Introduction
Public health efforts involving water fluoridation, nutrition, and dental care access have enhanced the potential for optimal oral health in the United States (U.S.). Yet dental caries persists, with low-income and ethnic/racial minority children experiencing a disproportionate burden of disease. Among groups at risk for oral health disparities, prevalence of dental caries in American Indian and Alaska Native (AI/AN) children is among the highest in the U.S. (1). Compared to other ethnic/racial groups, over 62% of AI/AN preschoolers have early childhood caries (ECC) versus 42% of Mexican-American, 32% African American, and 25% non-Hispanic white children (2). Severity of disease, as measured by decayed, missing, and filled teeth (dmft), is 3-4 times higher in AI/AN preschoolers than the general population of U.S. children (3-5). Moreover, population-based studies reveal untreated dental decay increases with age among AI/AN children, with a 21% prevalence in 1-year-olds and 75% prevalence in 5-year olds (4). Advancing severity of oral disparities in reservation communities has become a major public health and policy issue.
General oral health outcome assessments indicate oral health beliefs and behaviors of American Indians (AI) differ compared to other U. S. ethnic/racial minority populations (World Health Organization International Collaborative Study of Oral Health Outcomes, ICS-II). For AI adults, barriers in accessing care and past negative dental experiences were associated with decreased likelihood of dental contact and worse perceived oral health status (6, 8). AI adults also reported lower frequencies of daily toothbrushing (7) and were more likely than other U.S. ethnic/racial minority populations to report total tooth loss (6). Beyond general surveys of AI adults, limited data are available related to determinants of oral health disparities for AI/AN children, including parental knowledge and behavior.
Oral health status of Alaska Native (AN) children was evaluated as part of an investigation involving Head Start children. Compared to other children, AN children experienced higher rates of ECC. Probability of developing dental caries was more than 4 times higher among AN than other non-AN children. Investigators attributed this disparity primarily to sociodemographic determinants and dietary patterns related to behavioral factors (9). In an oral health literacy study that included AI participants, caregivers’ oral health knowledge and behaviors and self-reported oral health status of their children were evaluated. Compared to whites and African Americans, AI caregivers were most likely to report poorer oral health status for their children, although parental oral health knowledge was not lower (10).
The complex interaction of poverty, health care system limitations, culture and ethnicity/race, and health behaviors affect oral health outcomes (11, 12). Accordingly, interest has grown in addressing oral health using a broader framework incorporating psychosocial and behavioral strategies (11, 13). The current study describes the first, essential step in developing such an approach for AI populations – identification of knowledge and behavior levels and associated factors. This community-based study is the first to examine and report outcomes for oral health knowledge and behavior in AI parents from the Northern Plains region. Study findings are being used to develop oral health messages and behavioral approaches for use within a manualized intervention intended to enhance parental oral health behaviors, with the ultimate goal of reducing dental caries prevalence in AI children.
Methods
To address oral health disparities among AI/ANs, the Center for Native Oral Health Research (CNOHR) at the University of Colorado Denver (UCD) is conducting multiple community-based clinical trials. This study is part of the community-based clinical trial “Promoting Behavior Change for Oral Health in American Indian Mothers and Children” (ClinicalTrials.gov NCT01116726), aimed at testing a multifaceted approach to reduce ECC disparities in AI children from a Northern Plains tribe. Data were collected as part of a pilot test to inform preparation for the larger clinical trial. Parental oral health knowledge and behavior were examined using cross-sectional data. To protect confidentiality of the participating community, a general description, rather than the tribal name will be referenced.
Study participants were at least 15 years of age, self-identified as AI, living on/near the reservation, and the parent/caregiver of a child under age 7 years. Recruitment posters were posted in locations across the reservation. A final sample of 147 participants represented a convenience sample (respondent compensation was $40/participant).
Institutional Review
The protocol was approved by the National Institute of Dental and Craniofacial Research (NIDCR), Colorado Multiple Institutional Review Board at UCD, and the participating tribe's Research Review Board. All participants provided written informed consent and Health Insurance Portability and Accountability Act authorization prior to participation. The tribal Research Review Board approved this article for publication.
Procedures
As community-based participatory research, the project began with input from the Community Advisory Board, consisting of 6 local service providers and health advocates. A careful process of community consultation involving the Community Advisory Board, community members, and focus group meetings was undertaken. This project built on previous research with the tribe and an existing strong relationship with the community.
Data Collection
During May-June, 2010, data were collected in 4 towns on/near the reservation at sites providing gathering areas for the general population (tribal colleges and community centers) and the project field office. Survey data were collected using an audio computer-assisted self-interviewing (ACASI) system. The ACASI system enabled survey delivery on a computer with simultaneous audio narration by a project staff member from the participating tribe. Participants could replay a given item, mute the audio, or remove their headphones. The ACASI data collection methods have been shown to improve reliability of reported health-related behaviors among other AI groups (14-16). Participants with more than one child were instructed to answer survey questions for only one child (age< 7years) for whom they were the parent/caregiver. The survey was programmed in SSI Web from Sawtooth Software (17) and implemented on encrypted Dell Inspiron Mini laptop computers. The ACASI system was determined to be an acceptable means of collecting survey data, with 93.5% participants reporting being comfortable using a computer to complete the survey.
Survey Development
Development of the oral health survey was a collaborative effort involving NIDCR-funded Oral Health Disparities Centers at UCD, Boston University, and University of California San Francisco. All items were specified, developed, and approved by a measure development workgroup comprised of investigators from NIDCR-funded Oral Health Disparities Centers. Survey items related to knowledge and behavior addressed 12 specific content areas that were incorporated into counseling messages for each Oral Health Disparities Centers’ clinical trials targeting ECC. Key messages were identified and guided development of survey questions focused on oral hygiene, diet, and preventive oral health concepts.
Sociodemographic Characteristics
Survey questions included parent/child gender and age, parental educational attainment/employment status, number of family members in the household, and household poverty status. Based on 2009 U.S. Department of Health and Human Services poverty guidelines (25), the ACASI program computed the specific poverty level for participants’ reported household size. To determine poverty status, participants were asked whether the combined income for all household family members was below the poverty level computed by ACASI. Participants could respond “Yes,” “No,” “Don't know,” or skip the question. In addition to sociodemographic data, utilization of dental care in the past year for a cavity or toothache not related to teething was assessed.
Parental Oral Health Knowledge
The survey included 3 sets of questions addressing parental oral health knowledge. Participants could respond, “Don't know” or skip any question they preferred not to answer. Responses were coded as correct or incorrect (“Don’t know” responses were identified as incorrect). Accuracy of responses was examined for individual knowledge items and a composite measure of parental oral health knowledge calculated as the percentage of 16 knowledge items answered correctly.
The first set of knowledge items asked parents to indicate whether each of 4 statements regarding oral health was true or false. A second set of items asked parents whether 8 specific behaviors were “good for your child's teeth, neither good nor bad for your child's teeth, or bad for your child's teeth.” To reduce the chance participants would respond similarly to all items, 2 distracter items were included (“Eating fresh vegetables” and “Eating meat”). A third set of 4 items assessed parents’ knowledge of important oral health recommendations: at what age can a child can begin brushing alone (age ≥6years); at what age should a child first have his/her teeth checked (age ≤1year); at what age should a child stop drinking from a baby bottle (age ≤1year); how many times a day should a child's teeth should be cleaned or brushed (≥2 times/day).
Parental Oral Health Behavior
Thirteen survey items addressed parental oral health behavior. For each item, responses were identified as “adherent” with current recommendations for good oral health care, as specified in oral health counseling messages developed for the collaborative oral health disparities centers. Parents’ responses to each behavioral item were examined and an overall behavior score computed, representing the percentage of 13 behaviors for which a parent reported adherence with standards of good oral health care. Analyses related to items addressing toothbrushing behavior were limited to children 1 year or older.
Convergent Validity Measures
Validity was assessed from the correlation of overall knowledge and behavior measures with parent education and the following constructs:
Parental Oral Health Locus of Control (LOC) – LOC represents a parent's beliefs regarding the source of control over their child's oral health status. Using items adapted from existing measures, (18, 19) the degree to which parents felt they controlled their child's oral health status (Internal LOC), that the dentist is in control (Powerful Others LOC), or their child's oral health is a matter of chance (Chance LOC) were examined.
Perceived barriers and benefits – Parents’ perceptions of barriers and benefits associated with recommended oral health behaviors were examined. Items were adapted from existing sources, (20, 21) or developed specifically to address the content of the study's counseling messages.
Parental dental self-efficacy – Self-efficacy represents an individual's confidence that he/she can engage in specific behaviors (22). Parents’ self-efficacy for recommended oral health behaviors was measured. Items were developed specifically to address the content of these messages or adapted from existing measures (23).
Child's oral health status – Using an item adapted from the National Survey of Children's Health, parents were asked to rate the health of their child's teeth and mouth on a scale from “Excellent” to “Poor,” with higher numbers representing better oral health (24).
Data Analysis
To assess validity, overall knowledge and behavior scores were correlated with convergent validity measures identified previously. Summary statistics regarding parent/child sociodemographics, oral health knowledge, and oral health behavior were computed. Mean overall knowledge and behavior scores were compared across participant demographic categories using analysis of variance (ANOVA). Additionally, the relationship between parent oral health knowledge and behavior was examined. Mean parent oral health knowledge score was compared across quartile groups of oral health behavior scores and mean parent oral health behavior score compared across quartile groups of oral health knowledge scores using ANOVA. Analyses were conducted in SAS version 9.3 (SAS Institute, Cary, NC).
Results
Table 1 presents descriptive information about the sample. Participants were primarily female (86%) and on average age 29 years (range 15-54 years). More than half the participants (61%) had a high school education or greater. The majority (67%) were unemployed and 51% reported living below the poverty line (37% declined to report income). Children were on average 2 years old, 95% were age 3 years or younger, with equal numbers of males and females. More than 12% of children had seen the dentist in the past year for care related to a cavity or toothache.
Table 1.
Parent/Caregiver and Child Characteristics (N=147)a
| Parent/Caregiver Characteristics | |
| Female (n, %) | 127 (86.4) |
| Age, years | |
| Mean (SD) | 28.6 (8.2) |
| Range | 15-54 |
| Education (n, %) | |
| Less than High School | 57 (39.0) |
| High School or GED | 34 (23.3) |
| More than High School | 55 (37.7) |
| Employment (n, %) | |
| Employed | 47 (33.3) |
| Unemployed | 94 (66.7) |
| Income (n, %) | |
| Above Poverty | 45 (30.6) |
| Below Poverty | 47 (32.0) |
| Income Not Known/Missing | 55 (37.4) |
| Child Characteristics | |
| Female (n, %) | 74 (50.3) |
| Age, years | |
| Mean (SD) | 2.1 (1.4) |
| Range | 0.02-6.6 |
| < 1 | 33 (25.4) |
| 1 to < 2 | 25 (19.2) |
| 2 to < 3 | 33 (25.4) |
| 3 to < 4 | 32 (24.6) |
| 4 or more | 8 (5.4) |
| Dental Care in Past Year for Cavity/Toothache (n, %) | 18 (12.3) |
Unless otherwise noted, results presented are N (%). Missing values have been excluded: education=0.7%, employment=4.1%, caregiver age=3.4%, child age= 11.6%.
Overall knowledge and behavior scores were significantly related to many of the convergent validity measures (Table 2). Parents with greater oral health knowledge had higher educational attainment, were less likely to indicate their child's oral health status was in the hands of the dentist or a matter of chance, perceived significantly greater benefit from engaging in recommended oral health behaviors, and reported greater confidence in their ability to do so. Parents who expressed greater confidence and those who perceived fewer barriers to recommended oral health behavior had better behavioral adherence scores. Engaging in more of the recommended oral health behaviors was associated with better pediatric oral health status.
Table 2.
Convergent Validity Analyses
| Knowledge Score | Behavior Score | |||
|---|---|---|---|---|
| Kendall's tau | p value | Kendall's tau | p value | |
| Internal Locus of Control | 0.086 | 0.172 | −0.014 | 0.814 |
| External Locus of Control – Chance | −0.165 | 0.009 | 0.082 | 0.168 |
| External Locus of Control – Powerful Others | −0.209 | <0.001 | 0.062 | 0.300 |
| Perceived Barriers | −0.059 | 0.333 | −0.250 | <0.001 |
| Perceived Benefits | 0.137 | 0.028 | 0.035 | 0.561 |
| Self-Efficacy | 0.210 | <0.001 | 0.306 | <0.001 |
| Parent/Guardian Education | 0.243 | <0.001 | −0.069 | 0.250 |
| Child's Oral Health Status (Parent Rated) | 0.063 | 0.346 | 0.174 | 0.006 |
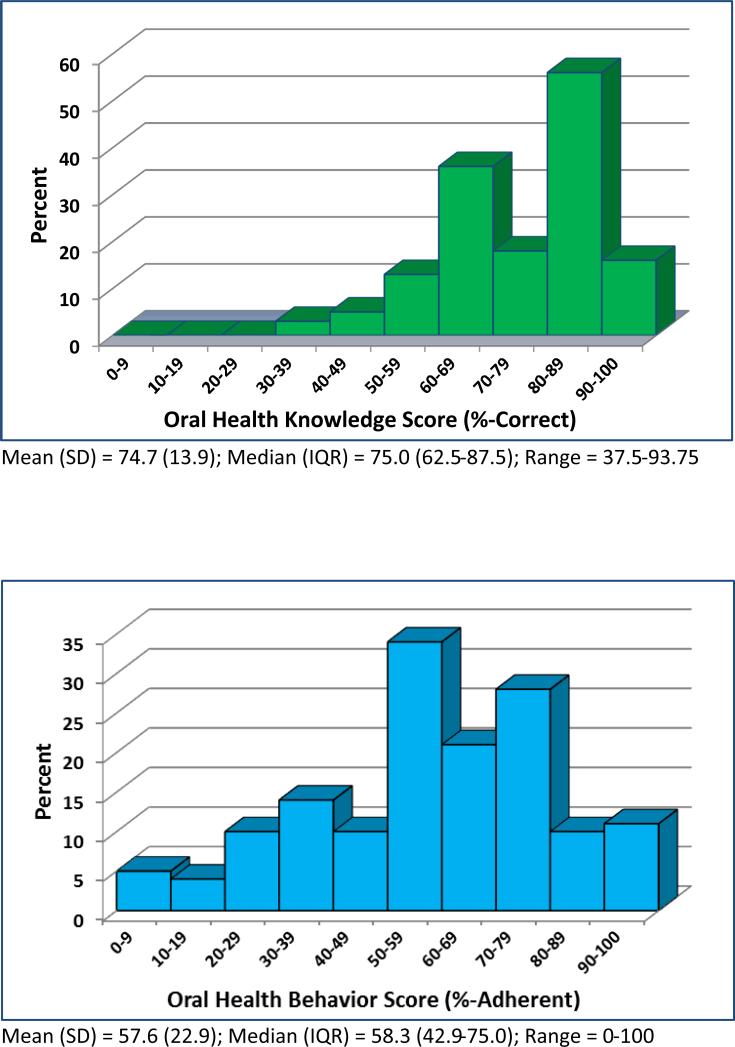
The overall oral health knowledge mean score was 75% (range 38-94%; Figure 1). Eighty-six percent of parents answered the majority of questions (>50 percent) correctly (Table 3). Accuracy was more limited for certain items. Approximately half the parents knew “drinking milk from a sippy cup at bedtime is bad for a child's teeth,” “eating something after brushing teeth but before going to bed is bad for a child's teeth,” and “eating chips is bad for a child's teeth.” Few parents knew the correct age at which a child can brush without adult involvement, with a high majority indicating very young children (ages 1-3 years) do not need assistance with toothbrushing.
Figure 1.
Distribution of Overall Knowledgeand Overall Behavior
Table 3.
Parental Oral Health Knowledgea
| Knowledge Item | Answered Correctly, N(%) |
|---|---|
| A child's teeth should be brushed or cleaned at least twice a day. | 139 (95.2) |
| There's no need to go to the dentist unless children have a problem with their teeth. | 139 (94.6) |
| Sharing a toothbrush with your child is bad for a child's teeth. | 138 (93.9) |
| A child should stop drinking from a baby bottle at one year of age or younger. | 135 (91.8) |
| Cavities are caused by germs in the mouth. | 131 (90.3) |
| A parent checking their child's teeth every month for changes or spots is good for a child's teeth. | 131 (89.7) |
| Drinking soda is bad for a child's teeth. | 131 (89.7) |
| Because they do not stay in your child's mouth very long, baby teeth are not that important. | 130 (88.4) |
| It is best to use toothpaste with fluoride when brushing a child's teeth. | 119 (81.5) |
| Getting fluoride varnish put on your child's teeth is good for the child's teeth. | 115 (79.3) |
| A child should first have his/her teeth checked by a dentist or doctor at age one year or younger. | 108 (74.0) |
| Using the same spoon to taste the food and feed the child is bad for a child's teeth. | 107 (73.8) |
| Drinking milk from a sippy cup at bedtime is bad for a child's teeth. | 82 (56.2) |
| Eating something after brushing teeth but before going to bed is bad for a child's teeth. | 77 (52.7) |
| Eating chips is bad for a child's teeth. | 72 (49.0) |
| A child can brush his/her teeth by himself/herself at age six or older. | 3 (2.1) |
Items are presented in order based on the percentage of participants answering correctly. Missing values were excluded; no more than 2% for any statement.
Parents scored considerably lower on the oral health behavior questions (Table 4). Wide variation was observed in the overall behavior score, with adherence only 58%, on average, for recommended behaviors (range 0-100%; Figure 1). For only 6 of 13 behavior questions did 50% or more of parents indicate adherence with recommended oral health behaviors. Parents were particularly likely to report poor bedtime oral health behavior. Forty-six percent of parents reported their child only drinking water from a bottle or sippy cup at bedtime, 33% reported always brushing or wiping their child's teeth at bedtime, and 27% reported their child did not eat or drink anything other than water after brushing and before going to bed. Children ate sugary foods frequently, with 50% of children drinking sweet or sugary drinks less than once/day and 48% eating sweet or sugary foods less than once/day. Less than one-third of parents reported checking their child's teeth once/month for spots or problems and helping their child with brushing. Fifty percent of parents reported their child's teeth were brushed twice/day and 21% reported less than once/day. In contrast, 67% of parents reported brushing their own teeth twice/day or more.
Table 4.
Parental Oral Health Behaviora
| Recommended Behavior | Adherent, N (%) |
|---|---|
| The child stopped drinking from a bottle at age one or younger.b | 74 (85.1) |
| Child age one or older does not drink from a bottle. | 113 (76.9) |
| When the child's teeth are brushed, fluoride toothpaste is usually used.c | 69 (74.2) |
| Parent brushes his/her own teeth twice a day or more. | 98 (66.7) |
| Child does not put anything in his/her mouth that has just been in someone else's mouth. | 81 (55.1) |
| Child's teeth are brushed twice a day or more.d | 48 (50.0) |
| Child drinks sweet or sugary drinks less than once a day. | 73 (49.7) |
| Child eats sweet or sugary foods less than once a day. | 70 (47.6) |
| On a typical day, the child does not drink anything other than water from a bottle or a sippy cup at bedtime or naptime. | 68 (46.3) |
| In the past week, the child's teeth were brushed or wiped just before going to bed every night. | 48 (32.7) |
| In the past six months, the parent checked the child's teeth and gums for spots or problems six or more times. | 46 (31.3) |
| Parent or another adult always helps the child brush his or her teeth (for children under six years of age).c | 29 (31.2) |
| In the past week, the child never ate or drank something other than water after brushing and before going to sleep.c | 25 (26.9) |
Items are presented in order based on the percentage of participants indicating adherence with the recommended oral health behavior.
Limited to children who no longer drink from a bottle (N=87).
Limited to parents of children age one or older whose teeth were brushed within the past week (N=93).
Limited to parents of children age one or older (N=96).
Gender, education, income, and behavior scores were significantly associated with mean knowledge score, although utilization of dental care in the prior year was not (Table 5). Females averaged 10 points higher than males, and greater education was associated with an increasing mean knowledge score (p<0.01). Behavior score, broken by quartile, was positively associated with knowledge score. The lowest behavior score quartile had a mean accuracy rate of 68% for knowledge items versus the highest behavior score quartile with a mean knowledge accuracy rate of 77% (p=0.01). Conversely, the lowest knowledge score quartile had a mean behavior score of 48% versus the highest knowledge score quartile, which had a mean behavior score of 61% (p=0.01). Results suggest parents with stronger knowledge engaged in 61% of recommended oral heath behaviors, whereas those in the lowest knowledge quartile adhered to 48% of recommended behaviors. No parent sociodemographics were significantly associated with behavior score.
Table 5.
Mean Knowledge and Behavior Scores by Caregiver Demographics
| Knowledge Score Mean (SD) | ANOVA P-value | Behavior Score Mean (SD) | ANOVA P-value | |
|---|---|---|---|---|
| Gender | 0.003 | 0.122 | ||
| Male | 66.3 (14.8) | 50.2 (27.5) | ||
| Female | 76.0 (13.3) | 58.8 (22.0) | ||
| Education | <0.001 | 0.109 | ||
| Less than High School | 69.6 (15.6) | 59.0 (21.6) | ||
| High School or GED | 76.1 (11.6) | 62.7 (27.0) | ||
| More than High School | 79.2 (11.8) | 52.7 (21.1) | ||
| Employment | 0.227 | 0.705 | ||
| Employed | 77.1 (11.9) | 57.2 (20.2) | ||
| Unemployed | 74.2 (14.2) | 58.7 (23.9) | ||
| Income | 0.004 | 0.917 | ||
| Above Poverty | 78.8 (10.5) | 56.4 (22.5) | ||
| Below Poverty | 76.3 (11.3) | 58.1 (21.9) | ||
| Don't Know/Missing | 70.0 (16.9) | 58.2 (24.4) | ||
| Dental Care in Past Year for Cavity/Toothache | 0.527 | 0.689 | ||
| Yes | 76.7 (12.6) | 55.7 (19.0) | ||
| No | 74.5 (14.1) | 58.1 (23.4) | ||
| Behavior Score | 0.016 | |||
| Quartile 1 (0-41.7) | 68.2 (15.3) | . | ||
| Quartile 2 (42.9-57.1) | 76.0 (14.5) | . | ||
| Quartile 3 (58.3-75.0) | 77.0 (11.4) | . | ||
| Quartile 4 (76.9-100) | 77.2 (13.3) | . | ||
| Knowledge Score | 0.011 | |||
| Quartile 1 (37.5-62.5) | . | 47.5 (23.4) | ||
| Quartile 2 (68.8-75.0) | . | 58.6 (24.2) | ||
| Quartile 3 (81.3-81.3) | . | 64.6 (20.5) | ||
| Quartile 4 (87.5-93.8) | . | 60.6 (20.7) |
Discussion
The Northern Plains is one of the largest, most rural, and impoverished tribal regions. The AI population of 30,000 is dispersed over 2.8 million acres (25-28). Major access barriers include distance, extreme weather conditions, lack of paved roads, inconsistent access to a private car, and absence of public transportation, with walking and hitchhiking common. Access to dental services is further impacted by insufficient numbers of dental providers and clinics. Median age for the region is 24 years (27). Substantive economic disadvantage was reflected by study findings with a poverty rate 4 times higher than the general population and 2 times higher than other AI populations (27). Educational attainment was limited, with fewer participants completing at least a high school education compared to the general population and other AI subsets (27, 28). Results supported validity of oral health knowledge and behavior measures used in the study, indicating overall knowledge and behavior scores were associated with demographic and psychosocial measures in meaningful ways. Poverty and educational status were significantly associated with oral health knowledge, as reflected by participants with greater education and income demonstrating higher oral health knowledge. In addition, gender was positively associated with oral health knowledge, with females scoring higher. Stronger oral health knowledge for female participants may be due to AI/AN women's identities being closely tied to their role as mothers and caregivers (29). Oral health behavior was not associated with parental sociodemographics .Specific weaknesses in oral health knowledge were noted. Almost half the parents were not aware young children should not drink milk from a sippy cup at bedtime and not eat after brushing at bedtime. Knowledge was least accurate regarding the age at which children are capable of brushing without adult assistance. Virtually all parents indicated very young children (age< 3years) can brush their own teeth.
Behavioral adherence scores were notably lower than knowledge scores, with almost half the parents not engaging in standard recommendations. Behavioral compliance was specifically weaker related to parental adherence with recommendations regarding children's oral health habits at bedtime. Almost half the parents indicated their child drank something other than water from a bottle or sippy cup at bedtime. Only one-third reported their child's teeth were brushed before bed each night and only 27% reported their child did not eat or drink anything other than water after brushing at bedtime. Oral hygiene behavior was low, with a high majority of parents not always helping their child brush and half not brushing their child's teeth twice/day. About one-quarter of parents did not report using fluoride toothpaste when brushing their child's teeth, with one-third not brushing their own teeth at least twice/day. However, self-brushing was higher compared to brushing their child's teeth. These behaviors were inconsistent with knowledge responses by parents, virtually all of whom indicated a child's teeth should be brushed at least twice/day and most of whom indicated it is optimal to use fluoride toothpaste. Wide discrepancy in oral hygiene behaviors and knowledge merits further investigation to gain insight about possible contributors.
The majority of parents did not limit sugary drinks and foods, although half understood carbonated beverages are bad for teeth. Past evidence suggests mothers of caries-active children understand the relationship between diet and dental caries, but avoid restricting their children's diet to quiet and please their children and manage children's sleeping problems (30). In the current study, parents demonstrated weaker knowledge and lack of adherence with a range of oral health recommendations. However, the strongest relationship between knowledge and behavior was related to discontinuing use of a baby bottle by age 1 or younger. Compared to other responses, there was better consistency between these items, meriting further investigation about possible influences.
Current study findings were comparable to other Indigenous groups. ECC prevalence for Indigenous Canadian children (First Nations, Inuit and Métis) exceeds 90% in some communities(31). Poor oral health status for Indigenous Canadian children was associated with limitations in parental knowledge regarding bedtime bottle use, decreased adherence in weaning from a bottle, and not maintaining regular dental visits for their child(31,32). Less adherent preventive behavior was associated with parental perceptions that deciduous teeth are not important, and accepting ECC and dental surgery as inevitable. Increased access to dental care was associated with maternal post-secondary education(31,32).
There are no data in the literature on oral health knowledge and behavior in AI/AN populations. In order to address vast oral health disparities in this population, it is critical that researchers and practitioners understand limitations in knowledge and behavior. This study is important in identifying areas in which AI caregivers have strong knowledge of recommended oral health practices but are deficient in implementation, and areas where AI caregivers are lacking basic knowledge. Determining strengths and limitations will enable targeted interventions focused on changing behavior as opposed to solely improving knowledge.
This study is the first to examine and report outcomes for oral health knowledge and behavior in AI parents from the Northern Plains region. Survey information was collected as part of the larger study in which a cognitive-behavioral intervention for pregnant women and mothers will be evaluated for effectiveness in reducing ECC. As an initial pilot project, the current sample size was relatively small. Parents may have provided biased responses reflecting what they believed to be socially acceptable answers. Some degree of honest reporting was also suggested in comparing parents’ knowledge and behavioral adherence for a similar oral health concept. For example, virtually all parents correctly indicated children's teeth should be brushed twice/day, yet, only half reported their child's teeth were brushed twice/day. A high majority of parents’ correctly indicated drinking soda was bad for children's teeth, yet less than half reported limiting sweet or sugary drinks to less than once/day. Overall, results confirmed stronger knowledge did not consistently translate to greater adherence with recommended oral health behaviors among AI parents. Parents who expressed greater confidence and those who perceived fewer barriers to recommended oral health behavior had better behavioral adherence scores. These findings should be considered in design of future interventions and programs for dental caries prevention in AI/AN populations. Strategies focused on behavior change, rather than knowledge alone, may be most likely to affect oral health outcomes for AI/AN children.
Acknowledgements
Funding for the study was provided by the National Institute for Dental and Craniofacial Research (U54 DE019259-03, Albino).
References
- 1.United States Department of Health and Human Services Indian Health Service The 1999 Oral Health Survey of American Indian and Alaska Native Dental Patients: USDHHS. 2002 [Google Scholar]
- 2.Dental, Oral, and Craniofacial Data Resource Center [September 13, 2012];National Health and Nutrition Examination Survey 1999-2002. http://www.drc.gov.
- 3.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, Eke PI, Beltrán-Aguilar ED, Horowitz AM, Li CH. Trends in oral health status: United States, 1988–1994 and 1999–2004. National Center for Health Statistics. Vital Health Stat 11. 2007;248:1–92. [PubMed] [Google Scholar]
- 4.Phipps KR, Ricks TL, Manz MC, Blahut P. Prevalence and severity of dental caries among American Indian and Alaskan Native preschool children. J Public Health Dent. 2012;72:208–15. doi: 10.1111/j.1752-7325.2012.00331.x. [DOI] [PubMed] [Google Scholar]
- 5.Jones DB, Schlife CM, Phipps KR. An oral health survey of Head Start children in Alaska: oral health status, treatment needs, and cost of treatment. J Public Health Dent. 1992;52:86–93. doi: 10.1111/j.1752-7325.1992.tb02249.x. [DOI] [PubMed] [Google Scholar]
- 6.Davidson PL, Anderson RM, Marcus M, Atchison KA, Reifel N, Nakazono T, Rana H. Indicators of oral health in diverse ethnic and age groups: findings from the International Collaborative Study of Oral Health Outcomes (ICS-II) USA research locations. J Med Syst. 1996;20:295–316. doi: 10.1007/BF02257042. [DOI] [PubMed] [Google Scholar]
- 7.Davidson PL, Anderson RM. Determinants of dental care utilization for diverse ethnic and age groups. Adv Dent Res. 1997;11:254–62. doi: 10.1177/08959374970110020801. [DOI] [PubMed] [Google Scholar]
- 8.Davidson PL, Rams TE, Andersen RM. Socio-behavioral determinants of oral hygiene practices among USA ethnic and age groups. Adv Dent Res. 1997;11:245–53. doi: 10.1177/08959374970110020701. [DOI] [PubMed] [Google Scholar]
- 9.Jones DB, Schlife CM, Phipps KR. An oral health survey of Head Start children in Alaska: oral health status, treatment needs, and cost of treatment. Journal of Public Health Dentistry. 1992;52:86–93. doi: 10.1111/j.1752-7325.1992.tb02249.x. [DOI] [PubMed] [Google Scholar]
- 10.Vann WF, Jr, Lee JY, Baker D, Divaris K. Oral health literacy among female caregivers: impact on the oral health outcomes in early childhood. J Dent Res. 2010;89:1395–400. doi: 10.1177/0022034510379601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader M-J, Bramlett MD, Newacheck PW. Influences on children's oral health: a conceptual model. Pediatrics. 2007;120:e510–18. doi: 10.1542/peds.2006-3084. [DOI] [PubMed] [Google Scholar]
- 12.Finlayson TL, Siefert K, Ismail AI, Delva J, Woosung S. Reliability and validity of brief measures of oral health-related knowledge, fatalism, and self-efficacy in mothers of African American Children. Pediatr Dent. 2005;27:422–28. [PMC free article] [PubMed] [Google Scholar]
- 13.Resnicow K, DiIorio C, Soet JE, Ernst D, Borrelli B, Hecht J. Motivational interviewing in health promotion: it sounds like something is changing. Health Psychol. 2002;21:444–51. [PubMed] [Google Scholar]
- 14.Edwards SL, Slattery ML, Murtaugh MA, Edwards RL, Bryner J, Pearson M, Rogers A, Edwards AM, Tom-Orme L. Development and use of touch-screen audio computer-assisted self-interviewing in a study of American Indians. Am J Epidemiol. 2007;165:1336–42. doi: 10.1093/aje/kwm019. [DOI] [PubMed] [Google Scholar]
- 15.Krawczyk CS, Gardner LI, Wang J, Sadek R, Loughlin AM, Anderson-Mahoney P, Metsch L, Green S, Antiretroviral Treatment and Assessment Study Group Test-retest reliability of a complex human immunodeficiency virus research questionnaire administered by an Audio Computer-assisted Self-interviewing system. Med Care. 2003 Jul;41(7):853–8. doi: 10.1097/00005650-200307000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Waruru AK, Nduati R, Tylleskar T. Audio computer-assisted self-interviewing (ACASI) may avert socially desirable responses about infant feeding in the context of HIV. BMC Medical Informatics & Decision Making. 2005;5:24. doi: 10.1186/1472-6947-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sawtooth Software What is SSI Web? http://www.sawtoothsoftware.com/products/ssiweb/
- 18.Lencova E, Pikhart H, Broukal Z, Tsakos G. Relationship between parental locus of control and caries experience in preschool children - cross-sectional survey. BMC Public Health. 2008;8:208. doi: 10.1186/1471-2458-8-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carnahan TM. The development and validation of the Multidimensional Dental Locus of Control Scales. State University of New York; Buffalo, NY: 1980. [Google Scholar]
- 20.Nakazono TT, Davidson PL, Andersen RM. Oral health beliefs in diverse populations. Adv Dent Res. 1997 May;11(2):235–44. doi: 10.1177/08959374970110020601. [DOI] [PubMed] [Google Scholar]
- 21.Riley JL, 3rd, Gilbert GH, Heft MW. Dental attitudes: proximal basis for oral health disparities in adults. Community Dent Oral Epidemiol. 2006 Aug;34(4):289–98. doi: 10.1111/j.1600-0528.2006.00280.x. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 23.Litt MD, Reisine S, Tinanoff N. Multidimensional causal model of dental caries development in low-income preschool children. Public Health Rep. 1995 Sep-Oct;110(5):607–17. [PMC free article] [PubMed] [Google Scholar]
- 24.National Survey of Children's Health [February 21, 2013];Child and Adolescent Health Measurement Initiative, Data Resource Center on Child and Adolescent Health. 2007 website http://childhealthdata.org/learn/topics_questions/2007-nsch?itemid=K2Q01_D.
- 25.U.S. Department of Health and Human Services Federal Register. 2009 Jan 23;74(14) [Google Scholar]
- 26.Pickering K. Pine Ridge workforce study. Wawokiye Business Institute; Kyle, South Dakota: Jul, 2005. [Google Scholar]
- 27.United States Department of Commerce Bureau of the Census [July 27, 2013]; http://factfinder2.census.gov.
- 28.United States Department of Commerce Bureau of the Census . We the people: American Indians and Alaska Natives in the United States. US Department of Commerce Census Bureau; Washington, DC: 2006. [Google Scholar]
- 29.Bruerd B, Kinney MB, Bothwell E. Preventing baby bottle tooth decay in American Indian and Alaska Native communities: a model for planning. Public Health Rep. 1989;104:631–40. [PMC free article] [PubMed] [Google Scholar]
- 30.Volschan BCG. Getting to know the early child caries through qualitative analysis. Pediatr Dent. 2006;31:48–51. doi: 10.17796/jcpd.31.1.q772mm1503413835. [DOI] [PubMed] [Google Scholar]
- 31.Peressini S, Schroth RJ, Harrison RL, Lawrence HP, Peressini S. Forum Proceedings. Winnipeg; Jun 7 to 8, 2008. [July 16, 2013]. Using qualitative research methodology to aid in our understanding of children's oral health: An example from Manitoulin Island. Oral Health and the Aboriginal Child: A Forum for Community Members, Researchers and Policy-makers. www.mich.ca/files/docs/Conference Proceedings.pdf. [Google Scholar]
- 32.Assembly of First Nations, First Nations Information Governance Committee First Nations Regional Longitudinal Health Survey (RHS) 2002/03: Results for Adults, Youth and Children Living in First Nation Communities. The health needs of First Nations children: Dental treatment needs and use of dental services. 2nd edn. Assembly of First Nations; Ottawa: 2007. [July 16, 2013]. pp. 278–86. Chapter 32 www.rhs-ers.ca/sites/default/files/ENpdf/RHS_2002/rhs2002-03-technical_report.pdf. [Google Scholar]