Abstract
Background
Rural residents face numerous barriers to healthcare access and studies suggest poorer health outcomes for rural patients. Therefore we undertook a systematic review to determine if cardiovascular medication utilization and adherence patterns differ for rural versus urban patients.
Methods
A comprehensive search of major electronic datasets was undertaken for controlled clinical trials and observational studies comparing utilization or adherence to cardiovascular medications in rural versus urban adults with cardiovascular disease or diabetes. Two reviewers independently identified citations, extracted data, and evaluated quality using the STROBE checklist. Risk estimates were abstracted and pooled where appropriate using random effects models. Methods and reporting were in accordance with MOOSE guidelines.
Results
Fifty-one studies were included of fair to good quality (median STROBE score 17.5). Although pooled unadjusted analyses suggested that patients in rural areas were less likely to receive evidence-based cardiovascular medications (23 studies, OR 0.88, 95% CI 0.79, 0.98), pooled data from 21 studies adjusted for potential confounders indicated no rural–urban differences (adjusted OR 1.02, 95% CI 0.91, 1.13). The high heterogeneity observed (I2 = 97%) was partially explained by treatment setting (hospital, ambulatory care, or community-based sample), age, and disease. Adherence did not differ between urban versus rural patients (3 studies, OR 0.94, 95% CI 0.39, 2.27, I2 = 91%).
Conclusions
We found no consistent differences in rates of cardiovascular medication utilization or adherence among adults with cardiovascular disease or diabetes living in rural versus urban settings. Higher quality evidence is needed to determine if differences truly exist between urban and rural patients in the use of, and adherence to, evidence-based medications.
Keywords: Cardiovascular diseases, Rural population, Urban population, Medication adherence, Drug utilization
Background
Rural and urban communities have distinct characteristics in terms of demographics, social, and physical environments, and may vary in access to healthcare facilities and services. Rural residents tend to be older and are more likely to be obese, have less education, and lower income than urban residents [1-6]. Rural populations also have a higher prevalence of chronic conditions such as diabetes and heart disease [1,7-9]. Some studies have shown worse health outcomes among rural populations, including a higher risk of cardiovascular-related morbidity and mortality compared to urban populations [3,4,10-13]. For example, in Canada, mortality from circulatory diseases is higher in rural than urban communities, as is the risk of heart failure-related mortality, hospitalization and emergency department visits [4,10,11]. Similarly, in the UK a higher risk of in-hospital death due to ischemic heart disease has been observed among rural residents [12], and in Australia, mortality due to six major chronic diseases consistently increased in areas that were increasingly remote [13]. Collectively, these characteristics suggest increased healthcare needs for those living in rural communities.
However, rural residents report several barriers to accessing healthcare including transportation difficulties and distance to care, social isolation, financial constraints, limited health care facilities (hospitals and pharmacies), physician shortages, and lack of access to specialist care [14-19]. Indeed, in the US, rural areas contain 19% of the population but only 11% of the physician workforce [15], and the ratio of specialists per population consistently declines as locations become smaller and more remote [15,17]. The lack of access to primary care physicians, specialists, or health care facilities has been postulated to result in decreased prescribing of evidence based medications. However, a previous systematic review found no clear rural–urban difference in the prevalence or intensity of prescription drug use in older adults – although that review included a wide variety of health conditions and medications [20]. It is possible that important differences may exist for certain disease states or medication conditions. As a result, we conducted a systematic review that evaluated whether cardiovascular-related medication utilization and adherence patterns differ for rural versus urban adults with cardiovascular disease or diabetes. These two disease states were selected as they affect a large number of patients, are associated with high morbidity and mortality, often require multiple medications to manage, and outcomes are known to be different between rural and urban patients [21].
Methods
Inclusion and exclusion criteria
Controlled clinical trials or observational studies were included if they enrolled adults with established cardiovascular disease (atrial fibrillation, hypertension, heart failure, coronary artery disease) or diabetes, and reported cardiovascular medication use or adherence patterns for patients living in rural versus urban communities. Medications of interest included acetylsalicylic acid (ASA), antithrombotic, anticoagulant, antihypertensive (including angiotensin converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARB)), or lipid lowering agents. The research question, inclusion and exclusion criteria, and review methods were outlined in a protocol developed a priori according to the PRISMA guidelines [22].
Since the definition of rural and urban varied substantially between studies, we a priori defined populations described as urban, city dwelling, or metropolitan in the primary publication as urban. Conversely, rural descriptors included town, village, country dwelling, non-metropolitan or remote communities. Any definition of adherence or persistence used in primary studies was accepted. Only full text, peer reviewed articles, were included. Studies evaluating the use of medications for acute management, such as during hospitalization, were excluded, as were studies conducted in developing countries where management approaches may be substantially different. The populations of interest were those with established cardiovascular disease or diabetes, in whom several evidence-based medications are recommended for use. Two researchers (GKM, DLW) independently screened all studies and extracted all data using pre-defined forms and definitions, and disagreements were resolved through discussion, or by a third researcher (DTE).
Literature search strategy
A comprehensive search strategy implemented by a research librarian was done in April 2012 in the following electronic databases: MEDLINE®, PubMed, Embase, International Pharmaceutical Abstracts, CINAHL, and Web of Science® and reference lists of included articles were also manually searched. Previously identified included studies were searched in Scopus to gather additional subject headings. No language, study design or date restrictions were applied. The MEDLINE® search strategy is listed in (Additional file 1: Table S1).
Data extraction and quality assessment
Studies were evaluated for bias, and the STROBE checklist was used to assess the quality of reporting [23]. Study authors were contacted for missing information on rural–urban comparisons, and in two cases additional data were provided (unpublished data V. Maio 2012, I. Carey 2011). Both unadjusted and adjusted data were abstracted or calculated where possible [24]. If more than one adjusted analysis was reported, the analysis that adjusted for the most confounders was extracted, and medication use data for patients without contraindications to treatment were preferred over populations that may have included patients who were not eligible for a specific therapy. Where possible, studies reporting multiple rural or urban populations were combined.
Data analysis methods
To summarize the effects of rural and urban location on medication utilization or adherence both unadjusted and adjusted pooled effects were calculated. As we expected heterogeneity between studies, we pooled effect estimates using a random effects model with inverse variance weighting and Review Manager 5.1 software [25]. Heterogeneity was assessed using the I2 statistic with an I2 statistic >50% being considered as moderate heterogeneity. There was no a priori degree of heterogeneity that precluded pooling. For studies reporting multiple outcomes within the same cohort [e.g., % receiving beta-blockers (BB) and % receiving an ACEI], a pooled estimate of the odds of treatment were calculated using methods recommended by Borgenstein et al. [26] that accounts for the fact that patients within each outcome are not mutually exclusive (i.e., a patient may have received both a BB and an ACEI). Since the correlation of outcomes is unknown, we used a moderate correlation of 0.5 with sensitivity analyses using 0.25, 0.75 or 1 and found there was little impact on the results. Subgroup analyses were further conducted to explore the robustness of our results and potential sources of heterogeneity. Studies reporting data not suitable for meta-analysis (e.g. outcomes other than OR, or with missing data) were summarized narratively. Publication bias was assessed using funnel plots and Egger’s test.
Results
A total of 11092 citations were identified in the literature search and 51 unique studies (described in 52 publications), met the inclusion criteria (Figure 1) [2,8,9,27-75]. Fifteen studies were cohort studies and 36 were cross sectional or repeat cross sectional studies (Additional file 1: Table S2). The included studies were published over a 21-year time span (1990 to 2011) and had quality scores based on the STROBE checklist that ranged from 8.5 to 21 (median 17.5) out of a total of 22 possible items (0.5 points given for partial reporting). Two reports provided data on the same study [44,48], and six studies included data for more than one patient cohort [43,49,54,66,71,72]. Thus, 58 patient populations (or cohorts) were included in our study. Two studies were in a language other than English and were translated using on-line resources and local expertise [37,70]. There was good agreement between reviewers on study selection (kappa 0.82, 95% confidence interval [CI] 0.75 to 0.90).
Figure 1.
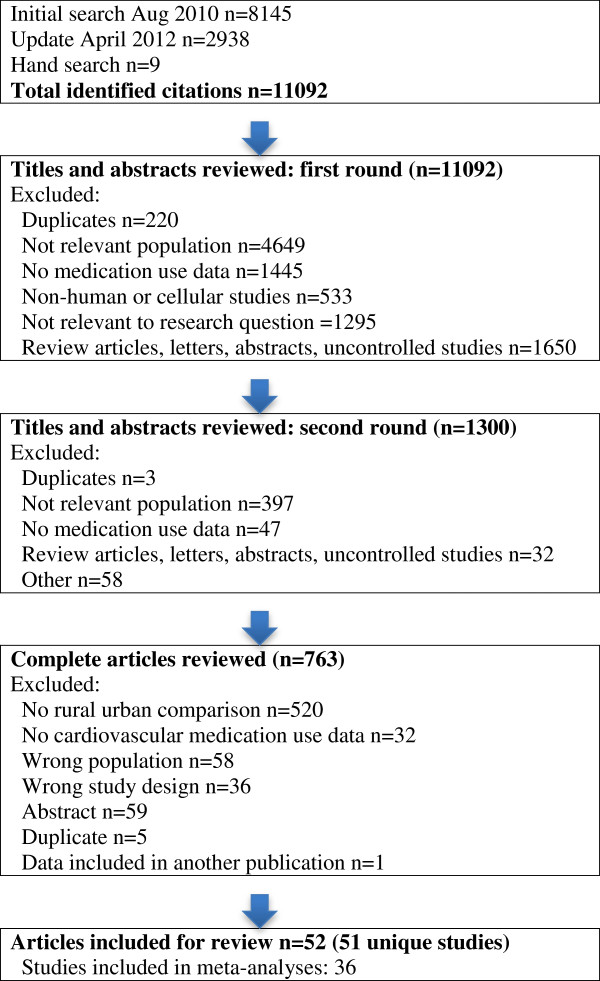
Flow chart of systematic search.
Patients were selected from a hospital setting in 12 studies, from ambulatory care practices in 17 studies, and in 22 studies, patients were selected from population-based or community-dwelling samples. Exploring rural–urban differences was the primary objective of 18 studies (35%) [2,27,28,30,31,35,36,39,43,44,49,51,54,59,68,69,71,73]. Seven studies reported medication adherence (the proportion of doses taken as prescribed over a specific time period) or persistence (the length of continuous treatment) [76], and 47 reported outcomes related to medication utilization. Among the studies, there were substantial variations in how medication utilization or adherence to medications was assessed. Overall, 16 studies included patient self-report, 31 studies included data from medical records or registries, and 5 studies were conducted using administrative databases. Nineteen studies reported crude utilization or adherence outcome data only [8,28,35-37,39,40,50,51,53,54,63,64,67,68,71,73-75].
Included studies varied in their characteristics (Additional file 1: Table S2). Studies ranged in sample size from 32 to approximately one million and were conducted in a range of areas including the US (30 studies), Europe (14), Canada (5) and Australia (2). Patient populations included those with acute myocardial infarction or coronary artery disease (18 studies), hypertension (16), diabetes (8), chronic heart failure (6), atrial fibrillation (5), or mixed cardiovascular disease populations (5). The average age of study participants ranged from 42 to 80 years, and 28% to 63% were female.
Medication utilization
Forty seven (92%) studies [2,8,9,27-36,38-47,49,51-69,71-73,75] evaluated cardiovascular medication utilization with 20 (39%) studies specifically evaluating utilization of ASA or other anti-thrombotic agents, 34 (67%) evaluating antihypertensive use, and 11 (22%) evaluating the use of lipid lowering agents (Additional file 1: Table S3). Substantial variation in the use of cardiovascular medications was observed between studies and between rural versus urban sub-populations within each study. Indeed, the absolute difference in the utilization of cardiovascular medications ranged from -46% to +4% in rural versus urban patients for ASA or other anti-thrombotic drugs, -37% to +25% for antihypertensive drugs, and -45% to +8% for lipid lowering agents. Of the 47 studies that evaluated cardiovascular medication use, sufficient data for pooling were available in 34 studies (39 separate cohorts as two cohorts were included in three studies [43,66,72] and three cohorts in one study [71]). In the unadjusted pooled analyses (23 studies) [27-29,35,36,38,39,41,43,44,46,47,51,53,55-58,64,68,71,73,75], patients in rural areas with cardiovascular disease or diabetes were less likely to receive evidence-based cardiovascular drug therapy compared to urban residents (pooled unadjusted OR 0.88, 95% CI 0.79, 0.98, p = 0.02; I2 = 97%) (Table 1). However, among the 21 studies that adjusted for potential confounders [9,27,29,34,38,41-45,47,52,55,56,58,60-62,66,69,72] pooled analysis indicated no statistically significant difference between rural and urban patients in the use of cardiovascular medications (pooled adjusted OR 1.02, 95% CI 0.91 to 1.13, p = 0.77, I2 = 97%) (Figure 2). In both analyses there was substantial heterogeneity between studies. Although numerous subgroup analyses by setting, drug class, disease, age, country, and publication year were undertaken, similar results were observed and these factors only partially explained some of the variation between studies (Table 1; Figures 2 and 3). Moreover, when studies were categorized according to how the outcome was assessed (patient self-report, medical chart review, or administrative data), similar results were observed (Table 1). Additional analyses by study quality, for countries with universal health care systems, and for specific drugs, such as ACEI/ARB, also found similar findings (Additional file 1: Table S4). Among studies reporting data not suitable for meta-analysis, the findings were also consistent in that there was no clear trend towards a reduction or increase in cardiovascular medication utilization between rural and urban patients [2,8,30-33,40,49,54,59,63,65,67].
Table 1.
Meta-analysis of medication utilization and adherence outcomes
| Analysis | N cohorts* | Rural/urban OR of treatment (95% CI) | I 2 (%) | Subgroup difference |
|---|---|---|---|---|
|
Cardiovascular medication utilization | ||||
| Overall - unadjusted |
26 |
0.88 (0.79, 0.98) |
97 |
NA |
| Overall - adjusted |
23 |
1.02 (0.91, 1.13) |
97 |
NA |
|
Subgroup analysis – adjusted |
|
|
|
|
|
Setting |
|
|
|
|
| Community or population-based |
8 |
1.15 (1.06, 1.25) |
71 |
P < 0.0001 |
| Hospital |
6 |
0.87 (0.83, 0.92) |
34 |
|
| Ambulatory care practice |
9 |
1.02 (0.85, 1.24) |
78 |
|
|
Drug class |
|
|
|
|
| Antithrombotic or anticoagulant |
9 |
1.00 (0.88, 1.14) |
88 |
P = 0.62 |
| Antihypertensive |
16 |
1.03 (0.90, 1.17) |
92 |
|
| Lipid lowering agent |
4 |
0.94 (0.83, 1.07) |
37 |
|
|
Disease |
|
|
|
|
| Atrial fibrillation |
3 |
0.83 (0.59, 1.16) |
67 |
P = 0.0001 |
| Cardiovascular disease |
11 |
0.95 (0.88, 1.03) |
67 |
|
| Hypertension |
6 |
1.07 (0.87, 1.33) |
79 |
|
| Diabetes |
3 |
1.21 (1.12, 1.31) |
76 |
|
|
Age (study mean or median) |
|
|
|
|
| <65 years |
8 |
1.15 (1.04, 1.26) |
80 |
P = 0.005 |
| ≥65 years |
12 |
0.98 (0.88, 1.08) |
70 |
|
| Not reported |
3 |
0.89 (0.77, 1.02) |
64 |
|
|
Country |
|
|
|
|
| US |
18 |
1.01 (0.92, 1.10) |
87 |
P = 0.67 |
| Non-US |
5 |
1.05 (0.88, 1.26) |
88 |
|
|
Publication Year |
|
|
|
|
| 1999-2005 |
7 |
1.06 (0.91, 1.22) |
76 |
P = 0.66 |
| 2006-2011 |
16 |
1.01 (0.88, 1.15) |
98 |
|
|
Data source |
|
|
|
|
| Administrative data |
2 |
1.17 (0.97, 1.41) |
87 |
P = 0.19 |
| Medical record |
14 |
0.97 (0.87, 1.08) |
86 |
|
| Patient self-report |
7 |
1.07 (0.93, 1.22) |
72 |
|
|
Cardiovascular medication adherence | ||||
| |
N |
Rural/urban OR of treatment (95% CI) |
I
2
(%) |
Subgroup difference |
| Overall - unadjusted | 4 | 0.94 (0.39, 2.27) | 91 | NA |
Figure 2.
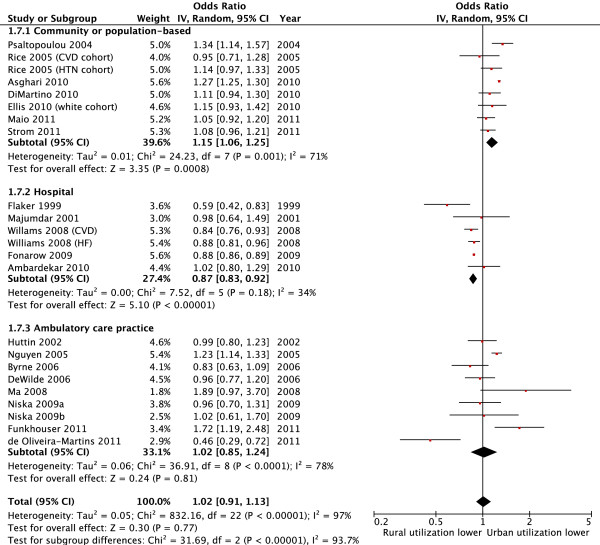
Use of cardiovascular drugs by rural versus urban patients, stratified by study setting (adjusted analysis).
Figure 3.
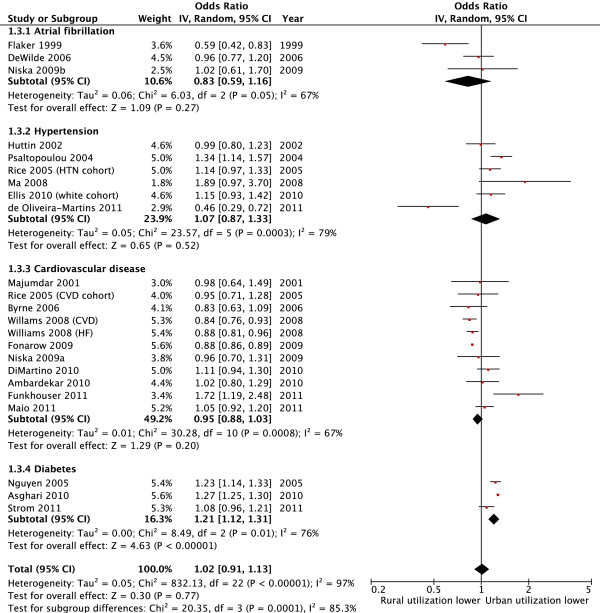
Use of cardiovascular drugs by rural versus urban patients, stratified by disease (adjusted analysis).
Publication bias was assessed by visually examining funnel plots and no obvious asymmetry was noted (Egger’s p value = 0.98).
Medication adherence or persistence
Six (12%) studies [29,37,46,70,73,74] evaluated cardiovascular medication adherence and two (4%) studies [46,50] evaluated medication persistence. Adherence was measured as the percentage of doses taken [73], the proportion of patients with a medication possession ratio ≥0.8 [46], and was undefined in three studies [37,70,74]. Persistence was measured as the proportion of patients remaining on the same [46,50] or any treatment [46] at the end of the follow up. In five studies, the drugs evaluated were antihypertensive agents, one study evaluated heart failure medications [73], and one assessed ASA or ACEI/ARB adherence [29].
Cardiovascular medication adherence or persistence findings were inconsistent across studies (Additional file 1: Table S3). The absolute difference in proportion adherent or persistent with medications ranged from -41% to +8% for rural versus urban patients. The odds of treatment persistence were significantly higher in rural versus urban patients in one report (adjusted OR 1.28, 95% CI 1.25, 1.32) [46], but was not statistically different in a second study (OR 0.96, 95% CI 0.55, 1.67) [50], Medication adherence data from three studies (4 cohorts) were pooled and showed no statistically significant difference between rural and urban patients (unadjusted OR 0.94, 95% CI 0.39, 2.27, p = 0.89, I2 = 91%) Table 1[29,37,70]. In two other reports with data not suitable for meta-analysis, medication adherence was significantly higher in one study (92% versus 83% of doses taken, p = 0.01) [73], and significantly lower in the other (10% versus 17% of patients compliant, p < 0.01) [74], for rural versus urban patients, based on unadjusted data. The three studies reporting treatment adherence adjusted for confounders reported adherence to be significantly higher in rural patients (OR medication possession ratio ≥0.8: antihypertensive agents 1.2, 95% CI 1.1, 1.3; ASA 1.14, 95% CI 1.10, 1.18; ACEI/ARB 1.18 95% CI 1.14, 1.23) or rural men (OR adherent 4.0, 95% CI 1.1, 13.9) [29,46,70].
Discussion
Our systematic review of the literature found that rural patients were 12% less likely to receive cardiovascular medications than urban patients in unadjusted analyses; however, pooling of data adjusted for patient, practitioner or other factors revealed no differences in the proportions of rural and urban patients receiving therapy. This suggests that differences in these characteristics between rural and urban residents are largely responsible for the discrepancies in medication use observed and is consistent with previous studies showing important differences in the demographics, health behaviors, and overall health of people living in rural and urban areas [1,3,4,7]. In this review, many of the included reports provided little data on the demographics or comorbidities of the rural and urban patient groups, which hindered our ability to assess the similarity of these populations. As a result, it is difficult to draw conclusions from those studies that reported only unadjusted rural–urban comparisons.
When medication utilization data were pooled, substantial between-study heterogeneity was observed (I2 = 97%). Some of this variability could be explained by differences in the setting (hospital, ambulatory care practice or community-based sample), age, and disease state. While most studies adjusted for some clinical characteristics, only some controlled for socioeconomic factors that could also have impacted medication use. Indeed only fourteen studies [27,32,34,42,43,45,47,52,57,58,61,62,66,69] reported adjustment for health insurance and previous studies have shown patients with a chronic condition who lack medication insurance are less likely to take medications or frequently skip doses due to cost [52,66,77].
Similarly, we found no consistent relationship between rural residence and cardiovascular medication adherence or persistence rates based on unadjusted data. The adjusted analysis suggested higher adherence and persistence for rural residents, although there were few studies reporting these outcomes. Rural–urban differences in other health behaviors, such as smoking, exercise, and consumption of fruits and vegetables have been reported [4], and considering the link between adherence and positive health outcomes [78], further study is warranted.
Although we conducted an exhaustive search for literature and conducted our systematic review in accordance to the highest reporting standards, our review is not without limitations. Firstly, studies evaluating differences in urban versus rural settings within subgroup analyses may not have been easily identified. Second, as in any systematic review, the findings are limited by the quality of the individual studies. Potential limitations included reporting bias [32,33,40,41,45,49,51,54,71,72], selection bias [9,35,54], lack of generalizability [9,28,36,37,39,50,51,59,71,73,74], limited sample size [28,36,37,39,50,64,73], no adjustment for confounders [8,28,35-37,40,50,54,64,74,75], and poor reporting (STROBE score below the 25th percentile) [8,28,36,37,40,44,50-52,54,59,64,70,71,74]. Third, we accepted a broad range of definitions for rural and urban populations, which may have affected study results. In 25 studies [8,28,34,36,37,40-43,45,46,50,52,53,55-60,64-66,72,74] no clear definition of rural and urban were provided and various definitions were used in the remaining studies. It is possible some of the heterogeneity observed in our pooled analysis is related to these differences in definitions, although subgroup analysis by studies with defined and undefined rural populations showed similar results. Fourth, between-study heterogeneity was high and not fully explained despite multiple subgroup analyses by setting, drug class, disease, age, country, publication year, and data source (self-report, administrative or medical records). Moreover, clinical indications and classification of disease may also have changed over time increasing the heterogeneity between studies. Last, our review only included adults with established cardiovascular disease as medication utilization for secondary prevention was expected to be high within patients; thus, improving the power to detect differences if differences exist between rural and urban patients. Moreover, as cardiovascular medications are widely prescribed medications in the general adult population, our results would be expected to be highly generalizable.
Conclusions
In conclusion, we found no consistent relationship between rural versus urban residence and utilization of, or adherence with evidence-based cardiovascular medications among adults with cardiovascular disease or diabetes. There was substantial between-study variation that was only partially explained by the setting, age, and disease. Higher quality evidence is needed to determine if differences in cardiovascular medication utilization and adherence between urban and rural patients truly exist.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GKM and DLW screened, extracted and assessed the quality of studies. GKM conducted the meta-analysis. LT conducted the literature search and prepared the bibliography. GKM, DTE and FAM drafted the report. All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and accuracy of the data analysis. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
The supplementary material includes Tables S1-S4, the literature search strategy, summary of the included study characteristics and results, and the supplementary meta-analyses.
Contributor Information
Gaetanne K Murphy, Email: gkmurphy@ualberta.ca.
Finlay A McAlister, Email: finlay.mcalister@ualberta.ca.
Daniala L Weir, Email: daniala@ualberta.ca.
Lisa Tjosvold, Email: tjosvold@ualberta.ca.
Dean T Eurich, Email: deurich@ualberta.ca.
References
- Krishna S, Gillespie KN, McBride TM. Diabetes burden and access to preventive care in the rural United States. J Rural Health. 2010;26:3–11. doi: 10.1111/j.1748-0361.2009.00259.x. [DOI] [PubMed] [Google Scholar]
- Vanasse A, Courteau J, Cohen AA, Orzanco MG, Drouin C. Rural–urban disparities in the management and health issues of chronic diseases in Quebec (Canada) in the early 2000s. Rural Remote Health. 2010;10:1548. [PubMed] [Google Scholar]
- Probst JC, Bellinger JD, Walsemann KM, Hardin J, Glover SH. Higher risk of death in rural blacks and whites than urbanites is related to lower incomes, education, and health coverage. Health Aff (Millwood) 2011;30:1872–1879. doi: 10.1377/hlthaff.2011.0668. [DOI] [PubMed] [Google Scholar]
- DesMeules M, Pong R, Lagace C, Heng D, Manuel D, Pitblado R, Bollman R, Guernsey J, Kazanjian A, Koren I. How Healthy Are Rural Canadians: An Assessment Of Their Health Status And Health Determinants. Ottawa, ON: Canadian Institute for Health Information; 2006. https://secure.cihi.ca/free_products/acknowledgements_rural_canadians_2006_report_e.pdf. Accessed 2012 Sep 01. [Google Scholar]
- Gartner A, Farewell D, Roach P, Dunstan F. Rural/urban mortality differences in England and Wales and the effect of deprivation adjustment. Soc Sci Med. 2011;72:1685–1694. doi: 10.1016/j.socscimed.2011.03.017. [DOI] [PubMed] [Google Scholar]
- Smith KB, Humphreys JS, Wilson MGA. Addressing the health disadvantage of rural populations: how does epidemiological evidence inform rural health policies and research? Aust J Rural Health. 2008;16:56–66. doi: 10.1111/j.1440-1584.2008.00953.x. [DOI] [PubMed] [Google Scholar]
- Jones A, Goza F. Rural, suburban and urban differences in the self-diagnosis of coronary heart disease in the United States. J Biosoc Sci. 2008;40:895–909. doi: 10.1017/S0021932008002769. [DOI] [PubMed] [Google Scholar]
- Banegas JR, Rodriguez-Artalejo F, de la Cruz Troca JJ, Guallar-Castillon P, del Rey Calero J. Blood pressure in Spain: distribution, awareness, control, and benefits of a reduction in average pressure. Hypertension. 1998;32:998–1002. doi: 10.1161/01.HYP.32.6.998. [DOI] [PubMed] [Google Scholar]
- Psaltopoulou T, Orfanos P, Naska A, Lenas D, Trichopoulos D, Trichopoulou A. Prevalence, awareness, treatment and control of hypertension in a general population sample of 26,913 adults in the Greek EPIC study. Int J Epidemiol. 2004;33:1345–1352. doi: 10.1093/ije/dyh249. [DOI] [PubMed] [Google Scholar]
- Gamble JM, Eurich DT, Ezekowitz JA, Kaul P, Quan H, McAlister FA. Patterns of care and outcomes differ for urban versus rural patients with newly diagnosed heart failure, even in a universal healthcare system. Circ Heart Fail. 2011;4:317–323. doi: 10.1161/CIRCHEARTFAILURE.110.959262. [DOI] [PubMed] [Google Scholar]
- Teng T-HK, Katzenellenbogen JM, Hung J, Knuiman M, Sanfilippo FM, Geelhoed E, Hobbs M, Thompson SC. Rural–urban differentials in 30-day and 1-year mortality following first-ever heart failure hospitalisation in Western Australia: a population-based study using data linkage. BMJ Open. 2014;4:e004724. doi: 10.1136/bmjopen-2013-004724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin KA, Leyland AH. Urban–rural inequalities in ischemic heart disease in Scotland, 1981–1999. Am J Public Health. 2006;96:145–151. doi: 10.2105/AJPH.2004.051193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chondur R, Li SQ, Guthridge S, Lawton P. Does relative remoteness affect chronic disease outcomes? Geographic variation in chronic disease mortality in Australia, 2002–2006. Aust N Z J Public Health. 2014;38:117–121. doi: 10.1111/1753-6405.12126. [DOI] [PubMed] [Google Scholar]
- Goins RT, Williams KA, Carter MW, Spencer SM, Solovieva T. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005;21:206–213. doi: 10.1111/j.1748-0361.2005.tb00084.x. [DOI] [PubMed] [Google Scholar]
- Fordyce MA, Chen FM, Doescher MP, Hart LG. 2005 Physician Supply and Distribution in Rural Areas of the United States. Final Report. WWAMI Rural Health Research Center, University of Washington; 2007. Report No: 116. http://depts.washington.edu/uwrhrc/uploads/RHRC%20FR116%20Fordyce.pdf. [Google Scholar]
- Aneja S, Ross JS, Wang Y, Matsumoto M, Rodgers GP, Bernheim SM, Rathore SS, Krumholz HM. US cardiologist workforce from 1995 to 2007: modest growth, lasting geographic maldistribution especially in rural areas. Health Aff (Millwood) 2011;30:2301–2309. doi: 10.1377/hlthaff.2011.0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pong RW, DesMeules M, Heng D, Lagace C, Guernsey JR, Kazanjian A, Manuel D, Pitblado JR, Bollman R, Koren I, Dressler MP, Wang F, Luo W. Patterns of health service utilization in rural Canada. Chronic Dis Can. 2011;31(Supp 1):1–36. [PubMed] [Google Scholar]
- Sibley LM, Weiner JP. An evaluation of access to health care services along the rural–urban continuum in Canada. BMC Health Serv Res. 2011;11:20. doi: 10.1186/1472-6963-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klepser DG, Xu L, Ullrich F, Mueller KJ. Trends in community pharmacy counts and closures before and after the implementation of Medicare part D. J Rural Health. 2011;27:168–175. doi: 10.1111/j.1748-0361.2010.00342.x. [DOI] [PubMed] [Google Scholar]
- Grymonpre RE, Hawranik PG. Rural residence and prescription medication use by community-dwelling older adults: a review of the literature. J Rural Health. 2008;24:203–209. doi: 10.1111/j.1748-0361.2008.00159.x. [DOI] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ. Heart disease and stroke statistics–2012 update: a report from the American heart association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Altman DG, Bland JM. How to obtain the confidence interval from a P value. BMJ. 2011;343:d2090. doi: 10.1136/bmj.d2090. [DOI] [PubMed] [Google Scholar]
- Review Manager (RevMan). [Computer program]. Version 5.1. Review Manager (RevMan). [Computer program]. Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2011. [Google Scholar]
- Borgenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. Chichester, UK: John Wiley & Sons; 2009. Multiple outcomes or time-points within a study; pp. 225–238. [Google Scholar]
- Ambardekar AV, Fonarow GC, Dai D, Peterson ED, Hernandez AF, Cannon CP, Krantz MJ. Quality of care and in-hospital outcomes in patients with coronary heart disease in rural and urban hospitals (from get with the guidelines-coronary artery disease program) Am J Cardiol. 2010;105:139–143. doi: 10.1016/j.amjcard.2009.09.003. [DOI] [PubMed] [Google Scholar]
- Andrus MR, Kelley KW, Murphey LM, Herndon KC. A comparison of diabetes care in rural and urban medical clinics in Alabama. J Community Health. 2004;29:29–44. doi: 10.1023/b:johe.0000007443.96138.03. [DOI] [PubMed] [Google Scholar]
- Asghari S, Courteau J, Drouin C, Gregoire JP, Carpentier AC, Paquet M, Vanasse A. Adherence to vascular protection drugs in diabetic patients in Quebec: a population-based analysis. Diab Vasc Dis Res. 2010;7:167–171. doi: 10.1177/1479164109360593. [DOI] [PubMed] [Google Scholar]
- Baldwin LM, Chan L, Andrilla CH, Huff ED, Hart LG. Quality of care for myocardial infarction in rural and urban hospitals. J Rural Health. 2010;26:51–57. doi: 10.1111/j.1748-0361.2009.00265.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin LM, MacLehose RF, Hart LG, Beaver SK, Every N, Chan L. Quality of care for acute myocardial infarction in rural and urban US hospitals. J Rural Health. 2004;20:99–108. doi: 10.1111/j.1748-0361.2004.tb00015.x. [DOI] [PubMed] [Google Scholar]
- Bradley EH, Herrin J, Mattera JA, Holmboe ES, Wang Y, Frederick P, Roumanis SA, Radford MJ, Krumholz HM. Hospital-level performance improvement: beta-blocker use after acute myocardial infarction. Med Care. 2004;42:591–599. doi: 10.1097/01.mlr.0000128006.27364.a9. [DOI] [PubMed] [Google Scholar]
- Bradley EH, Herrin J, Mattera JA, Holmboe ES, Wang Y, Frederick P, Roumanis SA, Radford MJ, Krumholz HM. Quality improvement efforts and hospital performance: rates of beta-blocker prescription after acute myocardial infarction. Med Care. 2005;43:282–292. doi: 10.1097/00005650-200503000-00011. [DOI] [PubMed] [Google Scholar]
- Byrne M, Murphy AW, Walsh JC, Shryane E, McGroarty M, Kelleher CC. A cross-sectional study of secondary cardiac care in general practice: impact of personal and practice characteristics. Fam Pract. 2006;23:295–302. doi: 10.1093/fampra/cml003. [DOI] [PubMed] [Google Scholar]
- Clark RA, Eckert KA, Stewart S, Phillips SM, Yallop JJ, Tonkin AM, Krum H. Rural and urban differentials in primary care management of chronic heart failure: new data from the CASE study. Med J Aust. 2007;186:441–445. doi: 10.5694/j.1326-5377.2007.tb00993.x. [DOI] [PubMed] [Google Scholar]
- Colleran KM, Richards A, Shafer K. Disparities in cardiovascular disease risk and treatment: demographic comparison. J Investig Med. 2007;55:415–422. doi: 10.2310/6650.2007.00028. [DOI] [PubMed] [Google Scholar]
- Czarnecka D, Pawelec M, Kopacz E, Kloch M. Socioeconomical status of life and regularity of intake of medicines among hypertensive patients. Przegl Lek. 2006;63:633–636. [PubMed] [Google Scholar]
- de Oliveira-Martins S, Oliveira T, Gomes JJF, Caramona M, Cabrita J. Factors associated with arterial hypertension in pharmacy users in Portugal. Rev Saude Publica. 2011;45:136–144. doi: 10.1590/S0034-89102010005000056. [DOI] [PubMed] [Google Scholar]
- Dellasega C, Orwig D, Ahern F, Lenz E. Postdischarge medication use of elderly cardiac patients from urban and rural locations. J Gerontol A Biol Sci Med Sci. 1999;54:M514–M520. doi: 10.1093/gerona/54.10.M514. [DOI] [PubMed] [Google Scholar]
- DeWilde S, Carey IM, Bremner SA, Richards N, Hilton SR, Cook DG. Evolution of statin prescribing 1994–2001: a case of agism but not of sexism? Heart. 2003;89:417–421. doi: 10.1136/heart.89.4.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWilde S, Carey IM, Emmas C, Richards N, Cook DG. Trends in the prevalence of diagnosed atrial fibrillation, its treatment with anticoagulation and predictors of such treatment in UK primary care. Heart. 2006;92:1064–1070. doi: 10.1136/hrt.2005.069492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMartino LD, Shea AM, Hernandez AF, Curtis LH. Use of guideline-recommended therapies for heart failure in the medicare population. Clin Cardiol. 2010;33:400–405. doi: 10.1002/clc.20760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis C, Grubaugh AL, Egede LE. The effect of minority status and rural residence on actions to control high blood pressure in the U.S. Public Health Rep. 2010;125:801–809. doi: 10.1177/003335491012500607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaker GC, McGowan DJ, Boechler M, Fortune G, Gage B. Underutilization of antithrombotic therapy in elderly rural patients with atrial fibrillation. Am Heart J. 1999;137:307–312. doi: 10.1053/hj.1999.v137.91403. [DOI] [PubMed] [Google Scholar]
- Fonarow GC, French WJ, Frederick PD. Trends in the use of lipid-lowering medications at discharge in patients with acute myocardial infarction: 1998 to 2006. Am Heart J. 2009;157:185–194. doi: 10.1016/j.ahj.2008.09.001. [DOI] [PubMed] [Google Scholar]
- Friedman O, McAlister FA, Yun L, Campbell NR, Tu K. Antihypertensive drug persistence and compliance among newly treated elderly hypertensives in Ontario. Am J Med. 2010;123:173–181. doi: 10.1016/j.amjmed.2009.08.008. [DOI] [PubMed] [Google Scholar]
- Funkhouser E, Houston TK, Levine DA, Richman J, Allison JJ, Kiefe CI. Physician and patient influences on provider performance: beta-blockers in postmyocardial infarction management in the MI-Plus study. Circ Cardiovasc Qual Outcomes. 2011;4:99–106. doi: 10.1161/CIRCOUTCOMES.110.942318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gage BF, Boechler M, Doggette AL, Fortune G, Flaker GC, Rich MW, Radford MJ. Adverse outcomes and predictors of underuse of antithrombotic therapy in medicare beneficiaries with chronic atrial fibrillation. Stroke. 2000;31:822–827. doi: 10.1161/01.STR.31.4.822. [DOI] [PubMed] [Google Scholar]
- Goldman LE, Dudley RA. United States rural hospital quality in the hospital compare database-accounting for hospital characteristics. Health Policy. 2008;87:112–127. doi: 10.1016/j.healthpol.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Hense HW, Tennis P. Changing patterns of antihypertensive drug use in a German population between 1984 and 1987. Results of a population based cohort study in the federal republic of Germany. Eur J Clin Pharmacol. 1990;39:1–7. doi: 10.1007/BF02657047. [DOI] [PubMed] [Google Scholar]
- Hicks PC, Bublitz Emsermann C, Westfall JM, Parnes B. Comparison of HTN management in patients with diabetes between rural and urban primary care clinics in Northeastern Colorado - a report from SNOCAP. Rural Remote Health. 2010;10:1–11. [PubMed] [Google Scholar]
- Huttin C. The role of different types of health insurance on access and utilization of antihypertensive drugs: an empirical study in a US hypertensive population. Dis Manag Health Outcome. 2002;10:419–430. doi: 10.2165/00115677-200210070-00003. [DOI] [Google Scholar]
- Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA. 2004;291:1864–1870. doi: 10.1001/jama.291.15.1864. [DOI] [PubMed] [Google Scholar]
- Lutfiyya MN, Bhat DK, Gandhi SR, Nguyen C, Weidenbacher-Hoper VL, Lipsky MS. A comparison of quality of care indicators in urban acute care hospitals and rural critical access hospitals in the United States. Int J Qual Health Care. 2007;19:141–149. doi: 10.1093/intqhc/mzm010. [DOI] [PubMed] [Google Scholar]
- Ma J, Stafford RS. Screening, treatment, and control of hypertension in US private physician offices, 2003–2004. Hypertension. 2008;51:1275–1281. doi: 10.1161/HYPERTENSIONAHA.107.107086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maio V, Marino M, Robeson M, Gagne JJ. Beta-blocker initiation and adherence after hospitalization for acute myocardial infarction. Eur J Cardiovasc Prev Rehabil. 2011;18:438–445. doi: 10.1177/1741826710389401. [DOI] [PubMed] [Google Scholar]
- Majumdar SR, Gurwitz JH, Soumerai SB. Undertreatment of hyperlipidemia in the secondary prevention of coronary artery disease. J Gen Intern Med. 1999;14:711–717. doi: 10.1046/j.1525-1497.1999.02229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majumdar SR, Inui TS, Gurwitz JH, Gillman MW, McLaughlin TJ, Soumerai SB. Influence of physician specialty on adoption and relinquishment of calcium channel blockers and other treatments for myocardial infarction. J Gen Intern Med. 2001;16:351–359. doi: 10.1046/j.1525-1497.2001.016006351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munschauer FE, Priore RL, Hens M, Castilone A. Thromboembolism prophylaxis in chronic atrial fibrillation: practice patterns in community and tertiary-care hospitals. Stroke. 1997;28:72–76. doi: 10.1161/01.STR.28.1.72. [DOI] [PubMed] [Google Scholar]
- Nguyen KX, Marinac JS, Sun C. Aspirin for primary prevention in patients with diabetes mellitus. Fam Med. 2005;37:112–117. [PubMed] [Google Scholar]
- Niska R, Han B. Statins for secondary cardiovascular disease prevention for older primary care patients. J Natl Med Assoc. 2009;101:705–710. doi: 10.1016/s0027-9684(15)30980-9. [DOI] [PubMed] [Google Scholar]
- Niska R, Han B. Anticoagulation for patients with atrial fibrillation in ambulatory care settings. J Am Board Fam Med. 2009;22:299–306. doi: 10.3122/jabfm.2009.03.080218. [DOI] [PubMed] [Google Scholar]
- Obisesan TO, Vargas CM, Gillum RF. Geographic variation in stroke risk in the United States - region, urbanization, and hypertension in the third national health and nutrition examination survey. Stroke. 2000;31:19–25. doi: 10.1161/01.STR.31.1.19. [DOI] [PubMed] [Google Scholar]
- Perez-Fernandez R, Marino AF, Cadarso-Suarez C, Botana MA, Tome MA, Solache I, Rego-Iraeta A, Mato AJ. Prevalence, awareness, treatment and control of hypertension in Galicia (Spain) and association with related diseases. J Hum Hypertens. 2007;21:366–373. doi: 10.1038/sj.jhh.1002158. [DOI] [PubMed] [Google Scholar]
- Pittrow D, Kirch W, Bramlage P, Lehnert H, Hofler M, Unger T, Sharma AM, Wittchen HU. Patterns of antihypertensive drug utilization in primary care. Eur J Clin Pharmacol. 2004;60:135–142. doi: 10.1007/s00228-004-0731-6. [DOI] [PubMed] [Google Scholar]
- Rice T, Lavarreda SA, Ponce NA, Brown ER. The impact of private and public health insurance on medication use for adults with chronic diseases. Med Care Res Rev. 2005;62:231–249. doi: 10.1177/1077558704273806. [DOI] [PubMed] [Google Scholar]
- Rowan SB, Bailey DN, Bublitz CE, Anderson RJ. Trends in anticoagulation for atrial fibrillation in the U.S.: an analysis of the national ambulatory medical care survey database. J Am Coll Cardiol. 2007;49:1561–1565. doi: 10.1016/j.jacc.2006.11.045. [DOI] [PubMed] [Google Scholar]
- Sheikh K, Bullock C. Urban–rural differences in the quality of care for medicare patients with acute myocardial infarction. Arch Intern Med. 2001;161:737–743. doi: 10.1001/archinte.161.5.737. [DOI] [PubMed] [Google Scholar]
- Strom JL, Lynch CP, Egede LE. Rural/urban variations in diabetes self-care and quality of care in a national sample of US adults with diabetes. Diabetes Educ. 2011;37:254–262. doi: 10.1177/0145721710394875. [DOI] [PubMed] [Google Scholar]
- Tuesca-Molina R, Guallar-Castillon P, Banegas-Banegas JR, Graciani-Perez Regadera A. Determinants of the adherence to therapeutic plan in elderly Spaniards, over 60 years of age. Gac Sanit. 2006;20:220–227. doi: 10.1157/13088853. [DOI] [PubMed] [Google Scholar]
- Wan Q, Harris MF, Davies GP, Jayasinghe UW, Flack J, Georgiou A, Burns JR, Penn DL. Cardiovascular risk management and its impact in Australian general practice patients with type 2 diabetes in urban and rural areas. Int J Clin Pract. 2008;62:53–58. doi: 10.1111/j.1742-1241.2007.01604.x. [DOI] [PubMed] [Google Scholar]
- Williams SC, Koss RG, Morton DJ, Schmaltz SP, Loeb JM. Case volume and hospital compliance with evidence-based processes of care. Int J Qual Health Care. 2008;20:79–87. doi: 10.1093/intqhc/mzm069. [DOI] [PubMed] [Google Scholar]
- Wu JR, Moser DK, Rayens MK, De Jong MJ, Chung ML, Riegel B, Lennie TA. Rurality and event-free survival in patients with heart failure. Heart Lung. 2010;39:512–520. doi: 10.1016/j.hrtlng.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yiannakopoulou EC, Papadopulos JS, Cokkinos DV, Mountokalakis TD. Adherence to antihypertensive treatment: a critical factor for blood pressure control. Eur J Cardiovasc Prev Rehabil. 2005;12:243–249. doi: 10.1097/00149831-200506000-00010. [DOI] [PubMed] [Google Scholar]
- Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, Gupta R, Kelishadi R, Iqbal R, Avezum A, Kruger A, Kutty R, Lanas F, Lisheng L, Wei L, Lopez-Jaramillo P, Oguz A, Rahman O, Swidan H, Yusoff K, Zatonski W, Rosengren A, Teo KK. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378:1231–1243. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong PK. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11:44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- Kwan J, Razzaq A, Leiter LA, Lillie D, Hux JE. Low socioeconomic status and absence of supplemental health insurance as barriers to diabetes care access and utilization. Can J Diabetes. 2008;32:174–181. doi: 10.1016/S1499-2671(08)23007-8. [DOI] [Google Scholar]
- Simpson SH, Eurich DT, Majumdar SR, Padwal RS, Tsuyuki RT, Varney J, Johnson JA. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ. 2006;333:15. doi: 10.1136/bmj.38875.675486.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The supplementary material includes Tables S1-S4, the literature search strategy, summary of the included study characteristics and results, and the supplementary meta-analyses.


