Abstract
Objective: It is necessary for both clinicians and researchers who study attention-deficit/hyperactivity disorder (ADHD) to obtain a medication history for patients/participants for a variety of purposes. Because of the complexity of constructing medication histories using official records, parental report of medication for children with ADHD is the most commonly used source of information. However, the reliability and validity of parent reports of medication history have not been thoroughly studied. Previous studies have only examined the psychometrics of interview assessments of medication use for a maximum of a 12 month recall period. The current study compares parent report provided by a questionnaire and physician records for children and adolescents with ADHD. This is the first study to examine validity of retrospective recall for an extended medication history (prekindergarten-12th grade) using a questionnaire, and the first to examine validity of parental report of dosage.
Methods: Participants with ADHD were part of the Pittsburgh ADHD Longitudinal Study. The current study utilized data from those in the ADHD group who had at least 1 year of data from the physician's records and corresponding records from the parent (n=178).
Results: Percent agreement for medication use was >80%. Intraclass correlation coefficients for parent–provider agreement on total daily dosage of ADHD medications were in the good to excellent range. There were no significant predictors of agreement.
Conclusions: Our findings indicate that it is acceptable for clinics and research studies to obtain information about medication use for children with ADHD retrospectively solely based on parental report.
Introduction
Establishing the psychometric properties of parental report of medication use for children with attention-deficit/hyperactivity disorder (ADHD) is useful for studies of treatment and utilization, longitudinal studies, and clinical trials with long-term follow-up (e.g., Jensen et al. 2004; Lahey et al. 2004; Merikangas et al. 2011). In addition, clinicians and physicians routinely obtain a history of medication use as part of the initial intake or office visit. Obtaining a history of physician records is a significant challenge for healthcare professionals in both clinical and research settings, because it involves contacting the patient's previous healthcare professionals, all of whom may differ in their record-keeping abilities. With limited time allotted for unreimbursable activities, and the diversity of record-keeping strategies, it may be challenging for service providers to compile and provide records for a medication history (Tang et al. 1994). This is particularly true when the history of medication use over the course of a patient's lifetime is desired. Furthermore, obtaining a medication history relating to mental health disorders is complex, because multiple and various types of service providers may have been involved. Therefore, the most common method of attaining medication histories in both research and clinical practice for children with ADHD is parental report. However, to our knowledge, the validity of these reports over an extended (>12 months) historical period has not been tested. Previous studies have examined the reliability and validity of interview assessments of medication, but none have examined a parent-report questionnaire format (Horwitz et al. 2001; Eaton Hoagwood et al. 2004; Mendenhall et al. 2010). The purpose of the current study is to examine the psychometric acceptability of a parental questionnaire for obtaining retrospective information about their child's ADHD medications.
Studies that have examined the psychometric properties of mental health services utilization measures have primarily focused on interview measures and reliability studies. Three studies examining the test–retest reliability of parental reports of psychotropic medication history have been conducted. These studies show that over 1–2 weeks, parents are able to reliably report the types of services used and the frequency of utilization for a variety of mental health services, including medication use. More specifically, two studies examining test–retest reliability of children's medication use demonstrated that for both lifetime and 12 month histories, parents can report with excellent reliability whether or not their child used medication (Horwitz et al. 2001; Hoagwood et al. 2004). Another study found excellent agreement for parent reports of medication use during a semistructured interview and chart records created from parent reports collected at an earlier date (Mendenhall et al. 2010). Parents were even able to recall some details reliably, such as dosage of medication for the past month and the number of times per day medication was taken (Horwitz et al. 2001; Eaton Hoagwood et al. 2004). Parent and provider reports, however, did not satisfactorily agree for the number of days that medication was actually taken in the past month and other items more specific to the dosing schedule, which is important for evaluating the efficacy of ADHD medications across settings (Horwitz et al. 2001). Although these studies reported that parents are reliable in their own reporting of medication use, these studies do not provide information on the validity of the report. The validity, or accuracy, of parental report is critical, as physicians tend to rely on parental report of medication history for treatment decisions. Relatedly, in research, parental report is often the only practical method for collecting information about medication history (Copeland et al. 1987).
Only two studies have been able to examine validity by directly comparing parental report and service provider report of medication use. Hoagwood and colleagues (2000) interviewed primary caregivers using the Services Assessment for Children and Adolescent (SACA) interview to obtain information about whether there was any medication use over the past 12 months, and compared it to chart and school records. Bussing and colleagues (2003) obtained parental report using the Child and Adolescent Services Assessment (CASA) interview and compared it with mental health and medical records from providers specified by the participant over a 12 month recall period. Bussing and colleagues (2003) found excellent agreement, whereas Hoagwood and colleagues (2000) found moderate agreement for parental reports of any medication use in the past 12 months. The comparison between parent report of whether or not the child had utilized psychotropic medication, and service provider records, demonstrated little variability, in that the 95% confidence intervals for the κ values ranged from good to excellent in one study, and remained in the excellent range in the other study (Hoagwood et al. 2000; Bussing et al. 2003). Even with this restricted range, there were some variables that correlated with higher and lower levels of agreement. Out of the 27 variables tested by Hoagwood and colleagues (2000), they found that better agreement was associated with female gender for the child and African American ethnicity for the parent; disagreement was associated with Caucasian ethnicity, small household, and stronger impact of the child's illness on the family. Bussing and colleagues (2003) found the same relationships with child gender and parental ethnicity as the previous study, and found an additional effect for socioeconomic status, with lower socioeconomic status relating to lower agreement. The results from these studies demonstrate that family-related stressors, ethnicity, and child gender are associated with agreement. Although these studies examine variables correlated with agreement, they do not examine predictors of agreement. Additionally, the two studies mentioned did not examine factors relating to medication use, such as the age at which the child started medication and the number of medications currently utilized, which may also influence the quality of parent–provider agreement.
Of additional interest is whether parents are able to validly report the details of medication history, such as type of medication, dosage, and specific time period of use. However, the validity of parental recall of the details such as dosage, or duration, has not been widely examined. The one exception was Bussing and colleagues (2003), who reported that parents were able to validly report the name of the medication taken within the past 3 months. No study to date has examined whether parents can recall more specific information about the history of psychotropic medication use, even though this type of information is routinely sought during healthcare appointments and for research purposes. Acquiring information about dosage is particularly important, because the distinct stimulant medications do not typically produce different effects as much as a change in dose would (Pliszka and AACAP Work Group on Quality Issues 2007).
Establishing validity for parental reports of medication use for recall periods >12 months is particularly relevant for ADHD, as it is possible for medication use to begin at a young age and continue for years. The most common age range during which children with ADHD initiate medication use is elementary school (Zuvekas and Vitiello 2012). Although there is an absence of studies that characterize long-term medication use for ADHD youth, the literature that is currently available suggests that medication use is variable and discontinuous throughout childhood (Bussing et al. 2005; Marcus et al. 2005; Molina et al. 2009; Stein et al. 2012). Medication status can vary from year to year based on the demands of the child's current classroom, the perceived effectiveness of the medication, availability of treatments, health insurance, the child's tolerability to the medication, and other factors. Consequently, one common challenge across all measures is the challenge of asking parents about discrete episodes of care (Eaton Hoagwood et al. 2004). Determining start and stop points for medication use is particularly important for ADHD, because of the probable variability in service use and the immediate effect of medication onset and symptom relief, and, contrastingly, medication stoppage and symptom exacerbation. The existing instruments instruct interviewers to ask about medication use during a specific recall period, (e.g. since the last visit, or the past 3 months). An additional way of asking about discrete episodes of care for children may be to ask about utilization by school grade. This may be practical for longer recall periods and particularly suited for children with ADHD, because their treatment needs are typically related to school behavior and performance.
The existing parental report instruments of medication history are interviews that require training with corresponding manuals. The time to administer these instruments varies from 2 to 45 minutes based on the number of affirmative responses parents provide to initial questions (Horwitz et al. 2001; Bussing et al. 2003; Jensen et al. 2004; Mendenhall et al. 2010). In many cases, where time and resources are limited, it may be desirable to have a tool for collecting this type of information without the need for an individual administrator. Unfortunately, reliability and validity of self-report paper and pencil questionnaires for child medication utilization has not yet been tested.
Among the existing studies comparing parent and provider reports of medication use, none have examined questionnaires or retrospective parental report beyond 12 months. The current study uses physician records and parental report of medication use from the participants with ADHD from the Pittsburgh ADHD Longitudinal Study (PALS) from prekindergarten age to twelfth grade. Agreement between parent and provider records was calculated for medication use and dosage. In addition, predictors of agreement are examined.
Methods
Participants
The ADHD group was recruited from a pool of 516 study-eligible participants diagnosed with American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. Revised (DSM-III-R) or American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV) (American Psychiatric Association 1987, 1994). ADHD in childhood and treated in the Summer Treatment Program (STP) at the Western Psychiatric Institute and Clinic (WPIC) in Pittsburgh, PA from 1987 to 1996. Of the 516, 493 were re-contacted an average of 8.35 years later (SD=2.79) to participate in annual interviews of the PALS. Of those contacted, 364 (70.5 %) enrolled in the PALS. At the first follow-up interview, the ADHD group ranged in age from 11 to 28 with 99% falling between 11 and 25 years of age. They were admitted to the follow-up study on a rolling basis between the years 1999–2003 and completed their first follow-up interview immediately upon enrollment. Further information about the sample can be found in Molina et al. (2007).
Current study
The current study utilized data from the PALS for those in the ADHD group who had at least 1 year of data from the physician's records and corresponding records from the parent (n=178). At study entry, 87 participants were currently taking psychotropic medication. At the time of study entry, 33% of our sample were already out of high school; 43% were currently in high school, 20% were in middle school, and 4% were in elementary school. The average age of the participants in the ADHD group at the first wave of the study was 16.86 years (range, 11–25).
Measures
Demographic information
The demographic questionnaire was developed for this study and was completed yearly by both parents and young adults. Participants were asked about their age, ethnicity, income, and household composition.
Impairment
Parent report of impairment was obtained by the Impairment Rating Scale (IRS) (Fabiano et al. 2006). The IRS asks the rater to assess the severity of a child's problems in functioning and the need for treatment and special services. In this report, one item asking about overall impairment was used. Ratings for each item range from 0 to 6. Higher scores indicate greater impairment.
Medication history
During the first follow-up, parents were asked to complete the Medication and Treatment Chronology questionnaire (Pelham et al. unpublished measure), which asks parents to provide as much information as possible about whether or not their child was medicated in each grade, and details such as the name of the medication and dosage. These reports were supplemented by adolescent self-report, and incomplete information was queried by the interviewer. When discrepant information was obtained between parent and youth, parent reports were used as the final indicator. Parents provided information for 1–13 grades (mean=10.91, SD=2.54). For 23% of the sample, the entire medication history reported was retrospective information. Eighty-eight percent of the sample also reported information for the grade they were currently attending, and, therefore, a small portion of their medication history was a current report. All medication names were coded into the following categories: 1) ADHD medication (any of the methylphenidate and amphetamine derivatives) or 2) non-ADHD medication (e.g., antidepressants, antipsychotics). In order to standardize doses for the different types of ADHD medications, all doses were converted into the immediate-release methylphenidate formulation, using guidelines from previously published work, before calculating reliability (long-acting methylphenidate formulations [Pelham et al. 2001]; mixed amphetamine salts [Pelham et al. 1999]; extended release mixed amphetamine salts [Pliszka and AACAP Work Group on Quality Issues 2007]; pemoline, dextroamphetamine, and sustained release methylphenidate [Pelham et al. 1990]). When more than one dose was reported for the grade, the doses were averaged.
Physician records
Physician records were obtained starting with the second follow-up of the PALS study only when parents indicated any previous or current medication for the child. The participants' prescribing doctors were contacted by a research assistant and asked to provide copies of all past medical records for the subjects. A total of 228 physicians were contacted, and 90% responded by faxing the records. A total of 178 records had medication reports for grades prekindergarten through 12. Records were coded and entered to fit the format of the medication history questionnaire by a research assistant. The physician reports that were collected represented, on average, 30% of the participant's school years (prekindergarten to grade 12).
Data analysis
Percent agreement was calculated to determine the concordance between the physician's records and parental report. Agreement for medication use was defined as a match between parents and physicians (e.g., yes/yes and no/no) for each grade in which a parent and physician report existed. Paired t tests were used to determine if the mean difference between the physician and parental reports for total daily dose of ADHD medication were significantly different from chance. Intraclass correlations for absolute agreement were then calculated for average total daily ADHD medication dosage for each grade. Following previous research, κ values >0.75 represented excellent agreement, values between 0.40 and 0.75 represented good agreement, and values <0.40 represented poor agreement (Bussing et al. 2003). Finally, logistic regression was used to determine predictors of medication use agreement. For the logistic regression, the outcome variable represented the percentage of grade reports for which the parent and physician matched on their response to the use of medication for that grade.
Results
Medication use
Over the entire assessment period, parent and physician reports indicated that children typically took an average of only one medication per grade. Agreement for whether or not the subject was currently medicated was >80% for each category of medication use (any use, ADHD medication, and non-ADHD medication). Agreement for whether or not the subject had taken medication during a specific grade was >80% for all categories (any use range, 80–96), (non-ADHD medication range, 82–96), (ADHD medication range, 80–93). The sample size ranged from 11 to 76 depending upon the grade, with the lowest sample size for prekindergarten.
For each parent-reported history, we calculated the total number of grades for which the parent and physician agreed. On average, physician and parental report of whether or not a child was taking any medication for each grade (prekindergarten to 12) agreed for 85% (range, 0–100%) of the grades for which we had both reports.
Predictors of agreement
As mentioned, the variable for average parent–provider agreement for the use of medication over the entire history was highly skewed with an average of 85% reports in agreement across the entire history and 73% of all histories in perfect agreement. Therefore, the variable was re-coded from a continuous variable into a dichotomous variable (0=<100% and 1=100%). A logistic regression was conducted with household income, number of children in the household, overall impairment, the age at which the subject was first medicated, the length of the follow-up interval, and the number of current medications as predictors of parent–physician agreement. The omnibus model was not significant, χ2 (6)=6.88, p=0.33.
Dosage
Table 1 displays the average total daily doses of ADHD medication reported for each grade along with the mean differences. The mean differences for each grade between parent-reported and physician-reported dose was not significantly different from chance.
Table 1.
Mean Differences Between Physician and Parent Reports of Total Daily Dosage of Attention-Deficit/Hyperactivity Disorder (ADHD) Medications
| Pairs | Mean | Standard deviation | t | df | Sig | r |
|---|---|---|---|---|---|---|
| Grade 1 | ||||||
| Physician | 23.18 | 12.15 | ||||
| Parent | 21.69 | 12.67 | 0.55 | 26 | 0.59 | 0.11 |
| Grade 2 | ||||||
| Physician | 22.13 | 12.23 | ||||
| Parent | 24.30 | 13.80 | −0.96 | 37 | 0.34 | 0.16 |
| Grade 3 | ||||||
| Physician | 26.92 | 15.22 | ||||
| Parent | 29.35 | 19.42 | −0.84 | 44 | 0.41 | 0.13 |
| Grade 4 | ||||||
| Physician | 28.99 | 16.41 | ||||
| Parent | 26.15 | 14.74 | 1.33 | 40 | 0.19 | 0.21 |
| Grade 5 | ||||||
| Physician | 30.10 | 16.31 | ||||
| Parent | 26.49 | 11.93 | 1.69 | 41 | 0.10 | 0.26 |
| Grade 6 | ||||||
| Physician | 33.58 | 22.47 | ||||
| Parent | 29.64 | 13.49 | 1.49 | 43 | 0.15 | 0.22 |
| Grade 7 | ||||||
| Physician | 35.97 | 22.86 | ||||
| Parent | 33.93 | 20.73 | 0.81 | 42 | 0.42 | 0.12 |
| Grade 8 | ||||||
| Physician | 38.98 | 18.93 | ||||
| Parent | 34.09 | 18.41 | 1.52 | 41 | 0.14 | 0.23 |
| Grade 9 | ||||||
| Physician | 37.92 | 16.12 | ||||
| Parent | 37.33 | 21.32 | 0.19 | 40 | 0.85 | 0.03 |
| Grade 10 | ||||||
| Physician | 36.60 | 16.45 | ||||
| Parent | 34.42 | 21.40 | 0.58 | 28 | 0.57 | 0.11 |
| Grade 11 | ||||||
| Physician | 45.80 | 37.83 | ||||
| Parent | 40.14 | 37.21 | 1.77 | 22 | 0.09 | 0.35 |
r=0.10, small effect; r=0.30, medium effect; r=0.50, large effect. Pre-kindergarten, kindergarten, and Grade 12 results were not included because of the small sample size. Doses of ADHD medications were standardized for an immediate-release methylphenidate formula.
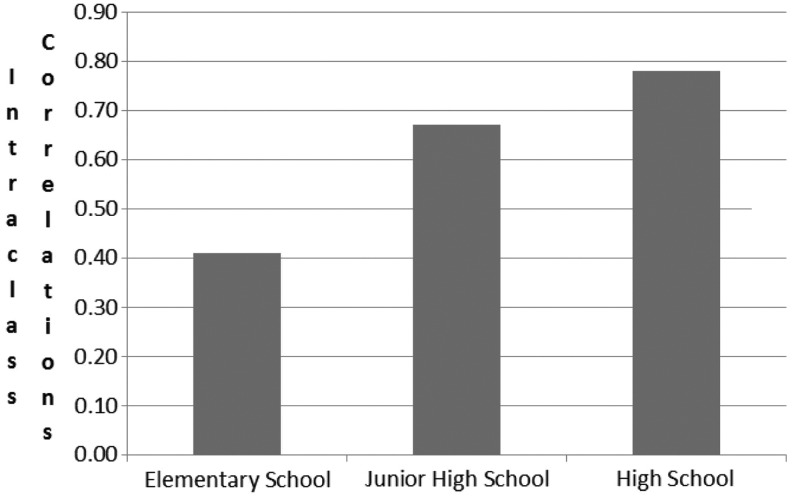
Figure 1 displays the intraclass correlation coefficients for total daily dosage of ADHD medications. Parents and physicians had good to excellent agreement for reports in elementary, junior high, and high school.
FIG. 1.
Intraclass correlations for total daily doses of attention-deficit-hyperactivity disorder (ADHD) medications indicated by physician and parent report.
Discussion
The current study evaluated the validity of parental retrospective report from a questionnaire for obtaining medication histories covering prekindergarten to 12th grade for individuals with ADHD. We utilized physician records and parent reports to examine agreement for medication use, and found that agreement on whether or not the subject was taking medication was >80% for each grade reported. In addition, parent and provider reports of total daily dosage for ADHD medications in each school period were in the good to excellent range. Furthermore, to our knowledge, this is the first study to report on the validity of parental report (vs. physician records) using a questionnaire method for an extended medication history, and the first study to report on the validity of ADHD medication dosage report from the parent (vs. physician records). Our findings indicate that it is acceptable for clinics and research studies to obtain information about medication use for children and adolescents with ADHD retrospectively solely based on parental report.
Our results demonstrate that parents are valid reporters of use even when at least 50% of the information reported is retrospective; for some of the oldest participants, recall periods extended ∼20 years back. When examining agreement for whether or not the subject took medication, we found that ∼75% of parent medication histories matched exactly with the medication histories based on the physician records. Our results, which examined a questionnaire instrument for a recall period beyond 12 months, extend the previous studies, which have reported excellent parent and provider concordance for medication use for recall periods up to 12 months, using interview assessments (Hoagwood et al. 2000).
Parents were even able to validly report the mean total daily dosage of ADHD medications compared with physician records. The mean differences for each grade of total daily dosage of ADHD medication were not significantly difference from chance. This indicates that parents and physicians agreed on their report of dose for the ADHD medications for each grade reported. The intraclass correlation, which is a more stringent measure of agreement than a paired t test, showed that for each school period (elementary, junior high, and high school) agreement was good to excellent. These findings suggest that clinics and research studies can use questionnaire measures for obtaining details beyond the general question of use, when physician records are not readily accessible. This finding is particularly useful considering that self-report data regarding health services utilization are commonly collected, and have the advantage of being more efficient and less costly than chart reviews (DiMatteo et al. 2003).
Previous studies found that ethnicity, subject gender, household size, and impact of illness predicted parent–provider agreement (Hoagwood et al. 2000; Bussing et al. 2003). The current study did not find any statistically significant predictors of parent–provider agreement for medication use. Our findings are in line with epidemiologic studies that examined long-term recall periods and did not find personal factors to be consistent predictors of recall ability (Friedenreich 1994).
Limitations
The results of the current study should be considered in the context of its limitations. One potential limitation is the generalizability of the sample. The PALS sample included subjects who participated in a therapeutic summer camp, and may differ from a non-clinic population of youth with ADHD. However, it is likely that the PALS sample is representative of the broader population of treatment-seeking families of children with ADHD. Another potential limitation is that compared with individuals who not participating in research, the individuals in this sample may be more aware of their medication because they knew they would be asked about their medication status at the yearly follow-up visits. However, the majority of the data from the current study were collected retrospectively from the 1st and 2nd year visits, reducing the possibility that study participation affected their reporting.
Conclusions
The information garnered from the questionnaire measure in the current study was found to be as psychometrically acceptable as other interview assessments for obtaining information about medication history. The high levels of agreement that we found, even for such an extended recall period, may have been a result of the structure of our questionnaire, as it asks about medication use by grade. Considering that parents often take into account teacher and school recommendations for ADHD treatment, asking about medication status by grade may lead the parent to construct a salient personal timeline, which has shown to be a helpful tool in reducing recall bias, and has been used in some interview assessments (Friedenreich 1994; Shaffer et al. 2000). Future studies on child treatment utilization should consider using a questionnaire such as ours (Medication and Treatment Chronology; Pelham et al. unpublished measure), as it is likely that referring to an episode of care by school grade aids in recall.
Clinical Significance
Clinicians often rely on parental report when obtaining a treatment history from patients. The results of the current study show that parental self-report of a child's medication history using a questionnaire is a psychometrically acceptable method for collecting information about medication history over an extended recall period. A parent-completed questionnaire to obtain medication history requires few professional/clerical resources, compared with a search of medical records, and involves less parental time and staff resources than an interview format.
Disclosures
Dr. Pelham has been a past consultant, scientific advisor, speaker and/or grant recipient for the following: Abbott, Celphalon, Lilly, McNeil/Alza/Janssen, Noven, and Shire. He is a current consultant for Noven. Dr. Molina, Dr. Sibley, Dr. Waschbusch, Mrs. Kuriyan, and Ms. Gnagy have no conflicts of interest or financial ties to report.
References
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. Revised. Washington, DC: American Psychiatric Association; 1987 [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- Bussing R, Mason DM, Leon CE, Sinha K: Agreement between CASA parent reports and provider records of children's ADHD services. J Behav Health Serv Res 30:462–469, 2003 [DOI] [PubMed] [Google Scholar]
- Bussing R, Zima BT, Mason D, Hou W, Garvan CW, Forness S: Use and persistence of pharmacotherapy for elementary school students with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 15:78–87, 2005 [DOI] [PubMed] [Google Scholar]
- Copeland L, Wolraich M, Lindgren S, Milich R, Woolson R: Pediatricians' reported practices in the assessment and treatment of attention deficit disorders. J Dev Behav Pediatr 8:191–197, 1987 [PubMed] [Google Scholar]
- DiMatteo MR, Robinson JD, Heritage J, Tabbarah M, Tabbarah M, Fox SA: Correspondence among patients' self-reports, chart records, and audio/videotapes of medical visits. Health Commun 15:393–413, 2003 [DOI] [PubMed] [Google Scholar]
- Eaton Hoagwood K, Jensen PS, Arnold LE, Roper M, Severe J, Odbert C, Molina BS: Reliability of the services for children and adolescents–parent interview. J Am Acad Child Adolesc Psychiatry 43:1345–1354, 2004 [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Pelham J, William E, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, Onyango AN, Kipp H, Lopez–Williams A, Burrows–MacLean L: A practical measure of impairment: Psychometric properties of the impairment rating scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. J Clin Child Adolesc Psychol 35:369–385, 2006 [DOI] [PubMed] [Google Scholar]
- Friedenreich CM: Improving longterm recall in epidemiologic studies. Epidemiology 5:1–3, 1994 [PubMed] [Google Scholar]
- Hoagwood K, Horwitz S, Stiffman A, Weisz J, Bean D, Rae D, Compton W, Cottler L, Bickman L, Leaf P: Concordance between parent reports of children's mental health services and service records: the Services Assessment for Children and Adolescents (SACA). J Child Fam Stud 9:315–331, 2000 [Google Scholar]
- Horwitz SM, Hoagwood K, Stiffman AR, Summerfeld T, Weisz JR, Costello EJ, Rost K, Bean DL, Cottler L, Leaf PJ: Reliability of the services assessment for children and adolescents. Psychiatr Serv 52:1088–1094, 2001 [DOI] [PubMed] [Google Scholar]
- Jensen PS, Eaton Hoagwood K, Roper M, Arnold LE, Odbert C, Crowe M, Molina BS, Hechtman L, Hinshaw SP, Hoza B: The services for children and adolescents–parent interview: Development and performance characteristics. J Am Acad Child Adolesc Psychiatry 43:1334–1344, 2004 [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Kipp H, Ehrhardt A, Lee SS, Willcutt EG, Hartung CM, Chronis A, Massetti G: Three-year predictive validity of DSM-IV attention deficit hyperactivity disorder in children diagnosed at 4–6 years of age. Am J Psychiatry 161:2014–2020, 2004 [DOI] [PubMed] [Google Scholar]
- Marcus SC, Wan GJ, Kemner JE, Olfson M.: Continuity of methylphenidate treatment for attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med 159:572, 2005 [DOI] [PubMed] [Google Scholar]
- Mendenhall AN, Davidson KH, Fristad MA: The service provider and medication usage grids: A new method to measure “Treatment as Usual”(TAU). Child Adolesc Social Work J 27: 423–434, 2010 [Google Scholar]
- Merikangas KR, He J, Burstein M, Swendsen J, Avenevoli S, Case B, Georgiades K, Heaton L, Swanson S, Olfson M: Service utilization for lifetime mental disorders in US adolescents: Results of the National Comorbidity Survey–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 50:32–45, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, Epstein JN, Hoza B, Hechtman L, Abikoff HB.: The MTA at 8 years: Prospective follow-up of children treated for combined type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry 48: 484, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BS, Pelham WE, Gnagy EM, Thompson AL, Marshal MP: Attention‐deficit/hyperactivity disorder risk for heavy drinking and alcohol use disorder is age specific. Alcohol Clin Exp Res 31:643–654, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelham WE, Aronoff HR, Midlam JK, Shapiro CJ, Gnagy EM, Chronis AM, Onyango AN, Forehand G, Nguyen A, Waxmonsky J: A comparison of Ritalin and Adderall: Efficacy and time-course in children with attention-deficit/hyperactivity disorder. Pediatrics 103:e43–e43, 1999 [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Burrows–Maclean L, Williams A, Fabiano GA, Morrisey SM, Chronis AM, Forehand GL, Nguyen CA, Hoffman MT: Once-a-day Concerta methylphenidate versus three-times-daily methylphenidate in laboratory and natural settings. Pediatrics 107: e105–e105, 2001 [DOI] [PubMed] [Google Scholar]
- Pelham WE, Greenslade KE, Vodde–Hamilton M, Murphy DA, Greenstein JJ, Gnagy EM, Guthrie KJ, Hoover MD, Dahl RE: Relative efficacy of long-acting stimulants on children with attention deficit-hyperactivity disorder: A comparison of standard methylphenidate, sustained-release methylphenidate, sustained-release dextroamphetamine, and pemoline. Pediatrics 86:226–237, 1990 [PubMed] [Google Scholar]
- Pliszka S, AACAP Work Group on Quality Issues: Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 46:894–921, 2007 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab–Stone ME: NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry 39:28–38, 2000 [DOI] [PubMed] [Google Scholar]
- Stein BD, Klein GR, Greenhouse JB, Kogan JN: Treatment of attention-deficit hyperactivity disorder. Psychiatr Serv 63:122–129, 2012 [DOI] [PubMed] [Google Scholar]
- Tang PC, Fafchamps D, Shortliffe EH: Traditional medical records as a source of clinical data in the outpatient setting. In: Proceedings of the Annual Symposium on Computer Application in Medical Care. Philadelphia: American Medical Informatics Association, 575, 1994 [PMC free article] [PubMed] [Google Scholar]
- Zuvekas SH, Vitiello B: Stimulant medication use among US children: A twelve-year perspective. Am J Psychiatry 169:160, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]