Abstract
Practice-based research networks bring together academic researchers and primary care clinicians to conduct research that improves health outcomes in real-world settings. The Washington, Wyoming, Alaska, Montana, and Idaho region Practice and Research Network implemented a health data-sharing infrastructure across 9 clinics in 3 primary care organizations. Following implementation, we identified challenges and solutions. Challenges included working with diverse primary care organizations, adoption of health information data-sharing technology in a rapidly changing local and national landscape, and limited resources for implementation. Overarching solutions included working with a multidisciplinary academic implementation team, maintaining flexibility, and starting with an established network for primary care organizations. Approaches outlined may generalize to similar initiatives and facilitate adoption of health data sharing in other practice-based research networks.
Keywords: data sharing, electronic health records, health information technology, primary care
PRACTICE-BASED RESEARCH NETWORKS (PBRNs) bring together academic researchers and primary care clinicians to conduct research that improves quality of care and health outcomes in real-world settings (Brown & Pavlik, 2013; Calmbach et al., 2012; Green & Dovey, 2001; Hartung et al., 2012). With 42.5% (Hsaio et al., 2013) of primary care physicians in 2012 using electronic health record (EHR) systems and new funding programs offering support for innovative ways to leverage EHR data for research and quality improvement (Agency for Healthcare Research and Quality, n.d.), the development of health data-sharing architectures within PBRNs is a natural extension of the PBRN research infrastructure. Researchers have identified technical challenges and suggest approaches to address challenges inherent in developing these data-sharing infrastructures (Delaney et al., 2012; Mold et al., 2012; Pace & Staton, 2005; Pace et al., 2009; Peterson et al., 2012;). However, nontechnical implementation barriers are less well understood, especially when data sharing is implemented across independent practices with disparate EHR systems.
The Washington, Wyoming, Alaska, Montana, and Idaho region Practice and Research Network (WPRN) recently implemented a health data-sharing infrastructure called “Data QUEST” (Stephens et al., 2012) in 9 clinics that are part of 3 diverse primary care organizations, with 3 separate EHR systems using 2 vendor-based EHRs (Allscripts and Centricity). We describe key nontechnical challenges that the academic implementation team encountered during this project. We aim to describe approaches that can be used to effectively address these challenges. These challenges may be common across similar PBRN data-sharing efforts, regardless of EHRs or geographic location. The solutions we developed may generalize to groups undertaking similar work, providing guidance to facilitate widespread adoption of health data sharing.
Methods
Data QUEST infrastructure
We developed Data QUEST using a participatory approach that incorporated input from organization partners and the academic implementation team. Data QUEST is an infrastructure (Figure) that facilitates sharing of EHR data across diverse primary care organizations within the WPRN, our regional PBRN. This federated data-sharing infrastructure was designed to meet the governance requests of our primary care organization partners to maintain local ownership and control of identified EHR data (Stephens et al., 2012). The architectural design for Data QUEST included storing the extracted EHR data in local repositories, behind a firewall at each organizational site. We worked with a commercial vendor, carefully selected for its expertise in working with disparate EHRs (Lin et al., 2010), to establish the physical servers at each site and map and extract the EHR data in a semantically aligned format across our different partner organizations. The federated system, combined with semantic alignment, allows combining of data across sites, while meeting compliance for Health Insurance Portability and Accountability Act and Institutional Review Board regulations as appropriate. Data QUEST achieved semantic alignment by storing data in identical data models and mapping codified data using the same coding schemes (ie, International Classification of Diseases, Ninth Revision-[ICD-9] codes, National Drug Code—NDC, proprietary laboratory and history codes, Current Procedural Terminology codes—CPT, etc). We targeted extraction from several main data domains in the EHRs, including demographic, visit, laboratory, diagnosis, problem, procedure, medication, medical/surgical/family history, and immunization data. Data QUEST's storage of data in repositories separate from the EHR allows us to query data easily, without being dependent on EHR vendor-based data-querying tools and without utilizing partner organization staff. The vendor monitors data quality. The WPRN Coordinating Center assesses data quality as it uses the data for research, identifying and addressing data quality issues with the organization partners and vendor as they arise. Data QUEST currently includes data codified within the primary-care based EHR, with plans for expansion to other data domains (eg, claims, patient-reported outcomes, hospital-based and specialty care–generated data). In addition to supporting data sharing, Data QUEST provides clinical tools for quality improvement to participating organizations including a point of care report and clinical registry system.
Figure.
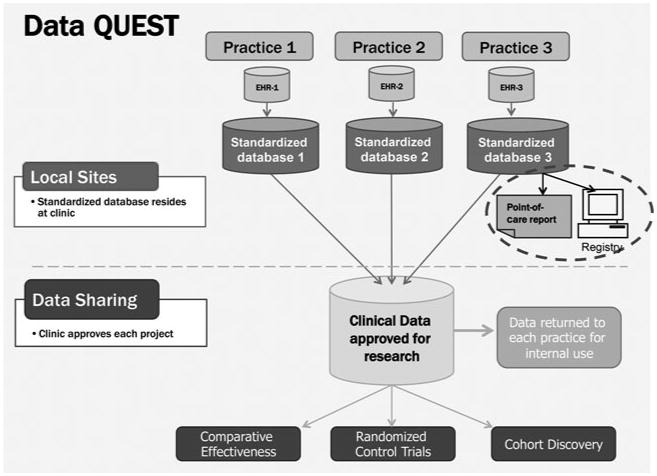
Data QUEST schematic. EHR indicates electronic health record.
Data QUEST extraction process
Partner organizations maintain ownership of the data and review and determine approval for all data requests. The vendor maintains remote access to the data repositories, governed by a business associate agreement with the partner organizations, and performs data extractions as needed for research purposes. All data queries and extractions are governed by data use agreements and data transfer agreements. The types and quantities of data shared between organization partners and researchers are determined on a project-by-project basis. Data extraction and acquisition costs are generally covered by project grants from academic investigators. For each funded project, the WPRN Coordinating Center collaborates with academic investigators to review projects, create data extraction specifications and data use agreements, develop budgets for the work, and facilitate transfer of de-identified data for research purposes.
Data QUEST implementation evaluation
The Data QUEST academic implementation team includes biomedical informaticists, primary care physicians, and WPRN coordinators (Lin et al., 2010; Stephens et al., 2012). Following implementation of Data QUEST, members of the academic implementation team conducted 3 debriefing sessions to evaluate materials related to implementation and document nontechnical challenges and solutions. Team members participating in the debriefing sessions carefully reviewed implementation processes and identified challenges and solutions by consensus. Academic implementation team members pinpointed specific solutions addressing each challenge, with an eye toward identifying solutions that could be generalized to other PBRN data-sharing efforts.
Results
We identified 3 overarching challenges in implementing Data QUEST. The Table outlines the key challenges we identified and the innovative approaches we created to address these challenges. First, we worked with a diverse group of independently owned primary care organizations, each with unique administrative and health information technology infrastructures and vendors. Second, the rapidly changing health care landscape required organizations to adapt quickly and frequently, impacting data availability and structures in EHR systems, staff/personnel availability, and workflow. Third, given limited resources to implement this project, we needed to find solutions that optimized those resources without placing undue burden on participating organizations.
Table. Innovative Approaches to Address Key Nontechnical Challenges During Implementation of Data QUEST.
| Key Challenge | Innovative Approaches |
|---|---|
| Diversity of organizations | Conducted feasibility evaluation that led to selecting a technical solution with clinical tools that added value for partner organizations |
| Engaged IT, clinical and operational stakeholders at each partner organization | |
| Individualized implementation process at each partner organization allowed implementation to fit existing infrastructure and resources | |
| Staggered implementation across partner organizations | |
| Engaged a vendor with experience, creating data-sharing infrastructures across diverse EHR systems | |
| Rapidly changing health care landscape | Used a nimble implementation process, allowing continuous contact with partner organizations and rapid response to changes |
| Conducted frequent site visits before, during, and after implementation to conduct direct observation and offer feedback | |
| Maintained flexibility in how and when clinical tools were implemented | |
| Limited resources | Received critical support from the Institute of Translational Health Sciences, our local Clinical Translational Sciences Award |
| Worked with commercial vendor to provide technical solution and support rather than relying on partner organizations' information technology resources | |
| Relied on a project coordinator to interface between the commercial vendor and the practice in order to lessen the burden of implementation for clinics |
Abbreviation: EHR, electronic health record.
Diversity of organizations
Harmonizing disparate EHRs was a clear challenge. In addition, each organization had its own set of workflows and personnel with varying roles and responsibilities in regard to data management for the EHR and concerns about data governance and privacy issues. As we developed Data QUEST, we conducted a thorough feasibility evaluation of 10 primary care organizations in the region to identify potential partner organizations and to assess the feasibility and barriers to developing a data-sharing infrastructure (Lin et al., 2010). We found that organizations were enthusiastic about data sharing, especially if the infrastructure created additional tools for clinical care and quality improvement. We used input from these site visits to define the Data QUEST technical infrastructure and recruited the top pilot partner organizations on the basis of initial capacity and readiness to implement Data QUEST.
A highly individualized implementation process was needed to address the diversity across organizations. We used a sequential implementation process, adding new sites over the course of 2 years, allowing us to meet the needs of the sites and balance the resource constraints of the academic implementation team. Implementation at each site included meetings with organization-based clinicians and leaders to orient them to the data-sharing infrastructure, highlighting motivations for data sharing and addressing concerns about organization impact. Following implementation, we conducted in-person site visits to assess implementation and address any technical, governance, and clinical issues. The WPRN Coordinating Center facilitated all aspects of the implementation process with each partner site including the relationship between the site and the Data QUEST vendor, tailoring the process to each partner organization's specific needs.
Rapidly changing health care landscape
During implementation of Data QUEST, we found that organizations and their health information technology systems underwent constant change, including creation of new EHR templates altering data flows, system upgrades, deployment and adoption of new EHR systems, IT staff shortages, shifting organizational priorities, and merging of local health systems, leading to organization leadership turnover. In addition, health care reform required adaptations, such as addressing incentives for achieving the Centers for Medicare & Medicaid Services Incentive Programs' “meaningful use” of EHRs, which influenced clinic initiatives and programs. At times, these real-world disruptions required organizations to focus resources toward clinical and business priorities and away from research efforts at times. A nimble implementation process was needed to address this rapidly changing environment. The presence of a dedicated project coordinator on the academic implementation team facilitated the implementation process, allowing continuous contact with the partner organizations and the ability for the team to respond quickly to changes. The implementation process also allowed flexibility in how and when clinical tools were deployed to minimize disruption to ongoing clinical care and to accommodate changes in EHR systems and clinic priorities. Partner organizations decided when and how to implement clinical tools associated with Data QUEST, and timelines were shifted as needed to minimize interference with business and clinical priorities. Site visits in various phases of implementation allowed us to conduct direct observations and offer feedback and lessons learned from other sites. Finally, ongoing communication ensured accurate information. Each partner organization identified an on-site project champion to facilitate communication and implementation.
Limited resources
Funding a data-sharing infrastructure for PBRNs is an ongoing challenge. The University of Washington's Institute of Translational Health Sciences, funded by the National Institutes of Health Clinical Translational Science Award program, provided pilot funding critical to building this innovative clinical and research resource. This funding supported the academic implementation team's time and the start-up vendor costs for this infrastructure. With this support in place, the academic implementation team was able to maintain flexibility and develop solutions to minimize the burden on the partner organizations. The organizations themselves had very limited resources to engage in data-sharing efforts; thus, identifying incentives to provide participating organizations with a viable return on investment case was important. Partner organizations were particularly interested in the addition of tools for clinical care and aligning health data-sharing efforts with meaningful use criteria.
The implementation process had to accommodate this resource-challenged environment. The vendor-based technical solution minimized reliance on participating organizations' IT staff and tools. Prior to implementation, we outlined concrete timelines and detailed resource impacts at each organization to clarify expectations. The academic implementation team worked as a liaison interfacing between the vendor and the organizations to minimize impact on the partner organizations.
Summary
Our multidisciplinary academic implementation team helped us maintain flexibility and respond nimbly to challenges, both critical strategies to successful implementation of an electronic health data-sharing infrastructure across diverse primary care organizations. These strategies were achievable because of the trust and the highly collaborative relationship that the WPRN's clinical organizations have with the WPRN Coordinating Center. This trust permitted us freedom during the project to make decisions efficiently. We were able to adjust timelines to accommodate the complicated scheduling encountered when working with geographically disparate and busy organizations and an off-site vendor and make adjustments to the governance and the technical architecture to respond to new situations.
Another key factor to the successful implementation of Data QUEST in diverse organizations has been a multidisciplinary effort informed by the partner organizations and the experience of national partners. The Institute of Translational Health Sciences provided crucial financial support, dedicated staff support, and technical expertise that allowed for implementation with flexibility and nimbleness that would not be afforded by disease-oriented research grants focused on specific clinical questions. This support minimized organizational burden for partner organizations. With initial Data QUEST implementation completed, more traditional research funding mechanisms can now be used to expand this data-sharing infrastructure.
Research projects and PBRNs developing data-sharing infrastructure across diverse organizations locally, regionally, and nationally are likely to face similar challenges to those described here. The academic implementation team's commitment to an iterative process led to many of the solutions described. The feasibility and technical evaluations allowed us to select resilient organizational partners that would participate in the iterative process and join an innovative venture that we plan to expand as more funds and projects are identified to support these efforts. Beginning with a small set of organizational partners allowed us to hone our process for deployment, providing a framework for scalability to future sites.
There is growing national interest in building EHR data-sharing infrastructures to be used for research, as evidenced by increased funding opportunities (Agency for Healthcare Research and Quality, n.d.; Stephen et al., 2010). Yet, best practices for developing these data-sharing networks are not well understood. DeVoe et al. (2012) reported on developing the OCHIN SafetyNet West Practice-Based Research Network (Patient-Centered Outcomes Research Institute, n.d.) and identified challenges in governance of data infrastructure and engaging busy clinicians. Although these are similar to our identified challenges, we had the additional challenge of implementing our infrastructure across practices with disparate EHR systems. Our federated system that allows organizations to maintain their data within their own protected environments may provide an important model for undertaking work with disparate primary care organizations with disparate EHR systems. The DARTNet Institute is a similarly federated national network of organizations sharing EHR, claims, and administrative data (Pace et al., 2009) DARTNet Institute served as an important resource during development and implementation of Data QUEST, and our partnership with DARTNet Institute has allowed us to explore data sharing on a larger scale. Partnering with existing national data-sharing efforts provided important information on existing strategies, vendors, and practices, and aligning efforts with existing networks will likely promote success for any PBRN-based data-sharing effort.
A continuing challenge is funding for the infrastructure and operations costs of implementing and maintaining data-sharing architecture. The Institute of Translational Health Sciences, with its commitment to developing tools that speed translation of discoveries into clinical practice, has supported the development of Data QUEST. This approach may be applicable to many PBRNs affiliated with institutions granted Clinical Translational Science Awards (DeVoe et al., 2012). Determining funding streams that allow for flexibility and nimbleness in the initial rollout of data-sharing infrastructures is critical to success, as is developing ongoing resources for maintenance and growth of the infrastructures. Although Clinical Translational Science Awards can play a critical role in development of health data-sharing infrastructures, more diverse funding streams are needed to ensure sustainability. Partnership with the DART-Net Institute allowed us to take advantage of economies of scale, and continued work with grant-funded local, regional, and national investigators will be critical for maintaining and growing the infrastructure in the long term.
Implications
We successfully created a collaborative network of primary care organizations that shares EHR data for research and quality improvement. Appropriately, much attention is devoted to the highly specialized technical aspects of creating data-sharing infrastructure. However, building these infrastructures is a complicated sociotechnical undertaking that also requires consideration of the nontechnical challenges reported here. Two key factors important to facilitating our success were project leadership by a multidisciplinary academic implementation team that included primary care researchers and biomedical informatics experts, and maintaining flexibility and nimbleness throughout the process. A final critical issue was identifying funding sources to support development and maintenance of the data-sharing infrastructure. Our solutions to these nontechnical challenges offer specific and concrete guidance to inform similar efforts for the increasingly prevalent data-sharing efforts in PBRNs.
Acknowledgments
This publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR000423. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors have disclosed that they have no significant relationships with, or financial interest in, any commercial companies pertaining to this article.
Contributor Information
Allison M. Cole, Department of Family Medicine, and WWAMI region Practice and Research Network, University of Washington, Seattle.
Kari A. Stephens, Institute of Translational Health Sciences, and Department of Psychiatry, University of Washington, Seattle.
Gina A. Keppel, Department of Family Medicine, and WWAMI region Practice and Research Network, University of Washington, Seattle.
Ching-Ping Lin, Institute of Translational Health Sciences, and Department of Psychiatry, University of Washington, Seattle.
Laura-Mae Baldwin, Department of Family Medicine, and WWAMI region Practice and Research Network, University of Washington, Seattle.
References
- Agency for Healthcare Research and Quality. (n.d.) Health information technology portfolio program overview. Retrieved September 9, 2013, from http://healthit.ahrq.gov/program-overview.
- Brown AE, Pavlik VN. Patient-centered research happens in practice-based research networks. Journal of the American Board of Family Medicine. 2013;26(5):481–483. doi: 10.3122/jabfm.2013.05.130201. [DOI] [PubMed] [Google Scholar]
- Calmbach WL, Ryan JG, Baldwin LM, Knox L. Practice-based research networks: meeting the challenges of the future. Journal of the American Board of Family Medicine. 2012;25(5):572–576. doi: 10.3122/jabfm.2012.05.120064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delaney BC, Peterson KA, Speedie S, Taweel A, Arvantis TN, Hobbs FD. Envisioning a learning health care system: the electronic primary care research network, a case study. Annals of Family Medicine. 2012;10(1):54–59. doi: 10.1370/afm.1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVoe JE, Likuahuwa S, Eiff MP, Nelson CA, Carroll JE, Hill CN, et al. Kullberg PA. Lessons learned and challenges ahead: report from the OCHIN Safety Net West practice based research network. Journal of the American Board of Family Medicine. 2012;25(5):560–564. doi: 10.3122/jabfm.2012.05.120141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green LA, Dovey SM. Practice based primary care research networks. They work and are ready for full development and support. BMJ. 2001;322(7286):567–568. doi: 10.1136/bmj.322.7286.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartung DM, Guise JM, Fagnan LJ, Davis MM, Stange KC. Role of practice-based research networks in comparative effectiveness research. Journal of Comparative Effectiveness Research. 2012;1(1):45–55. doi: 10.2217/cer.11.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao CJ, Jha AK, King J, Patel V, Rurukawa MF, Mostashari F. Adoption and routine use of electronic health records among U.S. office based physicians [published online ahead of print July 9, 2013] Health Affairs (Millwood) 2013;32(8) doi: 10.1377/hlthaff.2013.0323. Retrieved from www.healthaffairs.org. [DOI] [PubMed] [Google Scholar]
- Lin CP, Black RA, Laplante J, Keppel GA, Tuzzio L, Berg AO, et al. Stephens KA. Facilitating health data sharing across diverse practices and communities. AMIA Summits on Translational Science Proceedings. 2010;2:16–20. [PMC free article] [PubMed] [Google Scholar]
- Mold JW, Lipman PD, Durako SJ. Coordinating centers and multi-practice-based research network research. Journal of the American Board of Family Medicine. 2012;25(5):577–581. doi: 10.3122/jabfm.2012.05.110302. [DOI] [PubMed] [Google Scholar]
- Pace WD, Cifuentes M, Valuck RJ, Staton EW, Brandt EC, West DR. An electronic practice-based network for observational comparative effectiveness research. Annals of Internal Medicine. 2009;151(5):338–340. doi: 10.7326/0003-4819-151-5-200909010-00140. [DOI] [PubMed] [Google Scholar]
- Pace WD, Staton EW. Electronic data collection options for practice based research networks. Annals of Family Medicine. 2005;3:S21–S29. doi: 10.1370/afm.270. 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patient-Centered Outcomes Research Institute. (n.d.) Clinical Data Research Network (CDRN): Improving infrastructure for conducting patient-centered outcomes research (PCOR) Retrieved December 9, 2013, from http://pcori.org/funding-opportunities/funding-announcements/clinical-data-research-networks-cdrn-improving-infrastructure-for-conducting-patient-centered-outcomes-research-pcor/
- Peterson KA, Delaney BC, Arvantis TN, Taweel A, Sandberg EA, Speedie S, et al. Hobbs R. A model for the electronic support of practice-based research networks. Annals of Family Medicine. 2012;10(6):560–567. doi: 10.1370/afm.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens KA, Lin CP, Baldwin LM, Echo-Hawk A, Keppel GA, Buchwald D, et al. Tarczy-Hornoch P. LC Data QUEST: A technical architecture for community federated clinical data sharing. AMIA Summits on Translational Science Proceeding. 2012;2012:57–62. [PMC free article] [PubMed] [Google Scholar]
- Stephens KA, Anderson N, Lin C. Developing best practices for evaluating federated data sharing: Approaches from academic hospital and primary care clinic networks; Abstract and poster presented at the annual meeting of the American Medical Informatics Association; Washington, DC. 2010. Nov, [Google Scholar]


