INTRODUCTION
Squamous cell carcinoma is by far the most important and the most common malignant mucosal neoplasm of the head and neck accounting for over 90% of all malignancies. Conventional oral squamous cell carcinoma (OSCC) can present as several variants that make up in aggregate about 10-15% of all squamous cell carcinomas (SCC).[1] These variants include verrucous carcinoma (VC), adenoid/acantholytic/pseudoglandular SCC (AdSCC), spindle cell/sarcomatoid carcinoma (SCSC), adenosquamous carcinoma (ASC), basaloid SCC (BSCC) and papillary SCC (PSCC). Each of these variants has a unique histomorphological appearance. This is a short treatise designed to give a brief overview of the different histopathological variants of OSCC observed in our institute, the separation of which helped in achieving appropriate clinical management.
CASE REPORT
A brief overview of the clinico-pathological appearance of variants of OSCC cases reported in the Department of Oral and Maxillofacial Pathology is presented in Table 1.
Table 1.
Clinicopathological appearance of the reported cases of OSCC variants
DISCUSSION
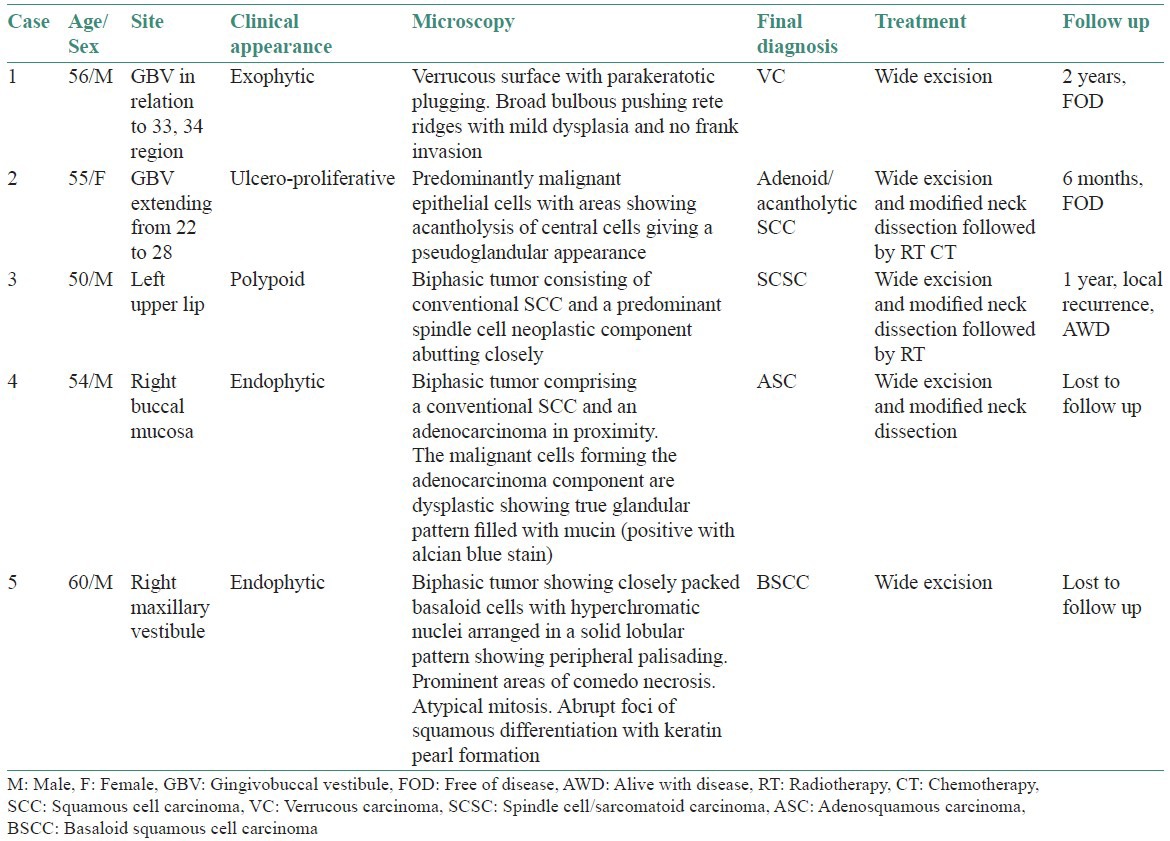
Conventional SCC [Figure 1] and variants of OSCC frequently arise within the oral cavity. Precise histopathological diagnosis can help the clinician to plan accurate treatment, as the prognosis of each of them differs considerably.
Figure 1.
Conventional oral squamous cell carcinoma-malignant epithelial islands showing keratin pearl formation. (H&E stain, ×100)
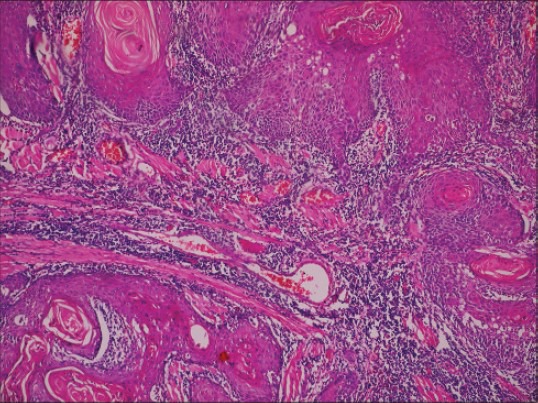
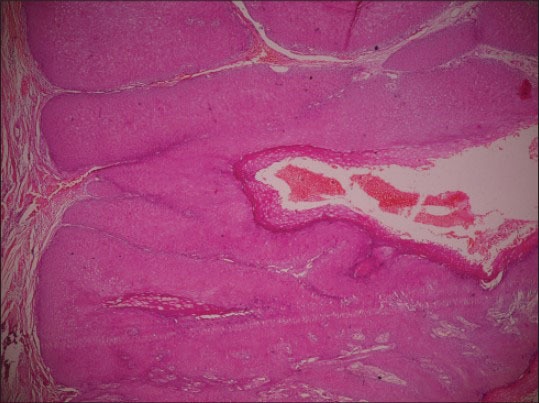
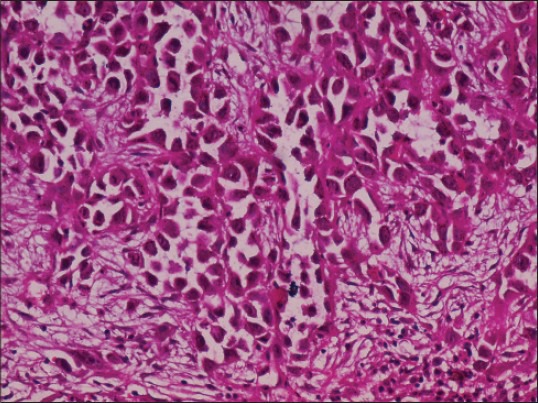
VC [Figure 2] is a very well-differentiated SCC that does not metastasize and has an excellent prognosis with 5-year survival rate of approximately 75%.[2] The lesion has a possibility of metastasis only if it is left long enough and allowed to become more invasive. AdSCC [Figure 3] occurs in the oral cavity infrequently as they usually affect sun-exposed areas with vermillion border of the lip being the most commonly affected site. They have a relative poorer prognosis as compared with conventional SCC [Figure 1]. SCSC [Figure 4] metastasizes to the regional lymph nodes in upto 25% cases, but distant metastasis is less common (5-15%). The 5-year survival rate varies between 65-95%.[1,3] ASC [Figure 5] has an aggressive behavior, poorer prognosis and a propensity for locoregional and distant metastasis, especially to the lungs. Larynx is most commonly affected (70%) followed by the oral cavity (30%). It shows approximately 2-year survival rate of approximately 55%. BSCC [Figure 6] is regarded as a high-grade tumor with an increased propensity for distant metastasis. It requires aggressive multimodality treatment. The 2-year survival rate is 40%.[4] PSCC more frequently affects the larynx. It has a better prognosis when compared with location and stage-matched conventional OSCC.[5]
Figure 2.
Verrucous carcinoma-broad bulbous pushing rete ridges with parakeratotic plugging (H&E stain, ×100)
Figure 3.
Adenoid squamous cell carcinoma -pseudoglandular pattern with acantholytic tumor cells. (H&E stain, ×200)
Figure 4.
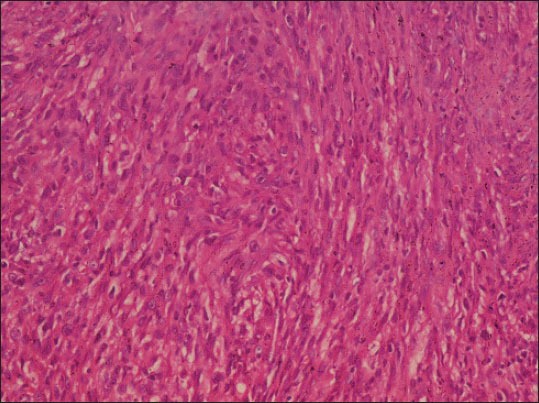
Spindle cell carcinoma-malignant epithelial cells showing spindling/sarcomatoid appearance (H&E stain, ×100)
Figure 5.
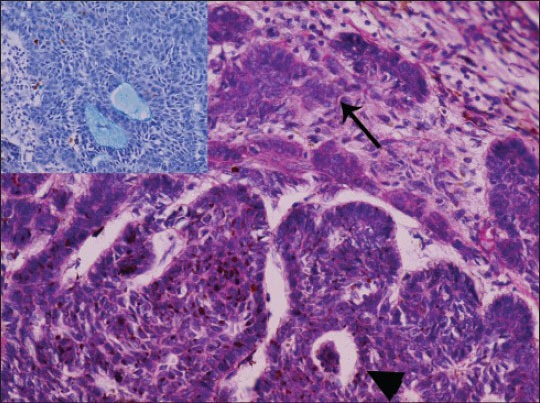
Adenosquamous carcinoma-biphasic tumor showing true glandular differentiation (arrowhead) along with squamous differentiation (arrow) (H&E stain, ×100). Inset depicts alcian bluepositive mucin secretion (×400)
Figure 6.
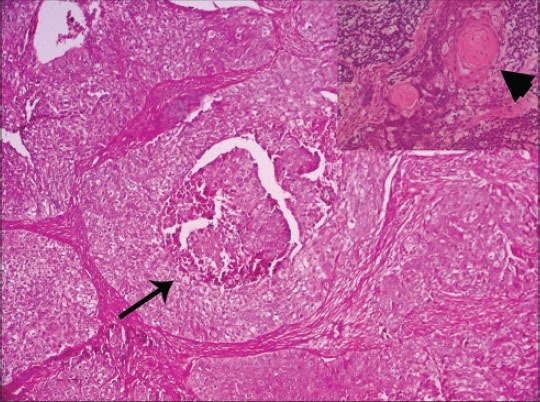
Basaloid squamous cell carcinoma biphasic tumor showing basaloid malignant islands with peripheral palisading and comedonecrosis (arrow) (H&E stain, ×100). Inset depicts squamous differentiation with keratin pearl formation (arrowhead) (H&E stain, ×100)
CONCLUSION
Histopathological variants of OSCC may pose a diagnostic challenge especially the SCSC and ASC, which warrants the use of immunohistochemistry and special stains for an accurate diagnosis. The prognosis, metastatic potential, survival rate and treatment of each of the variants are diverse, thus mandating their distinction.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Thompson LD. Squamous cell carcinoma variants of the head and neck. Curr Diagn Pathol. 2003;9:384–96. [Google Scholar]
- 2.Koch BB, Trask DK, Hoffman HT, Karnell LH, Robinson RA, Zhen W, et al. National survey of head and neck verrucous carcinoma: Patterns of presentation, care, and outcome. Cancer. 2001;92:110–20. doi: 10.1002/1097-0142(20010701)92:1<110::aid-cncr1298>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 3.Viswanathan S, Rahman K, Pallavi S, Sachin J, Patil A, Chaturvedi P, et al. Sarcomatoid (spindle cell) carcinoma of the head and neck mucosal region: A clinicopathologic review of 103 cases from a tertiary referral cancer centre. Head Neck Pathol. 2010;4:265–75. doi: 10.1007/s12105-010-0204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cardesa A, Zidar N, Ereño C. Basaloid squamous cell carcinoma. In: Barnes L, editor. World Health Organization Classification of Tumors. Pathology & Genetics of Head and Neck Tumours. Lyon: IARC Press; 2005. [Google Scholar]
- 5.Thompson LD, Wenig BM, Heffner DK, Gnepp DR. Exophytic and papillary squamous cell carcinomas of the larynx: A clinicopathologic series of 104 cases. Otolaryngol Head Neck Surg. 1999;120:718–24. doi: 10.1053/hn.1999.v120.a92773. [DOI] [PubMed] [Google Scholar]


