Abstract
Objective
To determine the status of serum zinc in pregnant women in different gestational ages and correlation with socio-demographic and anthropometric factors in Iranian women referring to prenatal care public health clinics.
Materials and methods
We analyzed the zinc concentrations in plasma samples obtained at different gestational ages from 961 women and recorded BMI at the first trimester in pregnant women who were screened for a trial designed to evaluate the zinc concentration. Subjects were from different socio economical backgrounds and attended public health clinics for their prenatal care. All analyses were performed by SPSS (version 16). P values < 0.05 were considered significant.
Results
The results showed that after plasma zinc concentrations were adjusted with Parity, weight (early pregnancy), BMI (at early pregnancy), age and educational statues. Plasma zinc deficiency declined as gestational age progressed, however it was not significant. There was no significant correlation between zinc concentration, anthropometric, method of contraception and socio factors. However, there were significant relation between parity (p = 0.007) and weight at early pregnancy (p= 0.039) with serum zinc levels.
Conclusion
We conclude that plasma zinc concentrations decreased during the late first trimester to the early third trimester and with parity. These findings may indicate that the deficient levels of zinc in the latter third of pregnancy suggest a tendency for insufficient maternal nutrition. However larger studies are required to support this finding.
Keywords: Anthropometry, Parity, Socio-Demographic Factors, Zinc
Introduction
It has long been known that zinc is an important trace element which has a major role in a number of biochemical reactions and systems in human body. It is necessary for the functioning of more than 300 different enzymes and plays a vital role in an enormous number of biological processes. The effects of zinc on maternal health and pregnancy outcomes have been studied in multiple observational and interventional studies. Studies linked the zinc deficiency with a wide range of complications including pregnancy induced hypertension, hemorrhage, infections, intrauterine growth retardation, low birth weight, congenital anomalies and increased neonatal morbidity (1).
The importance of zinc in pregnancy is due to its role in DNA and protein synthesis and as a result thenecessity of its availability for the appropriate growth and development of the fetus and neonate (2). Zinc deficiency, in addition to reducing cell proliferation, protein synthesis, or rate of tubule polymerization, decreases growth in embryonic and fetal periods (3).
Zinc nutriure of pregnant women has been assessed by measuring maternal zinc concentrations in plasma or serum, leukocytes, erythrocytes, and amniotic fluid as well as by other indexes including dietary zinc intake (4–10). Pregnant women are facing zinc deficiency more than the other groups, due to having fetus which need zinc for its proper growth (11). Higher age, lactation, alcoholism, and high consumption of iron, and folic acid, increase the risk of zinc deficiency (11, 12). Other researches have shown that the fetus grown by zinc deficiency is end up with abnormalities in central nervous systems (13, 14). In another study done on the zinc deficient pregnant women, it was indicated that congenital abnormalities, prolonged pregnancy, abnormal tasting sense, and other difficulties were seen in such subjects (14). Evidences suggest that zinc deficiency is one of the important problems within the developed and developing countries (15). Zinc deficiency in human was reported for the first time in 1961 (16). In 1991, a report was published which emphasized the importance of zinc and also indicated that in countries such as Iran, Egypt, Turkey, China, Yugoslavia, and Canada, due to low consumption of red meat, and high consumption of fiber, zinc deficiency was seen quiet often. A separate study in 2001 indicated that using supplementary zinc materials by pregnant mother, increased newborn birth weight, and decreased the mortality rate (17). The aim of this study was to investigate the relations between plasma zinc concentrations, socio-demographic and anthropometric factors during pregnancy.
Materials and methods
This research was an analytical- descriptive study, which was conducted on 961 pregnant, between January 2009 and December 2011. Subjects were mostly from low socioeconomic backgrounds and attended public health clinics for their prenatal care. For each participant a questionnaire was provided which contained the following items: mother age, weigh (at the first trimester), height, gestational age, number of deliveries, last method of contraception, occupation and educational statues. Written informed consent was obtained from all subjects. The participants had no history of systemic, cardiovascular, proliferative, or endocrine diseases, neoplasm, and anemia. They did not smoke or consume alcohol and were not addicted to illicit drugs. Also, they did not use any medications except for acid folic (1 mg) and Ferrous sulfate (50 mg elemental iron) since the beginning of the second trimester.
In this study, gestational age was calculated at the beginning of the study based on the first day of last menstrual period and height of fundus. If a woman did not remember the first day of her last menstrual period or her height of fundus differed with her gestational age for more than two weeks, ultrasound was employed to accurately determine the gestational age (less than 20 weeks).
The blood was collected and allowed to clot for 20 minutes and consecutively centrifuged at 3000 × g for 10 min. We analyzed the zinc concentrations in plasma samples obtained at different gestational age. We divided mothers according to age to different groups, (≤19 years), (20-24 years), (25-29 years), (30-34 years) and (≥35 years). The trial was reviewed and approved by Ethical Committee of Reproductive Health Research Center, Imam Hospital in Tehran, Iran, and each subject or guardian provided signed, informed consent. We also divided mothers according to number of deliveries to three groups, nullipara, primipara and multipara.
Body composition analyzer
Height was measured in the upright position with stadiometer. Weight, BMI measured with body composition analyzer (Inbody 3.0, Biospace Co, Ltd. KOREA) at the first trimester.
Zinc concentration assay
Serum Zinc levels were estimated using kit supplied following established literature procedures by Randox, Co kit, UK. The principle of this kit is when the Zinc present in the sample is chelated by 5-Br-PAPS-2-(5-bromo-2-pyridylazo)-5-(N-propyl-N-sulfopropylamino) -phenol in the regent. The formation of this complex is measured at a wavelength of 550 nm spectrophotometer, Cecil, CE, 2501 model, 2000, series (18, 19 20).
Sample size
Sample size adequate for estimating the prevalence of ZD was computed using single proportion sample size calculation formula with the inputs of 95% confidence level, 5% of margin of error, design effect of 2, non-response rate of 10% and expected prevalence of ZD of 72% (20). Accordingly, sample size of n= 920 was computed. However, in order to maximize the sample size for the analytic study component, n= 750 pregnant women were included in the study. The adequacy of the sample size for investigating the key determinants of ZD (parity, maternal age, and gestational age) was assessed via double proportion sample size calculation formula using an online application (21).
Data analysis
Data entry, screening and analysis were carried out by using SPSS 17.0. Descriptive analysis was done using mean, frequency and percentage. Independent t-test, bivariate correlations and one-way Analysis of Variance (ANOVA) used to compare serum zinc levels across categories of independent variables. The association between a determining factor was considered to be significant at p <0.0.
Results
As Table 1 shows, the age, primiparous, weight, height, body mass index at the gestational age on routine pregnancy. Moreover, all groups did not differ significantly by gestational age screening of pregnancy.
Table 1.
Characteristics of subjects by gestational age at screening (mean± SD)
| ≤ 11 wk n = 235 | 12-19 wk n = 301 | ≥20 wk n = 425 | p value | |
|---|---|---|---|---|
| Age (year) (mean± SD)* | 26.22± 4.46 | 26.59± 4.43 | 26.46± 4.80 | Non-significant |
| primiparous (%)** | 24.7 | 27.6 | 29.4 | Non-significant |
| Serum zinc (µg/dl) (mean± SD) * | 91.02± 25.99 | 88.62± 27.06 | 88.70± 25.08 | Non-significant |
| Zinc deficiency*** (%) ** | 16.2 | 16 | 17.3 | Non-significant |
One-way ANOVA test
χ2 test
<66 µgr/dl
The mean zinc level for gestational age of ≤11 wk, 12-19 wk and ≥20 wk were 91.02± 25.99,88.62± 27.06 and 88.70± 25.08 µg/dl respectively. The percentage of zinc deficiency level (<66 µgr/dl) for gestational age of ≤11 wk, 12-19 wk and ≥20 wk were 16.2%, 16 and 17.3 respectively. However there was not any relation between Zinc concentration and deficiency in different groups of gestational age.
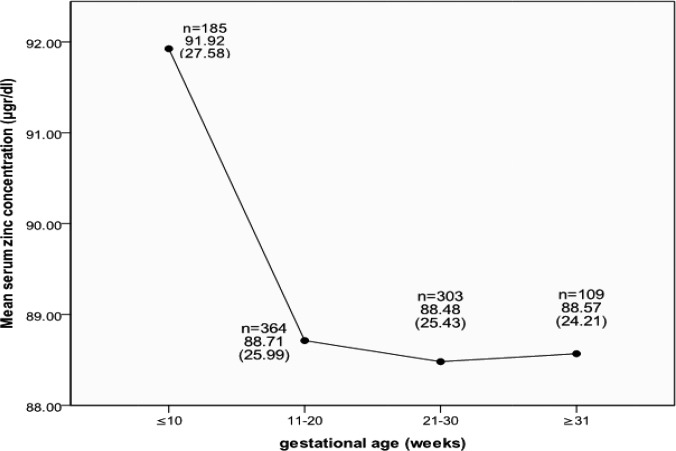
Figure 1 represents changes in mean serum zinc concentration level of all participants at gestational age of the study. As this figure shows, the mean zinc level for gestational age of ≤ 10 wk, 11-20 wk, 21-30 wk and ≥31 wk were 91.92± 27.58, 88.71± 25.99 and 88.48± 25.43 and 88.57± 24.21µg/dl respectively. Serum zinc decreased at 11-20 to ≥31 wks of pregnancy. However, no significant correlation was noted between serum zinc concentration and the gestational week.
Figure 1.
Changes in mean serum zinc concentration level of all participants at different gestational ages. Data are expressed as mean± SD
The prevalence of zinc concentration among the pregnant women was also studied according to the following items (Table 2): mother age divides to (≤19, 20-24, 25-29, 30-34 and ≥35 years), numbers of deliveries (0, 1 and ≥2). Results from this investigation indicated that there was no meaningful difference regarding Occupation (housekeeper and employed) and educational statues (≤5th grade, 6th -8th grade, 9th -12th grade and University). However, with number of parity the zinc concentration was decreased significantly (p< 0.05).
Table 2.
Characteristics of participants and comparison of serum zinc concentration of groups (mean± SD)
| Variable | n (%) (n = 961) | Serum zinc at screening (µg/dl) | p value | |
|---|---|---|---|---|
| Age (year)* | ≤19 | 42 (4.4) | 93.02 (27.93) | Non-significant |
| 20-24 | 317 (33.0) | 90.62 (27.63) | ||
| 25-29 | 360 (37.5) | 88.99 (24.88) | ||
| 30-34 | 192 (20.0) | 86.77 (24.53) | ||
| ≥35 | 50 (5.2) | 88.64 (25.73) | ||
| Body mass index (kg/m2)* at the first trimester | < 19.8 | 133 (13.8) | 90.51 (24.51) | Non-significant |
| 19.8-26 | 535 (55.7) | 89.99 (27.01) | ||
| 26.1-29.9 | 195 (20.3) | 86.83 (25.08) | ||
| ≥ 30 | 98 (10.2) | 88.22 (23.29) | ||
| Parity (n) | 0 | 612 (63.7) | 91.03 (26.14) | 0.022 |
| 1 | 266 (27.7) | 86.81 (26.58) | ||
| ≥2 | 83 (8.6) | 83.86 (20.58) | ||
| Occupation (%) ** | Housekeeper | 868 (90.3) | 89.44 (26.10) | Non-significant |
| Employed | 93 (9.7) | 86.97 (24.07) | ||
| Educational status ** | ≤ 5th grade | 95 (9.9%) | 88.92 (24.58) | Non-significant |
| 6th -8th grade | 139 (14.4%) | 84.83 (25.68) | ||
| 9th -12th grade | 586 (61.0%) | 90.33 (26.12) | ||
| University | 141(14.7%) | 89.87 (25.83) | ||
| Last method of contraception | Hormonal | 134 (13.9%) | 86.48 (24.12) | Non-significant |
| IUD | 50 (5.2%) | 84.98 (26.52) | ||
| Barrier | 94 (9.8%) | 87.73 (24.50) | ||
| Withdrawal | 489 (50.9%) | 89.61 (25.66) | ||
| Nothing or breast feeding | 194 (20.2%) | 92.84 (28.05) |
One-way ANOVA
T-test
The Table 3 indicated the Correlation between variable measurements and serum zinc z scores. The results showed there were significant relation (p < 0.05) between number of parity and weight of participants at the early of pregnancy and serum zinc z score.
Table 3.
Correlation between variable measurements and serum zinc z scores (mean± SD)
| Variable | Variable measurement | Coefficient between measure and serum zinc z score | p value |
|---|---|---|---|
| Age (year) | 26.44 (4.6) | −0.056 | Non-significant |
| Parity (n) | .47 (.71) | −0.084 | 0.007 |
| Weight (kg) | 62.64 (11.25) | −0.067 | 0.039 |
| Height (cm) | 160.81 (5.79) | −0.055 | Non-significant |
| Body mass index (kg/m2) at the first trimester | 24.22 (4.12) | −0.048 | Non-significant |
Significant level was set at P< 0.05.
Discussion
Pregnancy is associated with increased demand of all the nutrients like Iron, Zinc and antioxidant and deficiency of any of these could affect pregnancy (19). In spite of the fact that zinc deficiency is prevalent in pregnant women in Iran. The results of our study also revealed that with increase number of parity and weight at early of pregnancy of participants serum zinc decreased. This finding is consistent with other investigations (22, 23).
In developing countries, socioeconomic status is a complex term generally used for defining social inequalities and usually measured by income/educational level/occupation/living accommodation.
This is quite understandable as educational attainment has been established as a social variable that often displays the largest socioeconomic influence (24) because it affects both income and occupation. Educated women are also more likely to understand public-health message (25) and to maintain high personal hygiene than less-educated women. Educated women also belong to high social class and have access to adequate medicare and nutrition during pregnancy.
The prevalence of zinc deficiency in the different age of pregnancy showed meaningful difference, and that was due to mothers increasing requirement for zinc. Without a proper nutritional requirement the person falls in the state of zinc deficiency. In this study, the zinc level was determined according to the number of deliveries, and although we expected that with increasing the number of deliveries the prevalence of zinc deficiency worsen, however we founded significant (p < 0.05) difference with parity and zinc concentration. In this study zinc deficiency was not influenced by mothers’ education level. This finding was consistent with other investigations (26). However, it is premature to recommend a reinforcement of routine zinc supplementation for healthy mothers (27).
In this study there were reverse relation between maternal weight (in first trimester) and serum zinc concentration. Previous studies conducted by Gebremedhin et al, 2011 also supported the finding.
The outcome of the study suggests that low level of nutrient in mothers is associated with frequency of pregnancies especially if it is less than 24 months (28).
In many developing countries, these physiologic changes can be aggravated by under-nutrition, leading to micronutrient deficiency states that can have disastrous consequences for both mothers and newborn infants. Although a marginal zinc intake during pregnancy plays an important role in the duration of gestation and is associated with increased risk of preterm and very preterm delivery, scientists are still debating the healthy levels of zinc needed in pregnant women (28, 29).
We conclude that plasma zinc concentrations during the late first trimester to the early third trimester and with parity decreased. These findings indicate deficient level of zinc in the latter third of pregnancy which suggest a tendency for insufficient maternal nutrition. This might be due to the reason that nutritional care is not well integrated into maternity services. In addition, the provision of nutrition education might not be effective in the absence of concurrent livelihood promotion strategies. Although zinc intake during pregnancy plays an important role in mothers health, further studies with larger sample sizes are recommended to obtain more reliable results.
Ethical Considerations
Ethical issues including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc. have been completely observed by the authors.
Acknowledgement
The authors wish to thank Tehran University of Medical Sciences to support this grant (registration no: 2719), all colleagues at Vali-e-Asr Reproductive Health Research Center and authorities of all affiliated biomedical laboratories.
References
- 1.Shah D, Sachdev HP. Effect of gestational zinc deficiency on pregnancy outcomes: Summary of observation studies and zinc supplementation trials. Br J Nutr. 2001;85(Suppl 2):101–8. doi: 10.1079/bjn2000301. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Geneva: Trace elements in human nutrition and health [internet] Available from: http://whqlibdoc.who.int/publications/1996/9241561734_eng_fulltext.pdf. [Google Scholar]
- 3.Shah D, Sachdev HP, Cetin I, Berti C, Calabrese S. Role of micronutrients in the periconceptional period. Human Reproduction Update. 2010;16:80–95. doi: 10.1093/humupd/dmp025. [DOI] [PubMed] [Google Scholar]
- 4.Swanson CA, King JC. Zinc and pregnancy outcome. Am J Clin Nutr. 1987;46:763–71. doi: 10.1093/ajcn/46.5.763. [DOI] [PubMed] [Google Scholar]
- 5.Apgar J. Zinc and reproduction: an update. J Nutr Biochem. 1992;3:266–78. [Google Scholar]
- 6.Tamura T, Goldenberg RL. Zinc nutriture and pregnancy outcome. Nutr Res. 1996;16:139–81. [Google Scholar]
- 7.Meadows NJ, Ruse W, Smith MF, et al. Zinc and small babies. Lancet. 1981;2:1135–37. doi: 10.1016/s0140-6736(81)90587-0. [DOI] [PubMed] [Google Scholar]
- 8.Simmer K, Punchard NA, Murphy G, Thompson RPH. Prostaglandin production and zinc depletion in human pregnancy. Pediatr Res. 1985;19:697–700. doi: 10.1203/00006450-198507000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Tamura T, Weekes EW, Birch R, Franklin JC, Cosper P, Davis RO, et al. Relationship between amniotic fluid and maternal blood nutrient levels. J Perinat Med. 1994;22:227–34. doi: 10.1515/jpme.1994.22.3.227. [DOI] [PubMed] [Google Scholar]
- 10.Scholl TO, Hediger ML, Schall JI, Fisher RL, Khoo C-S. Low zinc intake during pregnancy: its association with preterm and verypreterm delivery. Am J Epidemiol. 1993;137:1115–24. doi: 10.1093/oxfordjournals.aje.a116615. [DOI] [PubMed] [Google Scholar]
- 11.Shah D, Sachdev HP. Effect of gestational zinc deficiency on pregnancy outcomes: summary of observation studies and zinc supplementation trials. Br J Nutr. 2001;85(Suppl 2):S101–8. doi: 10.1079/bjn2000301. [DOI] [PubMed] [Google Scholar]
- 12.Burits CA, Ashwood ED. Tietz text book of clinical chemistry. 2nd ed 1994. [Google Scholar]
- 13.Prasad AS. Zinc in human health. J Trace Elem. 1998;11:63–87. [Google Scholar]
- 14.Jameson S. Zinc status and pregnancy outcome in humans. First Edition. Alan R.Liss; 1982. pp. 39–52. [Google Scholar]
- 15.Sanders WB, Sandstead HH. Zinc deficiency, A public health problem? Am J Dischild. 1991;145:853–59. doi: 10.1001/archpedi.1991.02160080029016. [DOI] [PubMed] [Google Scholar]
- 16.Prasad AS. Syndrome of iron deficiency, anemia, hepatic, hypogonadism, dwarfism and geophagia. Am J Med. 1961;31:532–46. doi: 10.1016/0002-9343(61)90137-1. [DOI] [PubMed] [Google Scholar]
- 17.Osendarp SJ, Van Raaij JM, Darmstadt GL, Baqui AH, Hautvast JG, Fuchs GJ. Zinc supplementation during pregnancy and effects on growth and morbidity in low birth weight infants a randomized placebo controlled trial. Lancet. 2001;357:1080–85. doi: 10.1016/s0140-6736(00)04260-4. [DOI] [PubMed] [Google Scholar]
- 18.Norrozi M, Borna S, Hanachi P, Faghyhzadeh S, Haghollahi F, Golkho Sh. Evaluation of Zinc Supplementation Effect on Fetal Outcomes in Pregnant Women with Lower-than-Median Serum Zinc Concentration. Journal of Family and Reproductive Health. 2012;6:85–9. [Google Scholar]
- 19.Hanachi P, Golkho S, Norrozi M. The association of serum Zinc levels with socio demographic factors, red and white blood cells count in pregnant women. Journal Applied Science. 2008;8:4679–83. [Google Scholar]
- 20.Abebe Y, Bogale A, Hambidge KM, Stoecker BJ, Arbide I, Teshome A, Krebs NF, Westcott JE, Bailey KB, Gibson RS. Inadequate intakes of dietary zinc among pregnant women from subsistence households in Sidama, Southern Ethiopia. Public Health Nutr. 2008;11:379–86. doi: 10.1017/S1368980007000389. [DOI] [PubMed] [Google Scholar]
- 21.Pezzullo JC. Proportion Difference Power/Sample Size Calculation. http://statpages.org/proppowr.html.
- 22.Hunt IF, Murphy NJ, Cleaver AE, Faraji B, Swendseid ME, Coulson AH, et al. Zinc supplementation during pregnancy: zinc concentration of serum and hair from low-income women of Mexican descent. Am J Clin Nutr. 1985;37:572–82. doi: 10.1093/ajcn/37.4.572. [DOI] [PubMed] [Google Scholar]
- 23.Tuttle S, Aggett PJ, Campbell D, MacGillivray I. Zinc and copper nutrition in human pregnancy: a longitudinal study in normal primigravidae and in primigravidae at risk of delivering a growth retarded baby. Am J Clin Nutr. 1985;41:1032–41. doi: 10.1093/ajcn/41.5.1032. [DOI] [PubMed] [Google Scholar]
- 24.Andersen AMN, Mortensen LH. Socioeconomic inequality in birth outcomes: what do the indicators tell us, and where do we find the data. CMAJ. 2006;174:1429–30. doi: 10.1503/cmaj.060349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ugwuja EI, Ugwu NC. Helicobacter pylori in uninvestigated dyspepsia in primary health cares in Abakaliki, Nigeria. Online J Health Allied Sci. 2007;1:4–10. [Google Scholar]
- 26.Salimi S, Yaghmaei M, Joshaghani HR, Mansourian AR. Study of Zinc Deficiency in Pregnant Women. Iranian J Publ Health. 2004;33:15–18. [Google Scholar]
- 27.King JC. Determinants of maternal zinc status during pregnancy. Am J Clin Nutr. 2000;71(suppl):1334S. doi: 10.1093/ajcn/71.5.1334s. [DOI] [PubMed] [Google Scholar]
- 28.Gebremedhin S, Enquselassie F, Umeta M. Prevalence of prenatal zinc deficiency and its association with socio-demographic, dietary and health care related factors in Rural Sidama, Southern Ethiopia: A cross-sectional study. BMC Public Health. 2011;11:898. doi: 10.1186/1471-2458-11-898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldenberg RL, Tamura T, Neggers Y, Copper RL, Johnston KE, Dubard MB, et al. The effect of zinc supplementation on pregnancy outcome. JAMA. 1995;9:463–68. doi: 10.1001/jama.1995.03530060037030. [DOI] [PubMed] [Google Scholar]