Abstract
There currently exist a great number of different mouse lines in which the activity of a particular gene of interest has been inactivated or enhanced. However, it is also possible to insert specific mutations in a gene so that the pharmacological sensitivity of the gene product is altered. An example of such an approach shows how the abolition of the sensitivity of an L-type Ca2+ channel isoform to dihydropyridines allows the investigation of the physiological role of these channels in different tissues .
The LTCC family
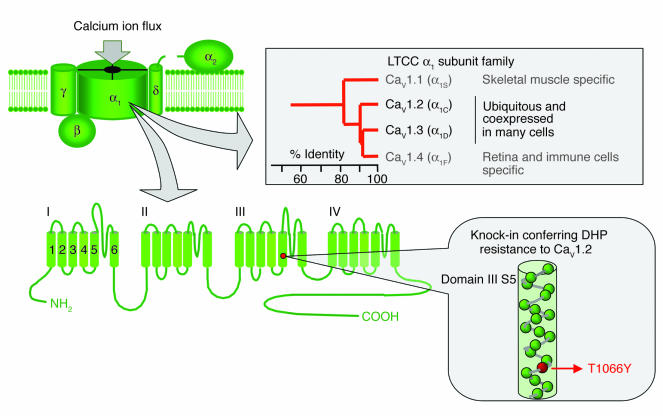
L-type Ca2+ channels (LTCCs) are formed by different pore-forming α1 subunit isoforms named Cav1.1, Cav1.2, Cav1.3, and Cav1.4 associated to auxiliary subunits (α2-δ, β, and γ) (1). The common pharmacological hallmark of all native and recombinant LTCCs is their sensitivity to dihydropyridines (DHPs). However, the small differences among the LTCC α1 isoforms in their affinity for DHPs (agonists and antagonists) have limited the study of the functional role of these channels in various tissues, including the cardiovascular system, the brain, and the endocrine glands.
In this issue of the JCI, Sinnegger-Brauns and coworkers report that they have developed a new mouse model resulting from a knock-in mutation of the CaV1.2 voltage-dependent LTCC subunit which abolishes the sensitivity of the channel to DHP (referred to herein as the CaV1.2DHP–/– mouse) (see Figure 1) (2). Since Cav1.2 is almost ubiquitously expressed in excitable cells, the model provides a very elegant and promising approach for investigating the physiological role of the other DHP-sensitive LTCC isoforms (Cav1.1, Cav1.3, and Cav1.4). This model is particularly useful for the exploration of the function of Cav1.3 channels, which are coexpressed with Cav1.2 but at a much lower level in most cell types investigated so far. The Cav1.1 subunit is responsible for excitation-contraction coupling in skeletal muscle (3), while Cav1.4 expression appears to be restricted to the retina and T lymphocytes (4–6). In contrast to the tissue-specific expression of Cav1.1 and Cav1.4, both Cav1.2 and Cav1.3 are widely expressed and distributed in the brain, the cardiovascular system, and neuroendocrine cells.
Figure 1.
LTCCs are multimeric complexes of subunits formed by an α1 pore-forming protein associated to three auxiliary subunits (α2-δ, β, and γ). Four genes encode the pore-forming subunit (Cav1.1_Cav1.4). The primary structure, α1, is represented in the figure showing the four domains composed of six transmembrane segments. Schematic representation of the knock-in mutation in the CaV1.2 gene (Thr1066 to Tyr) realized by Sinnegger-Brauns and coworkers in this issue of the JCI (2) to discriminate in vivo the contributions of CaV1.2 and CaV1.3 to various physiological functions.
Cav1.2 versus Cav1.3 in insulin secretion
Using the CaV1.2DHP–/– mice that exhibit a normal phenotype in spite of their DHP-insensitive Cav1.2 channels, the authors have been able to differentiate, both in vivo and in vitro, the roles of the Cav1.2 and Cav1.3 channels in insulin secretion, cardiac performance, and mood behavior (2). In particular, the finding that insulin secretion in these mice was completely insensitive to DHP agonists and antagonists provides strong evidence in the long-standing debate about the insulin secretagogue role of the Cav1.2 and Cav1.3 channels. Opposite conclusions about the importance of the Cav1.3 LTCC in this secretion process have been drawn by two previous studies using different mouse strains lacking the Cav1.3 LTCC (7, 8) and a β-cell–specific knockout of the Cav1.2 LTCC (9). The complete resistance of the insulin secretory process to DHPs in the CaV1.2DHP–/– mice strongly supports the minor role of Cav1.3 in this process.
LTCC isoforms in mood behavior
Another important aspect of the study concerns the role of the Cav1.3 LTCC in integrated neuronal functions. While the expression of the Cav1.2 LTCC isoform accounts for about 80% of the overall DHP-binding sites in the brain, the remaining 20% of binding can be attributed to Cav1.3 LTCCs, and little was known about the function of these channels. Indeed, DHP agonists such as BayK8644 cannot be used in vivo because of potent neurotoxic effects mediated by Cav1.2 channels. Abolition of the sensitivity of the Cav1.2 channel to DHPs allowed unmasking of a depression-like behavioral effect mediated by Cav1.3 channels (2). From a molecular point of view, these effects may rely on the recently identified specific interactions of the CaV1.3 channel with synaptic proteins (10), with possible consequences related to the control of neurotransmitter release classically implicated in depression (as shown by Sinnegger-Brauns et al. in the case of dopamine). Therefore, an attractive prospective application of these findings is in the development of new classes of antidepressant drugs that act selectively on Cav1.3 channels.
Relevance of the CaV1.2DHP–/– mouse in the study of heart physiology
The CaV1.2DHP–/– mouse model can also help to reveal the functional role of LTCCs in the physiology of the heart. It is widely accepted that the Cav1.2 subunit constitutes the most abundant LTCC subunit in the heart, where it plays an important role in excitation-contraction coupling in the working myocardium. In addition, a growing body of evidence indicates that the functional roles of Cav1.2 and Cav1.3 channels are distinct in the heart, with Cav1.3 channels playing a major role in pacemaker activity. Indeed, the fact that mice in which the gene encoding the Cav1.3 subunit has been inactivated show prominent dysfunctions in pacemaker activity in vivo and in vitro demonstrates that Cav1.3 channels constitute the major component of the L-type current in pacemaker cells (8, 11, 12). Experimental results presented by Sinnegger-Brauns and coworkers clearly support this view (2). More generally, the use of engineered mice such as CaV1.2DHP–/– mice will be of particular interest to further assess the contribution of the different ionic currents underlying diastolic depolarization in sinoatrial pacemaker cells. Automaticity in cardiac pacemaker cells is due to the slow diastolic depolarization phase, which drives the membrane voltage from the end of the action potential to the threshold of the following action potential. Both native and recombinant Cav1.3 channels exhibit more negative threshold for activation and slower inactivation kinetics than Cav1.2 channels. In other words, the low threshold of Cav1.3 current is consistent with a major role during diastolic depolarization (12), while a sustained calcium influx is required for the contractility of heart cells.
In conclusion, the originality of this model offers stimulating prospects for dissecting the physiological roles of calcium channels in various tissues (2). This genetic “reverse” pharmacology in vivo is likely to be applied in the future to other channels and receptor families sharing a similar pharmacology.
Footnotes
See the related article beginning on page 1430.
Nonstandard abbreviations used: dihydropyridine (DHP); L-type Ca2+ channel (LTCC).
Conflict of interest: The authors have declared that no conflict of interest exists.
References
- 1.Striessnig J. Pharmacology, structure and function of cardiac L-type Ca(2+) channels. Cell. Physiol. Biochem. 1999;9:242–269. doi: 10.1159/000016320. [DOI] [PubMed] [Google Scholar]
- 2.Sinnegger-Brauns MJ, et al. Isoform-specific regulation of mood behavior and pancreatic β cell and cardiovascular function by L-type Ca2+ channels. J. Clin. Invest. 2004;113:1430–1439. doi:10.1172/JCI200420208. doi: 10.1172/JCI20208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanabe T, Beam KG, Powell JA, Numa S. Restoration of excitation-contraction coupling and slow calcium current in dysgenic muscle by dihydropyridine receptor complementary DNA. Nature. 1988;336:134–139. doi: 10.1038/336134a0. [DOI] [PubMed] [Google Scholar]
- 4.McRory JE, et al. The CACNA1F gene encodes an L-type calcium channel with unique biophysical properties and tissue distribution. J. Neurosci. 2004;24:1707–1718. doi: 10.1523/JNEUROSCI.4846-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kotturi MF, Carlow DA, Lee JC, Ziltener HJ, Jefferies WA. Identification and functional characterization of voltage-dependent calcium channels in T lymphocytes. J. Biol. Chem. 2003;278:46949–46960. doi: 10.1074/jbc.M309268200. [DOI] [PubMed] [Google Scholar]
- 6.Koschak A, et al. Cav1.4alpha1 subunits can form slowly inactivating dihydropyridine-sensitive L-type Ca2+ channels lacking Ca2+-dependent inactivation. J. Neurosci. 2003;23:6041–6049. doi: 10.1523/JNEUROSCI.23-14-06041.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Namkung Y, et al. Requirement for the L-type Ca(+) channel alpha(1D) subunit in postnatal pancreatic beta cell generation. J. Clin. Invest. 2001;108:1015–1022. doi:10.1172/JCI200113310. doi: 10.1172/JCI13310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Platzer J, et al. Congenital deafness and sinoatrial node dysfunction in mice lacking class D L-type Ca2+ channels. Cell. 2000;102:89–97. doi: 10.1016/s0092-8674(00)00013-1. [DOI] [PubMed] [Google Scholar]
- 9.Schulla V, et al. Impaired insulin secretion and glucose tolerance in beta cell-selective Ca(v)1.2 Ca2+ channel null mice. EMBO J. 2003;22:3844–3854. doi: 10.1093/emboj/cdg389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hibino H, et al. RIM binding proteins (RBPs) couple Rab3-interacting molecules (RIMs) to voltage-gated Ca(2+) channels. Neuron. 2002;34:411–423. doi: 10.1016/s0896-6273(02)00667-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Z, et al. Functional roles of Ca(v)1.3 (alpha(1D)) calcium channel in sinoatrial nodes: insight gained using gene-targeted null mutant mice. Circ. Res. 2002;90:981–987. doi: 10.1161/01.res.0000018003.14304.e2. [DOI] [PubMed] [Google Scholar]
- 12.Mangoni ME, et al. Functional role of L-type Cav1.3 Ca2+ channels in cardiac pacemaker activity. Proc. Natl. Acad. Sci. U. S. A. 2003;100:5543–5548. doi: 10.1073/pnas.0935295100. [DOI] [PMC free article] [PubMed] [Google Scholar]