Abstract
Controversy exists regarding the safety and performance benefits of performing the squat exercise to depths beyond 90° of knee flexion. Our aim was to compare the net peak external knee flexion moments (pEKFM) experienced over typical ranges of squat loads and depths. Sixteen recreationally trained males (n = 16; 22.7 ± 1.1 yrs; 85.4 ± 2.1 kg; 177.6 ± 0.96 cm; mean ± SEM) with no previous lower limb surgeries or other orthopedic issues and at least one year of consistent resistance training experience while utilizing the squat exercise performed single repetition squat trials in a random order at squat depths of above parallel, parallel, and below parallel. Less than one week before testing, one repetition maximum (1RM) values were found for each squat depth. Subsequent testing required subjects to perform squats at the three depths with three different loads: unloaded, 50% 1RM, and 85% 1RM (nine total trials). Force platform and kinematic data were collected to calculate pEKFM. To assess differences among loads and depths, a two-factor (load and depth) repeated-measures ANOVA with significance set at the P < 0.05 level was used. Squat 1RM significantly decreased 13.6% from the above parallel to parallel squat and another 3.6% from the parallel to the below parallel squat (P < 0.05). Net peak external knee flexion moments significantly increased as both squat depth and load were increased (P ≤ 0.02). Slopes of pEKFM were greater from unloaded to 50% 1RM than when progressing from 50% to 85% 1RM (P < 0.001). The results suggest that that typical decreases in squat loads used with increasing depths are not enough to offset increases in pEKFM.
Keywords: biomechanics, deep flexion, back, joint, moment
INTRODUCTION
The back squat exercise is utilized in a wide variety of environments ranging from clinical rehabilitation to formal strength and conditioning programs to everyday gym environments. The squat exercise is popular because of its similarity and applicability to both activities of daily living and many athletic movements, and it is a multi-joint movement that requires many large muscle groups to function together (19, 24, 32). Many health professionals whose focus is on performance enhancement often recommend the squat exercise to increase ligament, tendon, and bone strength; develop strength, speed, and power of the lower back, hip and knee musculature; and improve neuromuscular efficiency (7, 31). However, other health professionals whose primary focus is rehabilitation after knee injury list the deep squat as a contraindicated exercise (5) and recommend performing the squat exercise with limited knee flexion due to the commonly held belief that the squat exercise may elicit dangerously high forces on the knee (15, 29). In spite of the large body of work performed studying the squat exercise (4, 6, 9, 11, 19, 26, 29, 30, 32, 33, 35, 36, 38, 41, 42), it remains difficult to reconcile the differences in recommendations between these two schools of thought due to lack of a comprehensive study comparing squats as recommended by both (11, 29).
The American College of Sports Medicine (ACSM) recommends that when engaging in resistance training, the apparently healthy adult should “perform every exercise through a full range of motion” (16). Working through a full range of motion allows for strength adaptations to occur at every angle the joint moves through, which may reduce injury potential in those ranges. In addition, utilizing full range of motion maintains flexibility for joint integrity. Some coaches even utilize the deep squat as an assessment tool for lower body flexibility and symmetry of movement (8). In addition, squatting type activities are widespread in many cultures where squatting below parallel is commonplace when toileting or resting (28). Even though many health professionals agree that working through full range of motion is important, the knee joint, and specifically the squat, are often seen as exceptions to the rule.
Many health professionals often recommend limiting squat depth to parallel or higher under the assumption that doing so will reduce the potential of knee laxity and minimize harmful forces at the knee joint (21), yet some studies have called into question the assumptions regarding muscle activation and knee laxity. In an electromyography study, Caterisano et al. found that increasing squat depth only resulted in increased relative contribution of the gluteus maximus (4). In a study of instrumented laxity, Chandler et al. reported no difference in knee laxity following an 8 week training program including either above parallel or below parallel squats (6). Chandler et al. also found that both powerlifters and weightlifters had less laxity, i.e. “tighter” knees, than controls (6). The concern for harmful forces at the knee centers on peak patellofemoral joint reaction force (pPFJRF), which may lead to patellofemoral pain syndrome (PFPS) by overloading the cartilage, potentially leading to cartilage degeneration and subsequent subchondral bone degeneration (23). PFPS is one of the most common disorders of the knee, accounting for nearly 30% of all knee injuries treated in sports medicine clinics and influencing both athletes and non-athletes alike (10, 13, 23). If the relationship between pPFJRF and PFPS is correct, it would be beneficial to understand how pPFJRF is influenced by variations in the squat exercise.
Previous biomechanical analyses have indicated that increased pPFJRF is coupled with increased knee flexion angles (9, 33). In squats up to 90° of knee flexion without an external load and with a load of 35% of subject’s body weight, pPFJRF was found to increase linearly with peak external knee flexion moments (pEKFM) in untrained males (38). Dahlkvist et al. estimated increases in pPFJRF while squatting to full depth in an unconventional squat with no external load where the heels do not remain on the ground (9). In contrast, when comparing squats with knee flexion angles of 70°, 90°, and 110° in trained females, Salem and Powers found no differences in pEKFM or pPFJRF with an 85% one repetition maximum (1RM) load (35). It is difficult to interpret these conflicting reports on knee loading due to the large variations between studies in load and technique. In addition, when basing loads off of 1RM values, 1RM values for each squat depth are not often independently tested. In studies using a conventional squat movement, pEKFM was found to be the major contributor of both pPFJRF as well as patellofemoral stresses (35, 38). Given the strong agreement between pEKFM and pPFJRF at flexion angles where both have been experimentally observed and the lack of data on pPFJRF above 110° of knee flexion, for this study we examined pEKFM as a surrogate for pPFJRF.
Our aim was to compare pEKFM during the squat with loads and depths that are often prescribed in both rehabilitation and strength training programs, including depth-specific 1RM measurements. To achieve our aim we tested the hypothesis that back squat 1RM will decrease with increased depth (i.e. above parallel 1RM > parallel 1RM > below parallel 1RM) and this decrease in 1RM would allow pEKFM to remain constant for load- and depth- matched squats (i.e. pEKFM for above parallel with 85% above parallel 1RM ≈ pEKFM for below parallel squat with 85% below parallel 1RM).
METHODS
Experimental Approach to the Problem
To investigate the effect of commonly prescribed squat loads and depths on pEKFM, nine combinations of differing loads and depths were analyzed. The three pre-determined depths consisted of the thigh being above parallel, parallel, and below parallel to the ground. These depths were defined as follows: the above parallel squat, to 90° of knee flexion; the parallel squat, to where the inguinal crease falls just below the proximal patella; and the below parallel squat or deep squat, to when the backs of the thighs come into contact with the calves. Normalized loading conditions were calculated based on the 1RM loads determined at each of the three depths. The three loads chosen for each depth were unloaded, 50% 1RM, and 85% 1RM. An unloaded squat may be prescribed during rehabilitation from injury or during the initial periods of learning. Loads of 50% 1RM and 85% 1RM are frequently used for power and strength training, respectively. The order of the nine trials was randomly chosen for each subject. Peak external knee flexion moments were determined for each trial.
Subjects
Sixteen healthy, recreationally trained males (n = 16; 22.7 ± 1.1 yrs; 85.4 ± 2.1 kg; 177.6 ± 0.96 cm; mean ± SEM) with no previous lower limb surgeries or other orthopedic issues and at least one year of consistent resistance training experience while utilizing the squat exercise participated in the study. All subjects were visually assessed for the ability to squat at full depth without pain and with appropriate technique including the maintenance of having both heels in contact with the ground and proper lumbar lordosis throughout the whole movement. Experimental protocols were approved by the Institutional Review Board at The Ohio State University and written informed consent was obtained by each subject following a full presentation of procedures.
Procedures
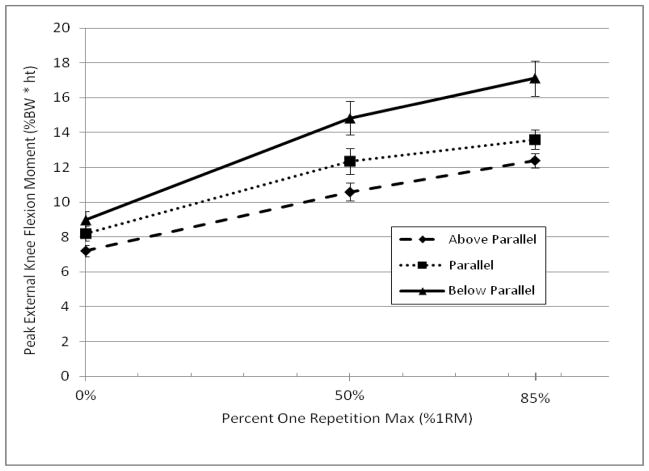
Data were collected during two separate sessions with greater than 24 hours and less than 1 week between sessions. All testing was conducted during the months of January-March. Subjects were instructed to maintain their typical daily routine in regards to hydration, nutrition, and sleep and to not engage in any heavy physical activity several days prior to testing. One repetition max (1RM) testing was performed during the first session following recommendations set forth by the National Strength and Conditioning Association (3). Subjects performed their normal warm-up typically done before squatting. The above parallel squat depth was determined by measuring 90° of knee flexion using a goniometer placed at the knee (Figure 1A). The parallel squat depth was determined when the inguinal crease fell just below the proximal patella (17) (Figure 1B). The below parallel squat depth was determined when the subject sat fully in a squat position where the hamstrings come into contact with the calves (Figure 1C). Subjects were instructed to take a natural stance. Order of 1RM testing was not randomized and started with the below parallel squat and ended with the above parallel squat as generally the 1RM is lower for the below parallel squat. Subjects were given as much time as they desired between attempts but took no less than 1 minute for each rest interval. Previous research has found that rest intervals as short as 1 minute do not affect 1RM back squat performance when a repeated 1RM attempt is made (25). Test-retest reliability for 1RM back squat testing has resulted in an intraclass correlation coefficient of r = 0.94 (P < 0.05) (25). Following 1RM testing, the second session was scheduled between 24 hours and 7 days later.
Figure 1.
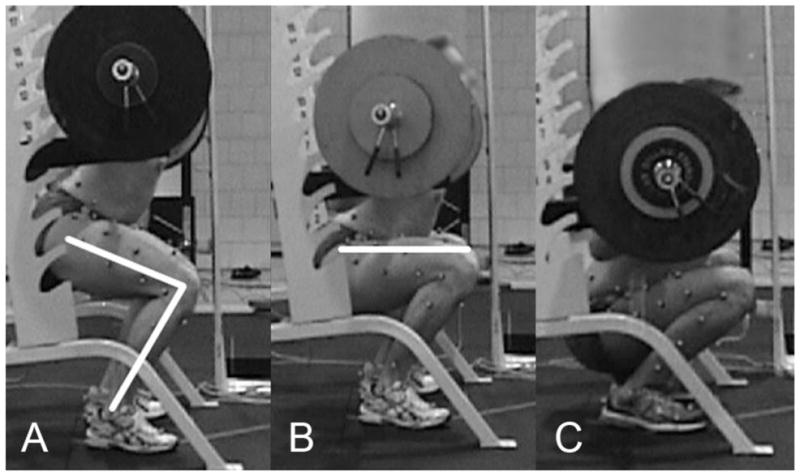
Above parallel (A); parallel (B); and below parallel (C) back squat.
A specially designed “light curtain” device (Banner Engineering Corp., Minneapolis, MN), visible signal light and programmable logic controller (Allen-Bradley Corp., Milwaukee, WI) were used to provide feedback to the subject to control squat depth and to limit any bouncing or inconsistencies in the amount of time in the bottom squat position for both 1RM and motion capture testing (Figure 2). The light curtain is a device that senses when an object passes through a rectangular “curtain” of infrared light between the two parts of the device. The position of the curtain was adjusted to the barbell height for each subject corresponding to each of the squat depths. The visible signal light indicated to the subject when to descend, when to hold in the bottom position, and when to ascend again. This technique ensured that each subject consistently descended to the appropriate depth for each trial and stayed at that depth for one second before ascending back to standing.
Figure 2.
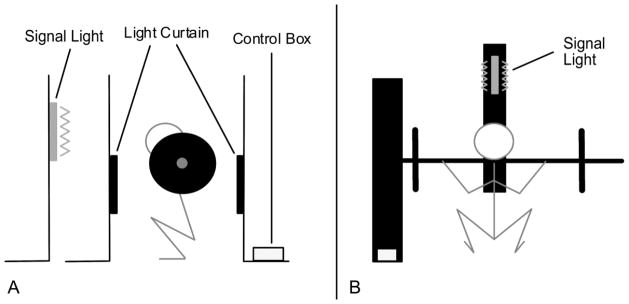
Light curtain setup. Sagittal view (A); posterior view (B).
Motion capture analysis was conducted during the second session. Retro-reflective markers (B&L Engineering, Santa Ana, CA) were attached to the legs of each subject with two-sided latex-free adhesive tape utilizing a modified Point-Cluster Technique (PCT) (1, 12) (Figure 3). This technique has shown comparable results to those obtained with intra-cortical pins placed into the femur and tibia (1) and has been used to study knee kinematics during walking and seated leg extension (12), run-to-cut maneuvers (20), and with ACL-reconstructed and uninjured contralateral knees (37). The modifications included a marker placed at the manubrium, as well as a ring of eight markers placed on the iliac spine including the anterior and posterior superior iliac spines, iliac crests, and the midpoints between iliac crest and posterior superior iliac spine markers. Nine total trials were randomly assigned, each containing a unique combination of squat depth (above parallel, parallel, or below parallel) and load (unloaded, 50% 1RM and 85% 1RM of the squat depth being performed). Unloaded squat trials consisted of the subject squatting with a PVC pipe held in the same position as a barbell to best mimic the normal squatting style for each subject. Loaded squats utilized a standard Olympic barbell and weight plates. Subjects were encouraged to use the same squatting style that they typically use in training. All subjects utilized a high bar technique with heels remaining in contact with the floor, a natural stance (43.91 ± 6.7 cm between markers on the posterior aspect of the heel; across all trials), a forward or upward gaze, and maintained lumbar lordosis throughout the squat. Marker motion and ground reaction force data were recorded using an eight camera Vicon MX-F40 system (Oxford Metrics, Oxford, UK), two Bertec 4060-10 force plates (Bertec Corporation, Columbus, OH), and Vicon Nexus software (Oxford Metrics, Oxford, UK). Three-dimensional marker data was filtered using a General Cross-Validation (GCV) Woltring filter (40) within Vicon Nexus. Custom scripts in MATLAB (The Mathworks, Natick, MA) and Vicon Bodybuilder (Oxford Metrics, Oxford, UK) were then used to calculate knee kinematics and kinetics, following previously-described methods for processing point-cluster data (1) and calculating net external joint reaction moments (2), using conventions for tibiofemoral kinematics described by Grood and Suntay (18). Peak external knee flexion moments (Nm) were normalized by body weight (BW, N) and height (ht, m) to obtain pEKFM (%BW*ht) used for analysis (27). Slopes of the pEKFM vs. %1RM curves were also calculated for analysis.
Figure 3.
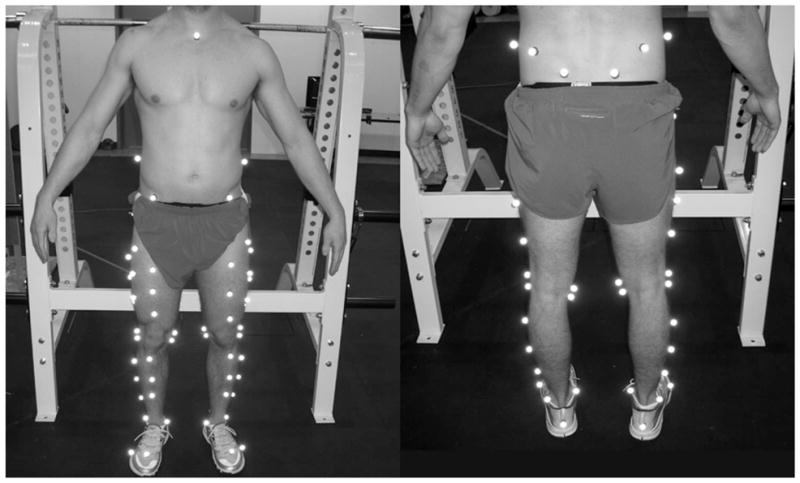
Marker placement utilizing the Point-Cluster Technique.
Statistical Analyses
A one-way repeated measures ANOVA was used to compare 1RM at each squat depth. Two separate two-way repeated measures ANOVA (depth*load and depth*load progression) were used to compare pEKFM and slopes. T-tests were used as a post-hoc analysis when a significant F-ratio was observed from the ANOVA. A Bonferroni correction was used for multiple comparisons. All data analyses were performed using SPSS version 19.0 (IBM SPSS Statistics Inc., Chicago, IL). Significance levels were set at P < 0.05. All data are presented as mean ± SEM.
RESULTS
Significant differences were found for squat 1RM at each depth (F1.50, 21.88 = 61.21, P < 0.001). The largest 1RM was found for the above parallel squat at 150.42 ± 4.92 kg decreasing to 129.97 ± 4.82 kg and 125.28 ± 4.34 kg (P < 0.05) for the parallel and below parallel squats, respectively (Figure 4).
Figure 4.
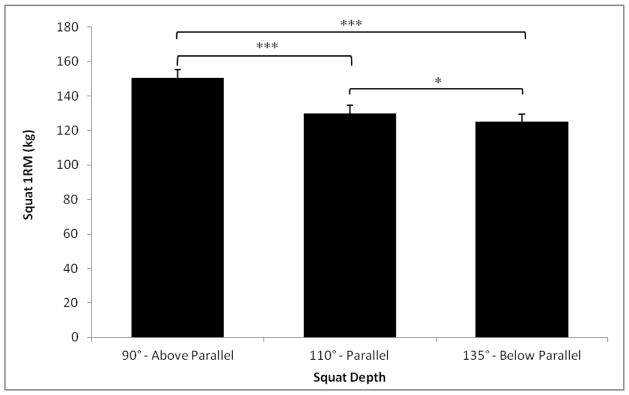
Squat 1RM values. Data are presented as mean ± SE (n = 16). Significant difference (* P < 0.05; *** P < 0.001) between 1RM values.
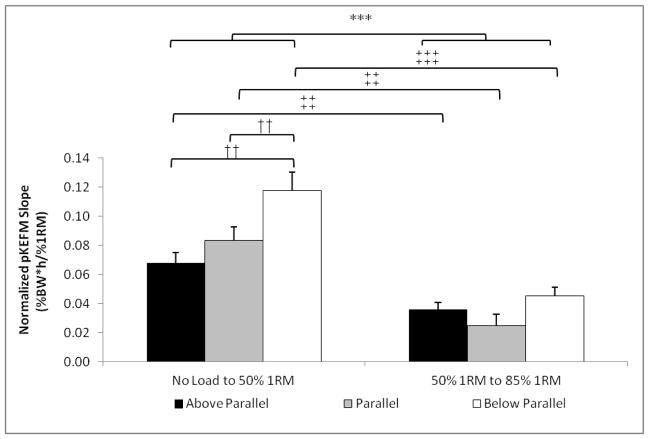
Significant main effects were found for load (F1.35, 20.29 = 191.36, P < 0.001) and depth (F1.23, 18.38 = 45.69, P < 0.001) in addition to a significant interaction effect for depth*load (F1.93, 28.87 = 10.18, P = 0.001) for pEKFM (Figure 5). Increases in either load or depth for the back squat exercise significantly increased pEKFM. Within each %1RM or squat depth, each point was significantly different from the other two (P ≤ 0.02; Figure 5).
Figure 5.
Normalized peak external knee flexion moments (%BW*ht) vs. normalized weight on the bar (%1RM). Data are presented as mean ± SE (n = 16). All trials were significantly different (P ≤ 0.02).
To check the consistency of knee flexion angle at different depths, peak knee flexion angles were calculated for each of the nine conditions (Table 1). On average, subjects squatted to a knee flexion angle of 98.73 ± 1.54° for the above parallel squat, 123.70 ± 2.03° for the parallel squat, and 140.51 ± 2.00° for the below parallel squat. Significant differences were found in the knee flexion angle for the above parallel and parallel squats as load increased. During the above parallel squats, knee flexion angle decreased as the load increased from unloaded to 50% 1RM (P = 0.001) and again to 85% 1RM (P = 0.014). Subjects also squatted with a knee flexion angle of ~5° less during the parallel squats with an 85% 1RM load compared to the unloaded and 50% 1RM trials (P < 0.05). No differences were seen in knee flexion angles for the below parallel squats.
Table 1.
Peak knee flexion angles.
| No Load | 50% 1RM | 85% 1RM | Average | |
|---|---|---|---|---|
| Above Parallel | 105.05 ± 1.44 | 97.33 ± 1.99** | 93.82 ± 1.81***† | 98.73 ± 1.54 |
| Parallel | 125.07 ± 2.46 | 125.51 ± 2.12 | 120.51 ± 1.92*†† | 123.70 ± 2.03 |
| Below Parallel | 139.89 ± 2.09 | 141.78 ± 2.13 | 139.87 ± 2.23 | 140.51 ± 2.00 |
Data are presented as mean ± SE. Significant difference (* P < 0.05; ** P < 0.01; *** P < 0.001) from the no load condition. Significant difference († P < 0.05; †† P < 0.01) from the 50% 1RM condition.
Analysis of pEKFM slopes (the 6 lines in Figure 5) demonstrated significant main effects for increases in load (unloaded-50 vs. 50–85, F1, 15 = 26.42, P < 0.001) and squat depth (F2, 30 = 11.09, P < 0.001). A significant load*depth interaction effect was also observed (F2, 30 = 5.88, P = 0.007) (Figure 6). The average slope of pEKFM for all three depths from unloaded to 50% 1RM was 70% higher than the average slope from 50% 1RM to 85% 1RM. Specifically, above parallel (P = 0.007), parallel (P = 0.001) and below parallel (P < 0.001) squats show significantly steeper slopes of pEKFM while progressing from unloaded to 50% 1RM than from 50% 1RM to 85% 1RM (Figure 6, marked with ‡‡,‡‡‡). Additionally, the below parallel squat has a significantly steeper slope of pEKFM while progressing from unloaded to 50% 1RM compared to the parallel and above parallel squats (P ≤ 0.004, Figure 6, marked with††).
Figure 6.
Bar graphs of the slopes of the normalized peak external knee flexion moments (%BW*ht) vs. weight on the bar from Figure 4. Data are presented as mean ± SE (n = 16). Significant differences were observed in the average slopes across all depths (***, 0–50% vs. 50–85%, P < 0.001), between below parallel and the other depths when increasing from 0–50% (†† P < 0.01), and at each depth (0–50% vs. 50–85%, ‡‡ P < 0.01; ‡‡‡ P < 0.001).
DISCUSSION
The present study demonstrates that the typical decreases in squat load seen with increasing squat depth were not enough to offset the increases in pEKFM seen with increasing knee flexion. As either load or depth is increased, pEKFM also increased. Therefore our hypothesis was not supported. Moreover, increases in load on the bar from unloaded to 50% 1RM exhibit higher slopes of increased pEKFM than when increasing load from 50% 1RM to 85% 1RM. Although it is currently unknown what threshold of peak or repetitive forces would be detrimental to the knee joint, the data reported here can be used to help design and implement programs utilizing the back squat exercise.
Our findings are somewhat contrary to previous research involving the squat exercise conducted by Salem and Powers who found no difference in external knee flexion moments (reported as internal knee extension moments) at 70°, 90°, and 110° of knee flexion utilizing a load of 85% 1RM (38). The authors did not specify whether depth-specific 1RM values were found, but if they only determined a single 1RM for the whole study, that alone would account for the differences between their data and ours. Other potential reasons for these contradictory results may be that the previous study had a small sample size of 5 subjects and utilized female collegiate athletes.
Comparing our data to previously reported data for squatting is challenging due to the wide range of squatting styles, experience levels of subjects, loads utilized, and methodological differences. A summary of comparison data on studies that have reported pEFKM can be found in Table 2. The largest values for pEFKM were found by Escamilla et al. in a study of Masters level powerlifters (14). They reported values as high as 756 Nm for a 1RM squat with a wide stance. Although the loads were nearly double that of the above parallel back squat with an 85% 1RM load in our study, the pEKFM were over 4 times as high. Some of the lowest values were reported by Wallace et al. (38). Body weight squats with the hands behind the head and barbell squats utilizing 35% of the subject’s body weight (24.85 ± 5.6kg) to 90° of knee flexion gave pEKFM of 0.62 and 0.88 Nm/kg respectively. Comparatively, we observed pEKFM values that were nearly double although our knee flexion angles were ~10° larger and our loaded trial was ~3 times greater (75.21 ± 9.83kg) accounting for the differences.
Table 2.
Comparison of studies that quantified peak knee moments for the squat. Data are presented as mean ± SE.
| Author | No. of Subjects |
Gender | Mean Height (cm) |
Mean Weight (kg) |
Experience Level |
Exercise Description |
Mean Load (kg) |
Load Description |
Peak Knee Flexion |
Absolute Peak Knee Moment (Nm) |
Relative Peak Knee Moment (Nm/kg) [%BW * ht] |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cotter - Current Study | 16 | M | 177.6 ± 0.96 | 85.4 ± 2.1 | >1 year of squat training | Back Squat - Above Parallel | 0 | No Load | 105.05 ± 1.44 | 103.75 ± 4.79 | 1.21 ± 0.04 [7.21 ± 0.33] |
| 76.28 ± 2.47 | 50% 1RM | 97.33 ± 1.99 | 152.53 ± 7.37 | 1.78 ± 0.06 [10.59 ± 0.51] | |||||||
| 128.13 ± 4.21 | 85% 1RM | 93.82 ± 1.81 | 178.51 ± 5.78 | 2.09 ± 0.04 [12.40 ± 0.40] | |||||||
|
| |||||||||||
| Back Squat - Parallel | 0 | No Load | 125.07 ± 2.46 | 118.02 ± 6.22 | 1.38 ± 0.05 [8.20 ± 0.43] | ||||||
| 65.91 ± 2.48 | 50% 1RM | 125.51 ± 2.12 | 177.82 ± 10.9 | 2.07 ± 0.08 [12.35 ± 0.76] | |||||||
| 110.65 ± 4.12 | 85% 1RM | 120.51 ± 1.92 | 195.67 ± 7.96 | 2.29 ± 0.07 [13.59 ± 0.55] | |||||||
|
| |||||||||||
| Back Squat - Below Parallel | 0 | No Load | 139.89 ± 2.09 | 129.03 ± 7.22 | 1.51 ± 0.06 [8.96 ± 0.50] | ||||||
| 63.78 ± 2.17 | 50% 1RM | 141.78 ± 2.13 | 213.66 ± 13.75 | 2.48 ± 0.10 [14.84 ± 0.95] | |||||||
| 106.53 ± 3.76 | 85% 1RM | 139.87 ± 2.23 | 246.29 ± 14.61 | 2.87± 0.12 [17.11 ± 1.01] | |||||||
|
| |||||||||||
| Escamilla (13) | 13 | M | 176.7 ± 1.9 | 82.4 ± 6.0 | Master’s level Powerlifters | Narrow Stance Squat | 208.3 ± 15.2 | 1RM | 106 ± 2.2 | 573 ± 49.6 | |
| 13 | M | 173.6 ± 2.0 | 93.1 ± 6.9 | Mid Stance Squat | 229.2 ± 17.9 | 102 ± 1.9 | 627 ± 64.6 | ||||
| 13 | M | 174.3 ± 1.9 | 97.5 ± 7.8 | Wide Stance Squat | 238.7 ± 15.0 | 99 ± 2.8 | 756 ± 65.2 | ||||
|
| |||||||||||
| Gullet (18) | 15 | 9M 6F | 171.2 ± 1.7 | 69.7 ± 1.6 | >1 year of squat training | Back Squat - Parallel | 61.8 ± 4.8 | 70% 1RM | 1.0 ± 0.10 | ||
| Front Squat - Parallel | 48.5 ± 3.6 | 70% 1RM | 0.7 ± 0.05 | ||||||||
|
| |||||||||||
| Nissell and Ekholm (27) | 1 | M | 181 | 110 | Experienced Powerlifter | Back Squat - Parallel | 0 | No Load | 120 | 83.3 | |
| 100 | ~30% 1RM | 120 | 145 | ||||||||
| 250 | ~70% 1RM | 120 | 233.3 | ||||||||
|
| |||||||||||
| Robertson (31) | 6 | M | 184 | 83.65 | Experienced Weightlifters | Back Squat | 93.1 | 80% 1RM | 120 | 100 | |
|
| |||||||||||
| Salem and Powers (32) | 5 | F | 178 ± 4.7 | 73 ± 4.5 | 3 Basketball/2 Volleyball Intercollegiate Athletes | Shallow Squat | 53 ± 5.4 | 85% 1RM | 72.8 | 127.4 | |
| Medium Squat | 91.5 | 128.7 | |||||||||
| Deep Squat | 109.7 | 138.4 | |||||||||
|
| |||||||||||
| Salem (33) | 8 | 7M 1F | 93.3 ± 6.4 | ~30 weeks after ACLr | Back Squat - Involved Leg | 32.65 | 35% of body weight | 106.98 ± 3.68 | 1.02 ± 0.11 | ||
| Back Squat - Uninvolved Leg | 109.55 ± 4.06 | 1.28 ± 0.10 | |||||||||
|
| |||||||||||
| Wallace (34) | 15 | 6M 9F | 171 ± 2.3 | 72 ± 4.1 | Healthy Adults | Unloaded Squat | 0 | Hands behind head | 90 | 0.62 ± 0.03 | |
| Loaded Barbell Squat | 24.85 ± 1.4 | 35% of body weight | 90 | 0.88± 0.0.03 | |||||||
|
| |||||||||||
| Wilk (35) | 10 | M | 177 ± 2.8 | 93 ± 4.4 | Experienced Weightlifters | Parallel Squat | 147 ± 12.3 | 4 reps with 12RM weight | 104 ± 3.5 | 150 ± 12.6 | |
|
| |||||||||||
| Wretenberg (37) | 6 | M | 170.8 ± 3.3 | 87 ± 8.2 | Powerlifters | Parallel Squat | 154.2 ± 8.6 | 65% 1RM | 111 ± 2.0 | 92 ± 20.1 | |
| Deep Squat | 126 ± 1.6 | 139 ± 26.2 | |||||||||
| 8 | M | 177.0 ± 2.7 | 82 ± 3.9 | Weightlifters | Parallel Squat | 101.9 ± 9.8 | 65% 1RM | 116± 1.7 | 131 ± 6.1 | ||
| Deep Squat | 138± 1.1 | 191 ± 14.4 | |||||||||
The present study showed that the slope of pEKFM was greater when progressing from an unloaded squat to squatting with a 50% 1RM than when progressing from 50% 1RM to 85% 1RM with the greatest slope seen for the below parallel squat. This important finding suggests that as beginners or individuals in a rehabilitation program make initial progressions in load and depth, caution should be expressed as increases in pEKFM occur at greater rates during these times. Further research should examine the relationship between pEKFM and load across the entire range of weight on the bar from unloaded to 100%1RM.
Currently, the data in this study can be a useful guide to those involved in prescribing the squat exercise. Progression can be maximized by incorporating the principle of “progressive overload,” or the gradual increase of stress placed upon the body (22), which should be considered when prescribing the squat exercise. In order to control for pEKFM while still working towards full range of motion movement, these results suggest that a squat progression should start with unloaded above parallel squats and progress to deeper squats before the addition of load. Squat progression should again proceed from above parallel squats to deeper squats once a load has been added.
As noted in Table 1, subjects only squatted to a consistent depth for the below parallel squat. This has important safety implications for the squat exercise. Considering that increased squat depth requires reduced loads, going below an intended depth may lead to a failed repetition and a potential increased risk of injury. When loads were increased to 85% 1RM, subjects squatted approximately 5–10° less during the above parallel and parallel squats. This may be done to decrease the difficulty of the exercise as loads become heavier. With below parallel squats where the thighs come into contact with the calves, there is a natural stopping point as a lower depth cannot be achieved. This eliminates the possibility of unintentionally going below the intended depth where there is an increased probability of a failed repetition.
Although this study adds important insight into how load and depth affect forces about the knee, understanding the limitations of this study will allow for proper interpretation of the results. The retro-reflective marker movement that occurred with the deeper squats may have affected values reported in this study. As depth increased, the cluster of markers on the thigh became visibly deformed, potentially causing error in the estimated knee flexion angle. Due to the fact that inverse dynamics calculations proceed upward from the foot, error due to thigh deformation should have had minimal effect on the estimation of pEKFM, but deformations of the foot or shank are a potential source of error in pEKFM. Additionally, co-contraction from the hamstrings and gastrocnemius with the quadriceps was not considered. Co-contraction would cause pPFJRF to increase without a change in the pEKFM, lessening the value of pEKFM as a surrogate. Optimal placement of markers on the thigh and pelvis as well as including the effects of co-contraction should be considered for future studies.
All data were presented in response to one repetition for each given load and depth. Subjects were not in a fatigued state and therefore application of the results should be made accordingly. pEKFM will likely change as subjects become fatigued and their squat technique suffers.
Thigh-calf contact generally occurs during deeper squat depths of approximately 130° of knee flexion. Thigh-calf contact produces a moment in the same direction as that of the quadriceps muscle group thereby decreasing the actual net flexion moment at the knee, causing an overestimation of pEKFM in this study. Recent research has shown that tibiofemoral compressive force, shear force, and patellar tendon force decreased while squatting to full depth where thigh-calf contact occurred (42). Future studies should consider thigh-calf contact using pressure sensors or the like when examining knee forces during high flexion activities.
Generalizing the present results beyond young, healthy, recreationally trained males should be done with care. A number of technique differences between elite powerlifters classified as low-skill or high-skill have been previously found (26). It remains unknown whether larger differences exist between elite and recreational weightlifters, or whether differences between males and females exist in squatting mechanics. Moreover, the recreationally trained males in this study varied in their performance of the squat. Four of the subjects were not able to increase 1RM load as squat depth decreased from a below parallel to a parallel squat. Advanced lifters may show greater differences between 1RM loads at varying depths, which could result in altered pEKFM. Subjects differing in age, gender, height, weight, experience level and health status may exhibit altered biomechanics in comparison to the presented results.
The main finding of this study is that the 1RM decreases seen with increasing depth are not enough to offset the increases in pEKFM at loads consisting of unloaded, 50% 1RM and 85% 1RM. While progressing from unloaded to 50% 1RM, slopes of pEKFM are 70% greater than when progressing from 50% 1RM to 85% 1RM loads. To our knowledge this is the first study investigating pEKFM utilizing a range of typical loads and depths found in rehabilitation and performance training settings. Health and fitness professionals are advised to utilize the information presented here in addition to individual assessments to determine how to best incorporate the squat exercise into rehabilitation and training programs.
PRACTICAL APPLICATIONS
The back squat is a commonly prescribed exercise due to its similarity to activities of daily living and many sporting activities as well as being a multi-joint movement incorporating large muscle groups. The hypotheses were that back squat 1RM would decrease with increased depth, and that this decreased 1RM would allow pEKFM to remain constant for load- and depth-matched squats. However, reducing the load based on the decrease in 1RM was not enough to allow pEKFM to remain constant, i.e. a 50% 1RM squat to parallel still resulted in greater pEKFM than a 50% 1RM squat to above parallel when utilizing the 1RM for each depth. Based on these findings, the professional designing a progression for a client should take into account the large increase in knee loading from an unloaded squat to a load consisting of a 50% 1RM, as forces increase at the greatest rate during these loads. The largest forces about the knee were found with the 85% 1RM load at the below parallel depth. Proper progressions should be designed to allow the client to adapt to the increasing forces at the knee. Close supervision and correct spotting techniques should be incorporated, especially at depths in which the thighs do not come into contact with the calves, as going below the intended depth may result in failed attempts. Given the age, gender, height, weight, experience level and health status of the subjects involved in this study, extrapolating the results to those with differing characteristics should be done cautiously. The information here should be used as a reference point for program design involving the squat exercise after a comprehensive individualized assessment has been completed.
Acknowledgments
The authors would like to thank all the subjects for graciously volunteering their time and effort. Additionally, the authors are grateful for the volunteer students and their tremendous help in completing this study.
References
- 1.Andriacchi TP, Alexander EJ, Toney MK, Dyrby C, Sum J. A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. J Biomech Eng. 1998;120:743–749. doi: 10.1115/1.2834888. [DOI] [PubMed] [Google Scholar]
- 2.Andriacchi TP, Johnson TS, Hurwitz DE, Natarajan RN. Musculoskeletal dynamics, locomotion, and clinical applications. In: Mow VC, Huiskes R, editors. Basic Orthopaedic Biomechanics and Mechano-Biology. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. pp. 91–122. [Google Scholar]
- 3.Baechle TR, Earle RW, Wathen D. Resistance training. In: Baechle TR, Earle RW, editors. Essentials of Strength Training and Conditioning. Champaign: Human Kinetics; 2000. pp. 395–425. [Google Scholar]
- 4.Caterisano A, Moss RF, Pellinger TK, Woodruff K, Lewis VC, Booth W, Khadra T. The effect of back squat depth on the EMG activity of 4 superficial hip and thigh muscles. J Strength Cond Res. 2002;16:428–432. [PubMed] [Google Scholar]
- 5.Navy and Marine Corps Public Health Center. Navy physical training series: Contraindicated exercises. Norfolk, VA: 2008. [Google Scholar]
- 6.Chandler TJ, Wilson GD, Stone MH. The effect of the squat exercise on knee stability. Med Sci Sports Exerc. 1989;21:299–303. [PubMed] [Google Scholar]
- 7.Dunn B, Klein K, Kroll W, McLaughlin T, O’Shea P, Wathen D. Coaches roundtable: The squat and its application to athletic performance. Strength Cond J. 1984;6:10–23. [Google Scholar]
- 8.Cook G. Athletic body in balance. Human Kinetics; 2003. [Google Scholar]
- 9.Dahlkvist NJ, Mayo P, Seedhom BB. Forces during squatting and rising from a deep squat. Eng Med. 1982;11:69–76. doi: 10.1243/emed_jour_1982_011_019_02. [DOI] [PubMed] [Google Scholar]
- 10.Devereaux MD, Lachmann SM. Patello-femoral arthralgia in athletes attending a Sports Injury Clinic. Br J Sports Med. 1984;18:18–21. doi: 10.1136/bjsm.18.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drinkwater EJ, Moore NR, Bird SP. Effects of changing from full range of motion to partial range of motion on squat kinetics. J Strength Cond Res. 2012;26:890–896. doi: 10.1519/JSC.0b013e318248ad2e. [DOI] [PubMed] [Google Scholar]
- 12.Dyrby CO, Andriacchi TP. Secondary motions of the knee during weight bearing and non-weight bearing activities. J Orthopaed Res. 2004;22:794–800. doi: 10.1016/j.orthres.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Earl JE, Vetter CS. Patellofemoral pain. Phys Med Rehabil Clin N Am. 2007;18:439–458. doi: 10.1016/j.pmr.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Escamilla RF, Fleisig GS, Lowry TM, Barrentine SW, Andrews JR. A three-dimensional biomechanical analysis of the squat during varying stance widths. Med Sci Sports Exerc. 2001;33:984–998. doi: 10.1097/00005768-200106000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Escamilla RF, Fleisig GS, Zheng N, Lander JE, Barrentine SW, Andrews JR, Bergemann BW, Moorman CT., 3rd Effects of technique variations on knee biomechanics during the squat and leg press. Med Sci Sports Exerc. 2001;33:1552–1566. doi: 10.1097/00005768-200109000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Franklin B, Whaley M, Howley E, Balady G. ACSM’s Guidelines for Exercise Testing and Prescription: Testing and Prescription. Lippincott Williams and Wilkins; 2000. [Google Scholar]
- 17.Fry A, Aro T, Bauer J, Kraemer W. A comparison of methods for determining kinematic properties of three barbell squat exercises. J Hum Movement Stud. 1993;24:83–95. [Google Scholar]
- 18.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of 3-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 19.Gullett JC, Tillman MD, Gutierrez GM, Chow JW. A biomechanical comparison of back and front squats in healthy trained individuals. J Strength Cond Res. 2009;23:284–292. doi: 10.1519/JSC.0b013e31818546bb. [DOI] [PubMed] [Google Scholar]
- 20.Jamison ST, McNeilan RJ, Young GS, Givens DL, Best TM, Chaudhari AMW. RCT of the effects of a trunk stabilization program on trunk control and knee loading. Med Sci Sports Exerc. doi: 10.1249/MSS.0b013e31825a2f61. ePub available online, 2012. [DOI] [PubMed] [Google Scholar]
- 21.Kemper K, Ferguson M. Contraindicated exercises revisited. IDEA Fitness Journal. 2007;4:34–37. [Google Scholar]
- 22.Kraemer W, Ratamess N. Fundamentals of resistance training: progression and exercise prescription. Med Sci Sports Exerc. 2004;36:674–688. doi: 10.1249/01.mss.0000121945.36635.61. [DOI] [PubMed] [Google Scholar]
- 23.LaBella C. Patellofemoral pain syndrome: evaluation and treatment. Primary Care. 2004;31:977–1003. doi: 10.1016/j.pop.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 24.Lutz GE, Palmitier RA, An KN, Chao EY. Comparison of tibiofemoral joint forces during open-kinetic-chain and closed-kinetic-chain exercises. J Bone Joint Surg Am. 1993;75:732–739. doi: 10.2106/00004623-199305000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Matuszak ME, Fry AC, Weiss LW, Ireland TR, McKnight MM. Effect of rest interval length on repeated 1 repetition maximum back squats. J Strength Cond Res. 2003;17:634–637. doi: 10.1519/1533-4287(2003)017<0634:eorilo>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 26.McLaughlin TM, Dillman CJ, Lardner TJ. A kinematic model of performance in the parallel squat by champion powerlifers. Med Sci Sports Exerc. 1977;9:128–133. [PubMed] [Google Scholar]
- 27.Moisio KC, Sumner DR, Shott S, Hurwitz DE. Normalization of joint moments during gait: a comparison of two techniques. J Biomech. 2003;36:599–603. doi: 10.1016/s0021-9290(02)00433-5. [DOI] [PubMed] [Google Scholar]
- 28.Mulholland SJ, Wyss UP. Activities of daily living in non-Western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res. 2001;24:191–198. doi: 10.1097/00004356-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Neitzel JA, Davies GJ. The benefits and controversy of the parallel squat in strength training and rehabilitation. Strength Cond J. 2000;22:30–37. [Google Scholar]
- 30.Nisell R, Ekholm J. Joint load during the parallel squat in powerlifting and force analysis of in vivo bilateral quadriceps tendon rupture. Scand J Sports Sci. 1986;8:63–70. [Google Scholar]
- 31.O’Shea J. The parallel squat. Strength Cond J. 1985;7:4–6. [Google Scholar]
- 32.Palmitier RA, An KN, Scott SG, Chao EY. Kinetic chain exercise in knee rehabilitation. Sports Med. 1991;11:402–413. doi: 10.2165/00007256-199111060-00005. [DOI] [PubMed] [Google Scholar]
- 33.Reilly D, Martens M. Experimental analysis of the quadriceps muscle force and patello-femoral joint reaction force for various activities. Acta Orthop Scand. 1972;43:126–137. doi: 10.3109/17453677208991251. [DOI] [PubMed] [Google Scholar]
- 34.Robertson DG, Wilson JM, St Pierre TA. Lower extremity muscle functions during full squats. J Appl Biomech. 2008;24:333–339. doi: 10.1123/jab.24.4.333. [DOI] [PubMed] [Google Scholar]
- 35.Salem GJ, Powers CM. Patellofemoral joint kinetics during squatting in collegiate women athletes. Clin Biomech. 2001;16:424–430. doi: 10.1016/s0268-0033(01)00017-1. [DOI] [PubMed] [Google Scholar]
- 36.Salem GJ, Salinas R, Harding FV. Bilateral kinematic and kinetic analysis of the squat exercise after anterior cruciate ligament reconstruction. Arch Phys Med Rehab. 2003;84:1211–1216. doi: 10.1016/s0003-9993(03)00034-0. [DOI] [PubMed] [Google Scholar]
- 37.Scanlan SF, Chaudhari AMW, Dyrby CO, Andriacchi TP. Differences in tibial rotation during walking in ACL reconstructed and healthy contralateral knees. J Biomech. 2010;43:1817–1822. doi: 10.1016/j.jbiomech.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wallace DA, Salem GJ, Salinas R, Powers CM. Patellofemoral joint kinetics while squatting with and without an external load. J Orthop Sports Phys Ther. 2002;32:141–148. doi: 10.2519/jospt.2002.32.4.141. [DOI] [PubMed] [Google Scholar]
- 39.Wilk KE, Escamilla RF, Fleisig GS, Barrentine SW, Andrews JR, Boyd ML. A comparison of tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am J Sport Med. 1996;24:518–527. doi: 10.1177/036354659602400418. [DOI] [PubMed] [Google Scholar]
- 40.Woltring HJ. Smoothing and differentiation techniques applied to 3-D data. In: Allard P, Stokes IAF, Blanchi JP, editors. Three-Dimensional Analysis of Human Movement. Champaign; Human Kinetics: 1995. pp. 79–99. [Google Scholar]
- 41.Wretenberg P, Feng Y, Arborelius UP. High- and low-bar squatting techniques during weight-training. Med Sci Sports Exerc. 1996;28:218–224. doi: 10.1097/00005768-199602000-00010. [DOI] [PubMed] [Google Scholar]
- 42.Zelle J, Barink M, De Waal Malefijt M, Verdonschot N. Thigh-calf contact: does it affect the loading of the knee in the high-flexion range? J Biomech. 2009;42:587–593. doi: 10.1016/j.jbiomech.2008.12.015. [DOI] [PubMed] [Google Scholar]