PTSD had a higher level of nicotine dependence as measured by the Fagerström, and a higher incidence of lifetime major depressive disorder, current anxiety disorder other than PTSD, and lifetime alcohol dependence. Overall, rates of lifetime alcohol and drug dependence in the sample were high (see Table 1). Of the 104 participants who initiated a quit attempt, 91 participants (88%) had at least one smoking lapse during the 7-day follow-up period. There were baseline differences by race in both positive and negative affect. We conducted unadjusted analyses of the influences of both affect variables and found that neither was related to lapse rate.
Table 1. Group Characteristics by Key Variables.
| PTSD n = 48 |
Control n = 56 |
Black n = 64 |
White n = 40 |
Female n = 52 |
Male n = 52 |
|
|---|---|---|---|---|---|---|
| Lapsed | 94% | 82% | 91% | 83% | 88% | 87% |
| Black | 54% | 68% | --- | --- | 62% | 62% |
| Veteran | 21% | 25% | 25% | 20% | 4% * | 42% |
| Female | 58% | 43% | 50% | 50% | --- | --- |
| Age | 42.8 (10.5) | 41.8 (9.8) | 44.3 (8.7) * | 39.2 (11.4) | 40.4 (9.9) * | 44.2 (9.7) |
| PTSD Severity | 10.7 (12.3) * | 1.2 (2.9) | 4.8 (7.6) | 7.0 (12.6) | 7.4 (12.7) | 3.8 (5.2) |
| Cigs/day | 18.0 (8.6) | 15.7 (6.8) | 15.9 (8.1) | 18.1 (6.9) | 15.9 (8.3) | 17.6 (7.0) |
| Menthol | 50% | 66% | 75% * | 33% | 62% | 56% |
| Fagerström | 6.2 (1.8) * | 5.2 (2.1) | 5.6 (2.0) | 5.8 (2.1) | 6.3 (1.9) * | 5.1 (2.0) |
| Self-efficacy | 167.8 (45.5) | 173.7 (45.4) | 171.7 (47.9) | 169.7 (41.5) | 170.9 (51.9) | 171.0 (38.1) |
| Hollingshead SES | 56.9 (12.0) | 53.1 (15.4) | 56.5 (12.8) | 52.2 (15.4) | 56.6 (14.0) | 53.1 (13.8) |
| Positive Affect | 29.4 (10.3) * | 35.3 (8.8) | 35.3 (9.4) * | 28.3 (9.2) | 32.7 (10.1) | 32.4 (9.7) |
| Negative Affect | 23.3 (7.95) * | 15.8 (6.1) | 17.6 (7.5) * | 21.9 (8.0) | 20.4 (8.2) | 18.1 (7.5) |
| Current MDD | 29% * | 0% | 9% | 20% | 17% | 10% |
| Current Anxiety | ||||||
| Disorder | 33% * | 0% | 13% | 20% | 21% | 10% |
| Lifetime Psychological Disorders | ||||||
| MDD | 65% * | 18% | 30% * | 55% | 46% | 33% |
| Anxiety Disorder | 42% * | 5% | 17% | 30% | 29% | 15% |
| Alcohol Dependence | 83% * | 32% | 47% * | 70% | 56% | 56% |
| Drug Dependence | 50% | 48% | 48% | 50% | 54% | 44% |
Significant group difference, p < .05. All group differences measured with t-test and chi-square test.
MDD = Major Depressive Disorder
All Cox proportional hazards regression results are presented in Table 2, which depicts effects on lapse rate within the first 7 days of the self-initiated quit attempt. Initial unadjusted analyses yielded significant effects on lapse rate by PTSD status, cessation self-efficacy, and SES. Ethnicity was marginally significant at the .10 alpha level. These variables, as well as gender, were retained for multiple regression analysis. All other variables (lifetime anxiety disorder other than PTSD, lifetime major depressive disorder, lifetime alcohol dependence, lifetime drug dependence, age, and menthol cigarette use) failed to be significantly related to rate of smoking lapse in unadjusted analysis, and were excluded from subsequent analyses.
Table 2. Cox Proportional Hazards Regressions Predicting Lapse Rate.
| Variable | Unadjusted Hazard Ratio | Adjusted Hazard Ratio | Interaction Model Hazard Ratio | |||
|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | p | Hazard Ratio (95% CI) | p | Hazard Ratio (95% CI) | p | |
| PTSD Group | 1.61 (1.06, 2.46) | .026 | 1.58 (1.02, 2.43) | .039 | 4.06 (1.74, 9.49) | .003 |
| Ethnicity (Ref: White) | 1.48 (0.96, 2.28) | .074 | 1.24 (0.80, 1.94) | .340 | 1.63 (0.72, 3.68) | .207 |
| Gender (Ref: Female) | 1.00 (0.66, 1.52) | .983 | 1.36 (0.88, 2.10) | .161 | 0.98 (0.39, 2.46) | .290 |
| Self-efficacy | 1.00 (0.99, 1.00) | .042 | 0.99 (0.99, 1.00) | .015 | 0.99 (0.99, 1.00) | .047 |
| Hollingshead SES | 1.03 (1.02, 1.05) | < .001 | 1.03 (1.01, 1.05) | < .001 | 1.03 (1.01, 1.05) | .001 |
| Fagerström | 1.08 (0.97, 1.19) | .163 | - | - | ||
| Age | 1.02 (1.00, 1.04) | .130 | - | - | ||
| Menthol Cigarette Smoker | 1.12 (0.73, 1.70) | .613 | - | - | ||
| Current MDD | 1.38 (0.76, 2.48) | .289 | - | - | ||
| Current Other Anxiety Disorder | 1.33 (0.76, 2.31) | .321 | - | - | ||
| Lifetime Anxiety Disorder | 1.20 (0.73, 1.95) | .476 | - | - | ||
| Lifetime MDD | 0.96 (0.63, 1.47) | .863 | - | - | ||
| Lifetime Alcohol Dependence | 1.14 (0.75, 1.73) | .537 | - | - | ||
| Lifetime Drug Dependence | 0.91 (0.60, 1.37) | .646 | - | - | ||
| PTSD × Minority | - | - | 0.30 (0.12, 0.74) | .009 | ||
| Gender × Minority | - | - | 2.03 (0.82, 5.02) | 1.26 | ||
| PTSD × Gender | - | - | 0.75 (0.31, 1.83) | .529 | ||
| Likelihood Ratio | 27.08* | 37.90* | ||||
p < .05.
SES = socioeconomic status; MDD = Major Depressive Disorder
The covariate-adjusted model demonstrated significantly increased fit over the null model (see Table 2). PTSD was associated with a reduced time to lapse, whereas cessation self-efficacy was associated with an increased time to lapse. Black smokers lapsed marginally more quickly than Whites, but the effect failed to reach statistical significance. When interaction variables for PTSD X Ethnicity, PTSD X Gender, and Ethnicity X Gender were added to the multivariate model, model fit was significantly increased, as assessed by the log-likelihood ratio change score, ΔX2(3) = 10.82, p = .013. PTSD X Ethnicity was the only interaction term to significantly predict lapse rate.
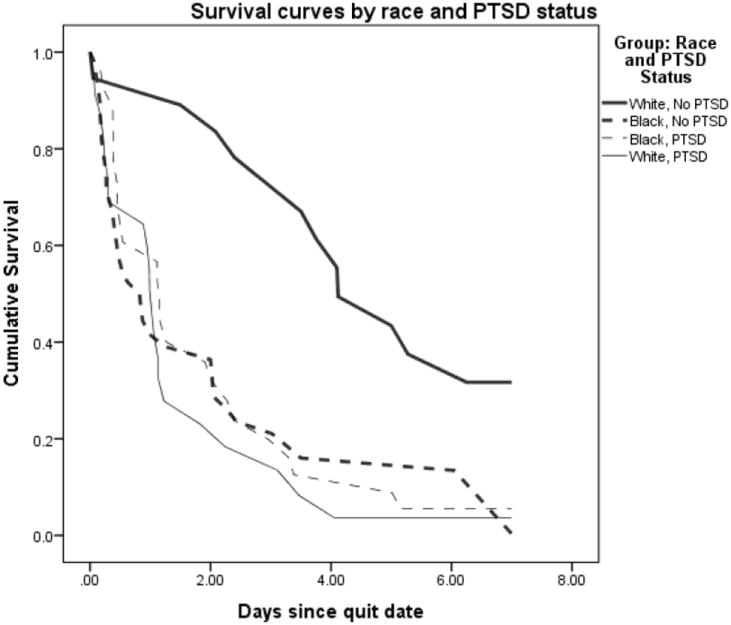
The PTSD X Ethnicity interaction was probed with simple plots. When ethnicity was considered a modifier, the effect of PTSD on smoking lapse was significant for Whites (HR = 6.19, p < .001) but not for Blacks (HR = 1.01, p = .974). White smokers without a PTSD diagnosis lapsed at a significantly slower rate than all other participants, including Black participants with and without PTSD as well as White participants with PTSD (see Figure 1).
Figure 1. Adjusted cumulative survival function for post-quit smoking lapse, minority status by PTSD interaction.
4. Discussion
This study yielded several findings with relevance for clinical treatment and provided the first prospective examination of how the effect of PTSD on time to lapse is moderated by ethnicity. In considering intervention in the early course of a smoking cessation attempt, the presence of PTSD is an established risk factor for early lapse. This report provided data suggesting that the effect of PTSD on early lapse is particularly evident in White smokers.
Results indicated that for Black smokers, PTSD may not present an additional risk to smoking lapse within the first week of quitting. This finding contrasts with results from a previous study in which Axis I psychiatric disorder was associated with decreased one-year smoking abstinence in Black smokers (Hickman et al., 2010). However, it is important to note that the study by Hickman and colleagues included individuals quitting smoking through a variety of methods, while our study provided behavioral counseling only. This could explain the higher rate of abstinence in the previous study, as nearly all of the Black smokers in our study lapsed in the first week. Our findings are more similar to those of Kivienimi and colleagues (2011), who found that psychological distress was associated with smoking behavior in Whites, but not Black or Latino/a smokers. The increase in negative affect associated with smoking cessation may function differently in Black smokers. Previous literature has suggested difficulty quitting smoking in Black smokers (King, Polednak, Bendel, Vilsaint, & Nahata, 2004), so it is possible that the levels of smoking cessation are already decreased in Black smokers due to other environmental or cultural factors that are more influential than psychiatric disorders such as PTSD. In contrast, elevated smoking cessation rates in Whites could be more sensitive to the influence of psychiatric disorders. It is possible that the absence of an effect of PTSD on early success in smoking cessation is due to limited variability, as nearly all Black smokers lapsed. Given efficacious intervention to increase cessation rates for Black smokers, the effect of PTSD may emerge in this population. However, additional research is needed to demonstrate this effect.
This study was limited by the lack of data from other minority ethnic groups in the community in which this study took place (e.g., Latino/a smokers). In addition, the short time to follow up means that these results can only be used to characterize the early quit experience. Further prospective research will be needed to determine how sociodemographic factors and interactions relate to long-term relapse, initiation of additional cessation attempts, and eventual abstinence. Though participants in this study received smoking cessation counseling, they did not receive pharmacotherapy or nicotine replacement, so results do not generalize to quit attempts using pharmacological smoking cessation methods to reduce craving and withdrawal.
Future studies of smoking cessation could benefit from inclusion of nicotine metabolism measures. Such measures could clarify to what extent the effects of psychiatric disorder and ethnicity on smoking cessation are due to physiological differences in how nicotine is metabolized prior to and during a quit attempt, or to environmental factors. Because Blacks smokers quit at lower rates than Whites, targeted smoking cessation interventions are warranted. One such smoking cessation intervention was culturally adapted for Black Americans and demonstrated increased efficacy compared to a non-targeted treatment (Matthews, Sánchez-Johnsen, & King, 2009).
5. Conclusions
The data presented in the current report are consistent with previous empirical research (Kiviniemi et al., 2011), suggesting that PTSD is not as closely related to smoking cessation success in Black smokers. As a result, biological and sociocultural factors influencing the cessation process in Black smokers are in need of further research. There is a need to go beyond previously identified sociocultural barriers to smoking cessation (e.g., low income and discrimination) in order to evaluate additional metabolic processes, social norms, attitudes, and social pressures that may further contribute to cessation outcomes.
Highlights.
Black ethnicity significantly moderated the effect of PTSD on time to first smoking lapse after quit date
PTSD significantly predicted time to smoking lapse for White smokers only
White smokers without PTSD lapsed at a significantly slower rate compared to Black smokers with/without PTSD and to White smokers with PTSD
Socioeconomic status predicted rate of smoking lapse independent of ethnicity
Acknowledgments
This work was supported primarily by the National Cancer Institute grant 2R01 CA091595 and the National Institute on Drug Abuse grant 2K24 DA016388, and the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development Clinical Science. The authors would like to thank the participants who volunteered to participate in this study. The views expressed in this presentation are those of the authors and do not necessarily represent the views of the National Institutes of Health or the Department of Veterans Affairs.
Role of Funding Sources
This work was supported primarily by the National Institutes of Health Grants R01CA081595, R01CA81595-07S1, K24DA016388, R21DA019704, and R21CA128965; the Department of Veterans Affairs Office of Research and Development, Clinical Science; and the Mid-Atlantic Mental Illness Research Education and Clinical Center.
Footnotes
Contributors
Drs. Beckham and Calhoun designed the parent study and wrote the protocol. Ms. Wilson conducted literature searches and devised specific hypotheses relevant to the current study. Ms. Dennis and Ms. Kirby oversaw data collection and prepared the dataset for analysis. Dr. Dennis conducted the statistical analysis. Ms. Wilson and Dr. Dedert wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Beckham JC, Calhoun PS, Dennis MF, Wilson SM, Dedert EA. Predictors of lapse in first week of smoking abstinence in PTSD and non-PTSD smokers. Nicotine & Tobacco Research. 2013;15:1122–1129. doi: 10.1093/ntr/nts252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckham JC, Dennis MF, McClernon FJ, Mozley SL, Collie CF, Vrana SR. The effects of cigarette smoking on script-driven imagery in smokers with and without posttraumatic stress disorder. Addictive Behaviors. 2007;32:2900–2915. doi: 10.1016/j.addbeh.2007.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz NL. Clinical pharmacology of nicotine: Implications for understanding, preventing, and treating tobacco addiction. Clinical Pharmacology & Therapeutics. 2008;83:531–541. doi: 10.1038/clpt.2008.3. [DOI] [PubMed] [Google Scholar]
- Benowitz NL, Lessov-Schlaggar CN, Swan GE, Jacob P. Female sex and oral contraceptive use accelerate nicotine metabolism. Clinical Pharmacology & Therapeutics. 2006;79:480–488. doi: 10.1016/j.clpt.2006.01.008. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered posttraumatic stress disorder scale. Journal of Traumatic Stress. 1995;8:75–80. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Breslau N, Novak SP, Kessler RC. Daily smoking and the subsequent onset of psychiatric disorders. Psychological Medicine. 2004;34(2):323–333. doi: 10.1017/s0033291703008869. [DOI] [PubMed] [Google Scholar]
- Breslow NE. Covariance analysis of censored survival data. Biometrics. 1974;30:89–100. [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting & Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Cook JW, McFall MM, Calhoun PS, Beckham JC. Posttraumatic stress disorder and smoking relapse: A theoretical model. Journal of Traumatic Stress. 2007;20:989–998. doi: 10.1002/jts.20275. [DOI] [PubMed] [Google Scholar]
- Davidson JRT, Book SW, Colket JT, Tupler LA, Roth S, David D, Hertzberg MA, Mellman T, Beckham JC, Smith RD, Davidson RM, Katz R, Feldman ME. Assessment of a new self-rating scale for posttraumatic stress disorder: The Davidson Trauma Scale. Psychological Medicine. 1997;27:153–160. doi: 10.1017/s0033291796004229. [DOI] [PubMed] [Google Scholar]
- Dedert EA, Calhoun PS, Harper LA, Dutton CE, McClernon FJ, Beckham JC. Smoking withdrawal in smokers with and without posttraumatic stress disorder. Nicotine & Tobacco Research. 2012;14:372–376. doi: 10.1093/ntr/ntr142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derby KS, Cuthrell K, Caberto C, Carmella SG, Franke AA, Hecht SS, Murphy SE, Marchand LL. Nicotine metabolism in three ethnic/racial groups with different risks of lung cancer. Cancer Epidemiology, Biomarkers & Prevention. 2008;17:3526–3535. doi: 10.1158/1055-9965.EPI-08-0424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldner MT, Babson KA, Zvolensky MJ. Smoking, traumatic event exposure, and post-traumatic stress: A critical review of the empirical literature. Clinical Psychology Review. 2007;27:14–45. doi: 10.1016/j.cpr.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM-IV Disorders. New York, NY: Biometrics Research Department; 1994. [Google Scholar]
- Gwaltney J. Relapse situation efficacy questionnaire (RSEQ) Journal of Consulting and Clinical Psychology. 2001;69:516–527. [PubMed] [Google Scholar]
- Hapke U, Schumann A, Rumpf HJ, John U, Konerding U, Meyer C. Association of smoking and nicotine dependence with trauma and posttraumatic stress disorder in a general population sample. Journal of Nervous & Mental Disease. 2005;193:843–846. doi: 10.1097/01.nmd.0000188964.83476.e0. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hickman NJ, Delucchi KL, Prochaska JJ. A population-based examination of cigarette smoking and mental illness in Black Americans. Nicotine & Tobacco Research. 2010;12:1125–1132. doi: 10.1093/ntr/ntq160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB, Redlich RL. Social class and mental illness. New York: John Wiley; 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hukkanen J, Jacob P, Benowitz NL. Metabolism and disposition kinetics of nicotine. Pharmacological Review. 2005;57:79–115. doi: 10.1124/pr.57.1.3. [DOI] [PubMed] [Google Scholar]
- Japuntich SJ, Leventhal AM, Piper ME, Bolt DM, Roberts LJ, Fiore MC, Baker TB. Smoker characteristics and smoking-cessation milestones. American Jouranal of Preventive Medicine. 2011;40:286–294. doi: 10.1016/j.amepre.2010.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King G, Polednak A, Bendel R, Vilsaint M, Nahata S. Disparities in smoking cessation between African Americans and Whites: 1990–2000. American Journal of Public Health. 2004;94:1965–1971. doi: 10.2105/ajph.94.11.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiviniemi MT, Orom H, Giovino GA. Psychological distress and smoking behavior: The nature of the relation differs by race/ethnicity. Nicotine & Tobacco Research. 2011;13:113–119. doi: 10.1093/ntr/ntq218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenen KC, Hitsman B, Lyons MJ, Niaura R, McCaffery J, Goldberg J, Tsuang M, et al. A twin registry study of the relationship between posttraumatic stress disorder and nicotine dependence in men. Archives of General Psychiatry. 2005;62(11):1258. doi: 10.1001/archpsyc.62.11.1258. [DOI] [PubMed] [Google Scholar]
- Matthews AK, Sánchez-Johnsen L, King A. Development of a culturally targeted smoking cessation intervention for African American smokers. Journal of Community Health. 2009;34:480–492. doi: 10.1007/s10900-009-9181-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakajima M, Fukami T, Yamanaka H, Higashi E, Sakai H, Yoshida R, Kwon JT, McLeod HL, Yokoi T. Comprehensive evaluation of variability in nocotine metabolism and CYP2A6 polymorphic alleles in four ethnic populations. Clinical Pharmacology & Therapeutics. 2006;80:282–297. doi: 10.1016/j.clpt.2006.05.012. [DOI] [PubMed] [Google Scholar]
- Perez-Stable EJ, Herrera B, Jacob P, Benowitz NL. Nicotine metabolism and intake in black and white smokers. Journal of the American Medical Association. 1998;280:152–156. doi: 10.1001/jama.280.2.152. [DOI] [PubMed] [Google Scholar]
- Piper ME, Cook JW, Schlam TR, Jorenby DE, Smith SS, Bolt DM, Loh W. Gender, race, and education differences in abstinence rates among participants in two randomized smoking cessation trials. Nicotine & Tobacco Research. 2010;12:647–657. doi: 10.1093/ntr/ntq067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum P, O’Shea R. Large-scale study of Freedom from Smoking clinics - factors in quitting. Public Health Reports. 1992;107:150–155. [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Gibson LE, Vujanovic AA, Gregor K, Bernstein A, Kahler C, Lejuez CW, Brown RA, Feldner MT. Impact of posttraumatic stress disorder on early smoking lapse and relapse during a self-guided quit attempt among community-recruited daily smokers. Nicotine & Tobacco Research. 2008;10:1415–1427. doi: 10.1080/14622200802238951. [DOI] [PubMed] [Google Scholar]


